Abstract
Background:
Lumbar segmental stability is an important biomechanical component that influences symptoms amongst patients with Mechanical low back pain.
Aims:
To compare the efficacy of segmental stabilization exercises utilizing multifidus and transversus abdominis muscles versus a placebo treatment in patients with lumbar segmental instability.
Materials and methods:
The study was an observer-blinded randomized placebo-controlled cross-over study of 18 adults (12 men, 6 women), of mean age 22.5 ± 1.09 yrs who scored 7/13 in subjective aspects and 8/14 in objective aspects of Delphi criteria for lumbar segmental instability. The selected subjects were then randomized to receive either placebo-control (prone lying) or experimental (lumbar segmental stabilization) as a first treatment. Each treatment was followed by a wash-out period of 24 hours. Outcomes were measured four times- pre- and post- first intervention, pre- and post- second intervention. The outcome measures used were pain on Visual analogue scale, Pressure pain threshold and Joint play grading scale (0-6 scale) on that level.
Results:
Two-way analysis of variance and post-hoc analysis using Bonferonni test were used with level of significance set at p<.05 using Statistical package for social sciences version 12.0.1 for Windows. Visual analogue scale changed significantly in both the periods of intervention- in control (P =.016) and experimental (P =.000) periods. However this improvement was more significant in the experimental period. The Joint play grading scale scores improved only in the experimental condition compared to the control condition significantly. The Pressure pain threshold also improved significantly in the experimental condition (P =.000) while the changes in control condition was not statistically significant (P=.816).
Conclusion:
Segmental stabilization exercise was more effective than placebo intervention in symptomatic lumbar segmental instability.
Keywords: Lumbar instability, segmental stabilization exercise, crossover study
Introduction
Low back pain remains to be the single most common reason for a visit to a general practitioner and is also the greatest cause for work- related disability. Low back pain from mechanical origin is identified by the presence or absence of symptoms and signs with different postures or movements. Mechanical low back pain is commonly treated conservatively with physical therapy. Poor or delayed response to conservative treatment will indicate surgery. Surgery too, has its own poor outcomes. Hence proper management must ensue once the diagnosis of mechanical low back pain is made clinically[1].
Lack of clear definition or diagnostic criteria posed a new category of non- specific low back pain which might be the subtype which is the greatest in the group of chronic low back pain patients. Thorough subjective and objective examination is thus indicated to accurately identify the sub population who would not show a general predictable response to therapy so that they could then be evaluated further for providing suitable management[2].
Assessment of segmental motion is inherent in any spinal examination to localize the level of involvement and to precisely target that affected level with suitable manual techniques. Segmental motion analysis is done clinically using the central PA pressure where the examiner applies pressure vertically over the spinous processes of the vertebrae. Symptom reproduction which correlates to the subjective complaints is considered as an important comparable sign. The examiner then detects the passive accessory mobility and compares across levels to diagnose abnormal mobility at that level. The validity of central PA pressure increases when it is correlated to the subjective perception of pain intensity during the assessment than objective sensation of resistance to the accessory examination[3].
Segmental vertebral motion analysis done using central postero-anterior pressure would show normal, decreased or excessive mobility depending on the structural involvement. This available joint play is then graded using the seven point grading scale termed the Joint Play Grading Scale initially introduced by Stanley Paris. The scale has seven categories (0, ankylosed; 1, considerable hypomobility; 2, mild hypomobility; 3, normal mobility; 4, mild hypermobility; 5, considerable hypermobility; and 6, unstable)[3].
The passive tissues supporting the spine resist the postero anterior forces applied by the operator with a property termed the postero anterior stiffness. Reduced stiffness may be indicative of segmental instability whereas increased stiffness may be suggestive of segmental hypomobility[4]. Whereas hypomobility or dysfunctions of the lumbar spine are often treated with manual vertebral mobilization, the effects of manual mobilization are however limited in segmental instability. Application of manual techniques to the involved level of segmental instability would necessarily potentiate complications and adverse therapeutic effects[5].
Assessment of pressure pain thresholds is a valid and reliable clinical tool to evaluate the subjective perception of pain in response to application of pressure. Pressure algometry is used in manual therapy to objectively quantify the pressure pain thresholds and it was shown that a predictable variation exists across various spinal levels from cervical to lumbar levels[6]. Objectivity of central postero anterior pressure assessment on lumbar spine would thus be improved if assessment is correlated with the spinal pressure pain thresholds.
Management of lumbar segmental instability would be based on clinical and radiological findings after characterizing it into clinical or mechanical instability[7,8]. While mechanical instability (mostly resulting from macrotrauma) indicated surgery or lumbar supports as treatment, clinical instability (resulting from microtrauma) was managed with motor control retraining and re-education programs involving postural control retraining, segmental stabilization exercise using transversus abdominis and multifidus co-activation[9–15].
Treatment of lumbar segmental instability focuses mainly on active subsystem stabilizing the spine, namely the global muscles- the transversus abdominis and local muscles- the multifidus. Though core stabilization using transversus abdominis strengthening is an inherent part of a comprehensive rehabilitation program for lumbar segmental instability, local multifidus strengthening using pressure biofeedback units also has been shown to be effective[15], but there was a paucity in the existing clinical scenario whether a program of segmental stabilization using multifidus strengthening would then be sufficient to improve stability in segmental instability subjects.
Hence the current study was aimed to study the immediate and short term effects of multifidus strengthening at the involved level in subjects with segmental instability of the lumbar spine as compared to a placebo intervention. It was hypothesized that spinal segmental stabilization exercise would be better than placebo intervention in mechanical low back pain patients identified to have segmental instability.
Materials and Methods
The study protocol was approved by the Institutional ethics committee of Kasturba Medical College, Manipal University, Mangalore. All participants were required to provide a written informed consent prior to their screening and participation in the study. The study was thus an open-labeled one.
Study Design
Observer-blinded randomized placebo-controlled crossover clinical trial. Out-patient treatment setting in a multispecialty university-affiliated teaching hospital. Study location was at the Dept of Physiotherapy Kasturba Medical College, Manipal University, Mangalore.
Sampling
Convenient sampling.
Subjects
Out-patients referred by a physician to the physical therapy department in Kasturba Medical College Hospital, Mangalore, for conservative treatment of leg pain and/or low back pain or discomfort.
Participant selection
The participants were selected based upon the criteria: Clinical diagnosis of segmental instability[9] for those who had localized midline pain in the low back and tenderness on palpation, painful arc during spinal movements, pain on jerky movements, positive prone segmental instability test, positive H-I instability test, hypermobility detected on passive accessory intervertebral testing using central postero-anterior pressure on that lumbar spinal level. Subjects with previous history of low back pain were also included and subjects with cognitive deficits were excluded. The diagnosis was confirmed by the tester using the Delphi checklist[16] provided in the appendix-I and only subjects who scored 7/13 in subjective aspects and 8/14 in objective aspects were included. This criterion was adapted from the earlier Delphi study findings and was validated and was found to be reliable predictors of spinal segmental instability. Patients who did not understand the instructions and who were unable to co-operate due to any other medical conditions were excluded.
Appendix I.
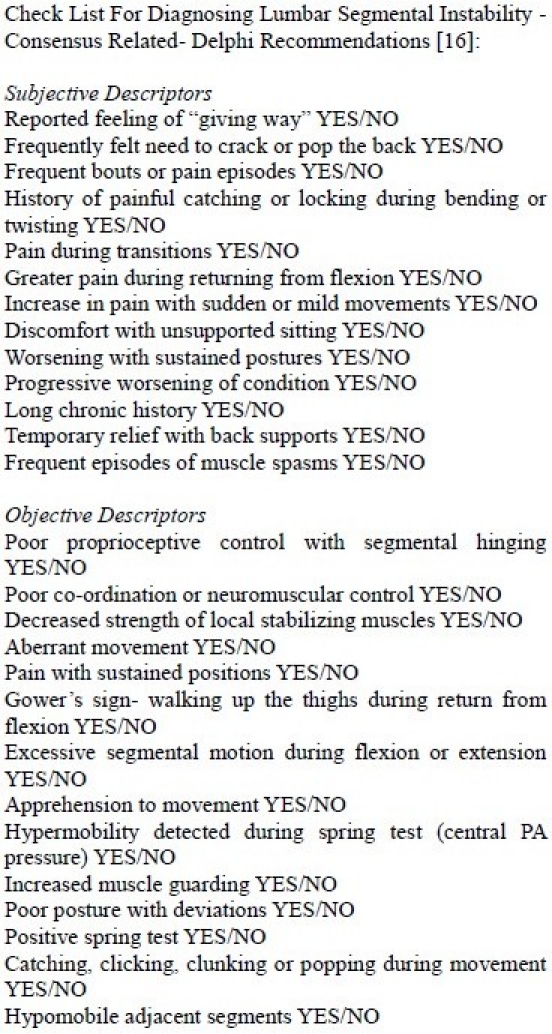
Testing Instruments
The following tools were used to measure the study's three outcome measures: A 10cm Visual Analogue Scale for assessing the intensity of perceived pain- The scale had 0-no pain and 10- maximum pain at either ends. The patient was asked to point out his pain where he felt would take its position in the scale. The scale was calibrated behind this side, where the rater noted down the values of pain. The lumbar spinal levels were chosen with reference to standard surface landmarks (Figures 1a, 1b). A Pressure Algometer (Mitutoyo® Corporation, Japan) for assessing the pressure pain threshold in pounds (lbs) at the affected lumbar spinal level (Figure 2). A Joint Play Grading Scale for assessing the segmental mobility of lumbar spine.
Fig. 1.
(a): Identification of L4 level from highest point of iliac crest; (b): Identification of L2 level from lowest margin of thoracic cage.
Fig. 2.

Assessment of spinal pressure-pain thresholds of the lumbar spine using the pressure algometer.
The scale had seven items 0-6: 0, Ankylosed; 1, Considerable hypomobility; 2, Mild hypomobility; 3, Normal mobility; 4, Mild hypermobility; 5, Considerable hypermobility; and 6, Unstable.
This scale was originally put forth by Stanley Paris, it was found to be a reliable and a valid tool for joint play assessments in clinical settings. Since it had a very high intra-rater reliability than the inter-rater, the scale was shown to be more useful for detecting prognosis in treatment when assessed by the same examiner.
The therapist applied a central postero-anterior pressure on lumbar spinal processes to evaluate the mobility and pain response in the lumbar spine. The grades of joint mobility were taken with relaxed spinal muscles versus spinal muscle contraction (Figures 3a, 3b).
Fig. 3.
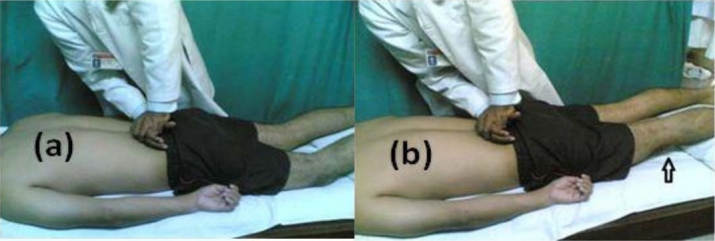
(a): Application of central postero-anterior pressure and assessment of joint play (without spinal muscle contraction); (b): Application of central postero-anterior pressure and assessment of joint play (with spinal muscle contraction- note the lifted knees indicated by an arrow).
Procedure
The subject was randomly allocated to either of the two study conditions.
Placebo Intervention
It consisted of maintaining a position of prone lying (directed by patient comfort pillows placed under abdomen if patient could not tolerate the neutral prone position) with pillow under the legs for 15 minutes under tester's supervision.
Segmental Stabilization Exercises
It was administered as per standard described procedure of Richardson and Jull[10]. The subject was asked to assume quadruped position. The tester assessed the neutral position of the lumbar spine by manually guiding the spine through full arc of flexion and extension. The subject was then instructed to tuck in the chin and hollow the abdomen with a posterior pelvic tilt. This would activate deep cervical short flexors and transversus abdominis, respectively. Then the subject was asked to slowly lift one arm while maintaining the earlier neutral spinal position when the tester palpated for the activation of multifidus at the tested level just medial to the facet joints on both sides simultaneously. Tester gave instructions to avoid substitution by the long extensor muscles. The steps were then repeated with lifting other arm. Ten repetitions were given for each side. Total treatment duration was 15 minutes (Figure 4).
Fig. 4.
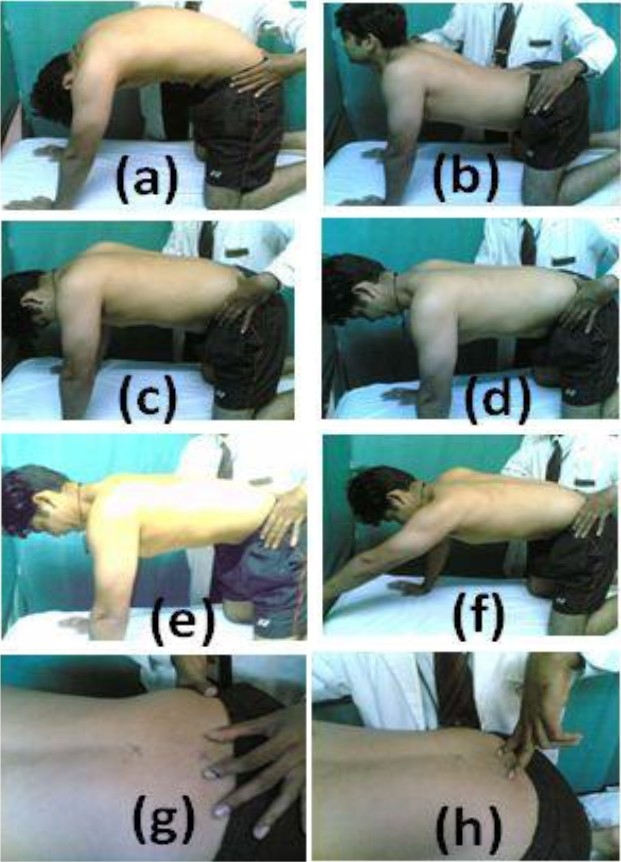
(a): Flexion of lumbar spine; (b): Extension of lumbar spine; (c): Neutral position of the lumbar spine; (d): Tucking in the chin to activate the deep cervical short flexors; (e): Hollowing the abdomen with tucked in chin to activate transversus abdominis; (f): Lifting one arm up with maintaining the neutral position; (g): Therapist's hand placement for palpating the contraction of multifidi; and (h): Application of quick stretch to facilitate the contraction of multifidi.
Data Collection
The three outcomes were taken four times, first- pre-first treatment; second- post-first treatment; third- pre-second treatment; and, fourth- post-second treatment by an independent blinded observer.
Data Analysis
The outcome measures (pre and post variables were taken as dependent variables) and hence were analyzed using two-way analysis of variance and post-hoc analysis using Bonferonni test at 95% confidence interval, using Statistical package for social sciences version 12.0.1 for Windows software.
Results
Of the 66 patients with low back pain contacted between July and September 2006, 62 consented and of them, 18 had lumbar segmental instability. The study population thus had 18 adults (12 men, 6 women), of mean age 22.5 ± 1.09yrs.
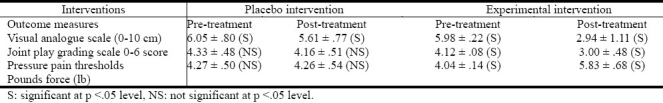
Visual analogue scale scores changed significantly in both the periods of intervention- in placebo group from 6.05 ±.80 to 5.61 ±.77 (P =.016) and experimental from 5.98 ±.22 to 2.94 ±1.11 (P =.000) periods. However this improvement was more significant in the experimental period (Table 1). The joint play scores improved in the experimental condition from 4.12 ±.08 to 3.00 ±.48 (p=.000) compared to the placebo condition from 4.33 ±.48 to 4.16 ±.51 (P =.25). The difference was significantly (P =.000) greater for the experimental intervention. The pressure pain thresholds also improved significantly in the experimental condition from 4.04 ± .14 to 5.83 ± .68 pounds-force (P =.000) while the changes in placebo condition from 4.27 ±.50 to 4.26 ±.54 pounds-force was not statistically significant (P =.816).
Table 1.
Between-group comparison of the three outcome measures in the study
Discussion
The study had some important observations: mechanical low back pain subjects had subclinical segmental instability which were identified by Delphi criteria, would warrant further appropriate research and management. Evaluation had shown that subjective and objective findings if they are correlated with clinical reasoning, could effectively be used in short term management of low back pain patients. Multifidus strengthening should be considered either as an adjunct or in combination with other exercises for the spinal segmental instability. The quadruped position would have challenged spinal proprioception to the maximum; hence the improvement in spinal stiffness could be attributed to the enhanced proprioception due to co-contraction with selective activation of the segmental muscles. Clinical improvement was observed in the placebo group, which may be attributed to the effects of prone lying position itself would have its own effects to induce relaxation of the muscles in spasm thus relieving the symptoms. Further randomized controlled trials are needed and studies should compare global versus local stabilization either individual or in combination.
Segmental stabilizing muscle especially multifidus was found in earlier studies that there is selective atrophy at the affected level and that recovery of multifidus is not spontaneous following the episode of symptoms of low back pain. This indicates that a routine exercise program would not have long term benefits without activation of multifidus[17]. The earlier studies found that altered trunk muscle activation existed in low back pain subjects which when treated with motor control approaches, would thus enhance the lumbar posteroanterior stiffness in low back pain individuals[18,19].
Thus a hypothetical association existed between reduced lumbar postero anterior stiffness (as that occurring in instability) detected by manual examination using central PA pressure and reduced pressure pain thresholds (less pressure leading to pain provocation). However this association was not demonstrated in the earlier findings on lumbar spine examination, be it in normals or in individuals with mechanical low back pain. There was no comparable data as to whether there is any difference in the pressure pain thresholds with any intervention in subjects with segmental instability.
The current study design ruled out the probability of effects of almost all the confounding variables which might alter the findings like age, sex, body weight, individual differences in occupation or lifestyle. The incorporation of cross over design is not available in the literature on management using segmental stabilization possibly because the interventions were given for least duration of three weeks. This study has its major limitation that there was no long term follow up to determine the reversibility. The treatment session was only one, the results would have been influenced by the shorter treatment duration. The results of this should be interpreted with caution, since the patients who fulfilled the Delphi criteria were the ones who responded to therapy[20].
Conclusion
Segmental stabilization exercise therapy was more effective than placebo intervention in symptomatic lumbar segmental instability amongst people with mechanical low back pain.
Acknowledgments
The author wishes to thank the patients for their whole-hearted participation in the study.
References
- 1.Pincus T, Vogel S, Breen A, Foster N, Underwood M. Persistent back pain- why do physical therapy clinicians continue treatment? A mixed-methods study of chiropractors, osteopaths and physiotherapists. Eur J Pain. 2006;10:67–76. doi: 10.1016/j.ejpain.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: an examination of validity for determining intervention strategies in patients with low back pain. Arch Phys Med Rehab. 2005;86:1745–1752. doi: 10.1016/j.apmr.2005.03.028. [DOI] [PubMed] [Google Scholar]
- 3.Maitland GD. Examination of the lumbar spine. Aust J Physiother. 1971;17:5–11. doi: 10.1016/S0004-9514(14)61102-8. [DOI] [PubMed] [Google Scholar]
- 4.Lee RYW, Evans JH. The role of spinal tissues in resisting postero-anterior forces applied to the lumbar spine. J Manip Physiol Ther. 2000;23:551–556. doi: 10.1067/mmt.2000.109676. [DOI] [PubMed] [Google Scholar]
- 5.Goodsell M, Lee M, Latimer J. Short term effects of lumbar posteroanterior mobilization in individuals with low back pain. J Manip Physiol Ther. 2000;23:332–342. [PubMed] [Google Scholar]
- 6.Vanderween L, Oostendorp R, Vaes P, Duquet W. Pressure algometry in manual therapy. Man Ther. 1996;1:258–265. doi: 10.1054/math.1996.0276. [DOI] [PubMed] [Google Scholar]
- 7.Abbott JH, McCane B, Herbison P, Moginie G, Chapple C, Hogarty T. Lumbar segmental instability: a criterion-related validity study of manual therapy assessment. BMC Musculoskel Disord. 2005;6:56. doi: 10.1186/1471-2474-6-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Behrsin JF, Andrews FJ. Lumbar segmental instability: Manual assessment findings supported by radiological measurement (a case study) Aust J Physiother. 1991;37:171–173. doi: 10.1016/S0004-9514(14)60539-0. [DOI] [PubMed] [Google Scholar]
- 9.O’Sullivan PB. Lumbar segmental instability: clinical presentation and specific stabilizing exercise management. Man Ther. 2000;5:2–12. doi: 10.1054/math.1999.0213. [DOI] [PubMed] [Google Scholar]
- 10.Richardson C, Jull G, Toppenberg R, Comerford M. Techniques for active lumbar stabilization for spinal protection: A pilot study. Aust J Physiother. 1992;38:105–112. doi: 10.1016/S0004-9514(14)60555-9. [DOI] [PubMed] [Google Scholar]
- 11.Slade SC, Keating JI. Trunk-strengthening exercises for chronic low back pain: a systematic review. J Manip Physiol Ther. 2006;29:163–173. doi: 10.1016/j.jmpt.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 12.Koumantakis GA, Watson PJ, Oldham JA. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85:209–225. [PubMed] [Google Scholar]
- 13.Rackwitz B, de Bie R, Ewert T, Stucki G. Segmental stabilizing exercises and low back pain. What is the evidence? A systematic review of randomized controlled trials. Clin Rehab. 2006;20:553–567. doi: 10.1191/0269215506cr977oa. [DOI] [PubMed] [Google Scholar]
- 14.Rasmussen-Barr E, Nilsson-Wikmarn L, Arvidssonn I. Stabilizing training compared with manual treatment in sub-acute and chronic low-back pain. Man Ther. 2003;8:233–241. doi: 10.1016/s1356-689x(03)00053-5. [DOI] [PubMed] [Google Scholar]
- 15.Fritz JM, Erhard RR, Hagen BF. Segmental instability of the lumbar spine. Phys Ther. 1998;78:889–96. doi: 10.1093/ptj/78.8.889. [DOI] [PubMed] [Google Scholar]
- 16.Cook C, Brisme JM, Sizer PS. Subjective and objective descriptors of clinical lumbar spine instability: A Delphi study. Man Ther. 2006;11:11–21. doi: 10.1016/j.math.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 17.Cornwall J, Harris J, Mercer SR. The Multifidus muscle and patterns of pain. Man Ther. 2006;11:40–45. doi: 10.1016/j.math.2005.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Arokoski JP, Valta T, Kankaanpa M, Airaksinen O. Activation of lumbar paraspinal and abdominal muscles during therapeutic exercises in chronic low back pain patients. Arch Phys Med Rehab. 2004;85:823–832. doi: 10.1016/j.apmr.2003.06.013. [DOI] [PubMed] [Google Scholar]
- 19.van Dieën Jaap H, Selen LPJ, Cholewicki J. Trunk muscle activation in low-back pain patients, an analysis of the literature. J Electromyograph Kinesiol. 2003;13:333–351. doi: 10.1016/s1050-6411(03)00041-5. [DOI] [PubMed] [Google Scholar]
- 20.Christopher J, Colloca DC, Keller TS. Active trunk extensor contributions to dynamic posteroanterior lumbar spinal stiffness. J Manip Physiol Ther. 2004;27:229–237. doi: 10.1016/j.jmpt.2003.11.001. [DOI] [PubMed] [Google Scholar]



