Abstract
Triad of leukoencephalopathy, cerebral calcifications and cysts (LCC) is a recently reported rare disease named ‘Labrune syndrome’ after the first case was reported in 1996 by Labrune et al. Herein, we report a case of a 36-year-old man with mild right-sided weakness and seizures for 5 years. CT of brain revealed extensive calcification involving bilateral basal ganglia, right thalamus and bilateral deep cerebellar nuclei. A supratentorial cystic lesion with blood fluid level was seen in left occipitotemporal region. MRI examination revealed diffuse symmetric white matter hyperintensity suggesting leukoencephalopathy. On follow-up, patient reported improvement in the weakness and no further seizure episodes. However, follow-up of MRI revealed persistence of lesions. Differential diagnosis considered were parasitic infections (hydatid, cysticercosis), Coat's plus disease and causes of diffuse cerebral calcification like Fahr's disease and post-radiotherapy/chemotherapy. Serology for parasitic infections was negative. No history of radiotherapy or chemotherapy in the past could be elicited in the history. Another close differential is Coat's plus disease which can mimic LCC pathologically.
Keywords: Calcification, cerebral cysts, labrune syndrome, leukoencephalopathy, cerebral calcifications and cysts
Introduction
The association of extensive cerebral calcification, white matter changes and cysts is a relatively rare entity first described by Labrune et al., in 1996[1] as LCC (leukoencephalopathy, cerebral calcifications and cysts). We are reporting a new case of LCC and its clinical and neuroradiological findings are discussed with review of literature. About less than 10 cases have been reported so far in the English literature commonly in children and adolescents, and here we report probably the second case of this syndrome in a middle-aged adult.
Case Report
A 36-year-old man was presented with a 5-year-history of simple partial seizures, right upper limb weakness and tremor with mild weakness of right lower limb as well. No other neurological symptoms were seen. General physical and ophthalmological examinations including visual fields were unremarkable. Neurological examination revealed reduced muscle power (4/5) on the right side with mild spasticity.
Hemogram, serum electrolytes, liver function tests and renal function tests were within normal limits. Serological tests for hydatid, toxoplasma, cysticercosis, cryptococcosis, cytomegalovirus and Human immunodeficiency virus (HIV) were negative. CT of brain revealed extensive calcification involving bilateral basal ganglia, right thalamus and bilateral deep cerebellar nuclei [Figure 1a–c]. Symmetric hypodensity in a butterfly pattern was seen involving bilateral cerebral white matter predominantly in the periventricular location. In addition, large rounded cystic lesion was seen in left occipito temporal region with mild chinking of ipsilateral atrium of the lateral ventricle. MRI of brain revealed similar changes. The supratentorial cyst showed mild surrounding edema. There was evidence of blood fluid level in occipito temporal cystic lesion suggesting hemorrhage within the cyst [Figure 2a–d]. There was extensive T2 hyperintensity involving bilateral periventricular white matter with sparing of subcortical U fibers and corpus callosum [Figure 2e]. The calcification seen in CT showed varying signal intensity from T2 hypointensity to T1 hyperintensity on MRI. Calcification usually shows T2 hypointensity but depending on the concentration and hydration of calcium phosphate, T1 shortening can also occur, explaining the varying signal intensity in our case. Patient was started on valproic acid for seizures. Limb weakness improved and had no further episodes of seizures on 6-month-follow-up. MRI after 6 months revealed no further changes.
Figure 1.
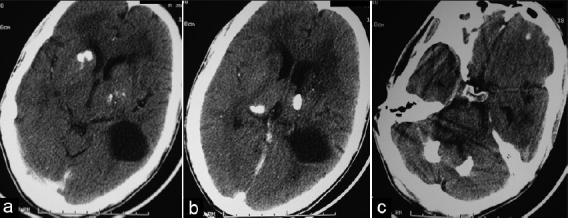
(a, b, c) CT image shows thalamus, basal ganglia and deep cerebellar nuclei calcification and the supratentorial cyst. Note also hypodensity of white matter in B/L frontal region
Figure 2.
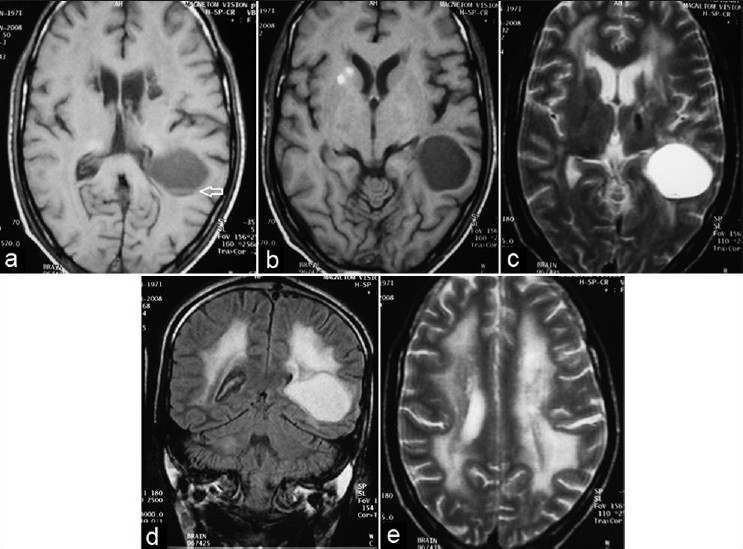
(a and b) T1-weighted MR image through the basal ganglia shows thalamus and basal ganglia calcification and the cyst with mass effect on the atrium of left lateral ventricle showing blood fluid level (arrow) (c) and coronal (d) T2-weighted MR image shows thalami calcification and the cyst with mass effect. Note T2 hyperintensity in B/L frontal white matter with sparing of corpus callosum (e) T2-weighted MR image shows diffuse symmetric T2 hyperintensity involving bilateral periventricular white matter and centrum semiovale
Discussion
LCC was first described in 1996 and is an extremely rare entity. To our best knowledge, only seven to eight cases have been reported in literature. When we encountered a rare association of basal ganglia calcification and white matter changes with supratentorial cyst, we searched the literature. Our case fitted exactly with LCC described by Labrune[1] and Nagae-Poetscher[2] et al. Close differential of parasitic infections like hydatid, cysticercosis and cryptococcosis was kept. In neurocysticercosis, there will be multiple cystic lesions with variable parenchymal calcification.[3] Gelatinous pseudocyst and parenchymal calcification are reported in HIV patients with cryptococcosis.[4] However, no serologic evidence was found for these infections and in addition, leukoencephalopathy is not a described feature of these entities. Basal ganglia calcifications with white matter changes have been described in post-radiotherapy and chemotherapy for malignancies more common in children. Other diseases which show extensive basal ganglia and cerebellar nuclei calcification like Fahr's disease do not have other features. LCC has been described to occur from infancy to adolescence. To our best knowledge, ours is probably the second reported case in a middle-aged adult. Etiopathogenesis of LCC is controversial. Obliterative microangiopathy was found to be the basic abnormality in histopathological examination.[1] It is postulated that cyst formation is due to necrotic process secondary to obliterative microangiopathy and calcification seen is nothing but dystrophic calcification.[5] White matter changes are not due to myelination abnormality but due to changes in water content. Clinical feature reported include convulsions, pyramidal, extrapyramidal and cerebellar features. Progression of the disease is variable. Calcifications are reported predominantly in basal ganglia but can also occur in cerebellum and cerebral cortex. Parenchymal cysts can occur both in cerebral hemispheres and infratentorial compartment. White matter changes are seen predominantly in relation to the cysts and in the periventricular location.[6] Follow-up of MRI after 6 months in our patient demonstrated no progression of imaging features. This is consistent with reported slow progression of the disease and patient was asymptomatic. Similar leukoencephalopathy, cysts and calcification have been reported in few cases in association with Coat's disease called as ‘Coat's plus’.[5] Coat's disease is unilateral retinal telangiectasia with exudation commonly occurring in boys sporadically without systemic features. However, in Coat's plus there is bilateral retinal telangiectasia with exudation along with systemic features in the form of LCC. However, in our case, examination of eyes was normal. Another entity which deserves a special mention is CRMCC-cerebroretinal microangiopathy with calcification and cysts.[7] This includes both LCC and Coat's plus diseases. According to Briggs TA et al., both LCC and Coat's plus represent a continuous spectrum of similar disease with primary pathogenesis being obliterative microangiopathy. However, further studies are needed for establishing this concept.
In conclusion we can say that, even though this triad of CT/MRI findings has not been found in another disease, whether LCC represents a distinct entity or not, needs more number of cases and follow-up with histopathological correlation.
Footnotes
Source of Support: Nil,
Conflict of Interest: Nil.
References
- 1.Labrune P, Lacroix C, Goutieres F, de Laveaucoupet J, Chevalier P, Zerah M, et al. Extensive brain calcifications, leukodystrophy, and formation of parenchymal cysts: A new progressive disorder due to diffuse cerebral microangiopathy. Neurology. 1996;46:1297–301. doi: 10.1212/wnl.46.5.1297. [DOI] [PubMed] [Google Scholar]
- 2.Nagae-Poetscher LM, Bibat G, Philippart M, Rosemberg S, Fatemi A, Lacerda MT, et al. Leukoencephalopathy, cerebral calcifications, and cysts: New observations. Neurology. 2004;62:1206–9. doi: 10.1212/01.wnl.0000119341.59445.cf. [DOI] [PubMed] [Google Scholar]
- 3.Turkulov V, Madle-Samardzija N, Canak G, Vukadinov J, Aleksic-Dordevic M. Clinical and diagnostic approaches to neurocysticercosis. Med Pregl. 2001;54:353–6. [PubMed] [Google Scholar]
- 4.Caldemeyer KS, Mathews VP, Edwards-Brown MK, Smith RR. Central nervous system cryptococcosis: Parenchymal calcification and large gelatinous pseudocysts. AJNR Am J Neuroradiol. 1997;18:107–9. [PMC free article] [PubMed] [Google Scholar]
- 5.Corboy JR, Gault J, Kleinschmidt-DeMasters BK. An adult case of leukoencephalopathy with intracranial calcifications and cysts. Neurology. 2006;67:1890–2. doi: 10.1212/01.wnl.0000244470.06748.18. [DOI] [PubMed] [Google Scholar]
- 6.Sener U, Zorlu Y, Men S, Bayol U, Zanapalioglu U. Leukoencephalopathy, cerebral calcifications, and cysts. AJNR Am J Neuroradiol. 2006;27:200–3. [PMC free article] [PubMed] [Google Scholar]
- 7.Briggs TA, Abdel-Salam GM, Balicki M, Baxter P, Bertini E, Bishop N, et al. Cerebroretinal microangiopathy with calcifications and cysts. Am J Med Genet A. 2008;15:182–90. doi: 10.1002/ajmg.a.32080. [DOI] [PubMed] [Google Scholar]


