Abstract
Objective
A callous-unemotional (CU) subtype of conduct disorder (CD) has been proposed as an addition to the fifth edition of the Diagnostic and Statistic Manual of Mental Disorders (DSM-5). This study tested the hypothesis that young girls with the CU subtype of CD will exhibit more severe antisocial behavior and less severe internalizing problems over time relative to girls with CD alone. Secondly, the developmental outcomes of girls with CU traits in the absence of CD was examined because these girls will be overlooked by the proposed CU subtyping scheme.
Method
Theses issues were examined in a community sample of 1862 girls aged 6-8 at study onset. Outcomes included internalizing and externalizing problems, academic achievement, and global impairment assessed concurrently and at a six year follow-up.
Results
Girls with the CU subtype of CD had higher levels of externalizing disorder symptoms, bullying, relational aggression, and global impairment than girls with CD alone. Girls with CD alone tended to have more anxiety problems than girls with the CU subtype of CD. Girls with high CU traits without CD exhibited higher ODD and ADHD symptoms and lower academic achievement at the six-year follow-up relative to girls without CU traits and CD. Group differences at the six year follow-up were primarily accounted for by baseline differences on the outcomes.
Conclusions
The proposed DSM-5 CU subtype of CD identifies young girls who exhibit lower anxiety problems and more severe aggression, CD symptoms, academic problems and global impairment across time than girls with CD alone.
Keywords: callous-unemotional, conduct disorder, longitudinal, DSM-5
The advisory committee on attention-deficit hyperactivity disorder (ADHD) and disruptive behavior disorders (DBD) for the fifth edition of the Diagnostic and Statistic Manual of Mental Disorders (DSM-5) has proposed possible modifications to diagnostic criteria for conduct disorder (CD)1. The most notable change involves adding a callous-unemotional (CU) subtype to CD based on evidence indicating these characteristics delineate a particularly malignant form of antisocial behavior2. CU traits include features such as a lack of empathy/guilt and shallow affect, akin to the affective features of adult psychopathy3. However, there remain concerns about the clinical utility of the proposed CU subtyping system, including the usefulness of delineating a CU subtype of CD in young girls1,2
The clinical utility of CU traits has previously been tested by examining whether these features predict serious and persistent antisocial behavior after controlling for co-occurring conduct problems. Longitudinal studies have shown that CU traits predict increases in conduct problems and antisocial behavior over time in both boys and girls, even after controlling for initial conduct problem severity4-6. Children with CD and high CU traits have also been shown to be at greater risk for continuing to meet criteria for CD three years later compared to children with CD alone7. In addition, evidence indicates that CU traits in adolescent boys and girls predicts adult offending and Antisocial Personality Disorder, even after controlling for co-occurring ODD/CD symptoms8.
The association between CU traits and internalizing problems is more complex. Some studies have found that CU traits are associated with lower levels of anxiety, while conduct problems are positively associated with anxiety, after controlling for their co-occurrence9-11. CU traits have also been associated with reduced anxiety/depression over time after controlling for co-occurring DBD symptoms in boys6. However, contradictory findings have also been reported, including evidence indicating that children with high CU and CD have problems with anxiety/depression equivalent to children with CD alone7. Moreover, CU traits may buffer girls with high levels of ODD/CD from experiencing anxiety problems, but not problems with depression11.
Based on the evidence briefly outlined above and detailed elsewhere1,3, members of the DSM-5 advisory committee have proposed using CU traits as a subtype of CD. To meet criteria for the proposed subtype, individuals must exhibit at least two out of four symptoms of CU traits that have consistently been identified in the literature2. We are aware of only two published studies that have tested the clinical utility of this specific subtyping scheme. The first consisted of 177 children (81% male) aged 6-11 years diagnosed with either ODD or CD who took part in a treatment outcome study. Children in the study who met criteria for the CU subtype did not have worse treatment outcomes across a three year follow-up period compared to children without the subtype12. The second study consisted of 754 adolescents (58% male) in the 7th grade who were part of a longstanding longitudinal study that originally oversampled kindergarteners with elevated behavior problems. This study found that the CU subtype of CD had good specificity and positive predictive power with respect to antisocial outcomes in later adolescence and early adulthood, but only nine youth met criteria for the subtype8. The first study assessed CU traits using only teacher report, while the second relied solely on parent report.
Current Study
Several issues regarding the clinical utility of the proposed CU subtyping scheme still need to be addressed. First, it is unclear whether the CU subtype can delineate a smaller subset of girls who meet diagnostic criteria for the childhood-onset subtype of CD. Second, there is limited evidence indicating that the proposed CU subtype of CD identifies girls with a more severe and persistent pattern of antisocial behavior and related problems (e.g., ADHD, poor academic performance) than girls with CD alone. Third, studies must clarify whether girls with the CU subtype of CD have a lower risk for developing internalizing problems relative to girls with CD alone. It is also unclear whether girls who meet the symptom threshold for the proposed CU subtype, but do not meet criteria for CD, are at risk for later maladaptive outcomes across multiple domains. This subgroup of girls are overlooked under the proposed CU subtyping scheme. These issues will be addressed using a large community sample of young girls assessed in early elementary school and then followed-up six years later.
Method
Participants
Participants were part of the larger Pittsburgh Girls Study (PGS), which consists of 2,451 girls aged 5-8 recruited from a sample of 103,238 households in the city of Pittsburgh. Enumeration was completed in 1999 with an oversampling of households in low-income neighborhoods. In total, 3,241 girls aged 5-8 were identified. A sample of 2,876 of these families were asked to participate in the study. A total of 2,451 (85.2%) families agreed (i.e., 588 five-year-olds, 630 six-year-olds, 611 seven-year-olds, 622 eight-year-olds). The current study included only the 1862 girls aged 6-8 because teacher reports of CU traits and CD symptoms were not available for the age 5 cohort. The racial distribution of the aged 6-8 girls was 53.5% African American, 40.7% Caucasian, 5.1% multiracial, and 0.8% Asian. In a majority of households (58.2%), the caretaker was cohabiting with a spouse/partner. Over one-third (38.1%) of families were receiving public assistance. Further details regarding the sample selection and characteristics are provided elsewhere13.
Procedures
Separate in-home interviews were conducted for the child and caretaker. Teacher information was obtained using self-administered questionnaires. This paper includes data collected at the initial assessment (Time 1) and a follow-up assessment that took place six years later (Time 7) when the girls were 12-14 years of age. The Time 7 assessment was the most recently completed and cleaned follow-up data at the time of analysis. All caretakers completed the interview at Time 1. Data were collected from 98.7% of girls and 80.1% of teachers at Time 1. At Time 7, data were collected from 91.1% of caretakers, 90.2% of girls, and 74.1% of teachers. Study procedures were approved by the University of Pittsburgh Institutional Review Board, and caretaker consent and child assent were obtained.
Measures
Conduct disorder
CD symptom counts and diagnoses were assessed using caretaker, teacher, and child reports on the Child Symptom Inventory – 4th edition (CSI-4)14 at Time 1 and on the Adolescent Symptom Inventory – 4th edition (ASI-4)15 at Time 7. Both measures include DSM-IV symptoms of CD worded very similarly and scored on a four-point scale (0=never to 3=very often). Teacher reports were collected on only 8 of the 15 DSM-IV symptoms of CD because teachers were not expected to have reliable knowledge about the other CD symptoms. At Time 1, caretakers and children rated all CD symptoms except for running away from home and truancy because these behaviors are practically non-existent in very young children. At Time 7, these symptoms were included in both measures. Items were combined across informants to reflect the highest value from any informant. Symptoms were dichotomized (present/absent) and summed using the standardized scoring procedures for the CSI/ASI14,15. Consistent with DSM-IV, girls with three or more symptoms were classified as having CD.
Callous unemotional traits
CU symptom counts at Time 1 and Time 7 were assessed using caretaker and teacher reports on four items from the Antisocial Processes Screening Device16. The items reflect the proposed DSM-5 symptoms of CU traits2: 1) Cares about how well she does at school/work; 2) Feels bad or guilty when she does something wrong; 3) Does not show her emotions to others; and 4) Is concerned about the feelings of others. Items were scored on a three-point scale (0=not at all true to 2=definitely true). In order for a symptom to be considered present, positively worded items must be rated as “not at all true,” and the one negatively worded item must be rated as “definitely true." A symptom is considered present if reported by either the parent or teacher. Consistent with the proposed subtyping scheme for DSM-5, girls with CD who exhibited at least two of the four symptoms of CU traits are delineated as having the CU subtype2.
Oppositional defiant disorder
The eight DSM-IV ODD symptoms were assessed using a combined estimate of caretaker and teacher reports on the CSI-4 at Time 1 and on the ASI-4 at Time 7. Items were combined to reflect the highest value from any informant. Symptoms were dichotomized (present/absent) and summed using the standardized scoring procedures for the CSI/ASI14,15. The internal consistency coefficient was α=.87 at Time 1 and α=.90 at Time 7.
Attention-Deficit Hyperactivity Disorder
DSM-IV ADHD symptoms were also assessed using a combined estimate that took the highest value of caretaker and teacher reports on each item using the CSI-4 at Time 1 and on the ASI-4 at Time 7. Symptoms were dichotomized (present/absent) and summed using the standardized procedures for the CSI/ASI14,15. The internal consistency coefficient was α=.89 at Time 1 and α=.91 at Time 7.
Depression
The nine DSM-IV symptoms of a major depressive episode were assessed from caretaker report on the CSI-4 at Time 1 and from a combination of caretaker and self-report on the ASI-4 at Time 7. Caretaker and child ratings at Time 7 were combined to reflect the highest value from any informant. Symptoms were dichotomized (present/absent) and summed using the standardized scoring procedures for the CSI/ASI14,15. The internal consistency coefficient was α=.52 at Time 1 and α=.62 at Time 7.
Anxiety
Problems with anxiety were measured with the Screen for Child Anxiety Related Emotional Disorders (SCARED)17 The SCARED subscales of generalized anxiety, panic/somatic, and social phobia were administered to the caretaker at Time 1 and the caretaker and child at Time 7. Items were combined at Time 7 by using the highest value between the two informants. Items were summed to created a total anxiety score. The internal consistency coefficient was α=.89 at Time 1 and α=.92 at Time 7.
Bullying
Problems with bullying were assessed using five items from the teacher-reported Mount Hope Family Center Bully-Victim Questionnaire.18 Items were summed to create a total bullying score. This scale was not administered until Time 3, so bullying behavior at this initial assessment was use as a proxy measure for baseline levels when predicting Time 7 bullying. The internal consistency coefficient was α=.91 at Time 3 and α=.93 at Time 7.
Relational aggression
Parent and teacher report of relational aggression was measured with the Children’s Peer Relationship Scale19at Time 1 and Time 7 The current study used five. common items that were administered to both informants, with items being combined to reflect the highest value across the informants. Items were summed to create a total relational aggression score. The internal consistency coefficient was α=.89 at Time 1 and α=.89 at Time 7.
Academic Achievement
Parents rated the girls academic achievement on a 5-point scale separately for reading, writing, and arithmetic at Time 1 and Time 7.19 Items were averaged so that higher scores indicated better academic achievement. The internal consistency coefficient was α=.89 at Time 1 and α=.89 at Time 7.
Global Impairment
Parents and staff that conducted the research interviews with the families completed the Child Global Assessment Scale (C-GAS)20 as a measure of the girls’ overall functioning. C-GAS ratings were reverse scored so that higher values indicated greater impairment (range = 1-100). The rating representing the greatest impairment across the two informants was used.
Data Analysis Plan
All data were analyzed within STATA version 9.221. Because the PGS over-sampled low income families, analyses were weighted using the inverse of the probability of being included in the sample due to the sampling design. Four mutually exclusive groups were created at Time 1. The groups included girls who did not meet criteria for either CD or CU (No CD/CU), those who only met symptom threshold criteria for CU (CU only), those who only met symptom threshold criteria for CD (CD only), and those who met threshold criteria for both CD and CU (CD/CU). Regression models were used to compare the four groups on internalizing and externalizing variables measured at the baseline assessment. Next, regression models were used to compare the groups on the same outcomes measured six years later. These models were first run without controlling for initial levels on the outcome and then run again controlling for baseline levels of the outcome.
Negative binomal regression was used for all symptom counts and the bullying outcome to account for the positive skew and overdispersion of the variables relative to a Poisson distribution. Ordinary least squares regression was used for all other outcomes because they approximated a Gaussian distribution. These variables were transformed to z-scores prior to the analysis so the beta weights represented group differences in standard deviation units.
Results
Prevalence of CD/CU Groups
All prevalence statistics are weighted to account for the oversampling of girls in low income neighborhoods. At Time 1, the prevalence of the CU subtype of CD was 3.0% and the prevalence of CD alone was 9.3% using the combined informant information. Another 4.3% of girls met symptom threshold for CU traits without CD. When parent and teacher reports were considered separately, the prevalence of CU subtype of CD and CD only was lower: parent (CD only=2.5%, CU/CD=0.5%) and teacher (CD only=3.1%, CU/CD=1.9%). For self-report alone, the prevalence of CD was 4.0%. The prevalence of the CU only group was 2.0% using only parent report and 2.5% using only teacher report.
Demographic Characteristics
Analysis revealed no significant differences between the four groups in terms of the girl’s age (ps>.05). Relative to the no CD/CU group, there was a greater proportion of minority girls in the CU (Odds Ratio(OR)=2.52, p<.001), CD (OR=3.46, p<.001), and CD/CU groups (OR=6.56, p<.001). The CD/CU group had a higher proportion of minority girls than the CU group (OR=6.56, p<.001), but the CD group was not significantly different from the CU or CD/CU groups (ps>.05). Minority status was controlled for in all subsequent analyses.
Symptom Profiles for CD/CU Groups
Figure 1 displays the CD and CU symptom profiles for each of the diagnostic groups. Girls in the CD/CU group were more likely to exhibit a lack of guilt (OR=5.76, p<.001) and lack of empathy (OR=6.36, p<.001) compared to the CU only group, but were less likely to exhibit shallow emotions (OR=0.31, p<.01) and a lack of school concern (OR=0.41, p<.05) than the CU only group. Girls in the CD/CU group were more likely to bully/threaten (OR=2.09, p<.05) and lie/con others (OR=2.89, p<.01) than girls in the CD only group.
Figure 1.
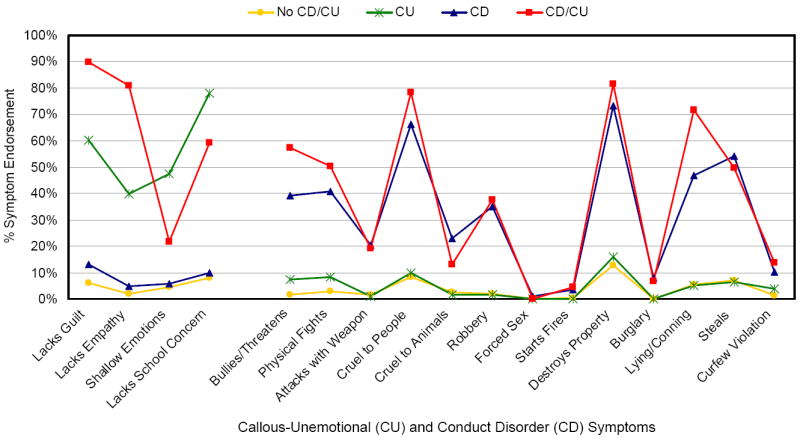
Symptom profiles for diagnostic groups at the initial assessment.
Group Differences at Initial Assessment
Group differences on externalizing and internalizing problems measured at Time 1 are presented in Table 1. Girls in the CU, CD, and CD/CU groups had significantly higher levels of ODD and ADHD symptoms, relational aggression, and global impairment and lower levels of academic achievement than girls in the No CD/CU group. Girls in the CD and CD/CU groups exhibited more pathological levels of all of these behaviors than girls in the CU only group, except for academic achievement. Girls in the CD/CU group had higher levels of ODD and ADHD symptoms, relational aggression, and global impairment than girls with CD alone. Girls in the CD only and CD/CU groups exhibited higher levels of depressive symptoms than girls in the No CD/CU group. Girls in the CD only group had higher levels of anxiety problems than girls in all other groups.
Table 1.
Comparison of Diagnostic Groups on Baseline Measures
| Incidence Rate Ratio (95% Confidence Interval) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group Means (Standard Errors) | Comparison with No CD/CU | Comparison Between Clinical Groups | ||||||||
| No CD/CU N=1553 |
CU N=79 |
CD N=173 |
CD/CU N=57 |
CU | CD | CD/CU | CD vs. CU | CD/CU vs. CU |
CD/CU vs. CD |
|
| ADHD symptoms | 2.28 (0.08) | 5.00 (0.46) | 6.42 (0.35) | 10.60 (0.64) | 2.50*** (1.75, 3.57) | 5.23*** (4.35, 6.30) | 10.29*** (8.5, 12.45) | 2.10*** (1.45, 3.03) | 4.12*** (2.85, 5.95) | 1.97*** (1.61, 2.40) |
| ODD symptoms | 0.53 (0.03) | 1.31 (0.23) | 2.75 (0.20) | 5.39 (0.38) | 2.11*** (1.73, 2.56) | 2.68*** (2.34, 3.07) | 4.26*** (3.69, 4.93) | 1.27* (1.03, 1.58) | 2.02*** (1.62, 2.53) | 1.59**** (1.34, 1.88) |
| Depression symptoms | 0.41 (0.02) | 0.56 (0.11) | 0.92 (0.09) | 1.01 (0.17) | 1.19 (0.77, 1.83) | 1.84*** (1.49, 2.28) | 1.99*** (1.34, 2.96) | 1.55 (0.98, 2.46) | 1.68 (0.96, 2.96) | 1.08 (0.71, 1.65) |
| Regression Coefficient (95% Confidence Interval) | ||||||||||
| Relational Aggression | -0.15 (0.02) | 0.26 (0.13) | 0.75 (0.08) | 1.42 (0.18) | 0.37*** (0.10, 0.63) | 0.84*** (0.67, 1.01) | 1.50*** (1.15, 1.84) | 0.47** (0.16, 0.78) | 1.13*** (0.70, 1.56) | 0.66*** (0.28, 1.04) |
| Anxiety Problems | -0.02 (0.03) | -0.08 (0.11) | 0.28 (0.08) | -0.17 (0.13) | -0.05 (-0.27, 0.16) | 0.31*** (0.15, 0.48) | -0.13 (-0.39, 0.13) | 0.37*** (0.11, 0.63) | -0.08 (-0.41, 0.25) | -0.45*** (-0.74, -0.15) |
| Academic Achievement | 0.08 (0.03) | -0.38 (0.12) | -0.34 (0.07) | -0.65 (0.15) | -0.40*** (-0.64, -0.17) | -0.36*** (-0.51, -0.21) | -0.64*** (-0.93, -0.34) | 0.05 (-0.23, 0.32) | -0.23 (-0.61, 0.14) | -0.28 (-0.61, 0.05) |
| Global Impairment | -0.15 (0.02) | 0.16 (0.14) | 0.89 (0.09) | 1.31 (0.18) | 0.29* (0.12, 0.57) | 1.02*** (.083, 1.20) | 1.43*** (1.07, 1.79) | 0.73*** (0.40, 1.06) | 1.14*** (0.69, 1.58) | 0.41* (0.02, 0.80) |
Note: Minority status was controlled for in all analyses. All values in bold are statistically significant at p < .05.
ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; CU = callous-unemotional; ODD = oppositional defiant disorder.
p<.05;
p<.01;
p<.001
Diagnostic Continuity Over Time
Information on the continuityof the four diagnostic groups fr om the initial assessment to the 6-year follow-up is presented in Figure 2. Relative to the No CD/CU group, girls in the CD/CU (OR=5.82, p<.001), and CD only (OR=2.98, p<.001) groups were more likely to be diagnosed with CD (regardless of CU traits) at follow-up. Girls in the CD only (OR=2.25, p<.05) and CD/CU group (OR=4.38, p<.001) were also more likely to be diagnosed with CD at follow-up relative to CU only group. The CD/CU group also had a higher prevalence of CD diagnosis at follow-up than the CD only group (OR=1.95, p<.05). No significant differences between the CU only and No CD/CU group were found for CD diagnosis at the 6-year follow-up (p >.05).
Figure 2.
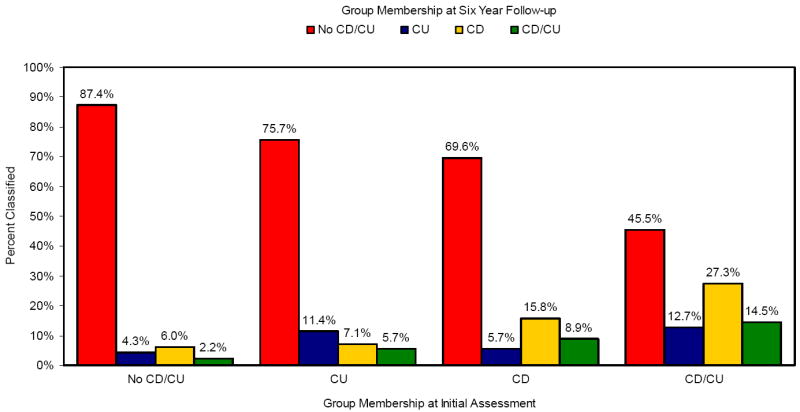
Stability of diagnostic classification from the initial assessment to the six-year follow-up. Note: CD = conduct disorder; CU = callous-unemotional.
Analysis also indicated that girls in the CU only (OR=2.20, p<.001), CD only (OR=1.78, p<.001), and CD/CU (OR=3.58, p<.001) groups were significantly more likely to meet symptom threshold for CU traits (regardless of a CD diagnosis) relative to girls originally classified in the No CD/CU group. However, there were no significant differences between these three baseline diagnostic groups in terms of meeting symptom threshold criteria for CU traits at follow-up (ps>.05).
Predictive Utility of CD and CU subgroups
Analyses examining outcomes of the four groups at the 6-year follow-up without controlling for prior behavior are presented in Table 2. Relative to the No CD/CU group, girls in the CU only group continued to exhibit higher ODD and ADHD symptoms and lower levels of academic achievement. The CD only girls continued to have more problems on all outcomes assessed relative to the No CD/CU group and had more problems associated with depression, anxiety, relational aggression, and global impairment than the CU only group. The CD group also had higher levels of anxiety in comparison to the CD/CU group. Relative to the No CD/CU and CU only groups, girls in the CD/CU combined group exhibited more problematic levels of all outcomes except for depression and anxiety. The CD/CU group also had lower levels of academic achievement and higher levels of ODD symptoms, relational aggression, bullying, and global impairment compared to CD only group.
Table 2.
Comparison of Diagnostic Groups on Outcomes Six Years Later Without Controlling for Baseline Differences
| Incidence Rate Ratio (95% Confidence Interval) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Group Means (Standard Errors) | Comparison with No CD/CU | Comparison Between Clinical Groups | ||||||||
| No CD/CU N=1409 |
CU N=70 |
CD N=158 |
CD/CU N=55 |
CU | CD | CD/CU | CD vs. CU | CD/CU vs. CU |
CD/CU vs. CD |
|
| ADHD symptoms | 2.57 (0.10) | 4.16 (0.58) | 5.54 (0.40) | 7.46 (0.77) | 1.48** (1.11, 1.97) | 1.97*** (1.66, 2.35) | 2.47*** (1.98, 3.07) | 1.33 (0.97, 1.82) | 1.67** (1.18, 2.34) | 1.25 (0.97, 1.61) |
| ODD symptoms | 0.85 (0.05) | 1.43 (0.27) | 2.02 (0.21) | 3.11 (0.40) | 1.57* (1.07, 2.3) | 2.20*** (1.74, 2.78) | 3.29*** (2.48, 4.37) | 1.4 (0.92, 2.12) | 2.10** (1.34, 3.27) | 1.50* (1.08, 2.07) |
| Depression symptoms | 1.73 (0.05) | 1.66 (0.21) | 2.34 (0.13) | 2.23 (0.22) | 0.92 (0.72, 1.17) | 1.30*** (1.15, 1.47) | 1.21 (0.99, 1.48) | 1.41** (1.09, 1.83) | 1.32 (0.97, 1.79) | 0.93 (0.75, 1.16) |
| Bullying | 1.19 (0.06) | 1.82 (0.34) | 2.73 (0.31) | 4.60 (0.59) | 1.26 (0.8, 2) | 1.77*** (1.38, 2.27) | 2.70*** (2.05, 3.57) | 1.40 (0.86, 2.29) | 2.14*** (1.29, 3.54) | 1.52* (1.09, 2.14) |
| Regression Coefficient (95% Confidence Interval) | ||||||||||
| Relational Aggression | -0.10 (0.03) | 0.08 (0.12) | 0.49 (0.08) | 0.93 (0.14) | 0.10 (-0.13, 0.33) | 0.50*** (0.33, 0.67) | 0.90*** (0.63, 1.17) | 0.40** (0.12, 0.67) | 0.80*** (0.45, 1.15) | 0.40* (0.09, 0.72) |
| Anxiety Problems | -0.02 (0.03) | -0.09 (0.12) | 0.27 (0.08) | -0.08 (0.15) | -0.07 (-0.3, 0.17) | 0.29*** (0.12, 0.46) | -0.07 (-0.38, 0.24) | 0.36* (0.08, 0.64) | 0.00 (-0.38, 0.38) | -0.36* (-0.07, -0.02) |
| Academic Achievement | 0.08 (0.03) | -0.27 (0.12) | -0.31 (0.07) | -0.73 (0.14) | -0.25*** (-0.49, 0.00) | -0.27*** (-0.43, -0.11) | -0.63*** (-0.90, -0.37) | -0.02 (-0.30, 0.26) | -0.39* (-0.74, -0.04) | -0.37* (-0.66, -0.07) |
| Global Impairment | -0.10 (0.03) | -0.04 (0.10) | 0.55 (0.08) | 0.99 (0.18) | 0.02 (-0.19, 0.24) | 0.61*** (0.44, 0.79) | 1.02*** (0.66, 1.38) | 0.59*** (0.33, 0.85) | 1.00*** (0.59, 1.41) | 0.41* (0.02, 0.80) |
Note. Minority status was controlled for in all analyses. All values in bold are statistically significant at p < .05.
ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; CU = callous-unemotional; ODD = oppositional defiant disorder.
p<.05;
p<.01;
p<.001
The models predicting the Time 7 outcomes were then re-run controlling for baseline levels of the outcomes at Time 1. Because bullying was not assessed until Time 3, levels of bullying at this assessment wave were controlled for in the analysis. As seen in Table 3, many group differences became non-significant after controlling for baseline differences. However, the CD only group exhibited higher levels of ADHD, ODD and depressive symptoms relative to the No CD/CU group, and higher levels of depressive symptoms relative to the CU only group. Girls in the CD only and CD/CU groups both exhibited higher levels of relational aggression and global impairment than the No CD/CU and CU only groups, and exhibited higher levels of bullying compared to the No CD/CU group. However, the CD/CU and CD only groups were not significantly different from one another on any outcomes.
Table 3.
Comparison of Diagnostic Groups on Outcomes Six Years Later After Controlling for Baseline Differences
| Incidence Rate Ratio (95% Confidence Interval) | ||||||
|---|---|---|---|---|---|---|
| Comparison with No CD/CU | Comparison Between Clinical Groups | |||||
| CU | CD | CD/CU | CD vs. CU | CD/CU vs. CU | CD/CU vs. CD | |
| ADHD symptoms | 1.06 (0.81, 1.4) | 1.26** (1.06, 1.50) | 1.09 (0.80, 1.48) | 1.18 (0.88, 1.59) | 1.02 (0.70, 1.50) | 0.87 (0.63, 1.18) |
| ODD symptoms | 1.41 (0.94, 2.12) | 1.55*** (1.20, 2.00) | 1.42 (0.90, 2.22) | 1.09 (0.70, 1.71) | 1.00 (0.57, 1.77) | 0.91 (0.59, 1.42) |
| Depression symptoms | 0.91 (0.72, 1.17) | 1.21** (1.07, 1.37) | 1.14 (0.93, 1.40) | 1.32* (1.02, 1.72) | 1.24 (0.91, 1.70) | 0.94 (0.75, 1.18) |
| Bullying | 1.24 (0.70, 2.18) | 1.43* (1.07, 1.93) | 2.16*** (1.52, 3.05) | 1.16 (0.63, 2.11) | 1.74 (0.93, 3.25) | 1.50§ (1.00, 2.27) |
| Regression Coefficient (95% Confidence Interval) | ||||||
| Relational Aggression | 0.02 (-0.19, 0.23) | 0.31*** (0.14, 0.48) | 0.57*** (0.27, 0.88) | 0.29* (0.03, 0.55) | 0.55** (0.19, 0.91) | 0.26 (-0.07, 0.59) |
| Anxiety Problems | -0.06 (-0.28, 0.15) | 0.16 (-0.01, 0.33) | -0.03 (-0.31, 0.26) | 0.23 (-0.03, 0.48) | 0.04 (-0.31, 0.39) | -0.19 (-0.51, 0.13) |
| Academic Achievement | -0.04 (-0.27, 0.18) | -0.12 (-0.27, 0.03) | -0.34* (-0.61, -0.08) | -0.08 (-0.34, 0.19) | -0.30 (-0.64, 0.04) | -0.22 (-0.52, 0.07) |
| Global Functioning | -0.05 (-0.26, 0.15) | 0.38*** (0.20, 0.56) | 0.67*** (0.32, 1.01) | 0.43** (0.17, 0.69) | 0.72*** (0.33, 1.11) | 0.29 (0.08, 0.66) |
Note. Minority status and baseline levels of the outcomes were controlled for in all analyses. Bullying at Time 3 was used as a control variable since this was the first phase it was administered. All values in bold are statistically significant at p < .05.
ADHD = attention-deficit/hyperactivity disorder; CD = conduct disorder; CU = callous-unemotional; ODD = oppositional defiant disorder.
p<.05;
p<.01;
p<.001;
p=.051.
Dimensional Approach
We conducted supplemental analyses to determine whether the results would be similar using a dimensional approach to assess CU traits and CD (see Supplement 1, available online). The primary analyses were repeated with CD and CU scales that were generated by summing the items used to define the subgroups as predictors. A CD by CU interaction term was also tested to determine if the association between CU traits the outcomes varied by level of CD symptom. Significant interactions were probed by examining the association between CU traits and the outcomes for girls with low (-1 SD), moderate (the mean), and high (+1 SD) levels of CD symptom severity. The findings will be briefly reviewed here.
The findings predicting baseline levels of the outcomes largely mimicked the categorical analyses (see Table S1, available online). Some notable exceptions involved significant interactions between CU traits and CD symptom severity. For example, findings indicated that CU traits were significantly associated with increased depressive symptoms, but only for girls with low and moderate levels of CD. In contrast, CU traits were associated with lower levels of anxiety only for girls with moderate and high levels of CD.
Results predicting outcomes at the six year follow-up (with and without controlling for baseline levels) were also largely consistent with the group-based findings (see Tables S2 and S3, available online). Even after controlling for baseline CD symptoms severity, CU traits predicted higher levels of CD symptoms at the six year follow-up. After controlling for baseline levels of the outcomes and CD symptoms, CU traits were also associated with lower levels of academic achievement and global functioning at the 6-year follow-up. CU traits were also associated with higher levels of bullying behavior, but only for girls with moderate and high levels of CD symptom severity. Conversely, CU traits significantly predicted higher levels of ODD and ADHD symptoms for girls with low and moderate CD symptoms at baseline. CD symptoms, but not CU traits, were associated with increased levels of anxiety and depression at the follow-up, even after controlling for baseline levels of these problems.
Discussion
The current study examined the clinical utility of the CU subtype of CD proposed for use in DSM-5 using a large community sample of young girls2. In support of the utility of the CU subtyping scheme, girls with the CU subtype of CD exhibited a more severe antisocial behavior that persisted across a six-year follow-up in comparison to girls with CD alone. At the follow-up assessment, the combined CD/CU girls were more likely to meet criteria for CD and had higher levels of both relational aggression and bullying behavior relative to girls with CD alone. This is consistent with evidence indicating that CU traits in adjudicated girls are associated with social goals involving dominating others and forcing “respect” in peer conflict situations22. Interestingly, girls with the CU subtype of CD were more likely than girls with CD alone to lie to con others, which is a core feature of adult psychopathy. Girls with the CU subtype of CD also had the greatest global impairment and lowest academic achievement at follow-up, further supporting the clinical utility of this subtyping scheme.
The differences between girls with CU subtype of CD and those with CD alone were reduced to non-significance at the six-year follow-up after controlling for group differences on the outcomes at the initial assessment. Consequently, girls with the CU subtype did not experience greater increases in antisocial behavior relative to girls with CD alone. However, other studies have found that CU traits may predict increases in general impairment in girls23, and externalizing problems in both boys and girls5,24 across shorter intervals of time. In addition, CU traits measured in early adolescence have been shown to significantly predict adult criminal behavior even after controlling for co-occurring CD symptoms in boys and girls8. It is possible that the long-term predictive utility of CU traits becomes more pronounced during adolescence as these features become more stable and solidified. However, when CU traits were measured using a dimensional approach, they were associated with higher CD symptom severity, higher impairment, and lower academic achievement at follow-up even after controlling for baseline levels of these problems and co-occurring CD symptoms. CU traits also predicted higher levels of bullying behavior for girls with high CD symptom severity. It is well documented that dimensional approaches are often superior to categorical conceptualization of mental health disorders when predicting clinical outcomes25, which is why different strategies for incorporating symptom severity information into the DSM-V are currently being considered26.
The pattern of findings for internalizing problems was quite different. Results indicated that girls with CD exhibited elevated depressive symptoms regardless of whether or not they had CU traits. While the CD only girls experienced increases in depressive symptoms over time relative to girls with no CD or CU traits, girls with the CU subtype of CD did not exhibit increased depression symptoms at the six-year follow-up. In fact, girls with the CU subtype of CD had lower levels of anxiety than girls with CD alone at the initial assessment and the six-year follow-up. Moreover, girls with high CU traits had the lowest overall anxiety scores relative to the other groups at both assessments. This finding is consistent with previous investigations indicating that the positive association between conduct problems and anxiety tends to become more pronounced when controlling for co-occurring CU traits 9,11. It is also congruent with evidence indicating that low fearfulness may contribute to the development of CU traits5
The continuity of the CU subtype of CD was relatively poor across the six-year follow-up, with 14.5% of girls initially classified as having the CU subtype of CD meeting criteria for this subtype six years later. Although this finding contradicts studies indicating that dimensional measures of CU traits are relatively stable in children24,27, it is consistent with evidence that categorically defined DSM mental disorders often have relatively poor temporal stability. For example, clinic-referred children with CD often exhibit a waxing and waning of symptoms across time, making the diagnostic continuity of CD across any two time points relatively low28. When the temporal stability of dimensional measures of CU traits and DBD symptoms have been directly compared in girls, evidence suggests that both have moderate levels of year-to-year stability29. While the childhood-onset subtype of CD was adopted in part to avoid the complexities associated with having a dynamic subtyping scheme, concerns have been raised about the unreliability of retrospective reports to assess age of onset in clinical practice1.
There has been increasing interest in examining the developmental outcomes of children with high CU traits who do not meet criteria for CD. This group of girls was relatively rare, making up only 4.3% (weighted) of the total sample. Interestingly, the CU only girls were more likely to exhibit shallow affect and a lack of concern about school work, and less likely to exhibit a lack of guilt and empathy than girls with the CU subtype of CD. The less pronounced callous disregard for the suffering of others in the CU only girls may have protected them from exhibiting more serious forms of antisocial behavior. However, these girls were not completely devoid of externalizing problems, as they exhibited higher levels of ADHD, ODD and relational aggression than girls with neither CD nor CU traits at baseline, and their elevated ODD and ADHD symptoms persisted across the 6-year follow-up.
The prevalence of CD among the girls in the study was higher than in previous investigations30. Girls in the study were recruited from an urban city with a poverty and crime rate slightly above the national average, which could partially account for the high prevalence rate. The use of a multiple informants approach that counted a symptom as present if endorsed by either the parent, teacher, or child also increased the prevalence rate. Weighted prevalence estimates of CD were 3.1%-5.0% when the informants were considered separately. While the best method for combining multiple informant symptom information is a matter of ongoing debate in the field, several studies support the use of the either/or method used in the current investigation31,32. However, the use of rating scales that do not take into account impairment or clinical expertise when making diagnoses may have also contributed to the increased prevalence rates.
The findings need to be considered in the context of other limitations. First, the results may not generalize to males or clinic-referred populations. The assessment of CU traits and CD took place in early childhood, and it is possible that the CU subtype of CD may have additional clinical utility and higher temporal continuity in adolescence. Lastly, the current study was focused on testing a specific definition of the CU subtype of CD2. Future studies should explore alternative subtyping schemes that include a more diverse array of CU symptoms and/or use diagnostic interviews to assess CU traits.
With these limitations in mind, the overall findings emphasize the multi-faceted problems that plague young girls with CD irrespective of the presence of CU traits. Effective interventions for girls with CD will likely need to include an array of services such as parent management training, medication management for ADHD, and individualized educational planning. Girls with the CU subtype of CD would likely benefit from interventions that emphasize gender-sensitive cognitive-behavioral skills training designed to reduce the types of bullying and relational aggression that often occur within female peer groups. Girls with CD in the absence of CU traits may require treatment programming that places a greater emphasis on building emotion regulation skills and modifying maladaptive cognitions that promote feelings of depression and anxiety.
The potential incorporation of CU traits into the diagnosis of CD in DSM-5 is a matter of ongoing debate. The current study provides some evidence for the clinical utility of a recently proposed CU subtype of CD in young girls that could at least supplement the childhood-onset distinction outlined in DSM-IV. Young girls with the CU subtype of CD appear to be at high risk for exhibiting serious and persistent forms of antisocial behavior in the absence of persistent internalizing problems, with the latter being more prevalent in girls with CD alone. If studies continue to support the utility of the proposed CU subtype of CD, difficult decisions will have to be made about whether it should replace or augment the existing age of onset subtype.
Supplementary Material
Acknowledgments
This study is funded by the National Institute of Mental Health (MH056630), National Institute on Drug Abuse (DA012237), the Federation of Independent School Alumnae Foundation, and the Falk Foundation. Salary support provided to Drs. Hipwell (K01MH071790) and Pardini (K01MH078039) from the National Institute of Mental Health was used to complete work on this manuscript.
We would like to thank Drs. Deena Battista of the University of Pittsburgh Medical Center, and Kate Keenan of the University of Chicago, for their assistance with this manuscript, along with the Pittsburgh Public Schools and the Pittsburgh Girls Study families.
Footnotes
Drs. Pardini, Stepp, Hipwell, Stouthamer-Loeber, and Loeber report no biomedical financial interests or potential conflicts of interest.
Supplemental material cited in this article is available online.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Moffitt TE, Arseneault L, Jaffee SR, Kim-Cohen J, Koenen KC, Odgers CL, Slutske WS, Viding E. Research review: DSM-V conduct disorder: Research needs for an evidence base. J Child Psychol Psyciatr. 2008;49:3–33. doi: 10.1111/j.1469-7610.2007.01823.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frick PJ, Moffitt TE. A proposal to the DSM-V Childhood Disorders and the ADHD and Disruptive Behavior Disorders Work Groups to include a specifier to the diagnosis of Conduct Disorder based on the presence of callous-unemotional traits. 2010 Retrieved July 23, 2010 from http://www.dsm5.org/Proposed%20Revision%20Attachments/Proposal%20for%20Callous%20and%20Unemotional%20Specifier%20of%20Conduct%20Disorder.pdf.
- 3.Frick PJ, White SF. Research review: The importance of callous-unemotional traits for developmental models of aggressive and antisocial behavior. J Child Psychol Psyciatr. 2008;49(4):359–375. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- 4.Frick PJ, Cornell AH, Barry CT, Bodin SD, Dane HE. Callous-unemotional traits and conduct problems in the prediction of conduct problem severity, aggression, and self-report of delinquency. J Abnorm Child Psychol. 2003;31(4):457–470. doi: 10.1023/a:1023899703866. [DOI] [PubMed] [Google Scholar]
- 5.Pardini DA, Lochman JE, Powell N. The development of callous-unemotional traits and antisocial behavior in children: Are there shared and/or unique predictors? J Clin Child Adolesc Psychol. 2007;36(3):319–333. doi: 10.1080/15374410701444215. [DOI] [PubMed] [Google Scholar]
- 6.Pardini DA, Fite PJ. Symptoms of conduct disorder, oppositional defiant disorder, attention-deficit/hyperactivity disorder, and callous-unemotional traits as unique predictors of psychosocial maladjustment in boys: Advancing an evidence base for DSM-V. J Am Acad Child Adolesc Psychiatry. 2010;49(11):1134–1144. doi: 10.1016/j.jaac.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rowe R, Maughan B, Moran P, Ford T, Briskman J, Goodman R. The role of callous and unemotional traits in the diagnosis of conduct disorder. J Child Psychol Psyciatr. 2010;51(6):688–695. doi: 10.1111/j.1469-7610.2009.02199.x. [DOI] [PubMed] [Google Scholar]
- 8.McMahon RJ, Witkiewitz K, Kotler JS. Conduct Problems Prevention Research Group. Predictive validity of callous-unemotional traits measured in early adolescence with respect to multiple antisocial outcomes. J Abnorm Psychol. 2010;119(4):752–763. doi: 10.1037/a0020796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frick PJ, Lilienfeld SO, Ellis M, Loney B, Silverthorn P. The association between anxiety and psychopathy dimensions in children. J Abnorm Child Psychol. 1999;27(5):383–392. doi: 10.1023/a:1021928018403. [DOI] [PubMed] [Google Scholar]
- 10.Pardini DA, Lochman JE, Frick PJ. Callous/unemotional traits and social-cognitive processes in adjudicated youths. J Am Acad Child Adolesc Psychiatry. 2003;42(3):364–371. doi: 10.1097/00004583-200303000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Hipwell AE, Pardini DA, Loeber R, Sembower M, Keenan K, Stouthamer-Loeber M. Callous-unemotional behaviors in young girls: Shared and unique effects relative to conduct problems. J Clin Child Adolesc Psychol. 2007;36(3):293–304. doi: 10.1080/15374410701444165. [DOI] [PubMed] [Google Scholar]
- 12.Kolko DJ, Pardini DA. ODD dimensions, ADHD, and callous-unemotional traits as predictors of treatment response in children with disruptive behavior disorders. J Abnorm Psychol. 2010;119(4):713–725. doi: 10.1037/a0020910. [DOI] [PubMed] [Google Scholar]
- 13.Keenan K, Hipwell A, Chung T, Stepp S, Stouthamer-Loeber M, Loeber R, McTigue K. The Pittsburgh Girls Study: Overview and initial findings. J Clin Child Adolesc Psychol. 2010;39(4):506–521. doi: 10.1080/15374416.2010.486320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gadow K, Sprafkin J. Child symptom inventories manual. New York, NY: Checkmate Plus; 1994. [Google Scholar]
- 15.Gadow K, Sprafkin J. Adolescent symptom inventories manual. New York, NY: Checkmate Plus; 1998. [Google Scholar]
- 16.Frick PJ, Hare RD. Antisocial process screening device technical manual. Toronto, Canada: Multi-Health Systems; 2001. [Google Scholar]
- 17.Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The screen for child anxiety related emotional disorders (SCARED): Scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. 1997;36(4):545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Shields A, Cicchetti D. Parental maltreatment and emotion dysregulation as risk factors for bullying and victimization in middle childhood. J Clin Child Psychol. 2001;30(3):349–363. doi: 10.1207/S15374424JCCP3003_7. [DOI] [PubMed] [Google Scholar]
- 19.Crick NR, Grotpeter JK. Relational aggression, gender, and social-psychological adjustment. Child Dev. 1995;66(3):710–722. doi: 10.1111/j.1467-8624.1995.tb00900.x. [DOI] [PubMed] [Google Scholar]
- 20.Setterberg S, Bird H, Gould M. Parent and Interviewer Versions of the Children’s Global Assessment of Scale. New York: Columbia University; 1992. [Google Scholar]
- 21.Intercooled Stata 9.2 for Windows [computer program]. Version 9.2. College Station, TX: Stata Corporation; 2005. [Google Scholar]
- 22.Pardini DA. Perceptions of social conflicts among incarcerated adolescents with callous-unemotional traits: “You’re going to pay. It’s going to hurt, but I don’t care.”. J Child Psychol Psyciatr. 2011;52:248–255. doi: 10.1111/j.1469-7610.2010.02336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keenan K, Wroblewski K, Hipwell A, Loeber R, Stouthamer-Loeber M. Age of onset, symptom threshold, and expansion of the nosology of conduct disorder for girls. J Abnorm Psychol. 2010;119(4):689–698. doi: 10.1037/a0019346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawes DJ, Dadds MR. Stability and malleability of callous-unemotional traits during treatment for childhood conduct problems. J Clin Child Adolesc Psychol. 2007;36(3):347–355. doi: 10.1080/15374410701444298. [DOI] [PubMed] [Google Scholar]
- 25.Fergusson DM, Boden JM, Horwood LJ. Classification of behavior disorders in adolescence: Scaling methods, predictive validity, and gender differences. J Abnorm Psychol. 2010;119(4):699–712. doi: 10.1037/a0018610. [DOI] [PubMed] [Google Scholar]
- 26.Pardini DA, Frick PJ, Moffitt TE. Building an evidence base for DSM-5 conceptualizations of oppositional defiant disorder and conduct disorder: Introduction to the special section. J Abnorm Psychol. 2010;119(4):683–688. doi: 10.1037/a0021441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frick PJ, Kimonis ER, Dandreaux DM, Farell JM. The 4 year stability of psychopathic traits in non-referred youth. Behav Sci Law. 2003;21(6):713–736. doi: 10.1002/bsl.568. [DOI] [PubMed] [Google Scholar]
- 28.Lahey BB, Loeber R, Hart EL, Frick PJ, Applegate B, Zhang Q, Green SM, Russo MF. Four-year longitudinal study of conduct disorder in boys: patterns and predictors of persistence. J Abnorm Psychol. 1995;104(1):83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- 29.Loeber R, Pardini DA, Hipwell A, Stouthamer-Loeber M, Keenan K, Sembower MA. Are there stable factors in preadolescent girls’ externalizing behaviors? J Abnorm Child Psychol. 2009;37(6):777–791. doi: 10.1007/s10802-009-9320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Canino G, Polanczyk G, Bauermeister JJ, Rohde LA, Frick PJ. Does the prevalence of CD and ODD vary across cultures? Soc Psychiatry Psychiatr Epidemiol. 2010;45(7):695–704. doi: 10.1007/s00127-010-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bird H, Gould M, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of American Academy Child Adolescent Psychiatry. 1992;31(1):78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Piacentini J, Cohen P, Cohen J. Combining discrepant diagnostic information from multiple sources: are complex algorithms better than simple ones? J Abnorm Child Psychol. 1992;20(1):136–143. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


