Abstract
Background:
The current rise of male infertility associated with bacterospermia and urogenital infection has been on the increase amongst adult married males in Benin metropolis and a major cause of concern to male fertility and reproduction in Nigeria.
Aim:
To microbiologically isolate and study the infectious agent that has led to male infertility and also to study the percentage occurrence of bacteropsermia and urogenital caused infertility in adult married males in Benin metropolis
Material and Method:
using standard microbiological methods of isolating and identifying the organism, specimen was collected and processed which includes the susceptibility profile of isolates and sperm quality. In this study a total of 140 sperm samples was collected from patient who were referred from the consultant outpatient department of the University of Benin Teaching Hospital and then evaluated bacteriologically using standard bacterial cultural methods
Results:
Among the total cases, 92 (65.7%) showed at least one pathogen. Staphylococcus aureus (28.3%), Staphylococcus Saprophyticus (13.0%), Pseudomonas aerouginosa (6.5%), Escherichia Coli (19.6%) Proteus mirabilis (10.8%) Klebsiella spp (10.8%) and Proteus vulgaris (10.8%).
Conclusion:
There was an outstanding significant relationship between bacteriospermia and the rate of total motility and morphologically abnormal sperms, The percentage of morphologically normal sperm was lower in this study. Staphylococcus aureus Staphylococcus saprohyticus and Escherichia coli were the most common pathogen having negative effects on sperm motility and morphology in this study.
Keywords: Bacterospermia, sperm quality, Infertility, urogenital
Introduction
Male urogenital tract infections is one of the most important causes of bacterospermia and male infertility worldwide. Genital tract infection and inflammation have been associated to 8-35% of male infertility cases[1,7,8]. Asymptomatic bacteriospermia may play a major role[2,9]. Male accessory sex glands infection is a major risk factor in infertility[5].
The significant of pathophysiology of bacteriospermia has been discussed in recent years. Some possible pathomechanisms of the development of infertility linked with infection are considered: direct effect on sperm function (motility, morphology, etc), deterioration of spermatogenesis, auto-immune processes induced by inflammation and dysfunction of accessory sex glands[2,8]. Hence, microbiology investigation of male partners in infertile couple can be useful to detect the male urogenital tract infection, especially asymptomatic infections.
The aim of this study was to investigate microbiology semen samples of infertile men.
Patients and Methods
Semen sample of 140 infertile men attending the infertility Consultant out-patient Department of the University of Benin Teaching Hospital were collected by masturbation, after a 3 days abstinence period. Patients should not have taken any antibiotic one week before collection of semen sample. Before collection, parents were advised to wash their hands and genital area with soap and water. Samples were collected into sterile universal containers.
All specimen collected were rapidly transferred to Microbiology Laboratory and processed according to the method of Cheesbrough 1984. Culture was incubated at 37 °C for 24-48 h. Semens were prepared on each sample on a slide and stained with gram staining techniques. All emergent colonies from culture were identified according to the criteria of Cowan and Steel 1985. Standard analysis of semen parameters was performed according to WHO, guidelines[10]. Nigrosin-Eosin Staining Technique and Sodium Bicabonate formalin fluid diluted 1/20 were used for the enumeration of sperm cells morphology and sperm count respectively. Control semen from fertile male patient was also treated according to the WHO guidelines on semen examination and evaluation.
Results
Out of a total number of 140 specimen processed, 92 (65.7%) yielded bacterial growth with Staphylococcus aureus, S. saprophyticus and Escherichia coli having the highest incidence rate of 28.3%, 19.6% and 13.0%, respectively. Trailing behind these were Proteus mirablis 10.8%, Klebsiella pneumonia 10.8% and Proteus vulgaris recorded 10.8% each respectively. Pseudomona aeruginosa had .5% (Table 1).
Table 1.
Bacterial isolates: morphology and sperm motility
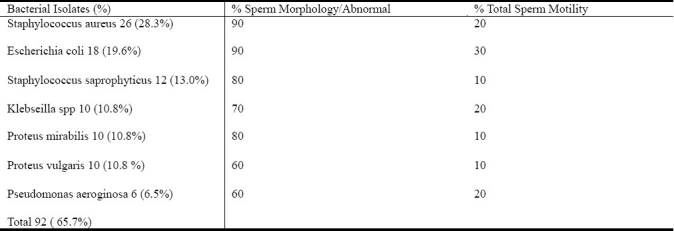
Using Chi-square statistical analysis, there was a relationship between Bateroispermia and Quality from these male infertile patients (Table 1), the susceptibility profiles of these organism to the various antibiotics showed a remarkable drug resistant pattern which may be a cause of reoccurent drug resistant bacteriospermia.
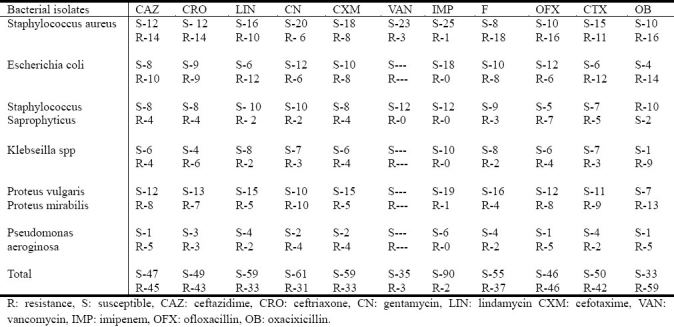
The was a total of 97% susceptibility to Imipenem and Staphylococus aureus and Staphylococcus saprophyticus had a 92% susceptibility to Vancomycin and 7.8% resistance to vancomycin, there is the increase in the resistance of Imipenem with 2.1% occurrence this is shown in (Table 2).
Table 2.
Bacterial susceptibility profile
Discussion
In this study 92 (65.7%) out of a total number of 140 semen samples from infertile males collected yielded bacterial growth. In Table 1, Staphylococcus aureus (28.3%), S. saprophyticus (13.0%) and Escherichia coli (19.6%) were the main organisms with the most negative influence on sperm motility and morphology.[6,7,11,12]. There was a definite relationship between Bacteriospermia (Bacterial Isolates), Leucocytes (Puscells) and Total sperm count (P< 0.001). The immobilization effect of certain bacteria particularly Escherichia coli had been reported[7]. The rate of non-motile sperm cells and abnormal morphology was also established through WHO 1999 evaluation techniques and was found to be affected by these bacterial isolates. The antimicrobial susceptibility profile showed that most of the organism are becoming drug resistance and also the increasing resistance to Vancomycin and Imipenem. Generally the risk of infertility increases by age but most of our investigated patients were young. The idea that bacterial infection may be partly responsible for male infertility arises from the clinical observation of the patients’ male reproductive system. Male urogenital tract infection is are one of the most important causes of male infertility worldwide[1,2,7]. Infection processes may lead to deterioration of spermatogenesis, impairment of sperm functions, and obstruction of the seminal tract[8]. In-view of the above, there is the need to institute a Microbiological intervention to detect the probable microbial agents. It should be noted that presence of urogenital tract infection and inflammation poses a danger to the fertility profile of male patient and should be eradicated by the use of appropriate prescribed antibiotics and anti-inflammatory treatment. Therefore, because of the important role of bacteriospermia in male infertility, more attention should be attached to young sexually active men health in this study.
Acknowledgments
Thanks to the patience and the National Academy for the Advancement of Science for the financial assistant and grants given.
References
- 1.Elnhar A. Male genital tract infection: the point of view of the bacteriologist. Gynecol Obstetrique Fertili. 2005;33(9):691–697. doi: 10.1016/j.gyobfe.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 2.Bukharin OV, Kuzmin MD, Ivanov IB. The role of the microbial factor in the pathogenesis of male infertility. Zhurnal Microbiologii Epidemiologii I Immunobiologii. 2003;(2):106–110. [PubMed] [Google Scholar]
- 3.Cheesbrough M. Microbiology. 2nd ed. II. Cambridge: University Press; 1984. Medical Laboratory Manual for Tropical Countries; pp. 100–196. [Google Scholar]
- 4.Cowan ST, Steel KJ. Manual for the Identification of Medical Bacteria. 4th ed. London: Cambridge University Press; 1985. p. 217. [Google Scholar]
- 5.Diemer T, Ludwig M, Huwe P, Haler DB, Weidner W. Influence of genital urogenital infection on sperm function. Curr Opin Urol. 2000;1(1):39–44. doi: 10.1097/00042307-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Esfandiari N, Saleh RA, Abdoos M, Ruozrokh A, Nazemian Z. Positive bacterial culture of semen from infertile men with asymptomatic leukocytosspermia. International J Fertil Wom Med. 2002;47(6):265–270. [PubMed] [Google Scholar]
- 7.Ibadin OK, Ibeh IN. Bacteriospermia and sperm quality in infertile male patient at University of Benin Teaching Hospital, Benin City, Nigeria. Mala J Microbiol. 2008;4(2):65–67. [Google Scholar]
- 8.Keck C, Gerber–Schafer C, Clad A, Wihelm C, Breckwoldf M. Seminal tract infections: impact on male fertility and treatment options. Hum Reproduct Updat. 1998;4(6):891–903. doi: 10.1093/humupd/4.6.891. [DOI] [PubMed] [Google Scholar]
- 9.Li H Y, Lui JH. Influence of male genital bacteria infection on sperm function. Zhonghoa Nan Ke Xue. 2002;8(6A):442–444. [PubMed] [Google Scholar]
- 10.Rebenstein J. Infertility, male. Sanfracisco, USA: University of california; 2005. [Google Scholar]
- 11.Rodin DM, Larone D, Goldstein M. Relationship between semen cultures, leukospermia, and semen analysis in men undergoing Fertility evaluation. Fertilsteril. 2003;3:1555–1558. doi: 10.1016/s0015-0282(03)00340-6. [DOI] [PubMed] [Google Scholar]
- 12.Sanack-Maciejewska D, Ciupinska M, Kurpisz M. Bacterial infection and semen quality. J Reproduct Immunol. 2005;18 doi: 10.1016/j.jri.2005.06.003. [Epubahead of print] [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO) Laboratory manual for the examination of human semen and sperm – cervical mucus interaction. 4th ed. Cambridge, UK: Cambridge University Inc; 1999. World Health Organization (WHO) pp. 1–138. [Google Scholar]


