Abstract
Background/Aim:
Acute upper gastrointestinal hemorrhage (AUGIH) is a life-threatening emergency that results in high morbidity and mortality. The mortality rate varies between 4% and 14%. The aim of the study was to determine the clinical outcome of AUGIH among patients admitted to a government hospital in Egypt.
Patients and Methods:
This was a cross-sectional hospital-based study performed in 1000 patients presenting with AUGIH over a 7-year period between January 2004 and January 2011.
Results:
One thousand patients were analyzed. Fifty-four percent were male. Mean age was 52 ± 17 years. Eighty-eight percent were emergency admissions and 12% were inpatients at the time of bleeding. At presentation 68% had major comorbidity and 50% had liver disease. Seven hundred and twenty-four patients (72%) underwent endoscopy. Bleeding varices accounted for 31% of AUGIH and peptic ulcer 28%. Two hundred and thirty-two patients had endoscopically diagnosed bleeding varices or peptic ulcer with a visible vessel or active bleeding. These received endoscopic therapy. Initial hemostasis was achieved in 207 (89%). Thirteen patients (6%) had therapy at a subsequent endoscopy for further bleeding. Surgery was performed on 9 patients (0.9%) with AUGIH. Complications were reported in 70 patients (7%) mainly liver failure (4%). Six hundred and eighty-four patients (68%) were discharged improved, 162 (16%) left hospital without a diagnosis and 4 (0.4%) were referred to another facility. The overall mortality was 15%. Mortality was 24% in patients ≥60 years, 37% among inpatients, and 21% in those who had a major comorbidity. Mortality was 22% in patients who had liver disease and 9% in variceal bleeding.
Conclusion:
The most common cause of AUGIH was variceal in origin. Endoscopic therapy was successful in most cases. Mortality after AUGIH was particularly high among elderly patients, inpatients, and patients who had a major comorbidity, liver disease, and variceal bleeding.
Keywords: Egypt, gastrointestinal hemorrhage, outcome
Acute upper gastrointestinal hemorrhage (AUGIH) is a life-threatening emergency that results in a high morbidity and mortality and therefore requires admission to hospital for urgent diagnosis and management. Despite new therapeutic tools such as the proton pump inhibitors, endoscopic interventions, and surgical advances, the clinical outcome has not changed significantly and mortality rate remains around 10%.[1]
Schistosomiasis and hepatitis C virus (HCV) are common diseases in Egypt. HCV currently infects 20.7% of the Egyptian population.[2] Bolak Eldakror Hospital is a secondary care government hospital in Giza, Egypt. The gastrointestinal endoscopy unit was set up in 1999. At that time patients presenting with AUGIH were referred to other hospitals. Some died before or during transfer. A plan for the management of AUGIH (within the available resources) was formulated in 2 stages. Stage one started in January 2000 and ended in January 2004. In this stage only selected cases were managed. A backup with a teaching hospital (Cairo University) was arranged. All therapeutic endoscopy procedures were performed under close supervision by a high level consultant from the teaching hospital. Stage two began in January 2004 when a management protocol was set up and all patients presenting with AUGIH were admitted and managed in house. As with most government hospitals in Egypt balloon tamponade, vasoactive drugs, surgical shunts, and transjugular intrahepatic portosystemic shunts are not locally available. The aim of the study was to determine the clinical outcome of AUGIH among patients admitted to a government hospital in Egypt.
PATIENTS AND METHODS
This was a cross-sectional hospital-based study performed in 1000 patients presenting with AUGIH over a 7-year period between January 2004 and January 2011. Patients with AUGIH were admitted, assessed, and resuscitated in a 3-bed intensive care unit. Acute bleeding was defined as bleeding within 3–7 days of presentation. A quality controlled disease management protocol for acute bleeding was established with the intention of improving the quality and efficiency of our heath care delivery. Clinical guidelines and a clinical care pathway were developed within the availability of local therapeutic options in order to provide a stand-alone practical guide for the team. The care pathway was developed to improve patient management and resource utilization based on the protocol designed by Courtney et al. and international guidelines.[3,4] The guidelines and care pathway were disseminated throughout the hospital to house officers, residents, attending physicians, and nursing staff. Therapy was given according to a standard protocol. A consultant gastroenterologist was on-call 24/7 days a week to attend resuscitation when bleeding was detected. The gastroenterologist served as a facilitator for the medical staff caring for the patients, often monitoring intravenous hydration and delivering blood/blood products. The aim was to decrease the time interval from admission to achievement of hemodynamic stability and improvement in hemoglobin level.
The patients were classified as being at low or high risk for rebleeding and mortality. Patients at low risk for rebleeding and mortality (young, without a major comorbidity, and minor bleeding) were discharged from hospital. Subsequently, they underwent diagnostic endoscopy on the next available list. Patients at high risk (elderly, had a major comorbidity, or major bleeding) underwent intense monitoring with early, rapid, and adequate resuscitation (fluids, fresh blood). Endoscopy was done on the morning of the second day with the intention of establishing the diagnosis and to provide therapeutic intervention(s) to control bleeding and prevent rebleeding if considered appropriate. Once an intervention has been undertaken, the procedure was considered successful if bleeding stopped and there was no recurrent bleeding. During hospitalization the patients were closely monitored in the medical department for rebleeding and complications until their discharge. Patients were observed for 5 days to assess stability or rebleeding. If hemostatic therapy was unsuccessful, either because bleeding was not controlled or rebleeding occurred, repeat endoscopy or surgery was considered. The endpoints were 2 weeks of follow-up or the death of the patient. Outcomes were analyzed annually. The reports were transmitted to an independent experienced endoscopist with a particular interest in gastrointestinal hemorrhage for comment and advice.
A standardized data collection form (sheet) was completed for each patient during the hospital admission. Recorded information included demographic information, the patient's condition at the time of bleeding, historical data (presenting symptoms, comorbid illnesses), physical examination findings (hemodynamic data), initial hemoglobin level, Child–Pugh classification, resuscitative efforts (blood transfusion requirement, time interval between presentation with bleeding and the correction of hemodynamic instability and hemoglobin level). Patients who did not undergo endoscopy were recorded. Endoscopy practice was noted, including the time interval between presentation and endoscopic intervention in patients at high risk, the reason for any inability to undertake endoscopy within 24 h and the endoscopic findings. The endoscopic components of the database included identification of the bleeding lesion, description of stigmata of bleeding, method of endoscopic hemostasis if any, and number of therapeutic attempts. Outcomes recorded included the success of endoscopic therapy, frequency of rebleeding, surgical therapy, complications, and mortality. The cause of death and the time interval (in hours) between admission and death was determined.
The data from the patients were registered, tabulated, and statistically analyzed using a program of SPSS version 15.
RESULTS
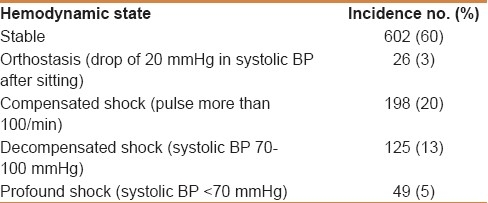
One thousand patients, fulfilling our definition of AUGIH were analyzed. Fifty-four percent were male and 46% female. Ages ranged from 13 to 95 years, mean 52 ± 17 years. Thirty-six percent of patients were ≥60 years. The most common presenting symptom was hematemesis (68%) [Table 1]. Eight hundred and eighty-five patients (88%) were emergency admissions and 115 (12%) were inpatients at the time of bleeding. Six hundred and eighty-two patients (68%) had a major comorbidity [Table 2] and 96 (10%) had a minor comorbidity (hypertension or diabetes mellitus). Five hundred and three patients (50%) had liver disease of whom 23% were Child–Pugh classification A, 25% B, and 53% C. One hundred and seventy-four patients (18%) had a systolic blood pressure (BP) less than 100 mmHg [Table 3]. The mean hemoglobin concentration was 9 ± 3 g/dl and 25% had initial hemoglobin less than 7 g/dl. Four hundred and fifteen patients (42%) required blood transfusion and the average number of transfused blood units was 3. The time interval to correct hemodynamic instability was 1–168 h (mean 10 ± 18). The time interval to correct the hemoglobin was 4–240 h (mean 56 ± 45).
Table 1.
Clinical presentation of the bleeding episode for patients with AUGIH
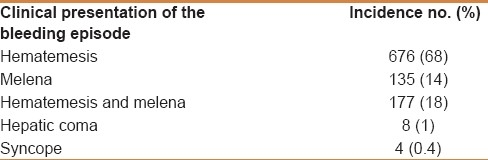
Table 2.
Major comorbidities among patients with AUGIH
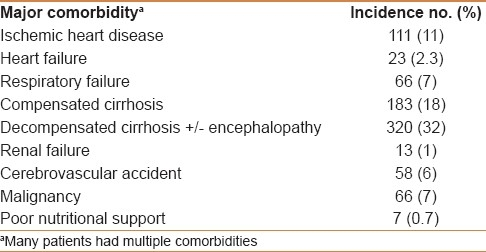
Table 3.
Hemodynamic state among patients with AUGIH
Some groups of patients were excluded from the analysis of endoscopic practice. These included 276 patients (28%) who did not have an inpatient endoscopy for the following reasons: 61 (6%) died rapidly on admission, 51 (5%) unfit for endoscopy, 43 (4%) self-discharging prior to endoscopy being undertaken, 41 (4%) had specific contraindication to endoscopy, 38 (4%) were specifically categorized as terminal care patients, 26 (3%) refused or their family refused consent for endoscopy, 13 (1%) had unsuccessful esophageal intubation or incomplete procedure due to agitated/uncooperative patient, 2 (0.2%) had unsuccessful esophageal intubation due to organic lesion, and 1 (0.1%) patient required direct and urgent surgical intervention because of rapid exsanguination.
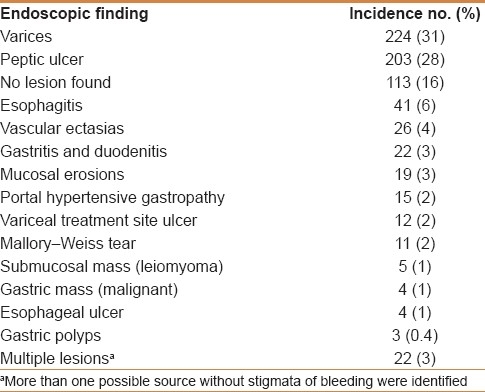
Seven hundred and twenty-four patients (72%) underwent endoscopy during admission of whom 537 (74%) had a high-risk bleed. The mean time from presentation to endoscopy in these patients was 24±23 h (15 min – 168 h). Endoscopy was conducted within 24 h of presentation in 404 high-risk patients (75%) and was delayed more than 24 h in 133 (25%). The reasons for delay were unavailable staff/equipment in 98 patients (18%), hemodynamic instability in 15 (3%), medical condition in 13 (2%), and no obvious explanation recorded in 7 (1%). A cause of bleeding was identified from endoscopy in 611 patients (84%) [Table 4]. Bleeding varices accounted for 31% of AUGIH and peptic ulcer 28%.
Table 4.
Endoscopic findings for patients with AUGIH
Two hundred and thirty-two patients (32%) with either endoscopically diagnosed bleeding varices or peptic ulcer and a visible vessel or active bleeding received endoscopic therapy at the time of initial endoscopy. Initial hemostasis was achieved in 207 patients (89%). One hundred and seventy-seven patients (24%) bled from esophageal varices, 47 (7%) from gastric varices, and 8 (1%) from peptic ulcer with a visible vessel or active bleeding. Sclerotherapy was performed in 123 patients (17%), rubber band ligation in 94 (13%), both in 7 (1%) and epinephrine injection in 8 (1%) patients. Injection sclerotherapy with ethanolamine oleate solution was used to treat 98 patients (44%) with bleeding varices and tissue adhesive (histoacryl) in 48 (21%). Initial hemostasis was achieved in 201 patients (90%) with variceal bleeding and 6 patients (75%) with peptic ulcer and a visible vessel or active bleeding.
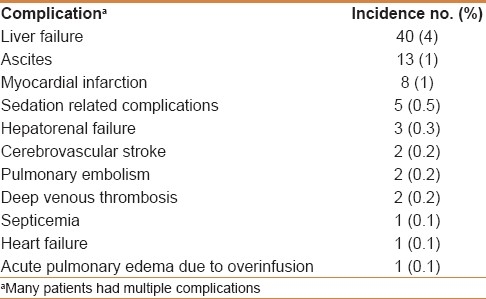
Thirteen patients (6%) had therapy at a subsequent endoscopy for further bleeding. Surgery was performed on 9 patients (0.9%) with AUGIH. Four patients (0.4%) had surgery for further bleeding and 5 (0.5%) because of an associated leiomyoma. Complications were reported in 70 patients (7%) during the same hospitalization [Table 5]. The most frequent complications were liver failure (4%), ascites (1%), and acute myocardial infarction (1%).
Table 5.
Complications among patients with AUGIH
Six hundred and eighty-four patients (68%) were discharged improved, 162 (16%) left hospital without a diagnosis and 4 (0.4%) were referred to another facility (cancer institute) for further treatment. One hundred and fifty patients (15%) died within the first 2 weeks of their hospital admission. One hundred and fourteen patients (11%) died without having an endoscopy. The time interval from admission or detection of bleeding to death ranged from 10 min to 312 h, mean 36 ± 59 h. Thirty-six patients (4%) died after they underwent inpatient endoscopy. The time interval from endoscopy to death ranged from 15 min to 288 h, mean 53 ± 71 h. Death was due to continuing bleeding or associated complications (mainly organ failure) in 127 patients (13%), comorbid disease (mainly cerebrovascular accident) in 19 (2%), endoscopy was considered a possible cause (sedation-related complications in patients with major comorbidity) in 3 (0.3%) and medical error (acute pulmonary edema due to fatal overinfusion) in 1 (0.1%).
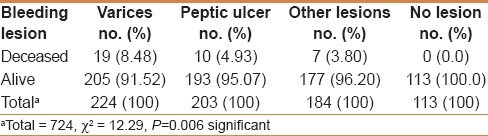
Mortality was 23.82% in patients ≥60 years of age versus 10.02% in patients <60 years (P<0.0001) [Table 6]. Mortality was 36.52% among inpatients versus 12.2% in emergency admissions (P<0.0001) [Table 7]. Mortality was 20.89% in patients who had major comorbidity versus 2.77% without any major comorbidity (P<0.0001) [Table 8]. Mortality was 21.87% in patients who had liver disease versus 8.05% without liver disease (P<0.0001) [Table 9]. Mortality was 7.43% in high-risk patients who underwent urgent endoscopy within 24 h versus 4.51% in high-risk patients in whom endoscopy was delayed more than 24 h (P<0.5, not significant) [Table 10]. Mortality was 8.48% in variceal bleeding, 4.93% in peptic ulcer bleeding and 3.80% in other lesions bleeding (P=0.006) [Table 11].
Table 6.
Mortality outcome versus age of patients with AUGIH
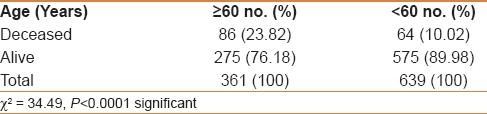
Table 7.
Mortality outcome and patient's condition at the time of bleeding among patients with AUGIH
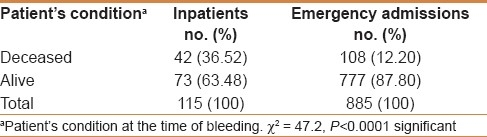
Table 8.
Mortality outcome versus the presence of comorbidities in patients with AUGIH
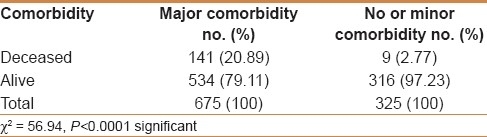
Table 9.
Mortality outcome versus the presence of liver disease in patients with AUGIH
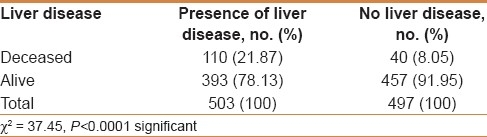
Table 10.
Mortality outcome versus time of endoscopy among high risk patients with AUGIH who required urgent endoscopy
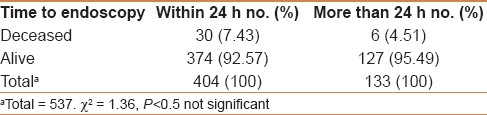
Table 11.
Mortality outcome versus endoscopic diagnosis in patients with AUGIH
DISCUSSION
Globally, AUGIH continues to be a common cause of hospital admission and has a high morbidity and mortality.[5] Endoscopy plays a pivotal role in its diagnosis and management. Mortality is lower in specialist endoscopy units; and this is probably not related to technical development but because of adherence to protocols and guidelines.[4]
Schistosomiasis and HCV are common diseases in Egypt, and AUGIH is a frequent emergency.[2] Despite the advent of endoscopy and endoscopic therapy, access to medical centers with experienced medical staff and adequate equipment in Egypt is still limited. Most government hospitals in Egypt refer patients with AUGIH to teaching hospitals, academic institutes, insurance hospitals, and private hospitals. Many patients never reach hospital.
Our plan for AUGIH was designed to be within the available resources and was formulated in 2 stages. Stage one, 2000–2004, was the training of staff and preparation. During this time we assessed the capability of the hospital for dealing with these cases. Following the assessment we went to stage two. In stage two, 2004–2011, a management protocol was established and all patients presenting with AUGIH were admitted and managed according to the protocol. Patients at high risk were identified. A standardized protocol contributes to improved management of bleeding by encouraging early provision of the most appropriate therapeutic interventions according to local conditions.[6]
One thousand patients admitted with AUGIH to our government hospital in Egypt were analyzed. Thirty-six percent of patients were ≥60 years of age. Eighty-eight percent were emergency admissions and 12% were inpatients at the time of bleeding. Sixty-eight percent had major comorbidity and 50% had liver disease. Seven hundred and twenty-four patients (72%) underwent endoscopy during admission of whom 537 (74%) had a high-risk bleed. Endoscopy was performed within 24 h of presentation in 75% of these patients. A national comparative audit in the United Kingdom showed that endoscopy was performed within 24 h of presentation in 50% of patients having medium- to high-risk pre-endoscopy Rockall score (ie, 3 or more).[7]
A bleeding site was detected in 84% of the patients in the present study. A bleeding site could be detected in about 75% of patients in other international studies.[1,6,8] The most common causes of bleeding were varices (31%) and peptic ulcer (28%). Two hundred and twenty-four patients with endoscopically diagnosed bleeding varices received endoscopic therapy at the time of initial endoscopy, and hemostasis was achieved in 90%. It is reported that the current endoscopic therapies are capable of stopping bleeding in nearly 90% of patients with acute variceal bleeding.[9] Eight patients with endoscopically diagnosed peptic ulcer and a visible vessel or active bleeding were treated with epinephrine injection and hemostasis was achieved in 75% and no patient rebled. The number of patients treated with epinephrine injection was very small for meaningful comparison. It is reported that epinephrine injection results in hemostasis in up to 100% of patients with bleeding peptic ulcers, but 15%–36% of patients rebleed.[10] The addition of a second endoscopic modality such as heat therapy to epinephrine injection (combination therapy) further reduces the risk of bleeding, the need for surgery, and mortality.[11] The unit was recently (2011) supplied with a bipolar electrocoagulation equipment for thermal hemostasis. The overall mortality was 15%. Factors significantly predictive of mortality were age ≥60 years, inpatients, major comorbidities, liver disease, and variceal bleeding. A mortality rate of 15%, 17%, and 21% were reported from Brazil, Tanzania, and Saudi Arabia, respectively.[6,12,13] Previous liver disease and variceal bleeding were important risk factors of mortality.
Six percent of our patients died rapidly on admission without having an endoscopy. Most of them died due to continued or rebleeding. The future plan is to perform endoscopy as soon as patients are stabilized with resuscitation. Perhaps surprising that mortality was increased (not significant) in high-risk patients who underwent endoscopy within 24 h compared with high-risk patients in whom endoscopy was delayed by more than 24 h. There appeared 2 reasons for this. Bleeding stopped spontaneously and there was no active bleeding during endoscopy in most of the patients in whom endoscopy was delayed by more than 24 h.
The present study was carried out to document information on the clinical outcome of patients admitted with AUGIH to a government hospital in Egypt with the intention of encouraging other similar institutions to consider the provision of a protocol led service for these seriously ill patients who require urgent and skilled management. There are no local data or published reports concerning clinical outcome of AUGIH in government hospitals in Egypt. If these hospitals are able to manage patients with AUGIH effectively, it will reduce the morbidity and mortality associated with this condition, one that is a particular problem in Egypt.
CONCLUSION
The most common cause of AUGIH was variceal in origin. Endoscopic therapy was successful in most cases. Mortality after AUGIH was particularly high among elderly patients, inpatients, and those with a major comorbidity, liver disease, and variceal bleeding. Patients with AUGIH can be managed at government hospitals effectively with careful planning and adherence to a well-designed protocol.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Vreeburg EM, Snel P, de Bruijne JW, Bartelsman JF, Rauws EA, Tytgat GN. Acute upper gastrointestinal bleeding in the Amsterdam area: Incidence, diagnosis, and clinical outcome. Am J Gastroenterol. 1997;92:236–43. [PubMed] [Google Scholar]
- 2.Zakaria S, Fouad R, Shaker O, El Akel W, Hashem A, El Aide S, et al. The natural history of untreated symptomatic acute hepatitis C infection in Egypt. Arab J Gastro. 2005;2:131–9. [Google Scholar]
- 3.Courtney AE, Mitchell RM, Rocke L, Johnston BT. Proposed risk stratification in upper gastrointestinal haemorrhage: Is hospitalisation essential? Emerg Med J. 2004;21:39–40. doi: 10.1136/emj.2003.012328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Palmer KR. Non-variceal upper gastrointestinal haemorrhage: Guidelines. Gut. 2002;51(Suppl 4):41–6. doi: 10.1136/gut.51.suppl_4.iv1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cello JP, Grendell JH, Crass RA, Weber TE, Trunkey DD. Endoscopic sclerotherapy versus portacaval shunt in patient with severe cirrhosis and acute variceal hemorrhage.Long-term follow-up. N Engl J Med. 1987;316:11–5. doi: 10.1056/NEJM198701013160103. [DOI] [PubMed] [Google Scholar]
- 6.Zaltman C, Souza HS, Castro ME, Sobral Mde F, Dias PC, Lemos V., Jr Upper gastrointestinal bleeding in a Brazilian hospital: A retrospective study of endoscopic records. Arq Gastroenterol. 2002;39:74–80. doi: 10.1590/s0004-28032002000200002. [DOI] [PubMed] [Google Scholar]
- 7.UK Comparative Audit of Upper Gastrointestinal Bleeding and the Use of Blood. 2007. Dec, [Last accessed on 2011 May 8]. Available from: http://www.bsg.org.uk/clinical/general/uk-upper-gi-bleeding-audit.html .
- 8.Rockall TA, Logan RF, Devlin HB, Northfield TC. Incidence of and mortality from acute upper gastrointestinal haemorrhage in the United Kingdom.Steering Committee and Members of the National Audit of Acute Upper Gastrointestinal Haemorrhage. BMJ. 1995;311:222–6. doi: 10.1136/bmj.311.6999.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharara AI, Rockey DC. Gastroesophageal variceal hemorrhage. N Engl J Med. 2001;345:669–81. doi: 10.1056/NEJMra003007. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson CB, Mitchell RM. Non-variceal upper gastrointestinal bleeding. Ulster Med J. 2006;75:32–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Calvet X, Vergara M, Brullet E, Gisbert JR, Campo R. Addition of a second endoscopic treatment following epinephrine injection improves outcome in high-risk bleeding ulcers. Gastroenterology. 2004;126:441–50. doi: 10.1053/j.gastro.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 12.Suba M, Ayana S, Mtabho C, Kipiki G. The aetiology, management and clinical outcome of upper gastrointestinal bleeding among patients admitted at the Kilimanjaro Christian Medical Centre in Moshi, Tanzania. Tanzan J Health Res. 2010;12:1–5. doi: 10.4314/thrb.v12i4.51073. [DOI] [PubMed] [Google Scholar]
- 13.Qari FA. Major Causes of Upper Gastrointestinal Bleeding at King Abdul Aziz University Hospital (Jeddah) Kuwait Med J. 2001;33:127–30. [Google Scholar]


