Sir,
Nontraumatic acute subdural hematoma (ASDH) is a rare condition, and the literature is limited to case reports and small series.[1] Myelodysplastic/myeloproliferative neoplasms (MDS/MPNs) are clonal myeloid neoplasms characterized, at the time of initial presentation, by the simultaneous presence of both myelodysplastic and myeloproliferative features.[2,3] We report a case of nontraumatic ASDH associated with MDS/MPNs.
A 74-year-old man diagnosed with chronic myelomonocytic leukemia (CMML), which is a subtype of MDS/MPNs, presented with sudden onset of headache and nausea, and referred to our hospital. On admission, neurological examination revealed consciousness disorder (somnolence), palsy of oculomotor nerve, and left-sided hemiparesis. Computed tomography (CT) revealed the presence of bilateral ASDH in the supratentorium [Figure 1]. In the three-dimension CT angiography, there was no abnormality of vessels including aneurysm or arteriovenous malformation. There was no history or obvious findings of head trauma. In the blood examination, white blood cell (WBC) counted 1,176,000/μl. Persistent peripheral blood monocytosis was detected (monocyte count, 9996/μl). Platelet counted 5700/μl. The coagulation system was normal, but the bleeding time was prolonged to 4 minutes 30 seconds. After admission, his consciousness became worse (semicoma) and he underwent operation for hematoma removal with a transfusion of two units of red blood cell concentrate in mannitol adenine phosphate (RC-M.A.P.), 10 units of platelet concentrate (PC). After removing the hematoma, there was no obvious origin of hemorrhage on the surface of the brain and dura mater. Hemostasis in these areas, including epidural area, could be achieved during closure of the craniotomy. The CT performed on the next day revealed acute epidural hematoma (AEDH) caused by rebleeding. Postoperative platelet counted 5,500/μl. He underwent reoperation of hematoma removal with a transfusion of 4 units of RC-M.A.P., 10 units of PC and 5 units of fresh frozen plasma (FFP). Hemostasis could also be achieved during and after surgery by platelet transfusion of 4 units of RC-M.A.P. and 10 units of PC. Postoperative CT after second surgery showed the AEDH was removed [Figure 2]. Platelet counted 5500/μl after second surgery.
Figure 1.
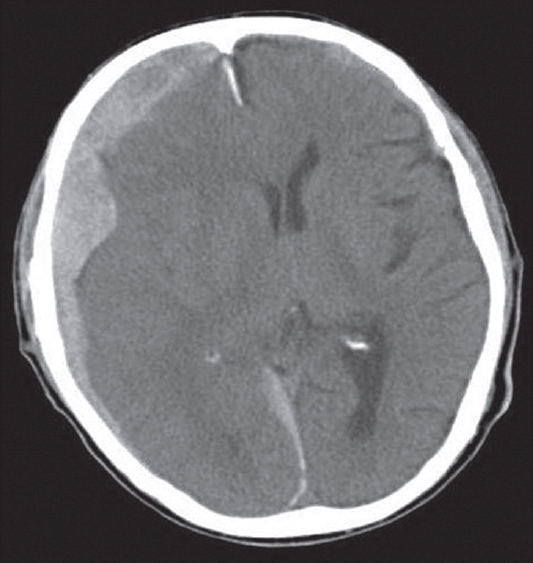
CT scanning showed both side of the ASDH in the supratentorium
Figure 2.
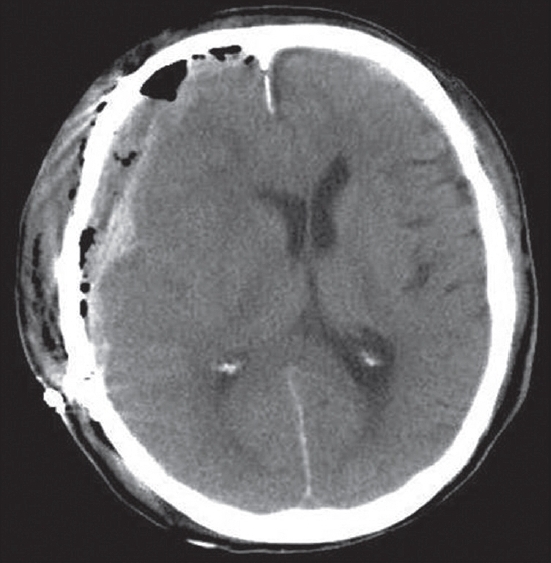
CT scanning after the second surgery showed the AEDH was removed
The following underlying causes of nontraumatic ASDH have been described: Aneurysm rupture, ruptured cortical artery, hypertensive cerebral hemorrhage, arteriovenous malformations and dural arteriovenous fistula, neoplasms, hematological disorders, anticoagulant and thrombolytic therapy, cerebral amyloid angiopathy, acquired immunodeficiency syndrome, cocaine abuse, and moyamoya disease.[4] The factors of neoplasm and hematological disorder were associated with the present case. Although there was neither a history of head trauma nor an obvious origin of bleeding on the brain and the dura of this patient, ASDH could have occurred after unrecognized or forgotten minor trauma.[4]
CMML is a subtype of MDS/MPNs with a typical manifestation of peripheral blood monocytosis.[3] CMML is diagnosed on the basis of persistent peripheral blood monocytosis with the monocyte count exceeding 1000/μl.[3] Because MDS/MPNs have characteristics of both ineffective erythropoiesis in myelodysplastic syndrome and hyperproliferation in MPNs,[2,3] platelet function was compromised by ineffective erythropoiesis in spite of normal blood cell counts, which might have caused nontraumatic ASDH, postoperative bleeding in this case. When conducting surgery, sufficient blood transfusion should be considered during and after surgery regardless of preoperative platelet counts and coagulation profiles.
References
- 1.Depreitere B, Van Calenbergh F, van Loon J. A clinical comparison of non-traumatic acute subdural haematomas either related to coagulopathy or of arterial origin without coagulopathy. Acta Neurochir (Wien) 2003;145:541–6. doi: 10.1007/s00701-003-0020-7. [DOI] [PubMed] [Google Scholar]
- 2.Foucar K. Myelodysplastic/myeloproliferative neoplasms. Am J Clin Pathol. 2009;132:281–9. doi: 10.1309/AJCPJ71PTVIKGEVT. [DOI] [PubMed] [Google Scholar]
- 3.Orazi A, Germing U. The myelodysplastic/myeloproliferative neoplasms: Myeloproliferative diseases with dysplastic features. Leukemia. 2008;22:1308–19. doi: 10.1038/leu.2008.119. [DOI] [PubMed] [Google Scholar]
- 4.Avis SP. Nontraumatic acute subdural hematoma. A case report and review of the literature. Am J Forensic Med Pathol. 1993;14:130–4. [PubMed] [Google Scholar]


