Abstract
Background:
Family's expressed emotion has been shown to be predictive of outcome in mental and physical illnesses in a variety of cultural settings. The relationship between caregiver burden and high level of expressed emotions has demonstrated a high level of relapse among the psychiatric patients in the West.
Aim:
The current study explores the relationship between caregivers’ burden and level of expressed emotions by the patients with schizophrenia in Indian setting.
Materials and Methods:
The sample for the study consisted of totally 70 subjects comprising 35 schizophrenic patients and 35 caregivers. The schizophrenic patients who were attending the Day Care Center run by Department of Psychiatric and Neuro Rehabilitation Unit at National Institute of Mental Health and Neuro Sciences (NIMHANS) in Bangalore, India (a tertiary care center) and their primary caregivers were included. Family emotional involvement and criticism scale and The burden assessment schedule were administered to assess the expressed emotions and caregivers’ burden. Carl Pearson Correlation test used to study the relationship between the variables.
Results and Conclusion:
The study highlighted the need for addressing expressed emotion in comprehensive psychosocial intervention plan. More attention should be paid to the needs of the caregivers in order to alleviate their burden in managing mentally ill patients.
Keywords: Burden, caregivers, expressed emotions, Schizophrenia
INTRODUCTION
Expressed emotion (EE) is currently among the most thoroughly investigated psychosocial research constructs in psychiatry.[1] The concept and measurement of the EE within families were developed in the 1960s, initially for use in schizophrenia. They were subsequently used for a number of physical and psychiatric conditions, ranging from dementia to diabetes and Parkinson's disease. The family's EE has been shown to be predictive of outcome in mental and physical illnesses in a variety of cultural settings.
The term EE refers to a global index of particular emotions, attitudes, and behaviors expressed by a relative about a family member diagnosed with schizophrenia.[2] The specific factors that make up the construct of EE are criticism, hostility and emotional over-involvement. Several naturalist studies have demonstrated[3,4] that patients in families having high levels of EE are significantly more likely to experience a clinical relapse than patients residing in households with low levels of EEs.[5–8]
The chronic burden of caregiving to a patient with schizophrenia is likely to generate negative emotions. With the advent of deinstitutionalization, caregivers have increasingly assumed greater responsibility for the care of their mentally ill relatives, with the consequent negative caregiving experience a likely cause of stress manifested in heightened EE. Caring for people with psychosis has been associated with subjective burden and loss, depression, distress, reduced quality of life, lower social support.[9–11] Higher subjective levels of burden and personal stress have been reported by high EE relatives compared with low EE relatives.[12] For many carers, frustration, anger, loneliness and despair are common.[12,13] Bentelspache et al.[14] identified predictors of high EE among caregivers of relatives with schizophrenia based on the stress-coping model. Caregivers’ appraisal of difficult behaviors and dependency were identified as the primary predictor of critical comments and emotional over-involvement, respectively.
Shanmugaiah et al.[15] reported increased EEs in the form of perceived criticism (PC) and emotional involvement (EI) among obsessive compulsive disorder patients compared to normative group. However, there was no significant correlation between PC and EI with Yale-brown obsessive compulsive scale (Y-BOCS) scores, duration of illness and age. Indian studies on the relationship between EEs and burden have been few.
The need for Indian studies therefore seems valid. This paper explores the relationship between caregivers’ burden and level of EEs expressed by the patients with schizophrenia in Indian setting.
MATERIALS AND METHODS
The study sample consisted of totally 70 subjects, out of which 35 were schizophrenic patients attending the day care centre run by Department of Psychiatric and Neuro Rehabilitation Unit at National Institute of Mental Health and Neuro Sciences (NIMHANS) in Bangalore, India (a tertiary care center) and the rest (35) were their primary caregivers. These patients were diagnosed as suffering from schizophrenia according to the criteria laid down by International Classification of Disorder-10. Patients with any co-morbid personality disorder, organic disorders and substance abuse disorder were excluded from the study. Caregivers with psychiatric or neurological disorders and those caring for another relative with psychiatric illness were excluded. The study had a cross-sectional design. Astandard form was used to collect the information on socio-demographic characteristics of patients and their caregivers. Informed consent was obtained from patients and caregivers and they were administered the following tools:
Family emotional involvement and criticism scale (FEICS) by Shields et al.[16] This is a 14-item scale with two subscales: PC and Intensity of EI. Both the scales have seven items each and are scored on Likert scale ranging from 1 to 5. Higher score indicates higher EE by the family members.
The Burden Assessment Schedule (BAS) by Sell et al.[17] The scale has 20 items. Each item is rated on a 3-point scale (not at all, to some extent and very much). The items of the schedule are categorized under five factors, i.e. impact well-being, marital relationships, appreciation for caring, impact on relationships with others, and perceived severity of disease. The scale measures the extent of subjective burden of caregivers and has been proven to have good inter-rater reliability and criterion validity.
RESULTS
The mean age of the patients was 33.5±8.5 years. 54.3% were females and 45.7% were males. Majority (80%) of the patients belonged to Hindu religion. 51.4% were married. The mean duration of illness was 5.8±3.6 years. The mean age of the caregivers was 47.3±13.2 years and duration of caregiving was 5.9±3.6. 48.6% of the caregivers were mothers.
The mean scores of FEICS and BAS
The mean total score of FEICS was 55.6±5.5 and BAS was 42.1±6.9. The mean scores of FEICS PC subscale was 27.9±3.1 and EI subscale was 27.2±3.4. The mean scores of BAS subscales were : i0 mpact well-being 10.3±1.4, marital relationships 2.0±4.1, appreciation for caring 9.3±1.7, impact on relation with others 9.7±1.5, and perceived severity of the disease 10.8±5.2. The mean scores of both the FEICS and BAS revealed high level of EE by caregivers toward patients and high level of subjective burden among the caregivers.
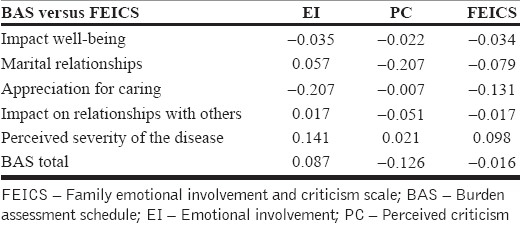
Correlation coefficient between FEICS and BAS
The scores of various domains of BAS [Table 1] were not associated with EI, PC and FEICS total scores. Non-significant association was found between impact well-being, marital relationships, appreciation for caring, impact on relationships with others, perceived severity of disease, and BAS total scores, and EI, PC and FEICS scores [Table 1].
Table 1.
Correlation between FEICS and BAS
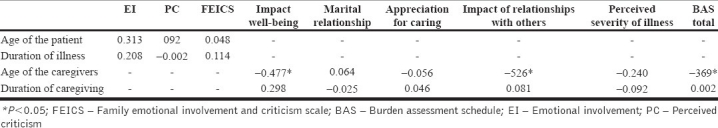
Correlation between FEICS and BAS with background variables of patients and caregivers
The scores of EI, PC and FEICS total were not associated with age and duration of illness of the patients. However, impact well-being (r=–0.477; P<0.05), impact on relationships with others (r=–0.526; P<0.05) and BAS total scores (r=–0.369; P<0.05) were significantly negatively correlated with age of the caregivers. BAS total scores and other subscale scores were found to have a non-significant relationship with the duration of caregiving of the patients [Table 2].
Table 2.
Correlation between FEICS and BAS with background variable
DISCUSSION
Few Indian studies have explored EEs in predicting relapse in schizophrenia.[18–20] However, caregivers’ burden and level of EEs, especially among schizophrenic patients, has not been examined. EE is a concept developed to quantify the family factors in schizophrenic relapse.[17,21,22] The present study found high level of EEs in the form of criticism and EI by the caregivers of schizophrenic patients. The high level of perceived comments and EI seem to indicate significant family pathology. Interestingly, in the current findings, the subjective burden of the caregivers was not associated with the level of expressed emotions among schizophrenic patients. The reasons could be that most of these patients are functional and have been attending to the daycare center regularly. However, caregivers reported higher level of burden on the domain of impact well-being and perceived severity of the disease subscales of BAS. The study of Scazufca and Kuipers[23,24] revealed that EE and burden care are related to each other. The findings suggested that EE and burden of care are more dependent on relatives’ appraisal of the patient's condition than on the patients’ actual deficits. Smith et al. showed that high EE relatives reported higher subjective burden and perceived themselves as coping less effectively than low EE relatives. High EE relatives also report that patients function less well than low EE relatives.[25,26]
This study has certain limitations. The sample for the study is very small and represents one setting and the findings may not be generalized. An adequately controlled group would have made the results more robust. Nevertheless, the study highlighted the need for addressing EE in comprehensive psychosocial intervention plan. The majority of the carers in our sample are parents and special attention should be paid to their needs in order to alleviate the role that such carers have taken on. The fact that EE and burden are lined makes it easier to identify which families might benefit most from psychosocial interventions. Intervention programs must focus on impaired patient's functioning, and the families’ ability to negotiate about these aspects might be valuable in improving carers’ burden and care.[23,24,27] The measure of burden care and EE are dependent on caregivers’ appraisal of the patient condition than on their actual deficits. Hence, understanding the caregivers’ burden is crucial in reducing the expressed emotions on patients is curial in reducing the relapses.[28]
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Kante J. Expressed emotions in families. Hosp Comm Psych. 1987;38:374–80. doi: 10.1176/ps.38.4.374. [DOI] [PubMed] [Google Scholar]
- 2.Brown G. The discovery of expressed emotion: Induction or deduction? In: Leff J, Vaughn C, editors. Expressed emotion in families. New York: Guilford Press; 1985. [Google Scholar]
- 3.Brown G, Birley L, Wing JK. Influence of family life on the course of schizophrenia disorders: A replication. Br J Psych. 1972;121:241–58. doi: 10.1192/bjp.121.3.241. [DOI] [PubMed] [Google Scholar]
- 4.Karno M, Jenkins JH, de la Selva A, Santana F, Telles C, Lopez S, et al. Expressed emotion and schizophrenic outcome among Mexican American families. J Neurol Mov Dis. 1987;175:143–51. doi: 10.1097/00005053-198703000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Fallon PH, Boyd JI, McGill CW. New York: Guilford Press; 1984. Family care schizophrenia: A problem solving approach to the treatment of mental illness. [Google Scholar]
- 6.Moline BA, Singh S, Morris A, Meltzer H. Family expressed emotion and relapse in schizophrenia in 24 urban American patients. Am Psychol. 1987;142:1079–81. doi: 10.1176/ajp.142.9.1078. [DOI] [PubMed] [Google Scholar]
- 7.Leff JP, Wig NN, Ghosh A, Bedi H, Menon DK, Kuipers L, et al. Expressed emotion and schizophrenia in North India III: Influence of relatives expressed emotion on the course of schizophrenia in Chandigarh. Br J Psychol. 1987;151:166–73. doi: 10.1192/bjp.151.2.166. [DOI] [PubMed] [Google Scholar]
- 8.Mintz L, Liberman R, Miklowitz DJ, Mintz J. Expressed emotion: A call for partnership among relatives, patients and professionals. Schizo Bull. 1987;13:227–35. doi: 10.1093/schbul/13.2.227. [DOI] [PubMed] [Google Scholar]
- 9.Foldemo A, Gullberg M, Ek AC, Bogren L. Quality of life and burden in parents of outpatients with schizophrenia. Social Psych Epi. 2005;40:133–8. doi: 10.1007/s00127-005-0853-x. [DOI] [PubMed] [Google Scholar]
- 10.Magliano L, Fiorillo A, De Rosa C, Maj M. Family burden and social network in schizophrenia vs.physical diseases: Preliminary results from an Italian national study. Acta Psychitr Scan. 2006;113:60–3. doi: 10.1111/j.1600-0447.2005.00719.x. [DOI] [PubMed] [Google Scholar]
- 11.Patterson P, Birchwood M, Cochrane R. Expressed emotion as an adaptation to loss: Prospective study in first episode psychosis. Br J Psycho. 2005;187:59–64. doi: 10.1192/bjp.187.48.s59. [DOI] [PubMed] [Google Scholar]
- 12.Smith J, Birchwood M, Cochrane R, George S. The needs of high and low expressed emotions families: A normative approach. Soci Psych Psych Epid. 1993;28:116–29. doi: 10.1007/BF00797827. [DOI] [PubMed] [Google Scholar]
- 13.Potasznik H, Nelson G. Stress and social support: The burden experienced by the family of a mentally ill person. Am J Commun Psychol. 1984;12:589–607. doi: 10.1007/BF00897214. [DOI] [PubMed] [Google Scholar]
- 14.Bentelspacher C, Chitran S, Abdul R, Marziyana B. Coping and adaptation patterns among Chinese, Indian and Malay families caring for a mentally ill relative: Families in Societies. J Cont Hum Serv. 1994;75:287–94. [Google Scholar]
- 15.Shanmugaiah A, Varghese M, Khanna S. Expressed emotion in obsessive compulsive disorder. Indian J Psychol. 2002;44:14–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Shields C, Franks P, Harp JJ, McDaniel SH, Campbell TI. Development of family emotional involvement criticism scale (FEICS): A self-report scale to measure expressed emotion. J Marital Fam Ther. 1992;18:395–407. [Google Scholar]
- 17.Sell H, Tara R, Padmavathi R, Kumar S. Series, 27, WHO-ROSA, New Delhi: 1998. Burden Assessment Scale. [Google Scholar]
- 18.Chan B. Negative caregiving experience: A predictor of high expressed emotion among caregivers of relatives with schizophrenia. Soc Work Mental Health. 2010;8:375–97. [Google Scholar]
- 19.Wig NN, Menon DK, Bedi H, Ghosh A, Kuipers L, Leff JA, et al. Expressed emotion and schizophrenia in north India, II: Distribution of expressed emotion components among relatives of schizophrenic patients in Aarhus and Chandigarh. Br J Psychol. 1987;151:160–5. doi: 10.1192/bjp.151.2.160. [DOI] [PubMed] [Google Scholar]
- 20.Wig NN, Menon DK, Bedi H, Ghosh A, Kuipers L, Leff JA, et al. Expressed emotion and schizophrenia in North India- I: Cross-cultural transfer of rating of relatives’ expressed emotion. Br J Psychol. 1987;151:160–5. doi: 10.1192/bjp.151.2.156. [DOI] [PubMed] [Google Scholar]
- 21.Vaughan K, Doyle M, McConaghy N. The relationship between relative's expressed emotion and schizophrenic relapse: An Australian replication. Soc Psychol Psych Epidemiol. 1992;27:10–5. doi: 10.1007/BF00788950. [DOI] [PubMed] [Google Scholar]
- 22.Warner R, Atkinson M. The relationship between schizophrenic patient’ perceptions of their parents and course of their illness. Br J Psychol. 1998;153:344–5. doi: 10.1192/bjp.153.3.344. [DOI] [PubMed] [Google Scholar]
- 23.Parker G, Johnson P, Hayward L. Parental expressed emotions as predictor of schizophrenic relapse. Arch Gen Psychol. 1998;4:806–13. doi: 10.1001/archpsyc.1988.01800330030003. [DOI] [PubMed] [Google Scholar]
- 24.Scazufca M, Kuipers E. Coping strategies in relatives of people with schizophrenia before and after psychiatric admission. Br J Psychol. 1999;174:154–60. doi: 10.1192/bjp.174.2.154. [DOI] [PubMed] [Google Scholar]
- 25.Scazufca M, Kuipers E. Links between expressed emotion and burden of care in relatives of patients with schizophrenia. Br J Psychol. 1996;168:580–8. doi: 10.1192/bjp.168.5.580. [DOI] [PubMed] [Google Scholar]
- 26.Barrowclough C, Tarrier M. Social functioning in schizophrenic patients: The effects of expressed emotion and family intervention. Soc Psych Psychi Epi. 1990;25:125–9. doi: 10.1007/BF00782739. [DOI] [PubMed] [Google Scholar]
- 27.Lawton MP, Kleban MH, Moss M, Rovine M, Glicksman A. Measuring caregiving appraisal. J Gerontol. 1989;44:61–71. doi: 10.1093/geronj/44.3.p61. [DOI] [PubMed] [Google Scholar]
- 28.Otsuka T, Nakane Y, Ohta Y. Symptoms and social adjustment of Schizophrenia patients as evaluated by family members. Acta Psychiatr Scan. 1994;89:111–1. doi: 10.1111/j.1600-0447.1994.tb01496.x. [DOI] [PubMed] [Google Scholar]


