Abstract
Background:
Type-2 diabetes mellitus and its complication are becoming more prevalent in Ethiopia. Evidence abound that the most important predictor of reduction of morbidity and mortality due to diabetes complication is the level of glycemic control achieved.
Aims:
The aim is to assess adherence to anti diabetic drug therapy and self management practice among type-2 diabetic patient in Ethiopia.
Patients and Method:
The study consists of two phases. A cross-sectional review of randomly selected 384 case notes of type-2 diabetic patient that attend diabetes mellitus clinic over 3 month and cross-sectional interview, with pre tested adherence and self management and monitoring tool questioner of 347 consecutive patients that attend in Jimma university specialized hospital diabetic clinic.
Result:
Oral hypoglycemic agent were prescribed for 351(91.4) of the patient while insulin and oral hypoglycemic agent was prescribed in 33(8.6%). About 312 (88.9%) patients on oral hypoglycemic agent were on mono therapy, the most frequently prescribed oral hypoglycemic agent was glibenclamide 232(74.3%) and metformine 80(25.7%). Only 41.8% of the patient had adequate glycemic control. The main external factors for non adherence were lack of finance (37.1%) followed by perceived side effect of drug 29.2%. Only 6.5% patient who missed their medications disclosed to physician during consultation. The knowledge and practice of critical component of diabetes self management behavior were generally low among the patient studied.
Conclusion:
Majority of the patient with type 2 diabetes in Ethiopia are managed by OHA monotherapy mainly glybenclamide and metformine. While the current prescribing strategy do not achieve glycemic control on majority of the patient. This is due to poor adherence with the prescribed drug regimen and poor knowledge and practice of successful self management.
Keywords: Type 2 diabetes, oral hypoglycemic agent, self-management, Ethiopia
Introduction
Diabetes mellitus comprise of a group of common metabolic disorder that share the phenotype of hyperglycaemia. Type-2 DM is a heterogeneous group of disorders characterised by variable degree of insulin resistance, impaired insulin secretion and increased glucose production[1].
The risk of death from cardio vascular disease is approximately three fold for patient with type-2 diabetes; and the risk of death from all cases is increased by 75% compared to patient without diabetes[2].
Evidence abound that the most important predictor of reduction of morbidity and mortality due to diabetes complications is the level of glycemic control achieved[3–6]. This has encouraged aggressive treatment of patients with the goal of achieving blood glucose level as close to normal as possible. Indeed, there has been a shift from monotherapy with OHAs to combination therapy with at least two agents often from different classes, with or without insulin; in an attempt to achieve better glycemic control, reduce incidences of acute/long term complications and improve patient survival[5,7,8].
However, achievement of optimal glycemic control, which reduces the likelihood of diabetic complications and risk of death, is predicated on rational use of available anti-diabetic regimen, good adherence to prescribed treatments and successful self-management by patients[9,10].
Worldwide, adherence rate for medication for diabetes vary between 36 and 93%. Adherence to prescribed medication is crucial to reach metabolic control as non-adherence with blood glucose lowering or lipid lowering drug is associated with higher HbAIc and cholesterol, levels respectively. The study conducted in Netherland on refill adherence and poly pharmacy among patients with type-2 diabetes in general practice show that mean adherence with oral glucose lowering drugs is between 61 and 85%. According to this study it has become apparent an increase in the number of co-medications tends to decrease the adherence of patient with type-2 diabetes to their treatment regiments[11]. A study on the adherence to anti diabetic drug therapy and self management practice among type- 2 diabetics conducted in south western Nigeria showed that about two third of patients are not adherent[10]. Glycemic control was assessed in stable type -2 DM black South African patients. At the beginning of this study the overall meal HbAIc was 9.1+ 0.1%. The target value of HbAIc is < 7 were achieved in only 20% of patient[12]. Adherence to antidiabetic agents was found to be positively associated with a decrease in HbA1c[13,14]. For each 10% increase in adherence, HbA1c decreased significantly by 0.14 to 0.16%. Nonadherence to medications among diabetic patients resulted in poor glycaemic control and hence increased risk of developing chronic complications as well as increased hospitalization and mortality[15]. Accurate assessment of medication adherence is necessary for effective management of diabetes. However, there is no gold standard for such assessment although various methods have been reported in the literature[17,18].
Poor adherence to treatment of chronic disease is worldwide problem of striking magnitude. Recently, the world health organization stated that only 50% of patient diagnosed with chronic illness were fully compliant with their treatment regimen, in developing country the rate are even lower. It is undeniable that many patient experiences difficulty in following treatment recommendations[2].
The status of patient adherence to anti diabetic therapy and self management practice was not yet been known in Ethiopia. Therefore, the purpose of this study is to identify patient, medication and environmental factors associated with non adherence to ant diabetic drug and self management practice.
Patients and Methods
The study was approved by the Ethics Committee of Jimma University. Verbal consent was obtained from each patient before the interview. The confidentiality of the data obtained was assured and the name and address of the patient was omitted from the questioner.
Study Area and Study Period
The study was conducted in Jimma University Specialized Hospital. This is the only Specialized Hospital in Southwest Ethiopia with 450 beds. The study was conducted from January 21 to Mar 28, 2010.
Study Design
Two methodological approaches were adopted. The first phase was cross-sectional drug use study in Jimma University Specialized Hospital. Three hundred eighty four Case notes of patients with type-2 diabetes who attended the DM clinic Outpatient Department Jimma University Specialized Hospital were assessed.
This was done by randomly drawing every 5th case note out of chronologically arranged 1000 case notes of patients that attended the DM clinic over the 3 month study period.
Data were extracted from the case notes using two pre-tested data collection forms. The first instrument collected data such as patients’ card number, age, gender and co-existing diseases. The second form was a Drug Use Evaluation instrument which was used to collect drugs prescribed, dose and frequency, Side effects, Patients’ mean fasting plasma glucose reading as at the first and the last clinic visit and Glycosylated hemoglobin (HbAIc) tests conducted with dates.
Adequate glyceamic control was defined as patients that have fasting plasma glucose level between 90mg/dL – 100mg/dL. Combination therapy was defined as successive prescription of two or more ant diabetic drug prescribed.
The second phase was cross-sectional interview of consecutive type-2 diabetic patients who visit the DM clinic during the study period. The interviews were conducted with pre-tested adherence and self management monitoring tool. The interviews were conducted with a pretested Adherence and Self-Management Monitoring Tool on 25 patients. The adherence and self-management monitoring tool essentially focused on exploring patients’ experience with current anti-diabetic prescriptions and possible challenges being experienced and patients’ knowledge and practice of diabetes self management behaviors such as self blood glucose monitoring, optimal blood glucose target, complications from poor glycemic control, feature of hypoglycemia and use of daily medication reminder (DMR).
Statistics Analysis
The validity of the questionnaires was assessed through in-depth discussion with experienced pharmacist and internists working in College of Public Health and Medical Science of Jimma University. The collected data was cleared, categorized, and coded. All data collected were then analyzed using the Statistical Package for the Social Sciences (SPSS), version 16.0 software. Tests of proportions were done with Chi-Square, and a p-value of <0.05 was considered as statistically significant.
Results
Patient Case Note Review
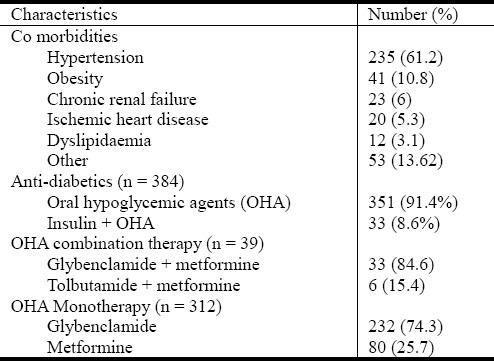
A total of 384 case notes of patient with type-2 diabetes were included. The majority 51.83% were males and 48.17% were females. The mean age was 48.3 year (SD =11.8). The most frequent co-morbidity was hypertension (61.2%) followed by obesity (10.8%), chronic renal failure (6%), coronary heart disease (5.3%), dyslipidaemia (3.1%), and other disease such as TB, anemia, osteoarthritis, asthma and hyperthyroidism with individual frequency of less than 3% all constituted 13.62% of the total co-morbid disease.
Oral hypoglycemic agent were prescribed for 351 (91.4%) of patients while insulin & OHA was prescribed in 33 (8.6%) of the patient. Of the patient on OHA, 312(88.9%) where on monotherapy while 39 (11.1%) where on combination therapy. The most frequently prescribed combination therapy contain giybenclamide and metformin 33 (84.6%) followed by tolbutamied & metformin 6(15.4%). Of the patient on mono therapy with OHA 232(74.3%) were on Glibneclamide followed by metformine 80 (25.7%). About 161 (41.9%) of the patient had adequate glycemic control. Glycosylated hemoglobin test was not employed for assessment and monitoring purpose. Fasting plasma glucose level was used frequently (Table 1).
Table 1.
Co-morbidities and Pattern of anti-diabetic drug prescribing among patients with type 2 diabetes in Southwest Ethiopia
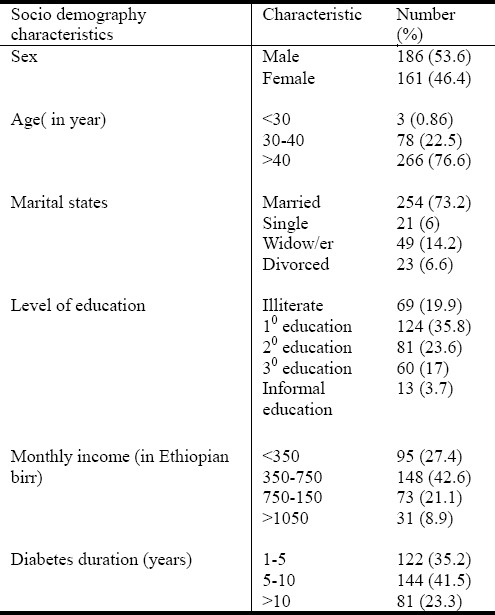
Patient Interview
Three hundred forty seven patients were involved in interview, among 384 patients who their records reviewed (response rate was 90.4%). The socio-demographic characteristics of the respondents are shown in Table 2.
Table 2.
Socio demography characteristic of type-2 diabetic patient who attended interview in JUSH diabetic clinic JAN, 2010
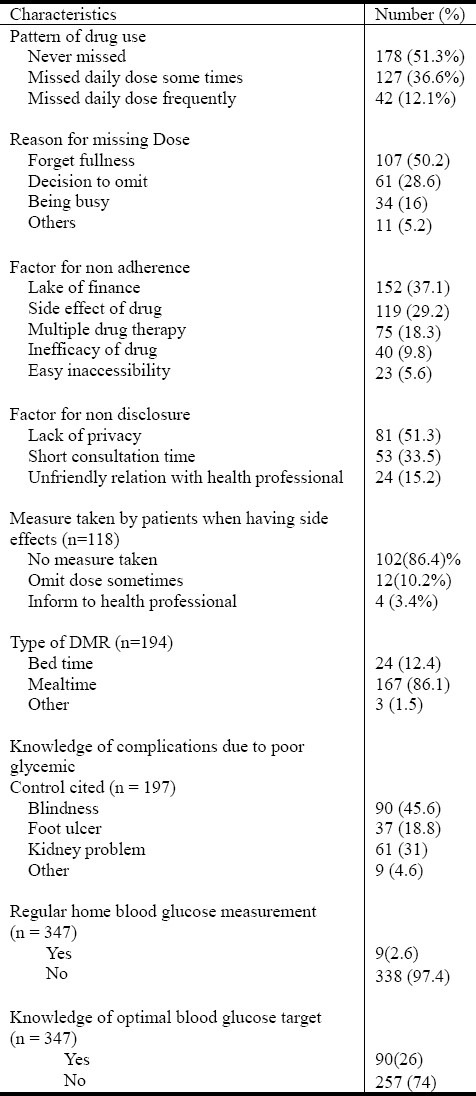
On the basis of self-report for their anti-diabetic drug adherence 72 (20.8 %) of the patients claimed that they had excellent tendency to take medication with the agreed recommendation from heath care provider, 98 (28.2%) very good, 117 (33.7%) good, and 60 (17.3%) said they had poor adherence. In self report for the pattern of drug use, 178 (51.3%) of patients said that they had never missed (neither daily dose nor time of taking) dose, 127 (36.6%) missed either daily dose or time of taking some times and 42 (12.1%) missed either dally dose or time of taking.
Among those who had missed their medication the most common reasons for missing medications were forget fullness 107 (50.2%), being busy 34 (16%), others including side effects of drugs, disappearance of the symptoms and perceived inefficacy of the prescribed anti diabetic drugs and others 72 (33.8%).
The factors identified by patients as underpinning non-adherence were lack of finance 152 (37.1%), side effect of the drugs 119 (29.2%), multiple drug therapy 75 (18.3%), perceived inefficacy of prescribed anti diabetic drugs leading to concomitant self medication with traditional medicine 40 (9.8%) and easily inaccessibility of drugs 23 (5.6%).
Only 11(6.5%) of the patients among those who missed their medication frequently and sometimes, claimed to have disclosed this to physicians during consultation. The frequently identified factors for non-disclosure were, lack of privacy 81 (51.1%) due to patient overcrowding and sharing of consulting rooms by physicians, short consultation time leading to short physicians patient contact 53 (33.5%), and unfriendly relation with physicians 24 (15.2%).
118(34.1%) of patients had an information about the side effects of drugs of the patient asked on measures they had taken to avoid the side effects, 102 (86.4)% respond that they did nothing, 12 (10.2%) omit dose sometimes and only 4 (3.4%) of them inform to health professional.
9 (2.6%) of patients regularly measure their blood glucose level at home. One hundred ninety four (56%) of patients use at least a daily medication reminder (DMR) to remind them to take their prescribed anti diabetic medication and of these, 62% were adherent while 38% were non-adherent. The use of DMR and not missing dose has significant association p < 0.002. The most commonly used DMR were mealtime (86.65%), bed time (12.63%) and other such as using alarm clock (1.72%). Only 90 (26%) of the patients could correctly state the desired blood glucose target: knowledge of the desired blood glucose target was significantly better among patients who were claimed to have excellent and very good adherence 170 (48.9%) with the prescribed anti diabetic drugs (P < 0.003). 122 (35.1%) of patients had knowledge of possible complication that could arise from poor control of blood glucose level. It was significantly better among patient who were never missed 178 (51.3%) their anti diabetic medication (P < 0.001). The possible complication cited includes blindness 90 (45.6%), kidney problem 61 (31%), foot ulcer 37(18.8) and other 4 % (Table 3).
Table 3.
Determinants of non-adherence with drug therapy and profile of self-management practices among type 2 diabetic patients
Discussion
Presently, there is no single measure accepted as the gold standard to measure medication adherence. Because all commonly employed methods has drawbacks. Patient interviews while straight forward and inexpensive are clearly limiter by their subjective nature. Pill counts are frequently utilized, inexpensive, and can proved information about the number of pills taken. However, it is difficult to determine actual medication consumption, and patients can intentionally or unintentionally manipulate this measure. Medication refill records provide unobtrusive information regarding refills histories and can be valuable in determining gaps in therapy but this method, similar to pill counts and electronic monitors indirect and cannot confirm actual medication consumption[19].
Hypertension (61.2%) and obesity (10.8%) as the most frequent co-morbidities among the patients studied. It is consistent with the established theory of metabolic syndrome, which is strongly associated with cerebrovascular disease in type- 2 diabetes[20,21]. This is in agreement with several studies[22]. The majority of the patients were on mono therapy mainly with either glibenclamide (74.3%) or metformin (25.7%) which is not consistent with recommended intensive control of blood glucose level[8,23]. Study in south Nigeria show that 70.3% of the patients were on combination therapy and it was reflected the necessity of intensive control of blood glucose level[10].
The study showed that only 41.8% of the patients had adequate glycemic control and it is consistent with other studies[10] who reported adequate glycemic control in 43.8% of type -2 diabetic patients. HbA1c test was not used to monitor or assess glycemic control in any of the patient, only FPG level is used to assess and monitor glycemic control. However, HbAIc is the established gold standard. The American diabetes association position statements with the standard of diabetic care recommend that, in patient with glycemic control, at least two HbA1c test be done per year, While in patients with poor glycemic control HbA1c test should be done quarterly per year[24] and this study finding suggest that monitoring of glycemic control in study site should be improved. Our findings, therefore, suggest that monitoring of glycemic control among Southwest Ethiopian diabetics may be less than optimal and this may be a probable contributory factor to late detection of patients at risk of complications and death from poorly controlled type-2 diabetes.
The knowledge and practice of basic components of diabetes self management practices were generally low among the patient studied. However, it was significantly higher among patients who were never missed their medication and those that have excellent and very good adherence to their prescribed anti diabetic medications. These findings indeed underscore the critical role played by patient awareness and practice of diabetes self management behaviors in improving adherence to drug therapy, ensuring achievement of adequate glycemic control and minimizing the likelihood of diabetic complication[25,26].
Adherence to prescribed anti diabetic medications is crucial to reach metabolic control as non adherence with blood glucose lowering or lipid lowering drugs is associated with higher HbA1c and cholesterol levels respect lively[13]. This study revealed that adherence to anti diabetic medication in type-2 diabetic patient is problematic, only 51.3% of the patients were never missed their daily medication and (20.8% and 28.2%) of the patient have excellent and very good adherence respectively which is similar with several study[7,10,12,23,27].
In this study the main external challenge of adherence is financial problem (37.1%). Ethiopia is a resource limited setting were the majority of the people estimated to live below poverty levels: so the economic access to anti diabetic medication appeared restricted by the average monthly cost of 32.7 birr ($2.0). Yet this does not include the cost of other adjunctive therapy such as anti hypertensive drugs required by the majority of the patient. This is in agreement with study done in Nigeria in which around 2/3 of the non-adherence is due to financial difficulty. According to this study the average monthly cost of anti diabetic drug was $ 22.9[10] which is much expensive as compared to this one, because in Ethiopia cost of medication is subsidized by government for some patient. The adoption of viable cost reduction strategies such as the pooled procurement, encouraging prescribing of low price but good quality generic anti diabetic drugs and strengthening of provision of subsiding by government and its collaborating with donor agencies may increase patient access to the needed ant diabetic medications which improve the adherence.
In this study, only 6.5% of the patients that missed their medication claimed to have disclosed this to health care provider during consultation. The main factor cited for non disclosure were, short consultation time & lack of privacy resulting in inadequate physician-patient interaction during consultations. This may arise due to shortage of health professional, high patient workload and poor work environment in Ethiopia.
About 56% of patients use DMR to remind them to take their prescribed medication. Meal time and bed time were the most frequently DMR used. This finding shows the patients personal dally routine plays a great role in maximizing adherence to prescribed medications. Therefore, careful identification of patient-specific routine, it use in planning patient medication regiment by physicians during prescribing and counseling during dispensing by pharmacists should be the part of the diabetes care process. These likely to increase the chance of achieving high patient adherence with prescribed medications and subsequent optimal glycemic control.
Generally, the fact that self management practices were generally low among the patient studied indicates the need of educational empowerments is critical if successful self management is to be achieved. This could be done with the use of a number of motivational strategies such as a scheduled home visits by designated health extension worker to evaluate and strengthen adherence with medications and self-management practices, peer-education and experiences through patient support groups; and confidential counseling by health professionals with each focusing on specific issues pertaining to their contributions to the diabetes care process.
Conclusion
The study have shown that majority of the patients with type 2 diabetes in Southwest Ethiopia are managed with OHA monotherapy. While the current prescribing strategy achieved glycemic control for less than half of the patients, majority are still not meeting the recommended blood glucose target. This appears mainly due to poor adherence with prescribed drug regimen and poor knowledge and practice of self management behaviors. There is a need for regular appraisal of drug prescribing and better monitoring of patient adherence with prescribed anti diabetic drugs and other diabetes self management practices. Training in learning processes and factors governing behavior are essential for all of those involved in delivery of patient care. Educational program should recognize the wide range of learning strategies used by different peoples. The prescriber before prescribing and pharmacist before dispensing drugs for diabetic patients, he/she should negotiate about the treatment plan that the patient understands and to which he or she commits.
Acknowledgments
This study was financed by Students Research Project (SRP) of Jimma University. The authors are grateful to patients, who participated in the study, for their time to participate in the study. Special thanks are due for research staff participated in data collection and write up. N. T. Wabe is principal investigator and participated in conception, patient identification, and design of the study. M.T. Angamo carried out the sequence alignment and drafted the manuscript. Sadikalmahdi Hussein carried out the analysis and interpretation of data. All authors read and approved the final manuscript.
References
- 1.Ramphal R. Endocronolgy and Methabolism. In: Fauci AS, Braunwald E, Kasper DL, editors. Harrison Principles of Internal Medicine. 17th ed. New York, NY: McGraw Hill Medical; 2008. pp. 949–956. [Google Scholar]
- 2.World Health Organization, diabetes mellitus fact sheet, number 238, 2002. [Accessed August 13, 2006]. at http://www.who.int/diabetes .
- 3.American Diabetes Association. Implications of the United Kingdom Prospective Diabetes Study. Diabetes Care. 1999;22:27–31. [PubMed] [Google Scholar]
- 4.Diabetes Control and Complications Trial Research Group. Lifetime benefits and costs of intensive therapy as practiced in the diabetes control and complications trial. JAMA. 1996;276:1409–1415. [PubMed] [Google Scholar]
- 5.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformine on complications in overweight patients with type 2 diabetes (UKPDS 34) Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 7.Cohen FJ, Conklin JE, Neslusan CA, Song X. Recent antihyperglyceamic prescribing trends for US privately insured patients with type 2 diabetes. Diabetes Care. 2003;26(6):1847–1851. doi: 10.2337/diacare.26.6.1847. [DOI] [PubMed] [Google Scholar]
- 8.Turner RC, Cull CA, Fright V, Holman RR for the UK Prospective Diabetes Study (UKPDS) Group. Glycemic control with diet, sulfonylurea, metformin or insulin in patients with type 2 diabetes mellitus: progressive requirement for multiple therapies. JAMA. 1999;281:2005–2012. doi: 10.1001/jama.281.21.2005. [DOI] [PubMed] [Google Scholar]
- 9.Defronzo RA. Pharmacologic therapy for type 2 diabetes mellitus. Ann Intern Med. 1999;131:281–303. doi: 10.7326/0003-4819-131-4-199908170-00008. [DOI] [PubMed] [Google Scholar]
- 10.Yusuff KB, Obe O, Joseph BY. Adherence to anti diabetic drug therapy and self management practices among type-2 diabetics in Nigeria. Pharm World Scl. 2008;30:876–883. doi: 10.1007/s11096-008-9243-2. [DOI] [PubMed] [Google Scholar]
- 11.Kingh, Aubert Re, Herman W. Global burden of diabetes from 1995-2005. Diabetes Care. 1998;21:1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 12.Erasmus RT, Blanco B, Okesina AB, Gqweta Z, Matsha T. Assessment of glycemic control in stable type 2 black South African diabetics attending a peri-urban clinic. Postgrad Med J. 1999;75:603–606. doi: 10.1136/pgmj.75.888.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pladevall M, Williams LK, Potts LA, Divine G, Xi H, Lafata JE. Clinical outcomes and adherence to medications measured by claims data in patients with diabetes. Diabetes Care. 2004;27:2800–2805. doi: 10.2337/diacare.27.12.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schectman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an Indigent population. Diabetes Care. 2002;25:1015–1021. doi: 10.2337/diacare.25.6.1015. [DOI] [PubMed] [Google Scholar]
- 15.Kuo YF, Raji MA, Markides KS, Ray LA, Espino DV, Goodwin JS. Inconsistent use of diabetes medications, diabetes complications, and mortality in older Mexican American over a 7-year period. Diabetes Care. 2003;26:3054–3060. doi: 10.2337/diacare.26.11.3054. [DOI] [PubMed] [Google Scholar]
- 16.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–530. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 17.Donnan PT, MacDonald TM, Morris AD. Adherence to prescribed oral hypoglycemic medication in a population of patients with type 2 diabetes: a retrospective cohort study. Diabet Med. 2002;19:279–284. doi: 10.1046/j.1464-5491.2002.00689.x. [DOI] [PubMed] [Google Scholar]
- 18.Hernshaw H, Lindenmeyer A. What do we mean by adherence to treatment and advice for living with diabetes? A review of the literature on definitions and measurements. Diabet Med. 2006;23:720–728. doi: 10.1111/j.1464-5491.2005.01783.x. [DOI] [PubMed] [Google Scholar]
- 19.Vanbruggen R, Gorter K, Stolk RP. Refill adherence and poly pharmacy among patients with type 2 diabetes in general practice. Pharmacoepidemiol Drug Saf. 2009;18:983–991. doi: 10.1002/pds.1810. [DOI] [PubMed] [Google Scholar]
- 20.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among US adults. Diabetes Care. 2004;27:2444–2449. doi: 10.2337/diacare.27.10.2444. [DOI] [PubMed] [Google Scholar]
- 21.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 22.Sullivan PW, Morrato EH, Ghushehyan V, et al. Obesity, inactivity and the prevalence of diabetes and diabetes-related cardiovascular co morbidities in the US, 2000–2002. Diabetes Care. 2005;28:1599–1603. doi: 10.2337/diacare.28.7.1599. [DOI] [PubMed] [Google Scholar]
- 23.Chuang LM, Tsai ST, Huang BY, Tai TY. Diabcare-Asia 1998 Study Group.The status of diabetes control in Asia- a cross-sectional survey of 24,317 patients with diabetes mellitus in 1998. Diabetes Med. 2002;19:978–985. doi: 10.1046/j.1464-5491.2002.00833.x. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association (ADA). Standard of medical care in diabetes. Diabetes Care. 2005;28:10–20. [Google Scholar]
- 25.Glasgow RE, Strycker LA, Hampson SE, Ruggiero L. Personal model beliefs and social-environmental barriers related to diabetes self-management. Diabetes Care. 1997;20:556–561. doi: 10.2337/diacare.20.4.556. [DOI] [PubMed] [Google Scholar]
- 26.Day JL. Diabetic patients’ education: determinants of success. Diabetes Metab Res Rev. 2000;16(Supl 1):S70–S74. doi: 10.1002/1520-7560(200009/10)16:1+<::aid-dmrr110>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 27.Kolawole BA, Adegbenro C, Ayoola ZO, Opebiyi B. Diabetes mellitus related treatment goals: awareness and attainment in the Ife-Ijesha zone of south-western Nigeria. Afr J Med Sci. 2005;34(4):389–394. [PubMed] [Google Scholar]


