Abstract
Background:
Omega-3 fatty acids from fish have been shown to have favorable effects on platelet aggregation, blood pressure, lipid profile, endothelial function, and ischemic stroke risk, but there are limited data on racial and geographic differences in fish consumption.
Methods:
Reasons for Geographic and Racial Differences in Stroke (REGARDS) is a national cohort study that recruited 30,239 participants age ≥45 years with oversampling from the southeastern Stroke Belt and Buckle and African Americans (AAs). Centralized phone interviewers obtained medical histories and in-home examiners measured weight and height. Dietary data for this cross-sectional analysis were collected using the self-administered Block98 Food Frequency Questionnaire (FFQ). Adequate intake of nonfried fish was defined as consumption of ≥2 servings per week based on American Heart Association guidelines. After excluding the top and bottom 1% of total energy intake and individuals who did not answer 85% or more of questions on the FFQ, the analysis included 21,675 participants.
Results:
Only 5,022 (23%) participants consumed ≥2 servings per week of nonfried fish. In multivariable analysis, factors associated with inadequate intake of nonfried fish included living in the Stroke Belt (vs non-Belt) (odds ratio [OR] 0.83, 95% confidence interval [CI] 0.77–0.90) and living in the Stroke Buckle (vs non-Belt) (OR 0.89, 95% CI 0.81–0.98); factors associated with ≥2 servings per week of fried fish included being AA (vs white) (OR 3.59, 95% CI 3.19–4.04), living in the Stroke Belt (vs non-Belt) (OR 1.32, 95% CI 1.17–1.50), and living in the Stroke Buckle (vs non-Belt) (OR 1.17, 95% CI 1.00–1.36).
Conclusions:
Differential consumption of fish may contribute to the racial and geographic disparities in stroke.
Fish consumption represents the main dietary source of the long-chain omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). These omega-3 fatty acids have been shown to have favorable effects on platelet aggregation, blood pressure, lipid profile, endothelial function, and ischemic stroke risk.1–9 In addition, EPA and DHA supplements have been shown to reduce the risk of major cardiovascular events in 2 randomized clinical trials.10,11 Results from these studies and others led to the American Heart Association (AHA) recommendation on dietary fish intake: consumption of at least 2 fish meals per week with an emphasis on oily fish for patients without documented cardiovascular disease and to consider additional supplements of EPA and DHA for those with documented cardiovascular disease.12
While it remains unclear if fish intake represents a surrogate for some other underlying healthy lifestyle factors,13 growing evidence suggests that the benefits are the result of nutrients within fish (e.g., omega-3 fatty acids).1–9 Alternatively, the act of frying fish has been associated with loss of these natural fatty acids in the fish and replacement with cooking oil.14 Given the evidence associating fish consumption with reduced risk of ischemic stroke,15–20 racial and geographic differences in fish consumption may represent one of the potential reasons for the racial and geographic differences in stroke incidence and mortality.21
The objective of this study was to examine racial and geographic differences in fish consumption among men and women participating in the Reasons for Geographic and Racial Differences in Stroke (REGARDS) Study.
METHODS
Study design.
REGARDS is a national, population-based, longitudinal cohort study with oversampling of African Americans (AAs) and persons living in the Stroke Belt region of the United States, an area that has stroke mortality rates higher than the rest of the country.22 Between January 2003 and October 2007, 30,239 individuals were enrolled, including 42% AA/58% white, 45% men and 55% women. The sample includes 21% of participants from the Stroke Belt Buckle (coastal plain region of North Carolina, South Carolina, and Georgia), 35% from the Stroke Belt states (remainder of North Carolina, South Carolina, and Georgia, plus Alabama, Mississippi, Tennessee, Arkansas, and Louisiana), and the remaining 44% from the other 40 contiguous states (referred to as non-Belt).
REGARDS participants were selected from commercially available lists (Genesys). A letter and brochure informed participants of the study and the upcoming phone call. During the call, verbal consent was obtained and a 45-minute questionnaire was administered. The telephone response rate was 33% and the cooperation rate was 49% (similar to the Multi-Ethnic Study of Atherosclerosis, which had a 39.8% participation rate among those contacted and to whom the study was explained).23 The questionnaire included questions on demographics, previous history of cardiovascular disease, and stroke and risk factors. After the survey, we asked the participants if they would be interested in participating in an in-home examination. Approximately 70% of people agreed to allow a person to come into the home to collect blood pressure, height, and weight measures, blood, and to perform an EKG. During the in-home visit, all medications and supplements used within the past 2 weeks were recorded and these listings were coded at the coordinating center. Self-administered questionnaires including the Block98 Food Frequency Questionnaire (FFQ) (NutritionQuest™, Berkeley, CA) were left with the participant to gather information. Participants were considered to be enrolled in the study if they completed the 45-minute telephone questionnaire and the in-person physical examination.
Standard protocol approvals, registrations, and patient consents.
The study methods have been reviewed and approved by the institutional review boards of participating institutions. Written informed consent was obtained from all participants who completed the in-home visit.
Dietary assessment.
This FFQ has been used extensively in the National Health and Nutrition Examination Survey (NHANES III) cohort and was validated in a population similar to REGARDS. It is an 8-page document that assesses usual dietary intake over the past year. The 5 questions specific to fish intake were the following: 1) How often do you eat oysters? 2) How often do you eat other shellfish like shrimp, scallops, or crabs? 3) How often do you eat tuna, tuna salad, or tuna casserole? 4) How often do you eat fried fish or a fish sandwich, at home or in a restaurant? 5) How often do you eat other fish, not fried? Participants select from the following options for each question: never, a few times per year, once per month, 2–3 times per month, once per week, twice per week, 3–4 times per week, 5–6 times per week, and every day. Participants also answered questions about usual portion size based on pictures provided. The study had an active tracking process to contact participants to return languishing questionnaires. Completed forms were received back from 72% of participants. After excluding the top and bottom 1% of total energy (kcal) intake and any individuals who did not answer 85% or more of the questions on the FFQ (n = 8,564), the primary analysis cohort included 21,675 participants of the 30,239 enrolled.
Measurements and variables.
One serving of fish is equivalent to 3 ounces.24 Fish intakes were calculated as the frequency of intake multiplied by the specified portion size. Adequate intake of nonfried fish was defined as consumption of ≥2 servings per week, modified from the AHA guidelines.12 Fish intakes included intakes of shellfish such as shrimp, scallops, and crabs, tuna including tuna salad and tuna casserole, oyster, fried fish, or fish sandwich, and other nonfried fish. Total fish consumption is the sum of all fish intake and nonfried fish consumption is the sum of all fish intake excluding the fried fish or fish sandwich. Fish oil supplements were composed of any medications, vitamins, or supplements under the names omega-3, fish oil, eicosapentaenoic acid, docosahexaenoic acid, Lovaza, or linolenic acid. Factors including age, sex, race, region, education, and income, body mass index (BMI) categories based on Centers for Disease Control and Prevention guidelines for adults, and energy intake in calories were also considered as potential covariates.
Statistical analyses.
All statistical analyses were performed using SAS 9.1.3; level of significance was assessed at α = 0.05. Descriptive characteristics comparing frequencies were assessed using Pearson χ2 statistics. Analysis of variance was used to test for differences in fish consumption adjusting for energy intake. All tests of associations were assessed by χ2 statistics. Logistic regression models were used to calculate odds ratios (ORs) in multivariable models and the ORs confidence intervals (CIs) were adjusted using the Wald statistic.
RESULTS
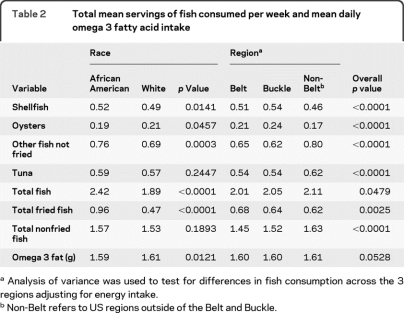
Of the study participants (n = 21,675), 34% were AA, 56% were female, 56% lived in the Stroke Belt, 74% were overweight (BMI ≥25.0), and mean (SD) age was 64.9 (9.26) years (table 1). Comparison of the study participants with those excluded from this analysis revealed that those excluded were more likely to be female, black, older than 75 years, obese, to live outside of the Stroke Belt and Buckle, and to have less than a high school education than our primary analysis cohort (data not shown).
Table 1.
Descriptive characteristics of the subjects in REGARDSa
Abbreviations: REGARDS = Reasons for Geographic and Racial Differences in Stroke.
For all variables, differences between black and white subjects were significant at p < 0.0001.
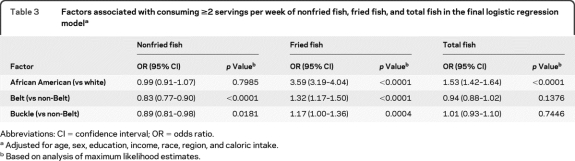
Energy-adjusted weekly servings of fish and daily omega-3 fat intakes are shown in table 2 stratified by race and region. Total mean servings of fish consumed per week were higher in AA than white subjects (2.42 vs 1.89, p < 0.0001), which included intakes predominantly from fried fish (0.96 vs 0.47, p < 0.0001). Total mean servings of nonfried fish consumed per week were similar for AA and white subjects although AA subjects had lower mean intakes of omega-3 fatty acids than white subjects, 1.59 vs 1.61 g per week (p < 0.0121). Only 1,329 (6%) participants reported current use of fish oil supplements, including 5.1% of white subjects and 1.0% of AA subjects (p < 0.0001).
Table 2.
Total mean servings of fish consumed per week and mean daily omega 3 fatty acid intake
Analysis of variance was used to test for differences in fish consumption across the 3 regions adjusting for energy intake.
Non-Belt refers to US regions outside of the Belt and Buckle.
Geographic differences in fish consumption were also found. Total mean servings of fish consumed per week were lower in study participants living in the Stroke Belt and Stroke Buckle than those living elsewhere (Belt 2.01, Buckle 2.05 vs non-Belt 2.11, p < 0.05), which included intakes predominantly from lower nonfried fish (Belt 1.45, Buckle 1.52 vs non-Belt 1.63, p < 0.05). Total mean servings of fried fish consumed per week were higher in participants living in the Stroke Belt compared with those living in the Stroke Buckle and elsewhere (Belt 0.68 vs Buckle 0.64, non-Belt 0.62, p < 0.05). No geographic differences in mean weekly intakes of omega-3 fat or use of fish oil supplements were seen.
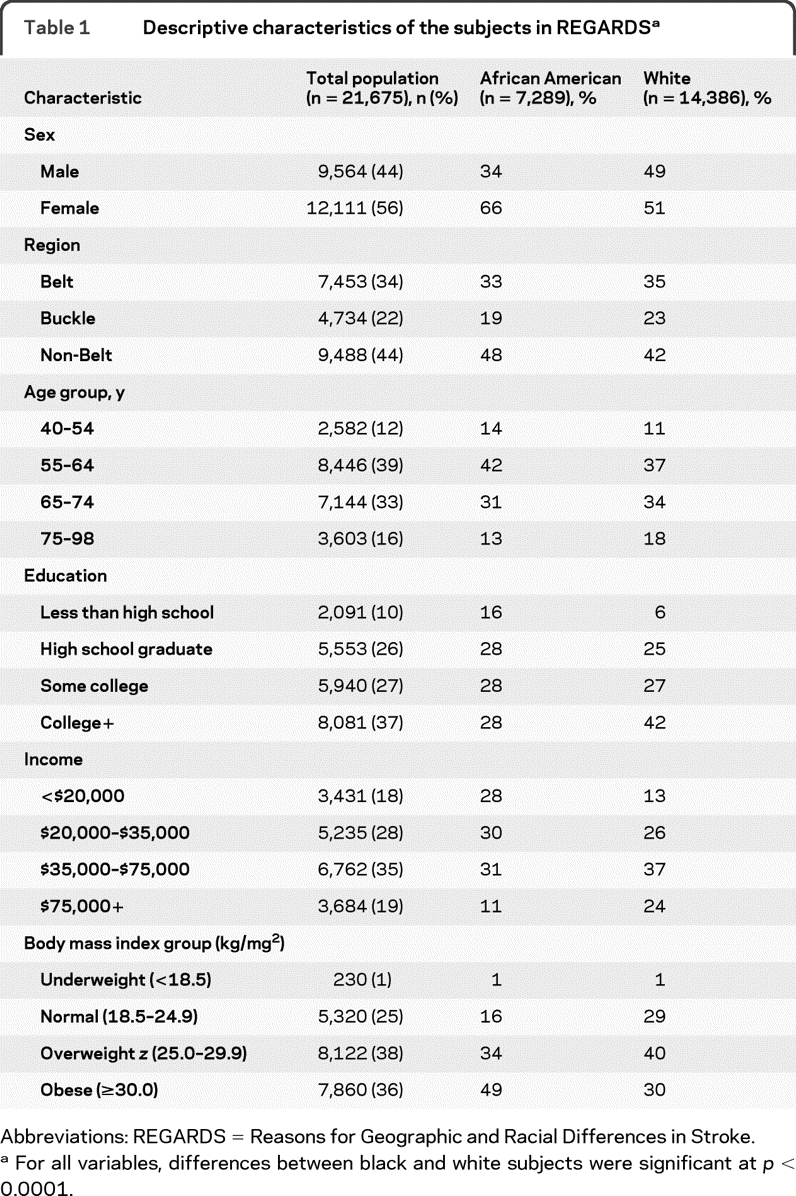
Only 5,022 (23%) participants consumed ≥2 servings per week of nonfried fish using our modified definition of the AHA recommendation. In multivariable analysis including adjustment for age, sex, education, income, race, region, and caloric intake, factors associated with inadequate intake of nonfried fish included living in the Stroke Belt (vs non-Belt) (OR 0.83, 95% CI 0.77–0.90) and living in the Stroke Buckle (vs non-Belt) (OR 0.89, 95% CI 0.81–0.98) (table 3). Factors associated with ≥2 servings per week of fried fish included being AA (vs white) (OR 3.59, 95% CI 3.19–4.04), living in the Stroke Belt (vs non-Belt) (OR 1.32, 95% CI 1.17–1.50), and living in the Stroke Buckle (vs non-Belt) (OR 1.17, 95% CI 1.00–1.36).
Table 3.
Factors associated with consuming ≥2 servings per week of nonfried fish, fried fish, and total fish in the final logistic regression modela
Abbreviations: CI = confidence interval; OR = odds ratio.
Adjusted for age, sex, education, income, race, region, and caloric intake.
Based on analysis of maximum likelihood estimates.
DISCUSSION
Our cross-sectional study found that while AA subjects consumed more total fish than white subjects, most of the additional consumption was in the form of fried fish. In addition, participants living in the Stroke Belt and Stroke Buckle were less likely to consume ≥2 weekly servings of nonfried fish but more likely to consume ≥2 weekly servings of fried fish than those living elsewhere. These differences remained evident even after adjusting for potential confounders including age, gender, education, income, race, and total energy intake.
Our findings are consistent with racial and geographic differences in fish consumption previously reported from the Foods of Our Delta 2000 study and a small community-based study.25,26 The only other national study to evaluate racial differences in fish consumption in the United States was NHANES III, which found that white and AA adults below 60 years obtained similar percentages of their total daily protein from fish though older AA subjects (≥60 years) had higher percentages of protein derived from fish intake compared with white subjects.27
The benefits of fish consumption may be related to the type of fish and cooking methods. While all fish contain EPA and DHA, the quantities vary among and within species depending on their diet and if the fish are wild or farm-raised. Fatty fish such as salmon, herring, and mackerel have significantly higher EPA and DHA content than lean fish such as cod and haddock.28 Farm-raised catfish have less EPA and DHA than do wild catfish. In the United States, most fish served fried tends to be from lean species.12 In addition, the act of frying fish has been associated with loss of natural fatty acids in the fish and replacement with cooking oil.14 For these reasons, we defined adequate fish intake based only on nonfried fish, a modification of the AHA guidelines, which advise ≥2 servings per week of preferably oily fish but do not specify the cooking method.
Limitations of our study include the cross-sectional design which cannot account for dietary changes over time. While the use of a FFQ allows for measurement of usual and long-term dietary intakes of individuals, disadvantages include its inaccuracy of absolute intakes and lack of detail regarding specific foods consumed. Additionally, we were unable to directly measure fatty fish intake from the FFQ. Finally, it is difficult to speculate how the results may or may not have been different if all REGARDS Study participants had completed their FFQs.
ACKNOWLEDGMENT
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Footnotes
- AA
- African American
- AHA
- American Heart Association
- BMI
- body mass index
- CI
- confidence interval
- DHA
- docosahexaenoic acid
- EPA
- eicosapentaenoic acid
- FFQ
- Food Frequency Questionnaire
- NHANES
- National Health and Nutrition Examination Survey
- OR
- odds ratio
- REGARDS
- Reasons for Geographic and Racial Differences in Stroke
AUTHOR CONTRIBUTIONS
Statistical analysis was conducted by A. Le and S. Judd.
DISCLOSURE
Dr. Nahab has received honoraria from the National Stroke Association and Imedex. Ms. Le reports no disclosures. Dr. Judd receives research support from the NIH/NINDS. Dr. Frankel receives research support from the NIH/NINDS and from Emory Healthcare Neuroscience Center. Dr. Ard receives research support from the NIH (NHLBI, CCTS and NIA), UAB Comprehensive Cancer Center, and the Robert Wood Johnson Foundation. Dr. Newby serves as a Contributing Editor to Nutrition Reviews; and receives/has received research support from General Mills Bell Institute of Health and Nutrition, the USDA, and the American Diabetes Association. Dr. Howard receives research support from the NIH/NINDS, serves on a scientific advisory board for and has received funding for travel from Amgen; her spouse serves on scientific advisory boards for Bayer Schering Pharma, Boehringer Ingelheim, Mitsubishi Tanabe Pharma Corporation, PhotoThera, and MediciNova, Inc.; her spouse has served as a legal consultant for Merck & Co., Inc.; and receives research support from the NIH (NINDS, NIDDK and NIOSH).
REFERENCES
- 1. Anand RG, Alkadri M, Lavie CJ, et al. The role of fish oil in arrhythmia prevention. J Cardiopulm Rehabil Prev 2008;28:2–8 [DOI] [PubMed] [Google Scholar]
- 2. O'Keefe JH, Jr, Abuissa H, Sastre A, et al. Effects of omega-3 fatty acids on resting heart rate, heart rate recovery after exercise, and heart rate variability in men with healed myocardial infarctions and depressed ejection fraction. Am J Cardiol 2006;97:1127–1130 [DOI] [PubMed] [Google Scholar]
- 3. Ventura HO, Milani RV, Lavie CJ, et al. Cyclosporine-induced hypertension: efficacy of omega-3 fatty acids in patients after cardiac transplantation. Circulation 1993;88:281–285 [PubMed] [Google Scholar]
- 4. Thies F, Garry JM, Yaqoob P, et al. Association of n-3 polyunsaturated fatty acids with stability of atherosclerotic plaques: a randomized controlled trial. Lancet 2003;361:477–485 [DOI] [PubMed] [Google Scholar]
- 5. Din JN, Harding SA, Valerio CJ, et al. Dietary intervention with oil rich fish reduces platelet-monocyte aggregation in man. Atherosclerosis 2008;197:290–296 [DOI] [PubMed] [Google Scholar]
- 6. Geleijnse JM, Giltay EJ, Grobbee DE, et al. Blood pressure response to fish oil supplementation: metaregression analysis of randomized trials. J Hypertens 2002;20:1493–1499 [DOI] [PubMed] [Google Scholar]
- 7. Zhao G, Etherton TD, Martin KR, et al. Dietary alpha-linolenic acid inhibits proinflammatory cytokine productions by peripheral blood mononuclear cells in hypercholesterolemic subjects. Am J Clin Nutr 2007;85:385–391 [DOI] [PubMed] [Google Scholar]
- 8. Mehra MR, Lavie CJ, Ventura HO, et al. Fish oils produce anti-inflammatory effects and improve body weight in severe heart failure. J Heart Lung Transplant 2006;25:834–838 [DOI] [PubMed] [Google Scholar]
- 9. Davidson MH, Stein EA, Bayes HE, Combination of prescription Omega-3 with Simvastatin (COMBOS) Investigators Efficacy and tolerability of adding prescription omega-3 fatty acids 4 g/d to simvastatin 40 mg/d in hypertriglyceridemic patients: an 8-week, randomized, double-blind, placebo-controlled study. Clin Ther 2007;29:1354–1367 [DOI] [PubMed] [Google Scholar]
- 10. Marchioli R, Barzi F, Bomba E, et al. , GISSI-Prevenzione Investigators Early protection against sudden death by n-3 polyunsaturated fatty acids after myocardial infarction: time-course analysis of the results of the Gruppo Italiano per lo Studio della Sopravivenza nell'Infarto Miocardico (GISSI)-Prevenzione. Circulation 2002;105:1897–1903 [DOI] [PubMed] [Google Scholar]
- 11. Yokoyama M, Origasa H, Matsuzaki M, Japan EPA lipid intervention study (JELIS) Investigators Effects of eicosapentaenoic acid on major coronary events in hypercholesterolaemic patients (JELIS): a randomized open-label, blinded endpoint analysis. Lancet 2007;369:1090–1098 [DOI] [PubMed] [Google Scholar]
- 12. Kris-Etherton PM, Harris WS, Appel LJ, American Heart Association Nutrition Committee Fish consumption, fish oil, omega-3 fatty acids, and cardiovascular disease. Circulation 2002;106:2747–2757 [DOI] [PubMed] [Google Scholar]
- 13. Schiepers OJ, de Groot RH, Jolles J, et al. Fish consumption, not fatty acid status, is related to quality of life in a healthy population. Prostaglandins Leukot Essent Fatty Acids Epub 2010 March 4 [DOI] [PubMed] [Google Scholar]
- 14. Candela M, Astiasaran I, Bello J. Deep-fat frying modifies high-fat fish lipid fraction. J Agric Food Chem 1998;46:2793–2796 [Google Scholar]
- 15. He K, Song Y, Daviglus ML, et al. Fish consumption and incidence of stroke: a meta-analysis of cohort studies. Stroke 2004;35:1538–1542 [DOI] [PubMed] [Google Scholar]
- 16. Iso H, Rexrode KM, Stampfer MJ, et al. Intake of fish and omega-3 fatty acids and risk of stroke in women. JAMA 2001;285:304–312 [DOI] [PubMed] [Google Scholar]
- 17. He K, Rimm EB, Merchant A, et al. Fish consumption and risk of stroke in men. JAMA 2002;288:3130–3136 [DOI] [PubMed] [Google Scholar]
- 18. Sauvaget C, Nagano J, Allen N, et al. Intake of animal products and stroke mortality in the Hiroshima/Nagasaki Life Span Study. Int J Epidemiol 2003;32:536–543 [DOI] [PubMed] [Google Scholar]
- 19. Zhang J, Sasaki S, Amano K, et al. Fish consumption and mortality from all causes, ischemic heart disease, and stroke: an ecological study. Prev Med 1999;28:520–529 [DOI] [PubMed] [Google Scholar]
- 20. Gillum RF, Mussolino ME, Madans JH. The relationship between fish consumption and stroke incidence: The NHANES I Epidemiologic Follow-up Study (National Health and Nutrition Examination Survey). Arch Intern Med 1996;156:537–542 [PubMed] [Google Scholar]
- 21. Howard G. Why do we have a stroke belt in the southeastern United States? A review of unlikely and uninvestigated potential causes. Am J Med Sci 1999;317:160–167 [DOI] [PubMed] [Google Scholar]
- 22. Howard VJ, Cushman M, Pulley L, et al. The Reasons for Geographic and Racial Differences in Stroke Study: objectives and design. Neuroepidemiology 2005;25:135–143 [DOI] [PubMed] [Google Scholar]
- 23. Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: objectives and design. Am J Epidemiol 2002;156:871–881 [DOI] [PubMed] [Google Scholar]
- 24. [Accessed March 15, 2010]. Available at: http://www.mypyramid.gov/pyramid/meat_counts_print.html.
- 25. Smit E, Nieto FJ, Crespo CJ, Mitchell P. Estimates of animal and plant protein intake in US adults: results from the Third National Health and Nutrition Examination Survey, 1988–1991. J Am Diet Assoc 1999;99:813–820 [DOI] [PubMed] [Google Scholar]
- 26. Tucker KL, Maras J, Champagne C, et al. A regional food-frequency questionnaire for the US Mississippi Delta. Public Health Nutrition 2005;8:87–96 [PubMed] [Google Scholar]
- 27. Weinrich SP, Priest J, Reynolds W, et al. Body mass index and intake of selected foods in African American men. Public Health Nurs 2007;27:217–229 [DOI] [PubMed] [Google Scholar]
- 28. [Accessed February 8, 2010]; Available at: http://www.health.gov/dietaryguidelines/dga2005/report/html/G2_Analyses.htm#omegafish. [Google Scholar]