Abstract
Background:
Epilepsy is a chronic medical condition with many co-morbid features. It has been observed that children with epilepsy (CWE) have a compromised quality of life (QOL).
Objective:
To assess the QOL in CWE and to study the various factors affecting QOL among CWE.
Materials and Methods:
The sample consisted of 102 CWE aged 5–15 years of either sex. QOL was measured by Quality of Life in Childhood Epilepsy (QOLCE) questionnaire, a 76-item, parent-reported questionnaire. Cronbach alpha was used to determine the internal consistency of the subscales and Pearson correlation to determine construct validity. The t-test and analysis of variance were used to compare mean QOLCE scores.
Results:
Factors affecting QOL included age, place of residence, socioeconomic condition, maternal education, seizure type and frequency and number of antiepileptic drugs.
Conclusion:
CWE have a relatively compromised QOL and comprehensive care needs to go beyond the attempt of controlling seizures.
Keywords: Children with epilepsy, health related quality of life, quality of life in childhood epilepsy questionnaire, quality of life
Introduction
Epilepsy can significantly affect the quality of life (QOL) not only because of its chronicity, need for regular medications, and their side effects, but also due to prejudices and social conventions that still surround it.[1]
The traditional medical goal in the management of epilepsy has focused almost exclusively on seizure control with minimal or no adverse medication effect,[1] whereas the importance of assessing QOL has been ignored. This is particularly true for Indian children, where the QOL is probably affected by the social stigma associated with the disease. Studies from India on children with epilepsy (CWE)[2,3] and a notable study in adults with epilepsy[4] have shown a relatively compromised QOL. We therefore conducted this study to highlight the need for formulating a comprehensive treatment program for CWE.
Materials and Methods
The study was conducted at Department of Pediatrics of a tertiary care teaching hospital in central India from October 2009 to November 2010.
Inclusion criteria
Epilepsy was defined as presence of two or more unprovoked seizures. Children aged between 4 and 15 years with minimum duration of epilepsy of 6 months were the cases.
Exclusion criteria
Children with co-morbid neurodevelopment conditions (mental retardation, developmental delay, cerebral palsy, autism, Attention deficit hyperactivity disorder (ADHD) behavioral disorders, etc.) and chronic medical conditions (asthma, hypertension, chronic renal failure (CRF), chronic lung disease (CLD), thalassemia, hypothyroidism, etc.) were excluded. Children whose primary caregiver was not available to answer the questionnaire were also excluded.
Instrument
The QOL instrument used was Child Epilepsy Questionnaire (Parental form) (CEQ-P). This parental questionnaire has two parts that together take 20 minutes to complete. Part one contains items assessing demographic profile, seizure description and medication (Child Seizure Profile, CSP); Part two contains items specifically assessing the health related quality of life (HRQOL) of CWE (Quality of Life in Childhood Epilepsy or QOLCE questionnaire).
CEQ-Part 1
The questionnaire included: (i) demographic data of children, such as age, gender, educational status of both the mother and children; (ii) clinical data of epilepsy, such as age at onset, age at diagnosis, current medication and duration of treatment, seizure frequency, and type of seizure; and (iii) familial economic state (according to modified Prasad classification).
CEQ-Part 2
QOLCE questionnaire was used to evaluate the QOL of the children. The QOLCE is a parental, multifaceted epilepsy-specific scale for evaluating the HRQOL of children aged 4-18 years. The questionnaire was developed by Mark Sabez et al. for measurement of QOL in CWE and to demonstrate instrument's validity, reliability and sensitivity. It contains 76 items with 16 subscales covering seven domains of life function: Physical activities, social activities, cognition, emotional well-being, behavior, general health, and general QOL.[5]
A researcher was present during the completion of the questionnaire and clarified any queries, and thereby ensured that the questionnaire items were not misunderstood. The tool used in the study was translated to Hindi by a bilingual medical person (pediatrician) and retranslated to English by a non-medical language expert. This version was compared with the original and anomalies were rectified by the same process. The final translated version was piloted on 20 children prior to the start of the study. test-retest reliability of translated version was established by using the cronbach alpha and Pearson correlation which showed good internal consistency construct validity.
The full score is 100. The higher the score, the better is the QOL of the children. In this study, QOLCE scores were used to identify relationship association trends of various factors affecting QOL. The QOLCE has not been validated for Indian patients; we translated it only for use in this study.
Parents/primary caregivers of all CWE fulfilling the inclusion criteria were approached for participation in the study. After an informed written consent was obtained from the caregivers and after giving detailed directions in filling the form, the questionnaire was provided to them for completion. One of the authors was available to address any queries during the process of filling the questionnaire. For illiterate patients, the author completed the questionnaire.
Data were analyzed by the biostatistician using Chi-square test for discrete variables and Student's t-test for continuous variables. Within group variations were analyzed using analysis of variance (ANOVA) and post hoc Tukey test. A P value <0.05 was considered as significant.
Results
A total of 149 children fulfilling the inclusion criteria were approached for participation and 102 patients were ultimately enrolled.
The baseline characteristics of the study population are depicted in Table 1. The mean age of the patients was 8.75 ± 3.6 years. Of the 102 patients, 61 (59.8%) were boys. Ratio of boys to girls was 1.58:1. Majority of CWE [62 (60.8%)] belonged to rural area. Socioeconomically, 7 (6.9%) belonged to upper high class, 2 (2%) to high class and 93 (70.6%) to low socioeconomic class. 66 (64.7%) children had no seizure in last 1 month, while 36 (35.3%) cases had a seizure frequency of 2–10 per month. Most of the cases [80 (79.4%)] were well controlled and on monotherapy, while 21 (20.6%) were on one or more than one drug. Most common type of seizures were partial seizure [58 (56.9%)] followed by generalized tonic-clonic seizure (GTCS) in 31 (30.4%), and absence seizure was seen in 7 (7.8%) cases.
Table 1.
Descriptive information of sample
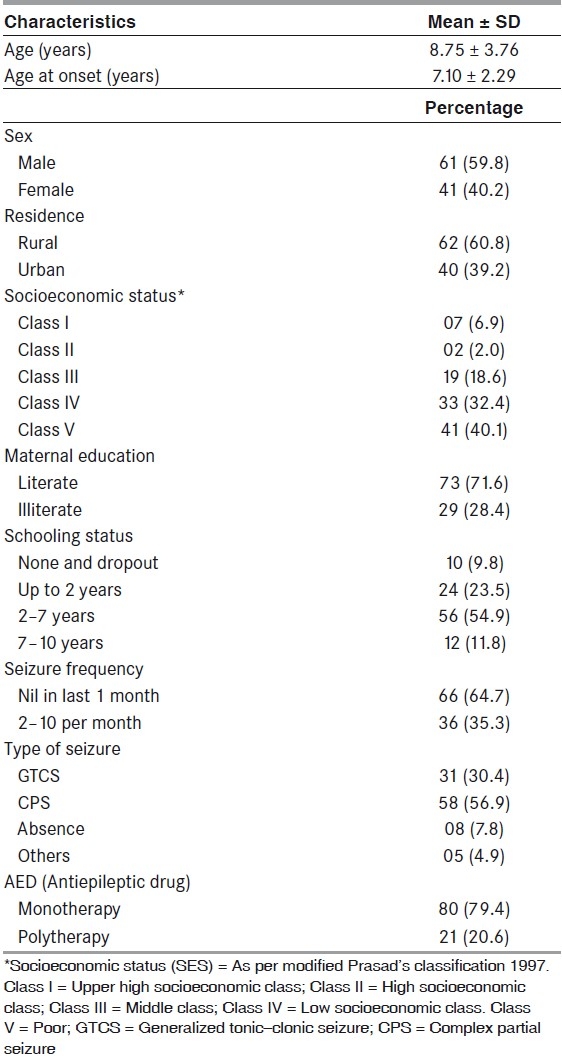
Majority of the caregivers (78.4%) were mothers, 19.6% were fathers and the rest were either relatives or neighbors. 71.6% of the mothers were literate. The socioeconomic status (SES) of the families is given in Table 1. 67.4% of the caregivers did not know their correct age.
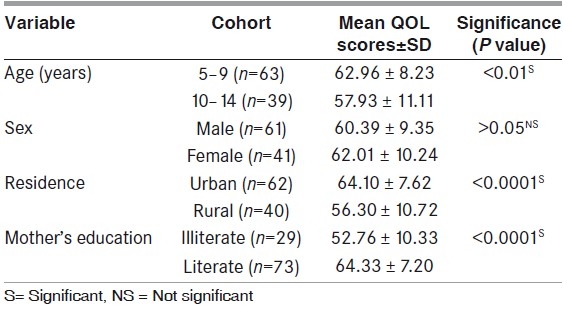
The relationship between QOL scores and various patient characteristics is shown in Table 2. Factors significantly associated with QOL were age, residence, maternal education, seizure type and frequency, and number of antiepileptic drugs.
Table 2.
Relationship of demographic variables with quality of life
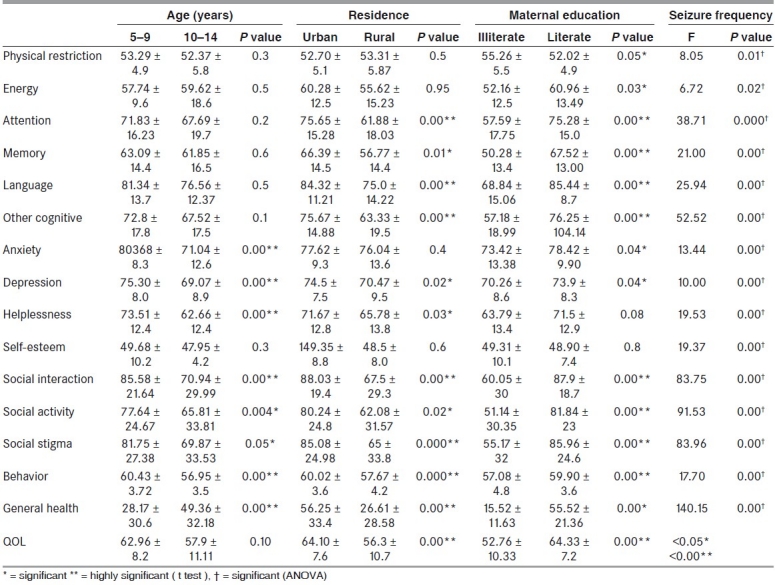
The various sub-domains of the QOL were also assessed to determine which domains were affected by the various patient and disease characteristics. The results are shown in Table 3. Behavioral, social, and emotional functions were significantly affected in rural areas, particularly in the older age group.
Table 3.
Relationships of various patient and disease characteristics with the sub-domains of the quality of life
Discussion
In our cross-sectional study to identify various factors affecting the QOL in CWE, we have tried to establish the association of demographic and epilepsy variables with QOL. Overall QOL was affected more in older children, those living in rural areas, those with lower SES and in mothers with lower literacy levels. QOL was also affected by disease characteristics, with a poorer QOL in children with higher seizure frequency and in those receiving polytherapy, having partial seizures, and longer duration of treatment.
The major strength of the study was the large sample size, much more than that of a previous similar study.[2]
Overall QOL was affected more in older children as compared to younger age group, similar to that reported by Devinsky et al.[6] Emotional, social and behavioral domains were affected more in older age group. This may be due to the fact that older children are more likely to perceive a greater negative impact on life and general health and have more negative attitude toward epilepsy. Language and memory were also found to be affected in the older age group. Rochelle Caplan et al.[7] reported that older epileptic children had more language impairment and a wider range of linguistic defects. As the instruments used in different studies are different, direct comparison was not possible. Furthermore, in some of the studies, the age groups were different and mostly of higher age than in our study.
Better QOL is observed in children of literate mothers and those from higher socioeconomic group, in all domains of life.[6] Maternal education explained significant amount of variance in qol scores of children in Prabhjot Malhi and Pratibha Singhi's study.[2] QOL in children living in rural area was highly compromised as compared to QOL of those in urban area. Behavioral and social domains were more significantly affected in rural areas. This may be due to the additive effect of lack of access to medical facility, illiteracy and more negative attitude and stigma present in rural community. Pal et al.,[8] for the first time, studied the social activities of children with epilepsy and their peers in rural India and found all groups of CWE had significant social deficit. Parental attitudes toward their children were found to be negative in 25%. Social stigma was found to be present more in CWE of rural area. In another study[9] involving the same families, the same research group measured mothers’ satisfaction with social support from informal sources and correlated it with a parental adjustment measure. They found positive independent correlation of satisfaction with social support. Our finding of impaired QOL with greater number of antiepileptic, longer duration of treatment and focal seizure is consistent with previous studies. Thomas et al., Sabez et al. and Devinsky et al.[4–6] have also reported a negative effect of polytherapy on QOL in CWE.
In the study, CWE had a more compromised QOL in psychological, social and behavioral functioning, whereas physical function was not found to be much affected. Austin et al.[10] showed that CWE had a relatively more compromised QOL in the psychological, social and school domains in contrast with other diseases which usually affect physical domain. The high prevalence of emotional, cognitive and behavioral problem in CWE is consistent with the results of previous studies. Rutter et al.[11] in their study reported 29% of CWE and 58% of CWE with seizure and CNS dysfunction had behavioral problems.
We found compromised QOL in Indian children with epilepsy, associated both with non-modifiable factors (demographic factors like socioeconomic status, maternal education, residence) as well as modifiable factors (seizure related variables like seizure frequency, number of antiepileptic drugs, etc.). Psychosocial and behavioral functioning has been found to be highly affected suggesting that QOL should be an important outcome measure in management of CWE, rather than only seizure control. It is suggested that children with epilepsy receive assessment of behavioral and academic functioning at initial diagnosis, and interventions designed to address behavioral and emotional problems in CWE should be an important management goal. In addition, QOL measures should also be a part of the periodic follow-up of children with epilepsy.
Acknowledgment
We acknowledge the help provided by Mr. Arvind Kawishwar, Biostatistician, Regional Medical Research Centre for Tribals, ICMR, Jabalpur, Madhya Pradesh, in the statistical work and analysis.
Footnotes
Source of Support: Nil,
Conflict of Interest: Nil.
References
- 1.Christianson AL, Zwane ME, Manga P, Rosen E, Venter A, Kromberg JG. Epilepsy in rural South Africa children-prevalence, associated disability and management. S Afr Med J. 2000;90:262–6. [PubMed] [Google Scholar]
- 2.Malhi P, Singhi P. Correlates of Quality of life with epilepsy. Indian J Pediatr. 2005;72:131–5. doi: 10.1007/BF02760697. [DOI] [PubMed] [Google Scholar]
- 3.Datta SS, Premkumar TS, Fielding S, Chandy S, Kumar S, et al. Impact of pediatric epilepsy of Indian Families: Influence of psychopathology and seizure variable. J Epilepsy Behav. 2006;9:145–51. doi: 10.1016/j.yebeh.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 4.Thomas SV, Koshy S, Nair CR, Sarma SP. Frequent seizures and polytherapy can impair quality of life in persons with epilepsy. Neurol India. 2005;53:46–50. doi: 10.4103/0028-3886.15054. [DOI] [PubMed] [Google Scholar]
- 5.Sabez M, Cairns DR, Lawson JA, Nheu N, Bleasel AF, Bye AM. Validation of a new quality of life measure for children with epilepsy. Epilepsia. 2000;41:765–74. doi: 10.1111/j.1528-1157.2000.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 6.Devinsky O, Westbrook L, Cramer J, Glassman M, Perrine K, Camfield C. Risk factors for poor health-related quality of life in adolescents with epilepsy. Epilepsia. 1999;40:1715–20. doi: 10.1111/j.1528-1157.1999.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 7.Caplan R, Siddarth P, Vona P, Stahl L, Bailey C, Gurbani S, et al. Languages in pediatric epilepsy. Epilepsia. 2009;50:2397–407. doi: 10.1111/j.1528-1167.2009.02199.x. [DOI] [PubMed] [Google Scholar]
- 8.Pal DK, Chaudhury G, Sengupta S, Das T. Social integration of children with epilepsy in rural India. Soc Sci Med. 2002;54:1867–74. doi: 10.1016/s0277-9536(01)00154-x. [DOI] [PubMed] [Google Scholar]
- 9.Pal DK, Chaudhury G, Sengupta S. Predictors of parental adjustment to children's epilepsy in rural India. Child Care Health Dev. 2002;28:295–300. doi: 10.1046/j.1365-2214.2002.00278.x. [DOI] [PubMed] [Google Scholar]
- 10.Austin JL, Dunn DW, Caffrey HM, Perkinsson Harzela KJ, Rose DF. Recurrent seizure and behavioral problem in children with first recognized seizure; a prospective study. Epilepsia. 2002;43:1564–73. doi: 10.1046/j.1528-1157.2002.26002.x. [DOI] [PubMed] [Google Scholar]
- 11.Rutter M, Graham P, Yule WA. Philadelphia: Lippincott; 1970. Neuropsychiatry study in childhood. Clinics in Developmental Medicine; pp. 35–6. [Google Scholar]


