Abstract
Background:
Screening at the community level will provide keys to promoting health and preventing diseases at the community level and serve as the fulcrum for timely detection and intervention. This study aims to assess the prevalence and nature of mental disorder among the general population using the patient health questionnaire (PHQ). It also compares the use of PHQ and GHQ as general screening tools for mental disorders.
Materials and Methods:
This community-based study is cross sectional in design. Multistage sampling technique was used to obtain a representative sample of the communities. The PHQ and GHQ-12 questionnaires were concurrently administered by health care workers that were nondoctors to screen for psychiatric symptoms.
Results:
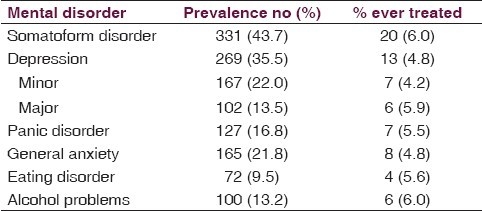
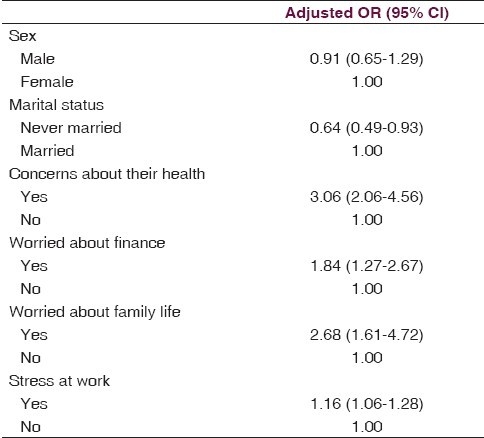
A total of 758 participants took part in the study, 496 (65.4%) of the subjects had a form of psychopathology or the other using PHQ and 143 (18.9%) using GHQ questionnaire (χ2 = 20.92, P = 0.000). Three hundred and thirty one subjects (43.7%) met the criteria for Somatoform disorder but 6.0% ever treated at PHC, 269 (35.5%) for depression and 4.8% ever treated, 127 (16.8%) for panic disorder and 5.5% ever treated, while 165 (21.8%) for general anxiety and 4.8% ever treated. Predictors of psychopathology were individuals who were singles (OR = 0.64, CI = 0.49–0.93) concerns about their health (OR = 3.06, CI = 2.06–4.56), worried about finance (OR = 1.84, CI = 1.27–2.67), worried about family life (OR = 2.68, CI = 1.61–4.72), and stressed at work (OR = 1.16, CI = 1.06–1.28).
Conclusion:
There is a high prevalence of psychopathology at the community level in this African population and few had ever been treated. PHQ as a general screening tool has a higher false-positive value compared to GHQ when used by nondoctors. PHQ should be used as an instrument to screen for specific mental disorders rather than a general screening tool for psychiatric morbidity at the community level.
Keywords: Assessment, mental disorders, patient health questionnaire, screening tool, western Nigeria
Introduction
Mental disorders have been estimated to present in at least 20% of primary care patient yet they seems to go undetected and untreated in 50%–75% of cases.[1–2] The majority of patients with mental disorders are cared for in the primary care rather than in the mental health sector. Four disorders—depression, anxiety, somatoform, and alcohol account for the majority of mental disorders in the primary care. Studies have shown consistently that physicians in the office settings fail to diagnose and treat up to 50% of patients suffering from common disorders, which usually result in substantial patient suffering, disability, and healthcare costs.[3–4] Surveys in a Nigerian population using GHQ and PHQ show a high prevalence among primary care patients.[5–7] Furthermore, a WHO collaborative study on psychological problems in 14 countries using a 2-stage case identification methodology shows that psychiatric morbidity in general health care setting is high.[8]
Screening tools are essential and important instrument in the diagnosis and treatment of mental disorders. PHQ has been found to be an essential screening tool for specific mental disorders, especially depression. In the absence of systematic screening, family physicians miss at least 50% of cases of major depression.[9] PHQ-9 has been well tested as a tool to screen for specific mental disorder, especially depressive illness in all age groups in varieties of countries,[10–12] and has been shown to be useful in general populations including outpatient clinic settings and sensitive to change in the elderly.[13–15] Its screening characteristics (sensitivity and specificity) had also been validated[16] and has also been recommended for depression screening in primary care.[17–19] The value of screening for depression in primary care is under debate, with the Unites States (US) Preventive services task force making the case for screening and the Cochrane review coming to the opposite conclusion.[20–21] The PHQ has diagnostic validity comparable to the original clinician administered Primary Evaluation of Mental Disorders (PRIME-MD) and is more efficient to use. Research has been carried out among Nigerians using the PHQ.[14–15,22–23]
Mental disorders have a dramatic effect on the lives of those who experience it and their families. It also has considerable economic impact on the society. It leads to impaired functional capacity, increased need for health care, and deterioration in the quality of life.[24,25] The rising tide of mental disorder may be related to factors such as economic change, political and social violence, and cultural disruptions. Dislocation from home by economic forces especially with the advent of global economic recession have been associated with great increase in varieties of mental disorders.[24]
Screening at the community level will provide keys to promoting health and preventing diseases at the community level. This will serve as the fulcrum for timely detection and intervention. This study aims to assess the prevalence and nature of mental disorder among the general population using the patient health questionnaire (PHQ). It also compares the use of PHQ and GHQ as screening tools for mental disorders generally. This study will provide baseline information for community physicians and psychiatrists in the prevention of mental disorder at the community level. It will help in health care planning for prevention, treatment, and rehabilitation of mental illnesses.
Materials and Methods
This community-based study is cross sectional in design and aimed at collecting data on mental disorders in a Nigerian community, Sagamu local government area of Ogun State, South-western Nigeria. Sagamu is an urban local government area with a population of about 269,890 people (NPopC).
Sampling procedure
Multistage sampling technique was used to obtain a representative sample of the communities in Ogun State.
Stage 1: Using a sampling frame of all the local government in Ogun State, Sagamu local government area was selected by simple random sampling.
Stage 2: Sampling frame of all the communities in Sagamu local government areas was drawn. The communities where the study was carried out were selected by simple random sampling (balloting). The communities selected were Makun and Sabo communities.
Stage 3: Using the PHC house numbering where available (in places where it has not been done the houses were numbered for the purpose of the study.) Systematic sampling technique was employed to select the houses that were visited in the chosen communities. Seventy four houses were visited in Makun community and 85 in Sabo community.
Stage 4: Every resident aged 15 years and above who has resided in the area for at least 6months was interviewed in the houses selected.
Sample size
A total of 758 subjects were recruited into the study. There was prevalence of 12.8% of poor mental illness using GHQ questionnaire among urban primary health care settings in Nigeria. A precision of 95% is desired with a power of 90%. The calculated sample size was 246, while this was tripled to 758 with response rate of 95% (758).
Study instrument
The survey instrument for the study was the PHQ.[5] It is a self-reported scale derived from PRIME-MD, which is a standardized and rapid procedure with demonstrated diagnostic performance (sensitivity of 83%, specificity of 88%, and positive predictive value of 80%) for the diagnosis of any psychiatry disorder in primary health care. The PRIME-MD was the first instrument designed for use in the primary care that actually diagnosed specific disorders using diagnostic criteria from Diagnostic and Statistic Manual of Mental Disorders, fourth edition (DSM IV). The PHQ has diagnostic validity comparable to the original clinician administered PRIME-MD and is more efficient to use. Research has been carried out among Nigerians using the PHQ.[22–23]
Data collection
The study was conducted using an interviewer administered structured questionnaire—the PHQ and GHQ. This questionnaire was translated into the local language for easy administration and translated back to English to ensure accuracy of translation. The questionnaires were administered by graduate research assistants who were health workers after adequate training and author's supervision. They were trained on how to extract the information on psychiatric symptoms and the relevance to the research work. They were also guided through a good number of the questionnaire until a reasonable level of competence had been attained before being left to complete the work.
Data analysis
Data generated in the study were manually cleaned and then entered into the computer using SPSS 10 Statistical software for analysis. Percentages or mean and standard deviation were computed for baseline characteristics of the subjects interviewed. The data analyzed focused on univariate frequency table and bivariate cross tabulations that identify important relationship between sociodemographic characteristics of the subjects and the presence of psychopathology were examined through bivariate analysis.
Logistic regression analysis was done to determine factors associated with mental disorders in Ogun State, and also to remove the effect of confounding variables. The dependent variable was mental morbidity as a dichotomous variable. All the variables significant in the bivariate analysis with P < 0.08 were fed into the model. Odd ratios were adjusted and P values of <0.05 were taken as significant for the study.
Results
Sociodermographic characteristics of the participants
A total of 758 participants took part in the study participants age ranged from 15 to 90 yrs with mean age of 41.64 + 18.01 yrs. Three hundred and twenty (42.2%) of the participants were males. About half (48.1%) of the participants were married. Forty eight (6.3%) of the participants had no formal education, 97 (12.8%) had primary education, 377 (49.7%) with secondary education, and 236 (31.1%) had tertiary education. Majority of the participants, i.e., 636 (83.9%) were indigenes (the Yorubas), while the remaining 122 (16.1%) were nonindigenes (Igbos, Hausas, and other tribes in Nigeria).
Psychopathology and socioenvironmental factors
A total of 496 (65.4%) of the subjects had a form of psychopathology or the other. Among those with psychopathology, 186 (24.5%) met criteria for only one diagnosis, 148 (19.5%) for two diagnosis, and 162 (21.4%) for three diagnosis. Three hundred and thirty one subjects (43.7%) were diagnosed to have Somatoform disorder, 269 (35.5%) met criteria for depression, while 165 (21.8) met the criteria for general anxiety.
The Singles (never married) have a higher morbidity rate when compared with the married (P = 0.026) [Table 1]. The male respondents had a higher morbidity when compared with the female sex (χ2 = 3.80, P = 0.03). The indigenes were significantly more mentally healthier than the nonindigenes (χ2 = 4.47, P = 0.021).
Table 1.
Spectrum of mental disorders assessed
Major environmental factors associated with psychopathology were stress at work (60.1% vs. 86.4%, χ2 = 37.43, P = 0.000), financial situation (54.3% vs. 77.1%, χ2 = 43.63, P = 0.000), concerns about their health (55.5% vs. 83.8%, χ2 = 61.34, P = 0.000), recent bad events (62.5% vs. 79.4%, χ2 = 13.63, P = 0.000), and lack of confidence (60.1% vs. 77.6%, χ2 = 21.82, P = 0.000) [Table 2].
Table 2.
Psychopathology and sociodermographic characteristics
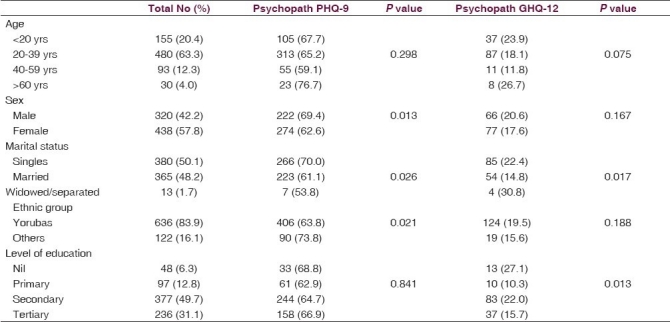
Comparison of PHQ with GHQ questionnaire
Using the GHQ questionnaire under the same condition as the PHQ, 143 (18.9%) were detected to have psychopathology. Assessment by GHQ and PHQ questionnaires shows a statistically significant difference (χ2 = 20.92, P = 0.000). The Singles (χ2 = 8.202, P = 0.017) and the illiterates (χ2 = 10.76, P = 0.013) had a higher psychopathology when compared with the married and the educated. There is no significant difference in psychopathology between the Yorubas and other ethnic groups (χ2 = 1.029, P = 0.188). There is also no significant difference in mental morbidity among male and female respondents (χ2 = 1.120, P = 0.167). All the socioenviromental factors significant for PHQ were also significant for GHQ questionnaire [Table 2].
Multivariate analysis
In the multiple logistic regression model, five variables were found to be independently associated with psychopathology [Table 3]. Predictors of psychopathology were individuals who were Singles (OR = 0.64, CI = 0.49–0.93) concerns about their health (OR = 3.06, CI = 2.06–4.56), worried about finance (OR = 1.84, CI = 1.27–2.67), worried about family life (OR = 2.68, CI = 1.61–4.72), and stressed at work (OR = 1.16, CI = 1.06–1.28).
Table 3.
Multivariate analysis—Predictors of psychopathology using PHQ-9
Discussion
This is a community-based study aimed at assessing the prevalence of mental disorders among the general population using the PHQ. This study shows that there is a high prevalence of psychopathology in the Nigerian population. This is similar to several other studies in various part of the world in recent times.[26–29] The rising tide of mental disorder may be related to factors such as economic change, political and social violence, cultural disruptions, dislocation from home by economic forces especially with the advent of global economic recession have been associated with great increase in varieties of mental disorders.[24]
The prevalence of depression in the study population is 35.5%, anxiety 21.8%, Somatoform disorder 43.7%, and alcohol-related problem 13.2% are high but similar studies in various parts of the world had shown a similar trend.[30–33] Similarity in prevalence of psychiatric disorder in the community found in the study and similar study carried out in primary care centers show that most people with psychopathology present in the clinics. This suggests a high level of awareness and prompt presentation of mental illness at the primary care centers.[34–36] The facts that a small proportion 3.8% of those that reported psychopathology have ever been treated before may suggest that the major problem in the management of mental illness is the issue of under- recognition at the primary care settings. This has been globally acknowledged.[37–38]
Surveys in a Nigerian population using GHQ and PHQ show a similarly high prevalence among primary care patients.[5–7] Furthermore, a WHO collaborative study on psychological problems in 14 countries using a 2-stage case identification methodology shows that psychiatric morbidity in general health care setting is high. It also shows that the common psychiatric health problems identified were depression, anxiety, alcohol abuse, somatoform disorders, and neurasthenia.[1,8]
The study shows that significantly more male participants exhibit psychopathology than females. This is similar to findings in several other studies.[5–6,17–18] This may be due to the dominant role of males in this culture. They are bread winners and are largely responsible for community survival. Furthermore, the fact that those that are singles and the other ethnic groups develop more mental morbidity than the indigenes and the married shows that companionship is an important factor in the development and management of psychiatric illnesses. This fact has been emphasized in several studies.[6–7,10] The process of adapting to a new culture and environment may present a significant challenge for other ethnic groups apart from the Yorubas. The fact that the elderly shows significantly more psychopathology than other age groups may indicate that the extended family structure which is fast breaking down in African community can no longer adequately cater for the health of the elderly. Its high time provisions are made for care of the elderly and day care centers provided especially in developing countries of the world.[22]
Mental health assessment by GHQ and PHQ questionnaires shows a statistically significant difference, thus indicating that both instruments may not be measuring the same mental indices. This is buttressed in the study by the fact that sociodemographic characteristics such as male sex, migrants, and marriage or companionship significantly associated with psychopathology using PHQ were not significant for GHQ. PHQ is more useful as an instrument to screen for specific mental disorders rather than a general screening tool for psychiatric morbidity at the community level. Thus, GHQ is a better general screening tool than PHQ since the prevalence of detection is lower and closer to prevalence detected by trained physicians from other studies in similar population.[22–23] This indicate that PHQ as a general screening tool has a higher false-positive value compared to GHQ as demonstrated in this study. Screening at the community level will provide keys to promoting health and preventing diseases at the community level and serve as the fulcrum for timely detection and intervention. It will sensitize both the general community and health workers to identification and recognition of mental morbidity at the community level before their presentation at the primary health care settings.
Conclusion
There is a high prevalence of psychopathology at the community level in this African population. The common mental disorders found in this study are similar to those found in several other studies namely Somatoform disorder, depressive and anxiety disorder, and alcohol-related problems in that order. Male sex, migration, loneliness, and the elderly age are the associated risk factors for mental disorders. PHQ has a higher false positive value compared to GHQ as demonstrated in this study. PHQ should be used as an instrument to screen for specific mental disorders rather than a general screening tool for psychiatric morbidity at the community level.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JB, deGruy FV, 3rd, et al. Health related quality of life in primary care patients with mental disorders. J Am Med Assoc. 1995;274:1511–7. [PubMed] [Google Scholar]
- 2.Sartorious N, Ustun TB, Costa e Silva JA, Goldberg D, Lecrubier Y, Ormel J, et al. An international study of psychological problems in primary care: Preliminary report from the World Health Organization Collaborative Project on Psychological Problems in General Health Care. Arch Gen Psychiatry. 1993;50:819–24. doi: 10.1001/archpsyc.1993.01820220075008. [DOI] [PubMed] [Google Scholar]
- 3.Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorder in primary care: The PRIME-MD 100study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 4.Philblic JT, Connely JE, Wofford AB. The prevalence of mental disorders in rural office practice. Am J Med. 1996;1:9–15. doi: 10.1007/BF02603478. [DOI] [PubMed] [Google Scholar]
- 5.Abiodun OA. A study of mental morbidity among primary care patients in Nigeria. Compr Psychiatry. 1993;34:10–3. doi: 10.1016/0010-440x(93)90030-8. [DOI] [PubMed] [Google Scholar]
- 6.Amoran OE, Lawoyin TO, Oni OO. Risk factors associated with mental illness in Oyo State, Nigeria: A community based study. Ann Gen Psych. 2005;4:19. doi: 10.1186/1744-859X-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gureje O, Obikoya BO, Ikueesan BA. Prevalence of specific disorders in an urban primary health care. East Afr J. 1992;69:282–7. [PubMed] [Google Scholar]
- 8.Sartorius N, Ustun TB, Lecrubier Y, Wittchen HU. Depression comorbid with anxiety: Results from the WHO study on psychological disorders in primary health care. Br J Psychiatry. 1996;169(Suppl):38–43. [PubMed] [Google Scholar]
- 9.US Preventive services task force. Screening for depression: Recommendations and rationale. Ann Intern Med. 2002;136:760–4. doi: 10.7326/0003-4819-136-10-200205210-00012. [DOI] [PubMed] [Google Scholar]
- 10.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study: Primary care evaluation of mental disorders: Patient health questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 11.Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients: A comparison of the center for epidemiologic studies-depression scale and the geriatric depression scale. Arch Intern Med. 1997;157:449–54. [PubMed] [Google Scholar]
- 12.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. J Gen Intern Med. 2007;22:1596–602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the patient health questionnaire: A systematic review. Gen Hosp Psychiatry. 2007;29:388–95. doi: 10.1016/j.genhosppsych.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med Care. 2004;42:1194–201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 16.The state of mental health and aging in America issue brief 1: What do the data tell us? Atlanta, GA: 2008. Centers for Disease Control and Prevention and National Association of Chronic Disease Directors. [Google Scholar]
- 17.The Macarthur foundation. The Macarthur initiative on depression and primary care. [cited in 2003]. Available from: http://www.depression-primarycare.org .
- 18.Nease DE, Jr, Maloin JM. Depression screening: A practical strategy. J Fam Pract. 2003;52:118–24. [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 20.Gilbody S, House AO, Sheldon TA. Screening and case finding instruments for depression. Cochrane Database Syst Rev. 2005;4:CD002792. doi: 10.1002/14651858.CD002792.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of the prime-MD: The PHQ primary care study: Primary care evaluation of mental disorders: Patient health questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 22.Ohaeri JU, Odejide OA, Gureje O, Olatawura MO. The prevalence of psychiatric morbidity among adult attenders in the five PHC facilities of a rural community in Nigeria. Psychopathol Afr. 1994;26:97–108. [Google Scholar]
- 23.Ogunsemi OO, Oluwole FA, Abasiubong F, Erinfolami AR, Amoran OE, Ariba AJ, et al. Detection of mental disorders with the Patient Health Questionnaire in primary care settings in Nigeria. Mental Illness. 2010;2:e10. doi: 10.4081/mi.2010.e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lyness JM. Naturalistic outcomes of minor and subsyndromal depression in older primary care patients. Int J Geriatr Psychiatry. 2008;23:773–81. doi: 10.1002/gps.1982. [DOI] [PubMed] [Google Scholar]
- 25.Lyness JM, Chapman BP, McGriff J, Drayer R, Duberstein PR. One-year outcomes of minor and subsyndromal depression in older primary care patients. Int Psychogeriatr. 2009;21:60–8. doi: 10.1017/S1041610208007746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Spitzer RL, Williams JB, Kroenke K, Linzer M, de Gruy FV, 3rd, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care: The PRIME-MD 1000 study. JAMA. 1994;272:1749–56. [PubMed] [Google Scholar]
- 27.Ansseau M, Dierick M, Buntinkx F, Cnockaert P, De Smedt J, Van Den Haute M, et al. High prevalence of mental disorders in primary care. J Affect Disord. 2004;78:49–55. doi: 10.1016/s0165-0327(02)00219-7. [DOI] [PubMed] [Google Scholar]
- 28.Avasthi A, Varma SC, Kulhara P, Nehra R, Grover S, Sharma S. Diagnosis of common mental disorders by using PRIME-MD patient health questionnaire. Indian J Med Res. 2008;127:159–64. [PubMed] [Google Scholar]
- 29.Goldberg D, Lecrubier Y. Form and frequency of mental disorders across centers. In: Ustun TB, Sartorius N, editors. In mental illness in General Health Care: An international study. Chichester: John Wiley and Sons; 1995. [Google Scholar]
- 30.Allgulander C, Nilsson B. A nationwide study in primary health care: One out of four patients suffers from anxiety and depression [in Swedish] Lakartidningen. 2003;100:832–8. [PubMed] [Google Scholar]
- 31.Nordstrom A, Bodlund O. Every third patient in primary care suffers from depression, anxiety or alcohol problems. Nord J Psychiatry. 2006;62:250–5. doi: 10.1080/08039480802141129. [DOI] [PubMed] [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study: Primary care evaluation of mental disorders: Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 33.Cameron I, Reid I, Lawton K. Appropriateness of antidepressant prescribing: An observational study in a Scottish primary-care setting. Br J Gen Pract. 2009;59:644–9. doi: 10.3399/bjgp09X454061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hickie I, Hooker AW, Hadzi-Pavlovic D, Bennett BK, Wilson AJ, Lloyd AR. Fatigue in selected primary care settings: Sociodemographic and psychiatric correlates. Med J Aust. 1996;164:585–8. doi: 10.5694/j.1326-5377.1996.tb122199.x. [DOI] [PubMed] [Google Scholar]
- 35.Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Mental health literacy: A survey of the public's ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Med J Aust. 1997;166:182–6. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- 36.Goldberg DP, Jenkins L, Millar T, Faragher EB. The ability of trainee general practitioners to identify psychological distress among their patients. Psychol Med. 1993;23:185–93. doi: 10.1017/s0033291700038976. [DOI] [PubMed] [Google Scholar]
- 37.Tobin M, Hickie I, Urbanc A. Increasing general practitioner skills with patients with serious mental illness. Aust Health Rev. 1997;20:55–67. doi: 10.1071/ah970055a. [DOI] [PubMed] [Google Scholar]
- 38.Primary care psychiatry - the last frontier. Canberra: Royal Australian College of General Practitioners and Royal Australian and New Zealand College of Psychiatrists; 1997. Report of the Joint Consultative Committee. [Google Scholar]


