Abstract
Context:
Carotid intima-media thickness (CIMT) and apolipoproteins have been found as a risk factor for ischemic stroke
Objective:
The objective was to study the carotid intima-media thickness, apolipoproteins, and their relation in patients of ischemic stroke in central rural India.
Settings and Design:
A cross-sectional study was performed in a rural hospital in central India.
Materials and Methods:
In all patients of ischemic stroke proven by computerized tomography (CT), CIMT, apolipoprotein A-I (ApoA-I), and apolipoprotein B(ApoB) were measured.
Statistical Analysis Used:
We used Student's t-test to compare means, a chi-square test to compare proportions, and a Mann-Whitney test to compare medians. A P value <0.05 was considered significant.
Results:
The mean age of our study population (N=106) was 61 years. The mean CIMT was 0.83 mm ranging from a minimum of 0.45 mm to a maximum of 1.096 mm. Mean CIMT was significantly higher than expected 0.67 values, which was calculated according to the age of the study population. The association of decreased ApoA-I < 100 mg/dl and increased ApoB > 90 mg/dl with CIMT > 0.7 mm was statistically significant with P<0.001.
Conclusions:
The CIMT in computerized tomography-proven ischemic stroke was significantly higher than expected for the age of the study population. The relation of decreased ApoA-I and increased ApoB with CIMT > 0.7 mm was also statistically significant.
Keywords: Atherosclerosis, apolipoproteins, carotid arteries, Carotid intima-media thickness, stroke
Introduction
Stroke is one of the leading causes of morbidity and mortality in the world today.[1] There has been a constant effort on the part of medical researchers to analyze this problem and search for factors that aid in its prevention. Carotid intima-media thickness (CIMT) measurement has emerged as one of the noninvasive methods of choice for determining preclinical (asymptomatic) atherosclerotic changes.[2,3] CIMT is a marker of subclinical atherosclerosis, a strong predictor of subsequent cardiovascular and cerebrovascular morbidity.[4,5] Measurement of CIMT, the anatomic extent of atherosclerosis and its progression helps in identifying high risk subjects, who are candidates of primary prevention.
The development of sonography technology has allowed the noninvasive evaluation of atherosclerosis in the carotid arteries. The initial manifestation of carotid atherosclerosis is characterized by a subtle increase in vascular IMT, the progression of which leads to plaque formation and vascular narrowing. Reflecting systemic atherosclerosis, increased CIMT is associated with a higher risk for stroke.
Early detection of atherosclerosis is desirable for the primary and or secondary prevention of atherosclerotic events like stroke and myocardial infarction. Similarly, the risk of stroke increases with increasing CMIT.
Atherosclerosis is the leading cause of occlusive arterial disease in patients over 40 years old; the highest incidence occurs in the sixth and seventh decades of life. The strongest predictors of CIMT, after adjusting for age and sex, were total cholesterol and smoking status besides ethnicity (African American versus white).[2,6] Apolipoprotein B (ApoB) and apolipoprotein A-I (ApoA-I) are identified as risk factors for cardiovascular and possibly cerebrovascular diseases. It has been documented in certain studies that ApoA-I is inversely related to the CIMT; this is specifically significant in cases of documented cerebrovascular diseases. An increase in ApoB and a decrease in ApoA-I indicate an increased risk for atherosclerotic complications.[7]
Apolipoproteins are good predictors of subsequent cerebrovascular events, and improve on predictions by conventional risk factors alone. Their use is simple and accurate and could be included in routine screening of cerebrovascular status.
Thus, the present study was carried out to measure CIMT and ApoB/ApoA-I ratio and demonstrate the correlation between them in patients of more than 18 years of age with ischemic stroke proven by computerized tomography (CT) in a resource-constrained setting in central rural India.
Materials and Methods
Ethics
The study was approved by the ethics committee of Mahatma Gandhi Institute of Medical Sciences (IRB00003623). We obtained a written informed consent from all study participants before enrolling them in the study.
Setting
We did this study in the department of Medicine and Radiology at Kasturba Hospital and Mahatma Gandhi Institute of Medical Sciences (MGIMS), Sevagram. Kasturba Hospital is a 720-bed rural teaching hospital of central India affiliated to MGIMS. Every year this hospital provides care to about 400,000 outpatients and 40,000 inpatients. In an inpatient setting, physicians typically order CT scan of brain estimation in patients clinically judged to have stroke, in all patients who come for treatment. We enrolled patients from inpatient settings in this study.
Patient enrollment
Since 1 May 2006 to 30 December 2007, we enrolled all consecutive inpatients with admission diagnosis of ischemic stroke proven by CT of more than 18 years of age in a cross-sectional observational study.
The diagnosis of ischemic stroke was based on the clinical profile and confirmed by CT as defined by ASA/AHA. Ischemic stroke was defined as an abrupt onset, nonconvulsive, focal neurological deficit probably vascular in origin lasting for more than 24 hours on the clinical profile and in neuroimaging studies demonstrating a recent, appropriately located ischemic lesion on CT scan.[8] Criteria for exclusion were recurrent stroke, normal CT scan of brain, CT scan showed hemorrhage, CT scan not feasible, and patients not consenting to the study.
Measurements
Baseline characteristics and clinical data were recorded for all patients. All patients received the standard line of management for stroke in accordance with ASA/AHA guidelines.
Measurement of carotid intima-media thickness
The measurements of CIMT were obtained by using a Logic Pro 2000 MDMR3 ultrasound system, equipped with a 7.5 MHz real-time, linear-array transducer B-mode scanner to examine the patient's ultrasound images of the common carotid artery, carotid bifurcation, and the internal carotid artery after admission in all enrolled patients’ CT scan-proven stroke carotid arteries. A single experienced operator carried out all ultrasonographic investigations.
Patients were asked to lie supine with the neck extended in a slightly lateral rotation. Then carotid artery and the lumen of the carotid artery beneath the surface of the neck were scanned. CIMT was defined as the distance between the leading edge of the first bright line (lumen intima interface) and the leading edge of the second bright line (media-adventitia interface) of the posterior (far) wall of the vessel and for the anterior (near) wall, between the trailing edge of the first bright line and the trailing edge of the second bright line. Three sites were selected in each carotid artery. CIMT was measured on the frozen frame of a suitable longitudinal image with the image magnified to achieve a higher resolution of detail. The first reading was taken 1 cm proximal to the carotid bulb while the second at a maximum diameter of the carotid bulb. The third reading was taken 1 cm distal to the carotid bulb along the internal carotid artery. For all three sites, both near wall and far wall measurements were taken. The average of each artery was computed taking into all six readings as (A+B+C+D+E+F)/6, where A= far wall of CCA, B= near wall of CCA, C= far wall of carotid bulb, D= near wall of carotid bulb, E= far wall of internal carotid artery (ICA), F= near wall of ICA.
The CIMT expected for age of the patient was calculated using the formula CIMT = (0.009×Age) + 0.116. The mean expected CIMT was 0.67 mm calculated according to the age of the study patients. Therefore CIMT > 0.7 mm is considered as the abnormal value.
Measurement of biochemical markers
Sera from all enrolled patients were collected for estimation of ApoB, ApoA-I on admission. The collected sera were stored at –20°c till they were tested by serologist who was unaware of the clinical data of the patients. ApoB, ApoA-I estimation was done on a fully automated BN-nephelometry system. Levels of ApoA-I were said to be low if they were < 100 mg/dl and of Apo B were said to be high if they were more than 90 mg/dl. The ApoB/ApoA-I ratio was considered to be high if it was > or equal to 0.8.
Venous blood samples drawn after a 12-hour overnight fast were immediately refrigerated and transported within 6 hours to central laboratory of hospital for total cholesterol, high-density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), triglycerides measurement by standard enzymatic tests. Levels were considered abnormal if total cholesterol > 200 mg/dl, LDL-C >130 mg/dl ,triglycerides >150mg/dl, and HDL-C < 40 mg/dl respectively. Random glucose and serum creatinine were also obtained on day 1 in all enrolled participants. During the hospital stay, patients were monitored daily for any complications.
We screened 207 consecutive patients of stroke for our study, between 1 May 2006 and 30 December and enrolled 106 patients of stroke who fulfilled our study inclusion criteria.
Statistical analysis
We entered the data electronically by Microsoft Excel and analyzed by STATA software (Version 10, Stata Corporation, Texas, USA). We analyzed normally distributed continuous variables by Student's t-test, proportions by a chi-square test, and continuous variables with skewed distribution by a Mann-Whitney test. The association of CIMT and apolipoproteins was calculated by the correlation coefficient.
Results
We used STROBE (Strengthening the reporting of observational studies in epidemiology) statement to report this study. We screened 207 consecutive patients of clinically suspected stroke and included 106 patients whose diagnosis was confirmed as an ischemic stroke by CT [Figure 1].
Figure 1.
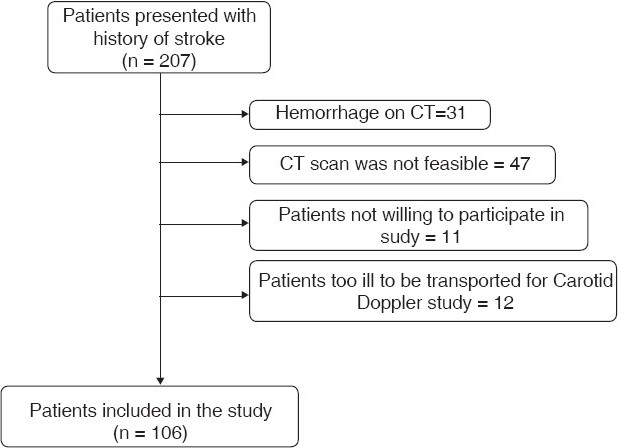
Study profile of the patients in the study
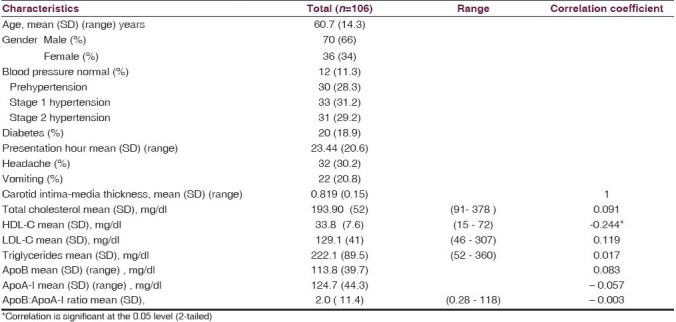
The baseline characteristics were recorded with respect to clinical profile, risk factor profile, and biochemical profile. The mean age of the patients was 61 years and 66% were male. The patients’ population had several high risk features, including prehypertension (28% of patients), stage 1 hypertension (31 % of patients), stage 2 hypertension (29.2% of patients), and diabetes (19% of patients). The mean total cholesterol was 193.90 mg/dl, mean HDL-C was 33.8 mg/dl, mean LDL-C was 129.1 mg/dl, and mean triglycerides’ value was 222.1 mg/dl. The mean time for presentation to enrolment was 23.4 hours. The correlation between CIMT and HDL-C was found to be significant (Pearson correlation coefficient 0.244) at the 0.05 level (two-tailed) but there was no significant correlation between CIMT and ApoB , ApoA-I, ApoB/ApoA-I ratio, total cholesterol, LDL-C, and triglycerides [Table 1].
Table 1.
Baseline characteristics of study patients
Carotid intima-media thickness
The mean CIMT was 0.83 mm ranging from a minimum of 0.45 mm to a maximum of 1.096 mm. The mean expected CIMT was 0.67 mm calculated to the age of study patients [Table 2]. The difference between the measured and the expected CIMT of the study patients for their age was significant with P < 0.005. Mean CIMT in male patients was 0.82 + 0.13 (95% CI, 0.79- 0.85) while in female patients it was 0.81 + 0.16 (95% CI, 0.75- 0.87). There was no statistical difference in mean CIMT in males and females (P= 0.75) [Table 3 and Figure 2]. There was statistically significant linear correlation of the intima-media thickness with age.
Table 2.
Relation between measured and expected carotid intima-media thickness of the study population
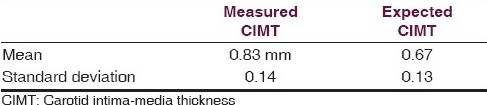
Table 3.
Carotid intima-media thickness of the study population
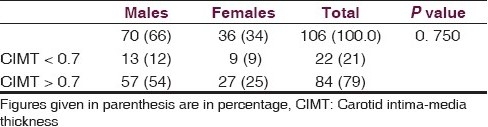
Figure 2.
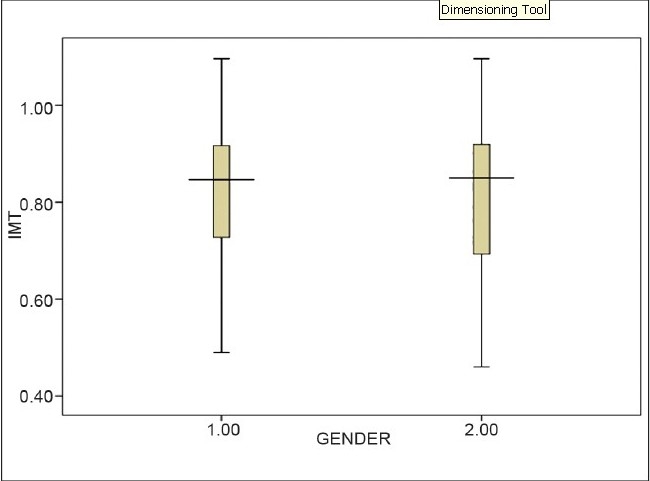
Box plot showing the relationship of carotid intima-media thickness in study patients according to gender
Apolipoproteins
The mean ApoB was 113.8 mg/dl and it was > 90 mg/dl in 75% of patients, of whom 69 patients (87%) had increased CIMT > 0.7 mm while 15 patients with normal ApoB < 90 mg/dl had increased CIMT. The association of ApoB > 90 mg/dl with increased CIMT > 0.7 mm was significant at 5% level with P<0.001. Thus patients with increased ApoB have increased CIMT and this association was significant [Table 4].
Table 4.
Relation of carotid intima-media thickness with ApoB, ApoA-I and ApoB/ApoA-I ratio
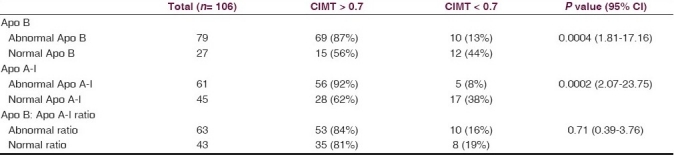
Of the 61 patients (58%) with abnormal ApoA-I < 100 mg/dl, 56 patients (92%) had increased CIMT > 0.7 mm while 28 patients (62%), with normal ApoA-I had increased CIMT > 0.7 mm. The association of decreased ApoA-I with CIMT > 0.7 mm was statistically significant with P<0.001. Thus patients with decreased ApoA-I had increased CIMT and this association was significant [Table 4].
There was an increased ApoB:ApoA-I ratio > 0.8 in 63 patients (59%), of whom 53 patients (84%) had increased CIMT > 0.7 mm while 35 patients (81%), with a normal ApoB:ApoA-I ratio < 0.8, had increased CIMT > 0.7 mm. The association of the ApoB:ApoA-I ratio > 0.8 with increased CIMT > 0.7 mm was not significant statistically (P=0.71). Though 84% of patients with a normal ApoB:ApoA-I ratio also had increased CIMT, the association was not statistically significant [Table 4].
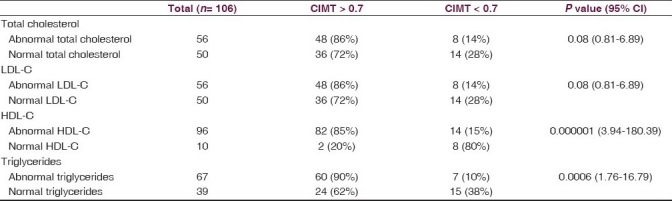
Of the 56 patients (53%) with abnormal total cholesterol, 48 patients (86%) had CIMT > 0.7 mm while 36 patients (72%), with normal cholesterol had CIMT > 0.7 mm. The association of abnormal total cholesterol with CIMT > 0.7 mm was not statistically significant (P=0.08 with 95% CI 0.81-6.89). Similarly statistically significant association was not found with increased LDL-C (P=0.08 with 95% CI 0.81-6.89) but the association of abnormal triglycerides (P=0.0006 with 95% CI 1.76-16.79) and HDL-C < 40 mg/dl (P= 0.000001 with 95% CI 3.94-180.39) with increased CIMT > 0.7 mm compared to those with normal levels of triglycerides and HDL-C was statistically significant (P<0.001) [Table 5].
Table 5.
Relation of carotid intima-media thickness with total cholesterol, LDL-C, HDL-C and triglycerides
Discussion
In the present study, the most significant finding we observed was that there is a statistically significant increase in the intimal-medial thickness of common carotid artery in patients with CT-proven ischemic stroke. A statistically significant association was found between the increase in the CIMT in patients with ischemic stroke and abnormal increased ApoB, decreased ApoA-I levels. Our data showed that the ApoB:ApoA-I ratio was not associated with stroke and with the change in CIMT ratio in patients of ischemic stroke.
Chien et al, found similar results in a community-based cohort study composed of 2,190 participants free of cardiovascular disease at baseline. A total of 94 cases of stroke were documented during the median 10.5-year follow-up. The multivariate RRs associated with a change of one standard deviation of maximal CIMT were 1.47 (95% CI, 1.28–1.69) and for internal carotid IMT were 1.52 (95% CI, 1.31–1.76) for stroke. The study reported a significant association between CIMT and incidence of stroke in Chinese adults,[9] whereas in a case- control study, which was aimed to assess association of increased CIMT and plaque score with acute ischemic stroke in patients with type 2 diabetes, it was found that CIMT and plaque scores in patients with diabetes and acute ischemic stroke were significantly greater than in patients with diabetes who were stroke-free. The crude odds ratios suggested that CIMT and plaque score are risk factors for acute ischemic stroke in patients with type 2 diabetes. Sex, current smoking habit, history of hypertension, and HDL-C levels differed significantly between the case and control groups. However, when after adjustment for cerebrovascular risk factors, CIMT and plaque score did not remain significantly associated with acute ischemic stroke.[10]
Cupini et al, concluded after a multinomial logistic regression procedure from a case-control study on 292 adult patients with an acute first-ever ischemic stroke that CIMT values and atrial fibrillation are the only independent factors able to discriminate between lacunar and nonlacunar patients.[11]
In another cohort study 1,289 Japanese men aged 60-74 years without a previous stroke or coronary heart disease have been followed-up for 4.5-years and examined for the association of CIMT and plaque characteristics with the risk of stroke. The combination of CIMT and internal carotid IMT as assessed by ultrasonography was found as a better predictor of the risk of stroke than was CIMT alone.[12]
Brenner et al, reported in a cross-sectional study on 470 white ischemic stroke patients that measured CIMT, osteopontin (OPN)-443C allele, and monocyte chemoattractant protein-1 (MCP-1) were associated with increased CIMT. The OPN and MCP-1 genes, coding for two cytokines with known roles in atherosclerosis, may contribute to increase CIMT.[13]
In this study, we did not found an increased ApoB:ApoA-I ratio in patients with ischemic stroke. Lima et al, also reported in their study that the ApoB:ApoA-I ratio was important for identifying an increased trend for coronary and cerebral atherosclerosis, in spite of the fact that heterogeneous distribution of ApoB and ApoA-Ilevels was observed among the different groups. In spite of the increased trend for the ApoB/ApoA-I ratio in ischemic stroke and CAD groups, the studied variables cannot be considered in an isolated way and additional studies are required to extend the evaluation of the ApoB/apoA-I ratio in different populations and in different types of atherosclerosis events.[14] In several studies, similar results have been seen with either only ApoB or ApoA-I or their ratio being found significant, while Angelantonio et al, concluded from their study that lipid assessment in vascular disease can be simplified by measurement of either total and HDL-C levels or apolipoproteins without the need to fast and without regard to triglyceride as they found that hazard ratios for ischemic stroke were 1.02 (95% CI, 0.94-1.11) with triglyceride, 0.93 (95% CI, 0.84-1.02) with HDL-C, and 1.12 (95% CI, 1.04-1.20) with non-HDL-C.[15] Chien et al, found in a community-based cohort consisting of 3602 adults in the Taiwan, after multiple Cox proportional hazard regression models controlling for age and sex, that individuals with ApoA-I at the highest quartile were more likely to have a stroke event than those at the lowest quartile level (relative risk [RR]_2.02, P for trend_0.010). The corresponding risk of stroke predicted by ApoB was also significant (RR_1.88, P for trend_0.020). After adjustment for age, sex, hypertension, and diabetes status, the interaction between hypertension and ApoA-I level remained significant in predicting stroke events in men but not in women (RR_1.71, P_0.033 in men; RR_2.29, P_0.071 in women).[16]
Gardener et al, reported that ApoB was associated with risk of plaque (OR per SD = 1.29, 95% CI 1.03-1.60), ApoA-1 was associated with a decrease in multiple plaques (OR per SD = 0.76, 95% CI 0.60-0.97), while lipoprotein A was associated with an increased risk of multiple plaques (OR per SD = 1.31, 95% CI 1.03-1.66). The ApoB/ApoA-I ratio had the strongest relation with carotid plaque (OR per SD = 1.35, 95% CI 1.08-1.69). Among the common lipid parameters, LDL-C has the strongest relation with carotid plaque. Other lipid precursor proteins such as ApoB and ApoA-I may be stronger predictors of subclinical atherosclerosis, however, and better targets for treatment to reduce plaque formation and risk of cerebrovascular disease.[17]
We found that patients with increased ApoB > 90 mg/dl and decreased ApoA-I < 100 mg/dl have increased CIMT more than 0.7 mm significant at 5% level of significance with P<0.001. We also found statistically significant (P<0.001) association between triglycerides and low HDL-C < 40 mg/dl with increased CIMT > 0.7 mm compared to those with normal levels but the association was not statistically significant with total cholesterol >200 mg/dl and increased LDL-C > 130 mg/dl with increased CIMT > 0.7 mm.
Thus for the present study we concluded that apolipoproteins are good predictor of subsequent cerebrovascular events, and improves on predictions by conventional risk factors alone. It is simple and accurate and could be included in routine screening of high risk patients.
CIMT has been recently recognized as a surrogate marker for evaluating therapeutic interventions in atherosclerotic disease. Therefore, to prevent ischemic stroke in high risk patients, control of hypertension, hyperglycemia, smoking, and low HDL-C, together with monitoring of CIMT, may be important.
Limitations of our study were that it was a cross-sectional study, and it had an inherent selection bias as CIMT was measured only in patients of known ischemic stroke and did not include age-related healthy controls. It was not population based, as all participants were members of a single healthcare scheme, but it did represent a typical community population. In future, the relationship between CIMT and ischemic stroke must be examined in all patients with strokes (TIA, acute, and chronic) and without strokes (healthy controls).
The study had few strengths as well. Our study is one of the few studies available demonstrating the association of the CIMT with apolipoproteins in patients of ischemic stroke in central rural India. The interobserver variability CIMT was low (coefficient of variation 3%).[18] Therapeutic interventions with antihypertensive drugs, control of hyperglycemia, lipid-lowering agents, and life style modification in high risk patients can slow the progression of CIMT.
Conclusion
In patients with CT-proven ischemic stroke, there is an increase in intima-media thickness of common carotid-internal artery compared to the CIMT expected for the age, with increased apolipoprotein B and decreased apolipoprotein A-I.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Yang X, So WY, Kong AP, Ho CS, Lam CW, Stevens RJ, et al. Development and validation of stroke risk equation for Hong Kong Chinese patients with type 2 diabetes: The Hong Kong Diabetes Registry. Diabetes Care. 2007;30:65–70. doi: 10.2337/dc06-1273. [DOI] [PubMed] [Google Scholar]
- 2.Lanktree MB, Hegele RA, Yusuf S, Anand SS. Multi-ethnic genetic association study of carotid intima-media thickness using a targeted cardiovascular SNP microarray. Stroke. 2009;40:3173–9. doi: 10.1161/STROKEAHA.109.556563. [DOI] [PubMed] [Google Scholar]
- 3.Prati P, Tosetto A, Vanuzzo D, Bader G, Casaroli M, Canciani L, et al. Carotid intima media thickness and plaques can predict the occurrence of ischemic cerebrovascular events. Stroke. 2008;39:2470–6. doi: 10.1161/STROKEAHA.107.511584. [DOI] [PubMed] [Google Scholar]
- 4.Johnsen SH, Mathiesen EB, Joakimsen O, Stensland E, Wilsgaard T, Lochen ML, et al. Carotid atherosclerosis is a stronger predictor of myocardial infarction in women than in men: A 6-year follow-up study of 6226 persons: The Tromso Study. Stroke. 2007;38:2873–80. doi: 10.1161/STROKEAHA.107.487264. [DOI] [PubMed] [Google Scholar]
- 5.Amato M, Montorsi P, Ravani A, Oldani E, Galli S, Ravagnani PM, et al. Carotid intima-media thickness by B-mode ultrasound as surrogate of coronary atherosclerosis: Correlation with quantitative coronary angiography and coronary intravascular ultrasound findings. Eur Heart J. 2007;28:2094–101. doi: 10.1093/eurheartj/ehm244. [DOI] [PubMed] [Google Scholar]
- 6.Miwa K, Hoshi T, Hougaku H, Tanaka M, Furukado S, Abe Y, et al. Silent cerebral infarction is associated with incident stroke and TIA independent of carotid intima-media thickness. Intern Med. 2010;49:817–22. doi: 10.2169/internalmedicine.49.3211. [DOI] [PubMed] [Google Scholar]
- 7.Benn M, Nordestgaard BG, Jensen GB, Tybjaerg-Hansen A. Improving prediction of ischemic cardiovascular disease in the general population using apolipoprotein B: The Copenhagen City Heart Study. Arterioscler Thromb Vasc Biol. 2007;27:661–70. doi: 10.1161/01.ATV.0000255580.73689.8e. [DOI] [PubMed] [Google Scholar]
- 8.Kidwell CS, Warach S. Acute ischemic cerebrovascular syndrome: Diagnostic criteria. Stroke. 2003;34:2995–8. doi: 10.1161/01.STR.0000098902.69855.A9. [DOI] [PubMed] [Google Scholar]
- 9.Chien KL, Su TC, Jeng JS, Hsu HC, Chang WT, Chen MF, et al. Carotid artery intima-media thickness, carotid plaque and coronary heart disease and stroke in Chinese. PLoS One. 2008;3:e3435. doi: 10.1371/journal.pone.0003435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee EJ, Kim HJ, Bae JM, Kim JC, Han HJ, Park CS, et al. Relevance of common carotid intima-media thickness and carotid plaque as risk factors for ischemic stroke in patients with type 2 diabetes mellitus. AJNR Am J Neuroradiol. 2007;28:916–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Cupini LM, Pasqualetti P, Diomedi M, Vernieri F, Silvestrini M, Rizzato B, et al. Carotid artery intima-media thickness and lacunar versus nonlacunar infarcts. Stroke. 2002;33:689–94. doi: 10.1161/hs0302.103661. [DOI] [PubMed] [Google Scholar]
- 12.Kitamura A, Iso H, Imano H, Ohira T, Okada T, Sato S, et al. Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke. 2004;35:2788–94. doi: 10.1161/01.STR.0000147723.52033.9e. [DOI] [PubMed] [Google Scholar]
- 13.Brenner D, Labreuche J, Touboul PJ, Schmidt-Petersen K, Poirier O, Perret C, et al. Cytokine polymorphisms associated with carotid intima-media thickness in stroke patients. Stroke. 2006;37:1691–6. doi: 10.1161/01.STR.0000226565.76113.6c. [DOI] [PubMed] [Google Scholar]
- 14.Lima LM, Carvalho MG, Sabino Ade P, Mota AP, Fernandes AP, Sousa MO. Apo B/Apo A-I ratio in central and peripheral arterial diseases. Arq Bras Endocrinol Metabol. 2007;51:1160–5. doi: 10.1590/s0004-27302007000700020. [DOI] [PubMed] [Google Scholar]
- 15.Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Emerging Risk Factors Collaboration. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009;302:1993–2000. doi: 10.1001/jama.2009.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chien KL, Sung FC, Hsu HC, Su TC, Lin RS, Lee YT. Apolipoprotein A-I and B and stroke events in a community-based cohort in Taiwan: Report of the Chin-Shan Community Cardiovascular Study. Stroke. 2002;33:39–44. doi: 10.1161/hs0102.101626. [DOI] [PubMed] [Google Scholar]
- 17.Gardener H, Della Morte D, Elkind MS, Sacco RL, Rundek T. Lipids and carotid plaque in the Northern Manhattan Study (NOMAS) BMC Cardiovasc Disord. 2009;9:55. doi: 10.1186/1471-2261-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Depairon M, Tutta P, van Melle G, Hayoz D, Kappenberger L, Darioli R. Reference values of intima-medial thickness of carotid and femoral arteries in subjects aged 20 to 60 years and without cardiovascular risk factors. Arch Mal Coeur Vaiss. 2000;93:721–6. [PubMed] [Google Scholar]


