Abstract
Objective
To examine the factor structure of Attention-Deficit/Hyperactivity Disorder (ADHD) in a clinical sample of 1373 children and adolescents with ADHD and their 1772 unselected siblings recruited from different countries across a large age range. Hierarchical and correlated factor analytic models were compared separately in the ADHD and sibling samples, across three different instruments and across parent and teacher informants. Specific consideration was given to factorial invariance analyses across different ages and different countries in the ADHD sample.
Method
A sample of children and adolescents between 5 and 17 years of age with ADHD and their unselected siblings was assessed. Participants were recruited from seven European countries and Israel. ADHD symptom data came from a clinical interview with parents (PACS) and questionnaires from parents and teachers (Conners Parent and Teacher).
Results
A hierarchical general factor model with two specific factors best represented the structure of ADHD in both the ADHD and unselected sibling groups, and across informants and instruments. The model was robust and invariant with regard to age differences in the ADHD sample. The model was not strongly invariant across different national groups in the ADHD sample, likely reflecting severity differences across the different centers and not any substantial difference in the clinical presentation of ADHD.
Conclusions
The results replicate previous studies of a model with a unitary ADHD component and separable specific traits of inattention and hyperactivity/impulsivity. The unique contribution of this study was finding support for this model across a large developmental and multinational/multicultural sample and its invariance across ages.
Keywords: ADHD, hierarchical models, bifactor model, factorial invariance
Attention-Deficit/Hyperactivity Disorder (ADHD) is characterized by problems with attention, impulsivity, and hyperactivity. The diagnosis derives from 18 symptoms indexing these behavioural domains [American Psychiatric Association (APA), DSM-IV-TR, 2000]. There is substantial continuity in maintaining a diagnosis of ADHD from childhood to adolescence (Faraone, Biederman, & Mick, 2006); however the phenotypic expression is highly variable within the diagnosed group and across time (Barkley, 2006; Nigg, 2006). Current diagnostic formulations distinguish between symptoms of inattention and those of hyperactivity-impulsivity. Three ADHD subtypes are recognized in the DSM-IV: the predominantly inattentive type, the predominantly hyperactive-impulsive type, and the combined type (where patients meet criteria on both the inattention and the hyperactive/impulsivity domains). This formulation is currently under review as part of the deliberation of the DSM-5 panel. Indeed, this current characterization remains controversial (Barkley, 2001; Diamond, 2005; Hinshaw, 2001; Lahey, 2001; Milich, Balentine, & Lynam, 2001).
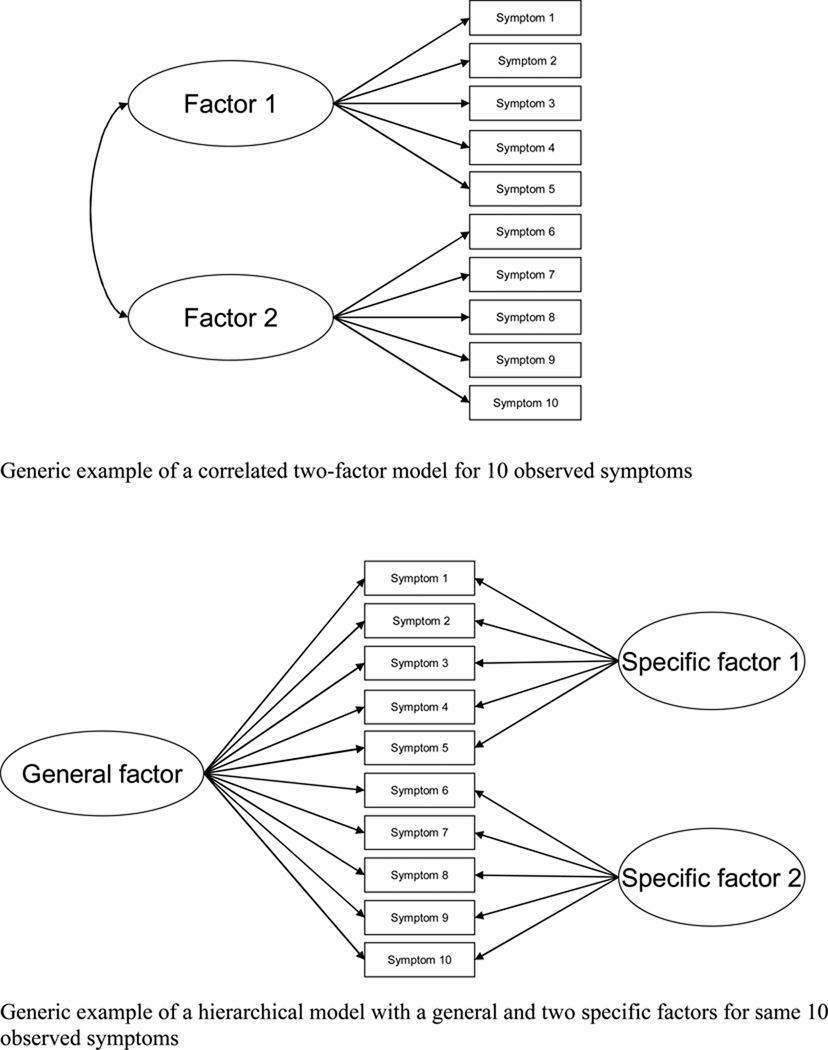
Here we focus on factor models of co-occurrence among ADHD symptoms. Two major types of factor models, correlated factor models and hierarchical models, have been used to examine coherence and distinctness among ADHD symptom domains. Hierarchical models provide a way to simultaneously conceptualize both the coherence and separability of symptoms from separate domains. These models include a single general factor accounting for covariation among all symptoms along with separate, specific factors of inattention, hyperactivity, and impulsivity that vary orthogonally from the general factor. These models are also termed as bifactor models in the statistical literature. Hierarchical models are different from correlated factor models that only have factors for the symptom domains of inattention and hyperactivity and/or impulsivity (see Figure 1). Several studies have shown hierarchical models with a general factor as having a better fit than correlated models for reported symptoms of ADHD (e.g., Dumenci, McConaghy, & Achenbach, 2004; Gibbins et al., in press; Martel, Von Eye, & Nigg, 2010; Toplak et al., 2009). These papers span clinical and community samples, and child, adolescent, and adult samples with ADHD. A one-factor model has also been considered, but thus far it has no empirical support (Dumenci et al., 2004).
Figure 1.
Generic example of a correlated two-factor model for 10 observed symptoms
Generic example of a hierarchical model with a general and two specific factors for same 10 observed symptoms
Hierarchical models explicitly acknowledge the common covariation among all ADHD symptoms, which is consistent with the conceptualization of ADHD as a single disorder. There are several lines of evidence suggesting that there is substantial commonality between the domains of inattention and hyperactivity-impulsivity. Inattentive symptoms tend to be more highly correlated with hyperactivity and impulsivity than with other domains of psychopathology (Adams, Kelley, & McCarthy, 1997; Conners, 2008; Strickland et al., 2011), with the exception of oppositional defiant disorder in some studies (Lahey et al., 2008). Current models of ADHD also highlight how the symptom domains of inattention, hyperactivity, and impulsivity likely interact to give rise to the heterogeneous expression of ADHD (Nigg & Casey, 2005; Sagvolden, Johansen, Aase, & Russell, 2005; Sonuga-Barke, 2005; Sonuga-Barke, Sergeant, Nigg, & Willcutt, 2008). To replicate and extend these findings, the current study examined different factor models in a large sample of ADHD patients recruited from a broad age range and from diverse national groupings. We were thus able to test whether a hierarchical model held for the whole sample and whether it also was invariant across different age groups and nationalities.
A developmental perspective is important to integrate into models of individual ADHD symptoms, such that a single set of factors could parsimoniously explain the changes that occur over development. Age differences in scores from ADHD measures may reflect true differences in the constructs being measured or may simply reflect measurement differences due to age. Therefore, establishing measurement invariance across age groups is important. The behavioural presentation of ADHD changes considerably from childhood to adolescence. For instance, the expression of hyperactivity seems to decrease from childhood to adolescence and inattention commonly appears later in development than hyperactivity and impulsivity (Biederman et al., 2000; Hart et al., 1995; Larsson et al., 2006; Nigg, 2006). This developmental change introduces complex issues with respect to diagnosis. Subtypes have been used to characterize these different symptom presentations, and the instability of ADHD subtypes in developmental samples has also been well demonstrated (Lahey, Pelham, Loney, Lee, & Willcutt, 2005; Todd et al., 2008). Some of this instability of subtypes may be attributable to measurement variability (Lahey et al., 2005; Valo & Tannock, 2010); however some of this variability would be expected from a developmental perspective, which would presume that children’s symptom presentations change over the course of development. What is needed is a coherent model that can represent these shifts and changes in symptoms.
In addition to the question of developmental change and continuity in ADHD symptoms, the current sample also had the unique characteristic of having recruited participants from seven European countries and Israel by 12 different research centers. Most studies examining cross-national samples have been concerned with whether there are comparable rates of prevalence across different countries (Faraone, Sergeant, Gillberg, & Biederman, 2003; Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007) rather than consistency in symptom patterns across countries. In addition to testing the five different factor models in the full sample, invariance analyses were also conducted to examine consistency of the best overall model across countries.
Thus, in the current study we first estimated five different factor models to determine which model best accounted for ADHD symptoms pooling all ages and locations using a sample of children and adolescents with ADHD and their siblings. The five factor structures included: a) a one-factor model of inattention/ hyperactivity/impulsivity; b) a non-hierarchical two-factor model with correlated inattention and hyperactivity/impulsivity factors (the correlated 2-factor model); c) a non-hierarchical three-factor model with correlated inattention, hyperactivity, and impulsivity factors (the correlated 3-factor model); d) a hierarchical model of a general ADHD factor with two specific factors of inattention and hyperactivity/impulsivity (the hierarchical 2-factor model); and e) a hierarchical model of a general ADHD factor with three specific factors of inattention, hyperactivity, and impulsivity (the hierarchical 3-factor model).
Based on previous research, we expected that a hierarchical model with a general ADHD factor would provide the best fit to observed ADHD symptoms in both the ADHD and sibling samples and across instruments and informants. We then examined whether these modeled relationships among symptoms are equivalent across different groups by formally assessing measurement invariance in the ADHD group. Group differences in observed scores on measurement instruments can be attributed to true differences on the constructs being measured only if measurement invariance or equivalence holds across groups (e.g., Widaman & Reise, 1997). Based on the best fitting model, we conducted invariance analyses to determine whether the measurement parameters relating the constructs implied by the model to the observed symptoms are equivalent across age groups and locations in the ADHD group.
Method
Participants and Procedure
Participants included 1373 ADHD proband children (87% males; aged 5 to 17 years, Mean age = 10.95, SD = 2.78) and their 1772 unselected siblings (50.2% male; Mean age= 10.87, SD=3.36), with reports from parents and teachers. Participants were recruited if they were diagnosed or suspected to meet criteria for ADHD combined subtype, as defined by the DSM-IV-TR (2000). Most of the ADHD proband children met criteria for ADHD combined subtype (n = 1217; 88.6%). A smaller proportion met criteria for the hyperactive/impulsive subtype (n = 27; 2.0%) or the inattentive subtype (n = 53; 3.9%), and 76 children did not meet criteria for ADHD (5.5%). The unselected siblings contained children and adolescents with ADHD symptoms on the whole continuum. The PACS interview was administered for the siblings only in cases of suspected ADHD, and the Conners Parent and Teacher forms were administered for all of the siblings included in this study. The data were obtained from the International Multicentre ADHD Genetics (IMAGE) project which includes a total of eight countries, specifically seven European countries (Belgium, England, Germany, Ireland, Spain, Switzerland, and The Netherlands) and Israel. This research meets ethical guidelines and adherence to the legal requirements of each study country. This project involved the collection of behavioural data from 1400 proband-sibling pairs and molecular genetic data on the children and their parents. Full details on this sample are reported in Müller et al. (2011a; 2011b).
Measures
Parental Account of Childhood Symptoms (PACS)
An adapted version of the PACS interview was used in the IMAGE study (see Chen et al., 2008; Müller et al., 2011a). The ADHD section of the PACS was included in this study, assessing for inattentive behavior (9 symptoms), hyperactive behavior (6 symptoms), and impulsive behavior (3 symptoms). In this interview, parents were asked to rate the frequency or severity of behaviors in prespecified contexts (when child was unmedicated), which were then mapped onto a scale with specific categories for each question. Parents were asked to rate their child’s behaviour not in terms of deviance from normality, but rather by describing the behaviour according to its frequency or severity. The ADHD-section of the PACS, which was used to confirm the ADHD diagnosis, covered ADHD-related behaviour in different situations (such as watching TV and doing homework). A specific age-adjusted algorithm combined and weighed the rated behaviour across situations ultimately leading to a dichotomous score for the presence or absence of the corresponding ADHD DSM-IV symptom.
Conners Parent and Teacher Ratings
The Conners rating scales (CPRS-R:L; CTRS-R:L; Conners, 1997) were completed by parents and teachers. Each scale contained a subset of 18 questions covering the DSM-IV ADHD symptoms. Each item had a 4-point response scale.
Statistical Approach
The entire ADHD sample was used for confirmatory factor analysis (CFA) to assess the best fitting model among hypothetical candidates. Because the PACS symptoms have a dichotomous response scale and the Conners rating scale items have a four-point response scale, all models were fitted to the matrix of polychoric correlations among symptoms to account for their categorical nature using a “robust” weighted least-squares estimator (see Flora & Curran, 2004), implemented as the mean- and variance-adjusted weighted least squares (WLSMV) estimator in Mplus (version 5.2; Muthén & Muthén, 2002). Model fit was evaluated using the root mean square error of approximation (RMSEA), comparative-fit index (CFI), and Tucker-Lewis index (TLI) with good model fit indicated by RMSEA values of 0.08 or lower along with CFI and TLI values of 0.95 or higher.
Invariance analyses were conducted comparing three different age groups (9 years and under, 10–12 years, and 13 years and older) in the current sample to determine whether the measurement properties of the instruments are equivalent across age with respect to the ADHD constructs. Invariance analyses were also conducted with different locations according to the following groupings based on language: Belgium and The Netherlands (n = 439), United Kingdom and Ireland (n = 431), Germany and Switzerland (n = 205), and Israel (n = 249). Spain was not included in the invariance analyses due to small sample size (n = 77). Sample sizes and means on the instruments for the ADHD group and the unselected siblings group are shown in Tables 1 and 2. These indices are also reported by each age group and location for the ADHD group.
Table 1.
Sample Characteristics
| Total ADHD Sample |
Ages 9 and under (ADHD) |
Ages 10 to 12 (ADHD) |
Ages 13 and older (ADHD) |
Unselected Siblings |
|
|---|---|---|---|---|---|
| M age (SD) | 10.95 (2.78) | 7.83 (1.12) | 10.98 (.82) | 14.31 (1.30) | 10.87 (3.336) |
| Mean # PACS parent reported symptoms (SD) | |||||
| N | 1373 | 450 | 512 | 411 | 401 |
| Total ADHD | 13.73 (3.04) | 13.63 (2.97) | 13.90 (3.04) | 13.62 (3.12) | 10.78 (4.58) |
| Inattention | 6.81 (1.65) | 6.62 (1.65) | 6.90 (1.64) | 6.93 (1.65) | 5.62 (2.45) |
| Hyperactivity and Impulsivity |
6.91 (2.00) | 7.02 (1.91) | 7.01 (1.97) | 6.69 (2.11) | 5.15 (2.87) |
| Mean rating on Conners Parent (SD) | |||||
| N | 1340 | 441 | 500 | 398 | 1770 |
| Total ADHD | 37.11 (9.26) | 37.58 (9.18) | 37.12 (8.78) | 36.55 (9.92) | 16.63 (23.71) |
| Inattention | 19.47 (5.11) | 18.99 (5.04) | 19.52 (4.91) | 19.94 (5.40) | 9.43 (15.47) |
| Hyperactivity and Impulsivity |
17.64 (5.62) | 18.58 (5.40) | 17.60 (5.38) | 16.65 (5.98) | 7.21 (13.70) |
| Mean rating on Conners Teacher (SD) | |||||
| N | 1269 | 425 | 476 | 358 | 1679 |
| Total ADHD | 30.50 (11.33) | 33.35 (10.80) | 30.16 (11.04) | 27.52 (11.53) | 19.40 (46.00) |
| Inattention | 16.37 (6.07) | 17.17 (6.00) | 16.30 (5.90) | 15.57 (6.26) | 11.15 (28.07) |
| Hyperactivity and Impulsivity |
14.08 (6.86) | 16.10 (6.47) | 13.81 (6.76) | 12.01 (6.79) | 8.14 (24.55) |
Table 2.
Sample Characteristics of ADHD Sample by Country Groupings
| Ireland and United Kingdom |
Belgium and The Netherlands |
Germany and Switzerland |
Israel | |
|---|---|---|---|---|
| M age (SD) | 11.68 (2.86) | 11.11 (2.72) | 10.30 (2.32) | 10.41 (2.81) |
| Mean Number of PACS parent reported symptoms (SD) | ||||
| N | 427 | 439 | 205 | 235 |
| Total ADHD | 14.18 (3.07) | 14.10 (2.64) | 14.01 (3.10) | 12.66 (3.15) |
| Inattention | 7.02 (1.68) | 6.88 (1.65) | 6.94 (1.51) | 6.51 (1.59) |
| Hyperactivity and Impulsivity |
7.16 (1.97) | 7.22 (1.64) | 7.07 (2.06) | 6.17 (2.22) |
| Mean Ratings on Conners Parent (SD) | ||||
| N | 386 | 417 | 194 | 224 |
| Total ADHD | 40.62 (9.22) | 36.31 (8.47) | 34.95 (9.40) | 33.33 (9.34) |
| Inattention | 21.34 (4.96) | 18.91 (4.85) | 18.57 (5.21) | 17.60 (5.18) |
| Hyperactivity and Impulsivity |
19.36 (5.69) | 17.36 (5.15) | 16.33 (5.74) | 15.71 (5.84) |
| Mean Ratings on Conners Teacher (SD) | ||||
| N | 354 | 402 | 188 | 201 |
| Total ADHD | 27.34 (12.83) | 29.32 (10.12) | 32.70 (10.82) | 32.86 (9.89) |
| Inattention | 15.12 (6.86) | 15.41 (5.55) | 17.78 (5.68) | 17.72 (5.49) |
| Hyperactivity and Impulsivity |
12.21 (7.50) | 13.92 (6.13) | 14.91 (7.00) | 14.96 (6.45) |
To test factorial invariance across age and location in the ADHD group, we followed procedures outlined by Widaman and Reise (1997) using a series of nested multiple-group CFA models. Although nested model comparisons often rely on χ2 difference tests, recent methodological research suggests that examining alternative fit indices is preferable because the χ2 statistic is overly sensitive to sample size and ignores model parsimony. Thus, in the current analyses two models were considered to have equivalent fit if the decrease in CFI (ΔCFI) was .01 or less and if the increase in RMSEA (ΔRMSEA) was not greater than .01 (Chen, 2007, Cheung & Rensvold, 2002).
To establish configural invariance in the ADHD group, we examined the fit of a two-group model in which the basic model specification was identical across groups, but all parameters were free to vary across groups (except those needed for overall model identification; see Millsap & Yun-Tein, 2004). Next, to test weak invariance, the fit of the initial configural invariance model was compared to that of a model with all factor loadings constrained equal across groups. If weak invariance held, we then tested strong invariance by comparing the fit of the weak invariance model to that of a model with all factor loading and all symptom threshold parameters constrained to equality across groups. However, because PACS items are dichotomous, model identification requires equal thresholds across groups (Millsap & Yun-Tein, 2004); thus, a weak invariance model with constrained loadings and freed thresholds is not estimable, while the PACS configural invariance model has freed loadings and constrained thresholds.
Results
The correlations between age and total scores for all 18 ADHD symptoms in the ADHD group were non-significant for the PACS interview and Conners Parent scale and significant for the Conners Teacher scale (r = −.23, p < .001). Age was not significantly correlated with inattention or hyperactivity/impulsivity ratings for all three instruments. Overall, correlations between age and ADHD symptoms were very small or non-significant.
CFA Model Selection
The 18 ADHD symptoms from the PACS parent interview and Conners Parent and Teacher scales were fitted to separate CFA models for each of these three instruments. The model fit statistics for the total ADHD sample are presented in Table 3. Across all three instruments, the hierarchical models had RMSEA values below .07 and demonstrated a better fit than the correlated models across both instruments and informants (although for the PACS, CFI and TLI did not meet conventional criteria for good fit). Within each instrument and informant, the hierarchical 2-factor and 3-factor models had very similar model fit. We focus our remaining results on the hierarchical model with two specific factors because it is more parsimonious than the model with three specific factors.
Table 3.
Fit of ADHD Symptom CFA Models by Instrument for ADHD Sample
| Model | df | χ2 | CFI | TLI | RMSEA | RMSEA 90% CI |
|---|---|---|---|---|---|---|
| Parent PACS (N = 1374) | ||||||
| One-factor model | 135 | 1050.41 | .790 | .761 | .070 | .066 – .074 |
| Correlated 2-factor | 134 | 786.54 | .850 | .829 | .060 | .056 – .064 |
| Correlated 3-factor | 132 | 752.65 | .857 | .835 | .059 | .054 – .063 |
| Hierarchical 2-factor | 117 | 426.54 | .929 | .907 | .044 | .039 – .048 |
| Hierarchical 3-factor | 117 | 417.11 | .931 | .910 | .043 | .039 – .048 |
| Parent Conners (N = 1388) | ||||||
| One-factor model | 135 | 2862.17 | .798 | .771 | .121 | .117 – .125 |
| Correlated 2-factor | 134 | 1375.37 | .908 | .895 | .082 | .078 – .086 |
| Correlated 3-factor | 132 | 1350.76 | .910 | .895 | .082 | .078 – .086 |
| Hierarchical 2-factor1 | 117 | 709.24 | .956 | .943 | .060 | .056 – .065 |
| Teacher Conners (N = 1350) | ||||||
| One-factor model | 135 | 4324.05 | .810 | .785 | .152 | .148 – .156 |
| Correlated 2-factor | 134 | 2197.52 | .906 | .893 | .107 | .103 – .111 |
| Correlated 3-factor | 132 | 2076.51 | .912 | .898 | .105 | .101 – .109 |
| Hierarchical 2-factor | 117 | 828.58 | .968 | .958 | .067 | .063 – .072 |
| Hierarchical 3-factor | 117 | 867.45 | .966 | .955 | .069 | .065 – .073 |
Note. df = degrees of freedom; χ2 = chi-square fit statistic; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root Mean Square Error of Approximation.
Fit statistics are not reported for the hierarchical 3-factor model for the Parent Conners instrument because the estimator did not converge to a proper solution.
Across all three instruments, all symptoms had significant, positive loadings on the general ADHD factor (all ps < 0.05; see Table 4 for standardized factor loading estimates and R2 values), with the exception of the “Does not seem to listen” symptom from the PACS interview. With the Conners Parent and Conners Teacher instruments, most inattention items were slightly more strongly related to their specific factor than the general factor, whereas this pattern was more mixed for the PACS inattention symptoms. For all three instruments, the hyperactivity/impulsivity symptoms were all more strongly related to the general factor than to their specific factor (except the “Blurts out answers” PACS symptom).
Table 4.
Completely Standardized Factor Loadings for Hierarchical 2-Factor Model Fitted for Parent PACS Interview, Parent Conners (CP), and Teacher Conners (CT) Across Full ADHD Sample
| Factor |
||||||||||||
| ADHD Symptom | General | Specific Ina | Specific Hyp/Imp | R2 | ||||||||
| PACS | CP | CT | PACS | CP | CT | PACS | CP | CT | PACS | CP | CT | |
| 1. Fails to give attention and makes careless mistakes. |
.357 | .399 | .359 | .628 | .551 | .555 | .522 | .464 | .438 | |||
| 2. Difficulty sustaining attention. | .589 | .451 | .526 | −.019 | .434. | .538 | .347 | .392 | .567 | |||
| 3. Does not seem to listen. | .021 | .581 | .513 | .249 | .299 | .382 | .062 | .427 | .410 | |||
| 4. Does not follow through on instructions. | .320 | .399 | .371 | .259 | .639 | .597 | .169 | .567 | .494 | |||
| 5. Difficulty organizing tasks. | .279 | .348 | .364 | .511 | .628 | .700 | .338 | .516 | .622 | |||
| 6. Avoids tasks that require sustained mental effort. |
.304 | .343 | .386 | .324 | .612 | .529 | .197 | .492 | .429 | |||
| 7. Loses things. | .322 | .325 | .370 | .729 | .545 | .520 | .635 | .402 | .407 | |||
| 8. Easily distracted. | .358 | .601 | .712 | .442 | .330 | .312 | .323 | .470 | .605 | |||
| 9. Often forgetful. | .269 | .375 | .160 | .698 | .583 | .557 | .559 | .481 | .336 | |||
| 10. Often fidgets. | .751 | .594 | .710 | .131 | .164 | −.084 | .581 | .380 | .511 | |||
| 11. Leaves seat in class. | .727 | .578 | .752 | −.075 | .187 | −.163 | .534 | .369 | .592 | |||
| 12. Runs about or climbs excessively | .729 | .686 | .765 | −.012 | .454 | −.209 | .531 | .676 | .628 | |||
| 13. Difficulty playing quietly. | .655 | .623 | .547 | .416 | .038 | .123 | .602 | .389 | .314 | |||
| 14. Always “on the go.” | .902 | .632 | .737 | −.202 | .301 | −.033 | .854 | .490 | .545 | |||
| 15. Often talks excessively. | .506 | .535 | .640 | .200 | −.138 | .265 | .296 | .305 | .480 | |||
| 16. Blurts out answers. | .525 | .649 | .642 | .639 | −.235 | .399 | .684 | .477 | .572 | |||
| 17. Difficulty waiting in lines. | .318 | .715 | .727 | .214 | −.009 | .350 | .147 | .512 | .652 | |||
| 18. Often interrupts. | .585 | .725 | .691 | .109 | −.229 | .347 | .354 | .578 | .599 | |||
Note. All factor loadings are significant (p < .05) except those in italics.
Overall, these findings confirm that a single, dominant general factor underlies all 18 DSM-IV ADHD symptoms along with separate specific factors accounting for residual covariation among symptoms from the same domain (i.e., inattention and hyperactivity/impulsivity). A larger proportion of the variance in hyperactive/impulsive symptoms was consistently associated with the general factor, whereas a larger proportion of the variance in inattentive symptoms was consistently associated with the inattention specific factor. For the PACS, the general factor explains only 11.69% of total variance for the inattention symptoms, while the inattention specific factor explains 23.38% of total inattention symptom variance. But, the general factor explains 42.68% of total variance for the hyperactivity/impulsivity symptoms, while the hyperactivity specific factor explains only 8.25% of total hyperactivity/impulsivity symptom variance. For the Conners parent report, the general factor accounts for 18.95% of inattention symptom variance and specific factor accounts for 27.83%. The general factor accounts for 40.99% of hyperactive/impulsive symptom variance and the specific factor accounts for only 5.41% of variance in these symptoms. For the Conners teacher report, the general factor accounts for 19.53% of inattention symptom variance and the specific factor accounts for 28.31%. The general factor accounts for 48.06% of hyperactive/impulsive symptom variance and the specific factor accounts for only 6.29% of variance in these symptoms.
The five models were also estimated in the sample of unselected siblings. For each of these instruments, the hierarchical 2-factor and 3-factor models had better fit than any of the non-hierarchical models. In fact, the hierarchical 2-factor and 3-factor models had the same values for the model fit indices (PACS: CFI=.96, TLI=.95, RMSEA=.06; Conners Parent: CFI=.99, TLI=.99, RMSEA=.07; Conners Teacher: CFI=.99, TLI=.99, RMSEA=.06).
Measurement Invariance Across Age and Location in the ADHD group
We examined factorial invariance by age for the hierarchical two-factor model separately for the three instruments, each time assessing invariance for the age 9 and under group compared to the age 10 to 12 group, and then comparing the age 10 to 12 group to the age 13 and older group. Strong factorial invariance holds across age groups for all three instruments in the ADHD group. Thus, the measurement properties of the PACS and Conners questionnaires are equivalent across age with respect to relating the ADHD constructs implied by the hierarchical factor models to the 18 observed symptoms. The results of the invariance analyses are presented in supplemental tables available online.
Next, we examined factorial invariance by location for the hierarchical two-factor model separately for the three instruments in the ADHD group. We estimated a series of two-group models, making all possible pairwise comparisons between the four country groupings (i.e., 1. Ireland/UK, 2. The Netherlands/Belgium, 3. Germany/Switzerland, and 4. Israel). For the PACS interview, strong invariance held between Holland/Belgium and each of the other locations. However, strong invariance was rejected across Ireland/UK versus both Germany/Switzerland and Israel and across Germany/Switzerland versus Israel. Therefore, while the hierarchical two-factor model fits the PACS data well across all locations (i.e., configural invariance), there is some variation in the factor loadings for this model as a function of location.
For the Conners Parent Scale, strong invariance held across all location comparisons with the exception of Ireland/UK versus Holland/Belgium and Ireland/UK versus Israel, for which weak invariance held but strong invariance was rejected. Similarly, for the Conners Teacher Scale, strong invariance held across all location comparisons with the exception of Ireland/UK versus Holland/Belgium and Holland/Belgium versus Israel, for which weak invariance held but strong invariance was rejected. Therefore, for both the Conners Parent and Conners Teacher scales, factor loadings for the hierarchical model are equivalent across all locations, but there is some variation in the individual symptom thresholds (i.e., rates of symptom endorsement for a given level of the unobserved constructs) across location.
Discussion
The present study compared five factor models to determine the best representation of the relationships among the ADHD symptoms from the dimensions of inattention and hyperactivity-impulsivity using a sample of 1373 children referred for ADHD and 1772 unselected siblings. Across all three instruments and across parent and teacher informants, the hierarchical, general factor model with two or three specific factors had a better fit than the single factor or correlated factor models. Invariance analyses indicated strong invariance across age but strong invariance was not obtained consistently across locations in the ADHD group.
The current findings replicate previous research that has shown the hierarchical or bifactor model to be a better fitting model than correlated factor models of ADHD symptoms (Dumenci et al., 2004; Gibbins et al., in press; Martel et al., 2010; Toplak et al., 2009). Importantly, the replication in the current study was obtained in the ADHD sample, as well as in the unselected siblings. The hierarchical models with two and three specific factors both fit the data well, but the model with two specific factors was interpreted as was the more parsimonious model. The pattern of loadings suggests that the hyperactive-impulsive symptoms were more strongly and consistently related to the general factor than were the inattentive symptoms. Inattentive symptoms also significantly loaded onto the general factor, but with more inconsistency in the strength of their relationships to both general and specific factors. The hyperactive-impulsive symptoms may have been reported with consistently more variability than inattention symptoms, reflecting the predominance of these symptoms in childhood. This hierarchical model accounted for 35% to 48% of the total variance in reported symptoms of inattention and 46% to 54% for symptoms of hyperactivity-impulsivity (depending on the instrument). The finding of the common and separate variance among the symptom domains of ADHD is reflected in the findings from quantitative genetic studies (Greven, Rijsdijk, & Plomin, 2011; McLoughlin, Ronald, Kuntsi, Asherson, & Plomin, 2007). Using population twins samples, these studies consistently found that the symptom domains of ADHD are influenced by partially overlapping sets of genes, with genetic influences that are shared between the two domains, in addition to domain-specific genetic influences.
The fact that strong invariance was obtained across three different age groups in the ADHD sample suggests that the general factor model is robust and equivalent across age with respect to the ADHD latent constructs generated from the 18 symptoms. This finding underscores the importance of continuities of relationships among ADHD symptoms across development. An integral and possibly interactive relationship between inattentive and hyperactive/impulsive symptoms has been demonstrated longitudinally in children and in quantitative genetic studies of ADHD. Ratings of hyperactivity-impulsivity in childhood have been shown to predict inattentiveness in early adolescence, but the reverse was not found (Greven, Asherson, Rijsdijk, & Plomin, 2011). These authors suggested that hyperactivity-impulsivity may exacerbate inattentive symptoms over time, although the mechanisms involved remain unclear and could involve behavioural, cognitive, or neurobiological pathways. In another longitudinal study examining trajectories of ADHD symptoms, hyperactivity-impulsivity symptoms decreased over time, whereas inattention symptoms increased over time (Larsson, Dilshad, Lichtenstein, & Barker, 2011). These results were interpreted as potentially explaining the developmental trajectories from hyperactive-impulsive to combined subtype in early to middle childhood and from the combined to inattentive subtype during the later transition to adolescence and young adulthood (Biederman et al., 2000; Hart et al., 1995).
In general, twin studies have shown that genetic influences on composite measures of ADHD are largely stable (Kuntsi, Rijsdijk, Ronald, Asherson, & Plomin, 2005; Larsson, Larsson, & Lichtenstein, 2004; Price, Simonoff, Asherson, Curran, Kuntsi, Waldman, et al., 2005), although there are new genetic influences acting on ADHD at different ages. The developmental relationship between inattention and hyperactivity-impulsivity is also influenced by shared genetic influences, with both new and stable genetic effects at different developmental stages (Larsson et al., 2006; Nadder, Rutter, Silberg, Maes, & Eaves, 2002; Greven et al., 2011). Moreover, during adolescent development, more than half of the genetic influences acting on the two symptoms domains were novel effects (Greven et al., 2011), which might be related to the developmental changes seen in the balance between inattentive and hyperactive-impulsive symptoms.
From a developmental perspective, it is also important to explain how inattention and hyperactivity-impulsivity are related to cognitive performance and behavioural phenotypes, although no consistent picture has emerged yet. Inattention has been reported to be strongly associated with executive function difficulties (Chhabildas, Pennington, & Willcutt, 2001; Nigg et al., 2005), whereas delay discounting has been associated with hyperactive-impulsive symptoms (Scheres, Lee, & Sumiya, 2008), though not consistently (Paloyelis, Asherson, Mehta, Faraone, & Kuntsi, 2010). Both of these general domains uniquely predicted ADHD symptoms in child samples (Campbell & von Stauffenberg, 2009; Sonuga-Barke, Dalen, & Remington, 2003). That these two domains have been implicated in ADHD has been a key component in dual-pathway conceptualizations of ADHD, in which executive and motivational pathways are not regarded as competing theories, rather that deficits in both processes are thought to give rise to the manifestation of ADHD (Sonuga-Barke, 2002; Sonuga-Barke 2003; Sonuga-Barke, 2005). Understanding the overlap and separability between these pathways will be critical for explaining the heterogeneity observed in ADHD. Halperin and Schulz (2006; Halperin, Trampush, Miller, Marks, & Newcorn, 2008) have used a developmental perspective to explain symptom change in ADHD as reflecting the degree to which prefrontally mediated executive functions develop and can compensate for stable subcortical deficits. Such developmental theories will play an important role in explaining the common and separable variance between inattention and hyperactivity-impulsivity in ADHD.
Strong invariance, however, did not hold consistently across all of the locations in the ADHD group. Notably, the same instruments were used in all locations, with proper training to establish reliable administration (Müller et al., 2011a). Thus, these differences are less likely to be attributable to differences in administration, but may be attributable to the rates of symptom endorsement in some locations. This is consistent with Müller et al.’s (2011a) report on symptom patterns in the IMAGE dataset, where the mean number of symptoms reported differed significantly across several countries. That was also the case in the present study, as participants in Israel had the lowest number of symptoms reported on the PACS (p < .0001), participants in Ireland and the United Kingdom had the highest ADHD ratings on the parent Conners (p < .0001) and lowest rating (with Belgium and The Netherlands) on the teacher Conners (p < .0001). This pattern likely explains why strong invariance was not obtained in the current study across locations. Therefore, the site differences likely reflect severity differences across the clinical ascertainment centers, and not any substantial difference in the clinical presentation of ADHD.
Clinically, the current study also suggests that the current DSM-IV conceptualization for diagnosing ADHD may not be the optimal set of constructs. The current findings support a unitary construct of ADHD, with additional covariation of symptoms manifest in the separate orthogonal factors of inattention and hyperactivity-impulsivity. A focus on specific symptoms or symptom domains may be too narrow in understanding the full clinical presentation of ADHD. A hierarchical factor model accommodates clinical presentations of predominantly inattentive symptoms and acknowledges the presence of levels of hyperactivity-impulsivity that may contribute to the presenting problems. The implications of this model suggest that all 18 symptoms should be rated together to derive a single overall score, with consideration to both inattention and hyperactivity/impulsivity as additional dimensional factors. These scores should all be taken into account in the assessment and treatment of ADHD. This model is therefore different from that implied by the current DSM-IV, as the diagnosis of inattentive and hyperactive/impulsive subtypes tend to disregard the contribution of the other symptom domain. Hierarchical factor models therefore may lend themselves to more dimensional approaches for modeling symptom domains, as opposed to categorical boundaries. Similar implications follow for other diagnostic classifications, such as the ICD-10 (WHO, 2007).
Limitations of the current study were the oversampling of children and adolescents with primarily combined type symptoms in the ADHD sample and the cross-sectional design. However, the hierarchical factor model has been shown to have a good fit in samples with a more substantial representation of youth with primarily inattentive symptoms (Toplak et al., 2009). Nonetheless, it is important to examine this model further in youth with purely inattentive symptoms. Criterion validation studies are also needed to determine whether the separate latent constructs are differentially associated with other variables, such as other forms of psychopathology (in particular, oppositional defiant disorder, Lahey et al., 2008) and executive functions or cognitive processes.
Conclusion
The current study demonstrated that the hierarchical factor model had a better fit compared to a single factor or correlated factor models of ADHD symptoms in a large-scale sample of children and adolescents with ADHD and separately among their siblings. The unique aspects of this sample were the inclusion of multiple countries that represent a diverse set of cultures. The hierarchical factor model, which formally acknowledges the common covariance among the inattention and hyperactive-impulsive symptoms, had the best fit across all age groups and across all locations. These findings were replicated across three different instruments (including a clinical interview and questionnaires) and across parent and teacher informants. The invariance analyses showed strong measurement invariance across age, but not across locations. This model highlights the importance of the common variance of individual symptoms from these separate domains across instruments, informants, and different ages throughout childhood in a large and diverse sample of children with ADHD and their unselected siblings.
Key points.
The current study replicated a hierarchical model with a general ADHD factor and two specific factors of inattention and hyperactivity in a large sample of children and adolescents with ADHD, and separately in their unselected siblings.
This replication extends previous work as consideration was given to different periods of child and adolescent development and different ethic/cultural groups. Strong measurement invariance was obtained holding by age.
A major implication of the general factor is that in addition to deriving a total score across all inattention and hyperactivity/impulsivity symptoms, these symptom domains should also be examined dimensionally and taken into account in the assessment and treatment planning of ADHD. This measurement should be taken even when these levels do not meet the current clinical threshold of six symptoms in each domain, as indicated in the current DSM-IV.
Supplementary Material
Acknowledgements
The IMAGE project is a multi-site, international effort supported by NIH grants R01MH62873 and R01MH081803 to S.V. Faraone. Site Principal Investigators are Philip Asherson, Tobias Banaschewski, Jan Buitelaar, Richard P. Ebstein, Stephen V. Faraone, Michael Gill, Ana Miranda, Fernando Mulas, Robert D. Oades, Herbert Roeyers, Aribert Rothenberger, Joseph Sergeant, Edmund Sonuga-Barke, and Hans-Christoph Steinhausen. Senior coinvestigators are Margaret Thompson, Pak Sham, Peter McGuffin, Robert Plomin, Ian Craig and Eric Taylor. Chief Investigators at each site are Rafaela Marco, Nanda Rommelse, Wai Chen, Henrik Uebel, Hanna Christiansen, U.Mueller, Cathelijne Buschgens, Barbara Franke, Lamprini Psychogiou. We thank all the families who kindly participated in this research.
The following is a list of potential conflicts of interest disclosed. Wai Chen served in an advisory or consultancy role for Shire and Flynn Pharma. He received conference attendance support or received speaker’s fee by Lilly, Flynn Pharma, Janssen, Shire. He is involved in a clinical trial conducted by Shire. He has grant support from NIMH, NIHR and Janssen-Cilag. The present work (funded by NIMH) is unrelated to the above other grants and relationships. Dr. Banaschewski served in an advisory or consultancy role for Bristol Myers-Sqibb, Develco Pharma, Lilly, Medice, Novartis, Shire and Viforpharma. He received conference attendance support and conference support or received speaker’s fee by Lilly, Janssen McNeil, Medice, Novartis, Shire, UCB. He is/has been involved in clinical trials conducted by Lilly, Shire and Novartis. The present work is unrelated to the above grants and relationships. Jan Buitelaar has been in the past 3 years a consultant to/member of advisory board of / and/or speaker for Janssen Cilag BV, Eli Lilly, Bristol-Myer Squibb, Shering Plough, UCB, Shire, Novartis and Servier. He is not an employee of any of these companies, and not a stock shareholder of any of these companies. He has no other financial or material support, including expert testimony, patents, royalties. Robert Oades received some support from Janssen, UCB pharma and Shire. Herbert Roeyers is a member of an Advisory Board to Shire and has received research funding and conference attendance support from Shire and Eli Lilly. Aribert Rothenberger has served on the advisory board and speakers bureau for Lilly, Shire, Medice, Novartis, received research support from German Research Society, Schwaabe, travel support from Shire, an educational grant from Shire, and has been a consultant for UCB/Shire; Lilly. Edmund Sonuga-Barke has served on the recent speaker board for Shire, UCB Pharma, conducted current & recent consultancy for UCB Pharma, Shire, received current & recent research support from Janssen Cilag, Shire, Qbtech, Flynn Pharma, served on the the Advisory Board for Shire, Flynn Pharma, UCB Pharma, Astra Zeneca, and received conference support from Shire. Hans-Christoph Steinhausen has worked as an advisor and speaker for the following pharmaceutical companies: Janssen-Cilag, Eli Lilly, Novartis, Medice, Shire, and UCB. He has received unrestricted grants for postgraduate training courses or conferences and research by Janssen-Cilag, Eli Lilly, Novartis, Medice, and Swedish Orphan International. Margaret Thompson in the last five years has received education sponsorship from Eli Lilley, Janssen-Cilag, Shire, unrestricted research grants from Eli Lilley, Janssen-Cilag, UCB, Shire, had PhD students funded by Eli Lilley, Janssen-Cilag Boards: Eli Lilley, Shire, and received lecture fees from Eli Lilley, Janssen-Cilag. Philip Asherson has consulted with, received educational grants from or spoken at sponsored meetings for Shire, Janssen-Cilag, Eli-Lilly, and Flynn Pharma. In the past year, Dr. Faraone received consulting income and research support from Shire and research support from the National Institutes of Health (NIH). In previous years, he received consulting fees or was on Advisory Boards or participated in continuing medical education programs sponsored by: Shire, McNeil, Janssen, Novartis, Pfizer and Eli Lilly. Dr. Faraone receives royalties from books published by Guilford Press: Straight Talk about Your Child’s Mental Health and Oxford University Press: Schizophrenia: The Facts.
Footnotes
Conflict of interest statement: Funding and potential conflicts disclosed in acknowledgements.
The manuscript was drafted by Maggie Toplak in collaboration with Philip Asherson, Stephen Faraone, and Edmund Sonuga-Barke. The factor analytic analyses were conducted by Geoff Sorge and David Flora. All of the authors reviewed and approved the manuscript.
References
- Adams CD, Kelley ML, McCarthy M. The Adolescent Behavior Checklist: Development and initial psychometric properties of a self-report measure for adolescents with ADHD. Journal of Clinical Child Psychology. 1997;26:77–86. doi: 10.1207/s15374424jccp2601_8. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual for mental disorders. 4th ed. Washington, DC: Author; 2000. [Google Scholar]
- Barkley RA. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 3rd ed. New York: Guilford; 2006. [Google Scholar]
- Barkley RA. The Inattentive type of ADHD as a distinct disorder: What remains to be done. Clinical Psychology: Science and Practice. 2001;8:489–493. [Google Scholar]
- Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: Impact of remission definition and symptom type. American Journal of Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- Campbell SB, von Stauffenberg C. Delay and inhibition as early predictors of ADHD symptoms in third grade. Journal of Abnormal Child Psychology. 2009;37:1–15. doi: 10.1007/s10802-008-9270-4. [DOI] [PubMed] [Google Scholar]
- Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Structural Equation Modeling. 2007;14:464–504. [Google Scholar]
- Chen W, Zhou K, Sham P, Franke B, Kuntsi J, Campbell D, Asherson P. DSM-IV combined type ADHD shows familial association with sibling trait scores: A sampling strategy for QTL linkage. American Journal of Medical Genetics Part B. 2008;147B:1450–1460. doi: 10.1002/ajmg.b.30672. [DOI] [PubMed] [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9:233–255. [Google Scholar]
- Chhabildas N, Pennington BF, Willcutt EG. A comparison of the neuropsychological profiles of the DSM-IV subtypes of ADHD. Journal of Abnormal Child Psychology. 2001;29:529–540. doi: 10.1023/a:1012281226028. [DOI] [PubMed] [Google Scholar]
- Conners CK. Conners 3rdEdition: Manual. Toronto, Canada: Multi-Health Systems Inc; 2008. [Google Scholar]
- Conners CK. Conners’ Rating Scales-Revised: Technical Manual. New York: Multi-Health Systems Inc; 1997. [Google Scholar]
- Diamond A. Attention-deficit disorder (attention-deficit/hyperactivity disorder without hyperactivity): A neurobiologically and behaviorally distinct disorder from attention-deficit/hyperactivity disorder (with hyperactivity) Development and Psychopathology. 2005;17:807–825. doi: 10.1017/S0954579405050388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumenci L, McConaghy SH, Achenbach TM. A hierarchical three-factor model of inattention-hyperactivity-impulsivity derived from the attention problems syndrome of the teacher’s report form. School Psychology Review. 2004;33:287–301. [Google Scholar]
- Faraone S, Biederman J, Mick E. The age dependent decline of Attention-Deficit/Hyperactivity Disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: Is it an American condition? World Psychiatry. 2003;2:104–113. [PMC free article] [PubMed] [Google Scholar]
- Flora DB, Curran PJ. An evaluation of alternative methods for confirmatory factor analysis with ordinal data. Psychological Methods. 2004;9:466–491. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbins C, Toplak ME, Flora DB, Weiss MD, Tannock R. General and specific factors in ADHD: Evidence for a bifactor model of ADHD in adults. Journal of Attention Disorders. doi: 10.1177/1087054711416310. in press. [DOI] [PubMed] [Google Scholar]
- Greven CU, Asherson P, Rijsdijk FV, Plomin R. A longitudinal twin study on the association between inattentive and hyperactive-impulsive ADHD symptoms. Journal of Abnormal Child Psychology. 2011;39:623–632. doi: 10.1007/s10802-011-9513-7. [DOI] [PubMed] [Google Scholar]
- Greven CU, Rijsdijk FV, Plomin R. A twin study of ADHD symptoms in early adolescence: Hyperactivity-impulsivity and inattentiveness show substantial genetic overlap but also genetic specificity. Journal of Abnormal Child Psychology. 2011;39:265–275. doi: 10.1007/s10802-010-9451-9. [DOI] [PubMed] [Google Scholar]
- Halperin JM, Schulz KP. Revisiting the role of the prefrontal cortex in the pathophysiology of attention-deficit/hyperactivity disorder. Psychological Bulletin. 2006;132:560–581. doi: 10.1037/0033-2909.132.4.560. [DOI] [PubMed] [Google Scholar]
- Halperin JM, Trampush JW, Miller CJ, Marks DJ, Newcorn JH. Neuropsychological outcome in adolescents/young adults with childhood ADHD: Profiles of persisters, remitters, and controls. Journal of Child Psychology and Psychiatry. 2008;49:958–966. doi: 10.1111/j.1469-7610.2008.01926.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Applegate B, Frick PJ. Developmental change in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Is the inattentive type of ADHD a separate disorder? Clinical Psychology: Science and Practice. 2001;8:498–501. [Google Scholar]
- Kuntsi J, Rijsdijk F, Ronald A, Asherson P, Plomin R. Genetic influences on the stability of attention-deficit/hyperactivity disorder symptoms from early to middle childhood. Biological Psychiatry. 2005;57:647–654. doi: 10.1016/j.biopsych.2004.12.032. [DOI] [PubMed] [Google Scholar]
- Lahey BB. Should the Combined and Predominantly Inattentive types of ADHD be considered distinct and unrelated disorders? Not now, at least. Clinical Psychology: Science and Practice. 2001;8:494–497. [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Lee SS, Willcutt E. Instability of the DSM- IV subtypes of ADHD from preschool through elementary school. Archives of General Psychiatry. 2005;62:896–902. doi: 10.1001/archpsyc.62.8.896. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Rathouz PJ, Van Hulle C, Urbano RC, Krueger RF, Applegate B, Garriock HA, Chapman DA, Waldman ID. Testing structural models of DSM-IV symptoms of common forms of child and adolescent psychopathology. Journal of Abnormal Child Psychology. 2008;36:187–206. doi: 10.1007/s10802-007-9169-5. [DOI] [PubMed] [Google Scholar]
- Larsson H, Dilshad R, Lichtenstein P, Barker ED. Developmental trajectories of DSM-IV symptoms of attention-deficit/hyperactivity disorder: Genetic effects, family risk, and associated psychopathology. Journal of Child Psychology and Psychiatry. 2011 doi: 10.1111/j.1469-7610.2011.02379.x. [DOI] [PubMed] [Google Scholar]
- Larsson J, Larsson H, Lichtenstein P. Genetic and environmental contributions to stability and change of ADHD symptoms between 8 and 13 years of age: A longitudinal twin study. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:1267–1275. doi: 10.1097/01.chi.0000135622.05219.bf. [DOI] [PubMed] [Google Scholar]
- Larsson H, Lichtenstein P, Larsson J. Genetic contributions to the development of ADHD subtypes from childhood to adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:973–981. doi: 10.1097/01.chi.0000222787.57100.d8. [DOI] [PubMed] [Google Scholar]
- Martel MM, Von Eye A, Nigg JT. Revisiting the latent structure of ADHD: is there a ‘g’ factor? Journal of Child Psychology and Psychiatry. 2010;51:905–914. doi: 10.1111/j.1469-7610.2010.02232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLoughlin G, Ronald A, Kuntsi J, Asherson P, Plomin R. Genetic support for the dual nature of attention deficit hyperactivity disorder: Substantial genetic overlap between the inattentive and hyperactive-impulsive components. Journal of Abnormal Child Psychology. 2007;35:999–1008. doi: 10.1007/s10802-007-9149-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milich R, Balentine AC, Lynam DR. ADHD Combined type and ADHD Predominantly Inattentive type are distinct and unrelated disorders. Clinical Psychology: Science and Practice. 2001;8:463–488. [Google Scholar]
- Millsap RE, Yun-Tein J. Assessing factorial invariance in ordered categorical measures. Multivariate Behavioral Research. 2004;39:479–515. [Google Scholar]
- Müller UC, Asherson P, Banaschewski T, Buitelaar JK, Ebstein RP, Eisenberg, Steinhausen HC. The impact of study design and diagnostic approach in a large multicentre ADHD study. Part 1: ADHD symptom patterns. BMC Psychiatry. 2011a;11:54. doi: 10.1186/1471-244X-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller UC, Asherson P, Banaschewski T, Buitelaar J, Ebstein R, Eisenberg J, Gill M, Manor I, Miranda A, Oades RD, et al. The impact of study design and diagnostic approach in a large multi-centre ADHD study. Part 2: Dimensional measures of psychopathology and intelligence. BMC Psychiatry. 2011b;11:55. doi: 10.1186/1471-244X-11-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 5th ed. Los Angeles, CA: Muthén and Muthén; 2002. [Google Scholar]
- Nadder TS, Rutter M, Silberg JL, Maes HH, Eaves LJ. Genetic effects on the variation and covariation of attention deficit-hyperactivity disorder (ADHD) and oppositional-defiant disorder/conduct disorder (ODD/CD) symptomatologies across informant and occasion of measurement. Psychological Medicine. 2002;32:39–53. doi: 10.1017/s0033291701004792. [DOI] [PubMed] [Google Scholar]
- Nigg JT. What causes ADHD? Understanding what goes wrong and why. New York: Guilford Press; 2006. [Google Scholar]
- Nigg JT, Casey BJ. An integrative theory of attention-deficit/ hyperactivity disorder based on the cognitive and affective neurosciences. Development and Psychopathology. 2005;17:785–806. doi: 10.1017/S0954579405050376. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Stavro G, Ettenhofer M, Hambrick DZ, Miller T, Henderson JM. Executive functions and ADHD in adults: Evidence for selective effects on ADHD symptom domains. Journal of Abnormal Psychology. 2005;114(3):706–717. doi: 10.1037/0021-843X.114.3.706. [DOI] [PubMed] [Google Scholar]
- Paloyelis Y, Asherson P, Mehta MA, Faraone SV, Kuntsi J. DAT1 and COMT effects on delay discounting and trait impulsivity in male adolescents with attention deficit/hyperactivity disorder and healthy controls. Neuropsychopharmacology. 2010;35:2414–2426. doi: 10.1038/npp.2010.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. American Journal of Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- Price TS, Simonoff E, Asherson P, Curran S, Kuntsi J, Waldman I, et al. Continuity and change in preschool ADHD symptoms: Longitudinal genetic analysis with contrast effects. Behavior Genetics. 2005;35:121–132. doi: 10.1007/s10519-004-1013-x. [DOI] [PubMed] [Google Scholar]
- Sagvolden T, Johansen EB, Aase H, Russell VA. A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. Behavioral and Brain Sciences. 2005;28:397–468. doi: 10.1017/S0140525X05000075. [DOI] [PubMed] [Google Scholar]
- Scheres A, Lee A, Sumiya M. Temporal reward discounting and ADHD: Task and symptom specific effects. Journal of Neural Transmission. 2008;115:221–226. doi: 10.1007/s00702-007-0813-6. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. Causal models of Attention-Deficit/Hyperactivity Disorder: From common simple deficits to multiple developmental pathways. Biological Psychiatry. 2005;57:1231–1238. doi: 10.1016/j.biopsych.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. The dual pathway model of AD/HD: An elaboration of neurodevelopmental characteristics. Neuroscience & Biobehavioral Reviews. 2003;27:593–604. doi: 10.1016/j.neubiorev.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS. Psychological heterogeneity in AD/HD - a dual pathway model of behaviour and cognition. Behavioral Brain Research. 2002;130:29–36. doi: 10.1016/s0166-4328(01)00432-6. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Dalen L, Remington B. Do executive deficits and delay aversion make independent contributions to preschool attention-deficit/hyperactivity disorder symptoms? Journal of the American Academy of Child Psychiatry. 2003;42:1335–1342. doi: 10.1097/01.chi.0000087564.34977.21. [DOI] [PubMed] [Google Scholar]
- Sonuga-Barke EJS, Sergeant JA, Nigg J, Willcutt E. Executive dysfunction and delay aversion in Attention Deficit Hyperactivity Disorder: Nosologic and diagnostic implications. Child and Adolescent Psychiatric Clinics of North America. 2008;17:367–384. doi: 10.1016/j.chc.2007.11.008. [DOI] [PubMed] [Google Scholar]
- Strickland J, Keller J, Lavigne JV, Gouze K, Hopkins J, LeBailly S. The structure of psychopathology in a community sample of preschoolers. Journal of Abnormal Child Psychology. 2011;39:601–610. doi: 10.1007/s10802-011-9487-5. [DOI] [PubMed] [Google Scholar]
- Todd RD, Huang H, Todorov AA, Neuman RJ, Reiersen AM, Henderson C, et al. Predictors of stability of attention-deficit/hyperactivity disorder subtypes from childhood to young adulthood. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:76–85. doi: 10.1097/chi.0b013e31815a6aca. [DOI] [PubMed] [Google Scholar]
- Toplak ME, Pitch A, Flora DB, Iwenofu L, Ghelani K, Jain U, Tannock R. The unity and diversity of inattention and hyperactivity/impulsivity in ADHD: Evidence for a general factor with separable dimensions. Journal of Abnormal Child Psychology. 2009;37:1137–1150. doi: 10.1007/s10802-009-9336-y. [DOI] [PubMed] [Google Scholar]
- Valo S, Tannock R. Diagnostic instability of DSM-IV ADHD subtypes: Effects of informant source, instrumentation, and methods for combining symptom reports. Journal of Clinical Child and Adolescent Psychology. 2010;39:749–760. doi: 10.1080/15374416.2010.517172. [DOI] [PubMed] [Google Scholar]
- Widaman KF, Reise SP. Exploring the measurement invariance of psychological instruments: Applications in the substance use domain. In: Bryant KJ, Windle M, West SG, editors. The science of prevention: Methodological advances from alcohol and substance abuse research. Washington, DC: APA; 1997. pp. 281–324. [Google Scholar]
- World Health Organization. International statistical classification of diseases and related health problems. WHO; 2007. 10th revision. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.