Abstract
Mobile phones are becoming an increasingly important platform for the delivery of health interventions. In recent years, researchers have used mobile phones as tools for encouraging physical activity and healthy diets, for symptom monitoring in asthma and heart disease, for sending patients reminders about upcoming appointments, for supporting smoking cessation, and for a range of other health problems. This paper provides an overview of this rapidly growing body of work. We describe the features of mobile phones that make them a particularly promising platform for health interventions, and we identify five basic intervention strategies that have been used in mobile-phone health applications across different health conditions. Finally, we outline the directions for future research that could increase our understanding of functional and design requirements for the development of highly effective mobile-phone health interventions.
Keywords: Mobile phone, SMS, consumer health, human-computer interaction
1 Introduction
In recent years, researchers have increasingly begun to use mobile phones as platforms for delivery of health interventions. This research has targeted a wide range of health conditions and has come both from health sciences and from disciplines in computer science, such as human-computer interaction (HCI) and ubiquitous computing. Text messaging interventions, for example, have been used to facilitate smoking cessation [1,2], to provide diabetes education [3], to encourage attendance of primary care appointments [4], and even to encourage sunscreen application [5]. Mobile phone applications allow physicians to monitor patients with chronic heart failure [6] and to detect early signs of arrhythmia or ischemia that can indicate an imminent heart attack [7]. In addition, patients themselves can use phone applications and sensing and measurement devices to keep track of their physical activities [8] and to monitor physiological markers relevant to their health status [9].
Our first goal in this paper is to map out the current state of this rapidly growing body of work. Rather than focus on a particular condition or health objective (e.g., encouraging weight loss), we present a taxonomy of the strategies and types of interventions that have been implemented with mobile phones. This approach, we hope, will both help the readers to understand the design space of mobile-phone health interventions and to construct new interventions by choosing elements that are most appropriate for their own application domains. Our second and related goal is to identify opportunities for improved and new interventions enabled by the ongoing developments in mobile phone technologies.
Although, when possible, we highlight the outcomes from the reviewed interventions, we do not offer a systematic review of effectiveness of mobile-phone interventions. The variety and combinations of intervention strategies and the diversity of the conditions that have been targeted make it hard to determine which features of the mobile-phone interventions used in different studies influenced their effectiveness. Consequently, effectiveness reviews can be best done at the level of a particular pathology—such as Krishna &Boren’s [10] recent review of interventions for diabetes. Such effectiveness reviews are clearly needed, but they must be more narrowly scoped than the work we take up in this paper.
The rest of this paper is organized as follows. After describing our methods in Section 2, in Section 3 we briefly discuss the reasons why mobile phones are a promising platform for delivering health interventions. In Section 4, we review the mobile phone technologies that are commonly used to create health interventions and the types of interventions that these technologies enable. In Section 5, the main part of this paper, we identify and provide examples of five general health intervention strategies for which mobile phones have been used, and the types of mobile-phone interventions that have been designed in service of these strategies. In Section 6, we discuss the opportunities for future work in this domain made possible by emerging forms of technology. Finally, in Section 7 we briefly discuss the limitations of this review.
2 Methods
The review we present in this paper is based on the literature identified through a search of PubMed, ACM Digital Library, and IEEE eXplore, the main databases that catalog the research literature on mobile phone-based health interventions. We searched PubMed for the following terms: “mobile phone,” “cell phone,” “SMS,” and “text message.” The ACM and IEEE databases were searched for combinations of the term ”health” and the terms listed above. Based on the abstracts retrieved through these queries and through PubMed’s Related Articles feature, we identified articles that described uses of mobile phones as a means of delivering health interventions. We eliminated articles that discussed mobile phones in other contexts (e.g., studies of the biological effects of radiation emitted by mobile phones). For each article in the resulting set, along with articles found through the citations in our search results, we identified how mobile phones were used to deliver a health intervention, what population was targeted, and, for articles that described an evaluation, what results were obtained. We then iteratively clustered the interventions described in the literature until we arrived at the taxonomy described in this paper.
Because our goal is to provide a review of the mobile phone design space, rather than a systematic review of efficacy evaluations, we present only illustrative examples of systems that use each type of intervention that we identified. Thus, although our review covers every intervention strategy and type that we identified in our search, it does not touch on every mobile-phone intervention found in the literature.
3 Why use mobile phones for health interventions?
Mobile phones are a particularly attractive avenue for delivering health interventions because of: (1) the widespread adoption of phones with increasingly powerful technical capabilities [11], (2) people’s tendency to carry their phones with them everywhere, (3) people’s attachment to their phones [12], and (4) recent context awareness features that can be enabled through sensing and phone-based personal information. We briefly review these reasons below.
First, over the past ten years, mobile phones have become ubiquitous. According to the latest report from the Pew Internet & American Life Project, 83% of American adults have an active mobile phone [11]. Of these, over a third (35%) use their phones not only to make calls and send text messages but also to access the Internet, and this trend is accelerating. According to the data from International Data Corporation, the worldwide market for smartphones—feature-rich phones capable of running third party applications, such as iPhones and Android devices—has grown by 39% in the last year [13]. These numbers indicate not only that the adoption of mobile phones has become nearly universal, but also that the market is rapidly shifting toward phones that are de facto pocket computers—powerful computational devices that can access the Internet and run a variety of complex applications. The deep penetration and technical capabilities of modern phones make sophisticated, phone-based health interventions appealing and widely applicable.
Second, unlike desktop computers or even laptops, mobile phones are nearly always with the person. Many of us are rarely more than a few feet away from our mobile phones, and more often than not, they are in our hand or in our pocket or purse. A study found that even in 2006 individuals were within arm’s reach of their phones on average 58% of the time [14]. As B. J. Fogg noted, we spend more time with our phones than we do with our partners or even at our workplace [15]. The fact that the phones are so close at hand makes it possible to drastically increase the number of points of care, from clinics (in standard practice) and patients’ homes (in traditional telemedicine), to nearly any place and time when the patient needs support [16].
Third, people’s relationships with their mobile phones are often deeply personal [12]. Phones are customized with user-selected ringtones and notification sounds, with images of loved ones, and with cases and decorations that express their owners’ style. Mobile phones are also used for a range of activities throughout the day, from calendaring and email to social networking, financial tracking, and playing games. As a result, phones often contain highly personal information, including pictures, intimate text messages, and financial information. The personal nature of mobile phones can reduce the barriers to adoption and increase acceptance of phone-based health interventions by integrating health education and other forms of health promotion with a tool that is an integral part of individuals’ daily routines and to which they often have positive emotional attachment.
Finally, the combination of their technical capabilities and the proximity to their owners means that phones can know a great deal about the users’ current situation [15]. Through embedded sensing (such as GPS location tracking, accelerometer-based exercise detection), and access to the user’s calendar, contacts and other personal information, mobile phone applications can infer where their users are and what they are doing. This knowledge, in turn, makes it possible to create just-in-time interventions that provide users with support at times when that support is most needed [17,18]. Such interventions can be particularly useful for discouraging unhealthy behaviors, such as eating unhealthy foods or smoking, where target behaviors are often strongly tied to particular contexts (e.g., snacking while watching TV at night). The ability to detect such contexts could enable us to provide users with assistance before they engage in such unhealthy behavior, as well as to provide post facto feedback, potentially greatly increasing the effectiveness of behavior change interventions.
4 Technology behind mobile-phone health interventions
Not all mobile-phone health interventions rely on the same type of technology. Technical capabilities of mobile phones vary widely, from the support for only voice and text messaging on basic feature phones to the support for third party applications, sensing, Internet access, and wireless connectivity with other devices on smartphones, such as iPhones, Blackberries, Windows Phones, and Android phones. Health interventions have taken advantage, to a greater or lesser degree, of all these capabilities. In this section, we provide a brief overview of the technical features of mobile phones and ways in which those features have been used in health interventions.
4.1 Text messaging (SMS)
Text messaging (short message service or SMS) is a service that enables 160 character messages to be sent from one phone to virtually any other mobile phone in the world. Because it is supported by even the simplest mobile phones, SMS is widely used not only in the first world but in the developing countries as well, where mobile phone penetration has reached 68% [19]. This widespread use makes text messaging the most universally accessible technology for phone-based health interventions and possibly the most accessible way of delivering health interventions of any kind.
Beyond its accessibility, text messaging has seen broad adoption as a health technology for two other reasons. First, text messages are a push technology, allowing intervention messages to be delivered without any effort on the part of the recipient. As such, text messages are often used for sending reminders [e.g., 4,5], tips and other educational content [e.g., 2,3], and for maintaining users’ awareness of their health goals [20]. Second, because text messages can be sent and received by both phones and computers, text messaging provides a way for users to log their health-related activities and physiological parameters (e.g., exercise, peak flow in asthma management [21], etc.) and to receive customized feedback based on these data. The ability to process text messages automatically makes it possible for the complete information exchange in an intervention to be done via SMS—users can be sent reminders to log relevant data, they can reply to reminder messages with the requested information, and the system can process these responses and send users feedback customized to their current situation. For example, Haug et al.’s [2] smoking cessation intervention for young adults uses precisely this kind of SMS information loop.
The diversity of these interactions provides evidence for just how flexible text messaging can be as a system for delivering health interventions.
4.2 Cameras
In recent years, cameras have become a standard feature on all but the most basic mobile phones. The quality of phone cameras is still below the quality of dedicated digital cameras, but their constant availability makes phone cameras a useful tool for collecting health-related data throughout the day. So far, health interventions have used cameras in three primary ways: (1) as an alternative way to journal health-related behaviors, such as food consumption [22,23], (2) as a way to provide healthcare providers with additional information about a condition, such as the appearance of psoriasis lesions [24], and (3) as a way to document circumstances relevant to the self-management process, such as the contextual factors that might influence diabetic patients’ ability to effectively manage their blood glucose levels [25]. Although photos cannot be automatically processed as easily as text can, in cases where a goal of an intervention is to support reflection or learning through active engagement with the user’s data [e.g., 23], phone cameras can be a valuable tool for low-effort collection of health-related information.
4.3 Native applications
All major smartphone platforms—iOS, Android, Symbian, Blackberry, webOS, and Windows Phone—provide developers with programming interfaces (APIs) that can be used to build special purpose applications. The APIs provide access to interface controls (e.g., dialog boxes, menus, calendar pickers), to the phone’s hardware features (e.g., accelerometers, cameras), and to other data and applications on the phone (e.g., contact list, calendar, email), enabling creation of complex and sophisticated applications.
Researchers and commercial companies have leveraged these capabilities to build several different types of health applications:(1) journaling applications that enable users to log and chart data about their diet [26,27], exercise [28,29], blood glucose levels [23], and other health-related behaviors and measures; (2) patient terminals for telemonitoring of conditions such as hypertension [30] and chronic heart failure [6]; (3) applications that receive data from pedometers, blood pressure monitors and other devices[9]; (4) games that teach health-related skills [31], and so on. We will review many of these application types below.
4.4 Automated sensing
Nearly all contemporary mobile phones can connect to sensing devices over Bluetooth or another form of personal area networking. In this way, mobile phones can connect to digital scales, blood pressure monitors, glucose meters, portable electrocardiograms (ECG), pedometers, and gym equipment, among other sensors. Mobile phones connected to such devices can act as receivers and data stores for the collection of a variety of health-intervention data.
In addition, over the last two years, an increasing number of mobile phones have begun to ship with sensors such as accelerometers and GPS built in, enabling detection of users’ behaviors even without the use of an external device. For example, the iPhone application RunKeeper (http://runkeeper.com) uses built-in GPS to automatically track how far users run or cycle, to create maps of their exercise routes, and to calculate how many calories were burned during these workouts. The trend toward sensors built into mobile phones will likely increase user acceptance of health interventions by freeing users from the need to keep track of, charge, and wear an additional device [28].
4.5 Internet access
Finally, one of the most important capabilities of mobile phones, from the standpoint of health interventions, is their ability to use the cellular network to connect to the Internet from nearly anywhere. This always-on connectivity means that users’ data, such as blood glucose levels or peak flow readings, can be uploaded to providers’ servers as soon as they are captured, thus enabling early detection of critical events. The data can also be uploaded to websites where users can easily view, chart, and edit their information. Lastly, always-on connectivity makes it possible to include web pages and online audio and video as part of phone interventions. The use of online resources makes it easier to keep the content of an intervention up to date without requiring users to repeatedly install updated versions of the application.
5 Design space of mobile-phone health interventions
Researchers have taken advantage of the technical capabilities described above to develop a wide range of different health interventions. Some interventions are relatively simple—for example, a number of interventions use SMS to send reminders to patients about upcoming appointments [4,32–34]—but many are complex, both in terms of the technology they use and the intervention strategies on which they rely.
In this section, we aim to map out the design space of mobile-phone health interventions by identifying the intervention strategies that have been used in phone-based interventions, and the specific forms that the interventions embodying these strategies take. Specifically, we have identified five key intervention strategies: (1) tracking health information, (2) involving the healthcare team, (3) leveraging social influence, (4) increasing the accessibility of health information, and (5) utilizing entertainment. Table 1 summarizes examples of these intervention strategies and phone features used. The rest of this section reviews the five intervention strategies in depth.
Table 1.
Examples of mobile-phone health interventions, broken by intervention strategies and phone features that they employ.
| Phone feature/intervention strategy | Text messaging | Cameras | Native applications | Automated sensing | Internet access |
|---|---|---|---|---|---|
| Tracking health information | Holtz & Whitten [43], Anhøj et al. [21], Franklin et al. [44], Haug et al. [2] | Brown et al. [22], Mamykina et al. [23], Mattila et al. [29] | Mamykina et al. [23], Denning et al. [26], Lee et al. [27], Consolvo et al. [28, 71], Mattila et al. [29], Gasser et al. [39], Kollmann et al. [40], Walters et al. [41] | Mamykina et al. [23], Denning et al. [26], Consolvo et al. [28, 71] | Mamykina et al. [23], Kollmann et al. [40], Walters et al. [41], Kim & Kim [51], Park et al. [52] |
| Involving the healthcare team | Obermayer et al. [1], Haug et al. [2], Holtz & Whitten [43], Franklin et al. [44], Kim & Kim [51], Park et al. [52] | Mamykina et al. [23], Schreier et al. [24] | Mamykina et al. [23], Walters et al. [41], Farmer et al. [50], Kearney et al. [56], Larsen et al. [57], Morris et al. [62] | Rubel et al. [7], Mamykina et al. [23], Farmer et al. [50], Villalba et al. [54], Scherr et al. [60] | Rubel et al. [7], Mamykina et al. [23], Farmer et al. [50], Villalba et al. [54], Scherr et al. [60] |
| Leveraging social influence | Obermayer et al. [1], Franklin et al. [44], Roger et al. [72], Riley et al. [74], Whittaker et al. [75] | Gasser et al. [39], Consolvo et al. [71] | Consolvo et al. [71] | ||
| Increasing the accessibility of health information | Wangberg et al. [3], Armstrong et al. [5], Leong et al. [33], Roger et al. [72], Gerber et al. [79], Curioso et al. [81], Strandbygaard et al. [82], Castaño & Martínez [85] | Consolvo et al. [28], Chiu et al. [87] | Consolvo et al. [28], Chiu et al. [87] | ||
| Utilizing entertainment | Armstrong et al. [5], Rogers et al. [72] | DeShazo et al. [31], Grimes et al. [91] |
5.1 Tracking health information
At the core of many mobile-phone health applications is a single strategy: using the phone to track health-related behaviors, physiological states, symptoms, and other parameters relevant to health. Tracked health data has many uses, but just the process of tracking itself—often referred to as self-monitoring—can provide many benefits, including increased frequency of desired behaviors and decreased frequency of undesired behaviors [35–38], better understanding and awareness of one’s behavior and health patterns [e.g., 8], and opportunistic engagement in desired behaviors [8,39]. In mobile-phone health interventions, self-monitoring has been implemented in three primary ways: through native journaling applications, via text messaging, and through automated sensing and recording.
5.1.1 Native journaling applications
Native journaling applications are custom designed to support logging of one or more health-related behaviors (e.g., physical activity or food intake), and relevant measures (e.g., blood glucose levels, blood pressure, or stress levels). They also typically provide ways to chart these data to foster reflection on trends over time. For example, UbiFit [8,28], an application for encouraging physical activity, enables tracking of cardiovascular exercise, strength training, different types of stretching, as well as of other activities that users considered to be physically demanding, such as scrubbing floors or chopping wood. UbiFit users can see daily and weekly views of their data as well as their proximity to their weekly physical activity goals. Similarly, Wellness Diary [29], a journaling application developed by Nokia Research, supports logging of a wide range of health-related states and activities, including—among others—physical activity, food intake, weight, mood, blood pressure, stress, and amount of sleep. Each of the measures can also be charted so that users can see trends in their data over time.
In the context of chronic disease management, Kollmann and colleagues [40] developed a java-based mobile-phone application called Diab-Memory to enable diabetic patients to self-monitor blood glucose levels, insulin use, intake of carbohydrates, and physical activity. The phone application synchronizes with a website where users can chart their data in different ways to better understand how various factors affect their blood glucose levels. Similarly, an intervention by Walters et al. [41] uses Wellness Diary to help patients who are undergoing cardiac rehabilitation to monitor their physical activity, diet, and risk behaviors, such as smoking and alcohol use. The data can be charted on the phone and on the companion website, Wellness Diary Connected, to which it is automatically synchronized.
Studies suggest that self-monitoring applications can have positive effects on users’ health. Kollmann et al.’s three-month feasibility trial of Diab-Memory with ten diabetes mellitus type 1 patients showed that the system helped the participants achieve a statistically significant improvement in HbA1c levels (from 7.9% ± 1.1% to 7.5% ± 0.9%, p=.02), as well as a slight—albeit not significant—decrease in blood glucose levels[40]. Similarly, the initial study of the Wellness Diary [29] indicated that phone-based journaling could be maintained over three months and that active use of the system helped individuals lose weight.
Designers of journaling applications can take several approaches to recording of health information, each of which presents a different set of trade-offs. With the Mobile Lifestyle Coach [39], for instance, users log their physical activity and diet using a simplified point system: a user gets one “lifestyle point” for 10 minutes of moderate or vigorous physical activity or one serving of fruit or vegetables. The system thus allows tracking of a variety of physical activities and foods without requiring effortful logging of every single type of activity or food individually. Similarly, with Wellness Diary [29] users can log their food intake by selecting from a simple list that includes “light snack,” “heavy snack,” “light meal,” and “heavy meal.” The convenience and speed of entry afforded by such simplified journaling is achieved at the cost of precision of the logged data. Although Wellness Diary’s diet logging might be sufficient to help users get a better sense of their overall eating patterns, it is not sufficiently detailed, for instance, to help diabetic patients to understand the effect of different foods on their blood glucose levels.
Other applications such as PmEB [27,42] and BALANCE [26] take a different approach to journaling. They incorporate caloric information for a variety of foods and activity types, enabling users to more accurately monitor their daily caloric expenditure but at the cost of higher journaling effort. A variety of commercial applications, such as Lose It (http://www.freshapps.com/lose-it/), take this same approach of supporting detailed logging. The decision to adopt detailed or simplified journaling depends on several factors, including how granular the data need to be, how many parameters need to be tracked, and how long tracking needs to continue.
Finally, native applications do not need to rely on textual entry for journaling. A number of systems attempt to reduce the effort involved in self-monitoring by enabling users to record their activities by taking photographs with the phone camera. Brown et al.’s [22] system for encouraging physical activity and healthy diet in college students allows users to use the phone camera to take pictures of their food and activities throughout the day. To increase users’ awareness of their eating and exercise patterns, these captured images are automatically shown in daily and weekly timeline views displayed on the users’ phones and computers. Similarly, both Wellness Diary and the diabetes management system MAHI [23] let users take pictures with the phone camera to log their food intake. Such photo-based journaling enables quick capture of complex data (e.g., a meal consisting of multiple foods), but makes it more difficult to graph the data and to automatically provide users with feedback on their activities and health parameters.
5.1.2 Tracking through text messaging
In addition to dedicated journaling applications, self-monitoring on mobile phones can also be implemented using text messaging. The nature of SMS limits how complex tracked data can be, making this strategy feasible only for conditions where individuals need to log a small set of well-defined parameters. Within these constraints, however, SMS can be a useful medium for self-monitoring because processing text messages on the server makes it possible to automatically analyze logged data and provide users with feedback on their activities and measures.
One area where SMS-based self-monitoring has been successfully used is in chronic disease management. In Holtz and Whitten’s [43] asthma intervention, participants use SMS to submit peak flow readings every morning. The system sends participants automatic feedback on whether the submitted readings are within a normal range, and it provides a web interface where they can see and chart all of their submitted data. Participants in Holtz and Whitten’s pilot study gave the SMS asthma monitoring system high satisfaction scores and expressed that they felt that the system provided them with an effective way of managing their condition. Anhøj et al.’s [21] asthma intervention uses a similar strategy: participants are sent three text messages a day, and they reply to these messages to log their peak flow readings, medications they have taken, and any sleep interruptions they had the previous night.
SMS has also been used for self-monitoring in diabetes. Users of the Sweet Talk system [44] can use text messaging to log their glucose level readings. Text messages sent by patients are processed by the Sweet Talk web application and the reported values are added into the user’s journal. If a text message contains text in addition to a numerical value representing the glucose reading, the message text is added to the reading as a note. By accessing the website, users are able to see charts of submitted data and read any associated notes.
For conditions where tracked information can take the form of simple numerical values such as glucose levels and peak flow readings, text messaging provides a lightweight way of implementing self-monitoring. Although limited in scope, the low-cost, high prevalence, and low technical requirements of SMS make it a good match for large-scale deployments of self-monitoring systems.
5.1.3 Automated sensing for tracking
One of the biggest downsides of self-monitoring has always been the effort involved in tracking one’s activities. For that reason, individuals rarely manage to keep up with traditional paper-based self-monitoring for longer than a few weeks [38]. One way to reduce that effort is to use sensors and connected measurement devices to automate logging of at least a subset of relevant activities and states. Wellness Diary [29] automates recording of how much the user walks by connecting to a pedometer. UbiFit [8,28] uses the Mobile Sensing Platform [45], a pager-sized wearable sensing device, to automatically detect walking, running, biking, using a stair machine, and using an elliptical trainer. As long as the MSP is turned on and is worn on the user’s waist, these activities are detected without any further user involvement. They are then transferred to the phone over Bluetooth and added to the user’s activity journal. Results from a three-month field study of UbiFit [8] indicated that automatic activity detection was very positively received, although study participants disliked having to wear a bulky sensing device. The follow-up work by Saponas et al. [46] has shown that recognition of a similar range of activities can be achieved through the use of accelerometers built into mobile phones, obviating the need for a second device. The use of such embedded sensing could help increase user acceptance of interventions that incorporate activity detection because it removes the need to wear, charge, and manage an additional sensing device.
In addition to automatic detection of health-related behaviors, a number of phone-based health applications can connect, often wirelessly, to devices for measuring and uploading physiological data. Devices that support external connections include digital scales [e.g., 6], glucometers [e.g., 47], blood pressure cuffs [e.g., 30], and even sophisticated portable electrocardiograms [7]. Connecting such devices to a mobile phone reduces the effort involved in transferring readings into a self-monitoring application and it decreases errors that can occur during manual transfers.
Although the use of sensing holds great potential for enabling long-term self-monitoring interventions, it is not a panacea. Miscalibration and incorrect use of measurement devices can introduce errors into the log. Similarly, automatic activity detection can fail, both by not detecting or inaccurately detecting activities that the user has performed and by erroneously detecting activities that the user has not done [28]. Other challenges remain as well. Finding ways to indicate to users the level of uncertainty of detected information and the ability to correct incorrectly detected activities is important for designing interventions that users can trust and are willing to continue to use. Similarly, finding ways to automatically summarize large sets of sensed data, as well as to collect and present data in ways that respect users’ privacy and levels of comfort with being monitored, will be important for wide adoption of such systems [48,49].
Self-monitoring is an essential component of a large number of health interventions, from applications that facilitate health behavior change to those that help with symptom monitoring in chronic conditions. Mobile phones can ease the effort involved in self-monitoring by putting sophisticated journaling applications close at hand, using photos to quickly document complex behaviors, and using measuring devices and sensors to automate logging of behaviors and physiological states.
5.2 Involving the healthcare team
Although tracking health information can provide useful support for encouraging health behavior change and for chronic disease self-care, effective management of many conditions requires support from the patient’s healthcare team. Keeping the healthcare team informed of the patient’s symptoms, activities, and physiological parameters can greatly enhance how effectively—and rapidly—care can be provided in such circumstances.
Two types of interventions, remote coaching and remote symptom monitoring, leverage mobile phones to keep the healthcare providers informed of the patient’s condition and to facilitate provider-patient care interactions. A third type of intervention, automated feedback, allows indirect clinician feedback through automatically activated rules or guidelines that people with clinical expertise can define. We review these three types of phone interventions next.
5.2.1 Remote coaching
Remote coaching interventions use the data that patients collect on mobile phones to enable learning interactions. In these interventions, tracking data is uploaded from the phone to a website where the data is reviewed by a member of the patient’s healthcare team. Based on the data, clinicians then work with patients to help them learn to manage their conditions more effectively. The coaching interaction itself typically takes place in one of three ways: over the phone, via SMS, or through a website.
One common strategy is for the data to be collected using a phone-based journaling application or SMS, but for the clinician-patient interaction to take place over the phone. For example, Farmer et al. [50] describe a mobile phone application for young people with diabetes. Patients used the application to upload their glucose readings from a Bluetooth-connected glucometer and to annotate these readings with information about what amount of insulin they injected, what they were about to eat, and how physically active they planned on being in the next few hours. Based on the data, a nurse worked with each patient during weekly phone calls to discuss the patient’s particular issues—for example, how much insulin the patient should be taking at night or how different types of meals seemed to affect her glucose levels. A randomized controlled trial (RCT) with 94 type-1 patients showed that the intervention group decreased their HbA1c levels significantly more than the controls. A similar intervention by Walters et al. [41] used the mobile and web versions of the Wellness Diary to provide coaching around health-related activities and goal-setting for patients undergoing cardiac rehabilitation.
In other interventions, feedback on the patients’ tracked data is delivered using text messages. Although this modality cannot provide the same kind of rich interaction that is possible over the phone, text messaging can deliver to patients highly specific and tailored feedback that can help them manage their conditions more effectively. For example, in Kim and Kim’s intervention for obese patients with type-2 diabetes [51], patients used a mobile phone or a web browser to log their glucose readings, insulin doses, and the amount of medication they were taking. A diabetes educator reviewed these data once a week and sent patients customized feedback using text messages and the website. The SMS feedback was highly specific. Kim and Kim write that examples of feedback included messages such as “please decrease the long-acting insulin by two units” and “please add one tablet of sulfonylurea in the evening” [51, p. 400]. Their results show that these brief coaching messages can be very effective. The intervention group in their study had significantly better HbA1c levels than the controls at three, six, nine, and twelve month follow-ups, with the glycemic control continuing to improve over that whole period. Park et al. [52] have recently used a very similar intervention with obese patients with hypertension, also with positive results. The Sweet Talk system for young adults with diabetes [44,53] also includes a SMS-coaching component. In Sweet Talk, users are able to send questions to their healthcare team via SMS. These questions are forwarded to the best person to answer them (e.g., a doctor or a dietician), who then writes a response that gets forwarded to the user’s phone as a text message. As with Kim and Kim’s study, a year-long RCT of Sweet Talk showed that SMS-based coaching interventions can have meaningful clinical impact. Over the course of the Sweet Talk trial, the intervention arm significantly decreased their HbA1c levels (from 10.1% ±1.7% to 9.2% ±2.2%, p<0.001), while the standard treatment arm showed no improvement.
Finally, in some interventions, clinician-patient interactions take place through a web application. For example, MAHI—Mamykina et al.’s [23] mobile phone application for people who are newly diagnosed with diabetes—lets users upload glucose readings and audio and photo diary entries about their diabetes management to a secure website. On the website, patients can reflect and comment on their data and can discuss the data with a diabetes educator. Mamykina et al. [23] report that many of their participants found the ability to get feedback about the concrete self-management problems they were struggling with to be the most valuable aspect of MAHI. The use of photographs worked well for this purpose. (Similarly, an earlier intervention by Smith et al. [25] showed positive results for the use of photographs to foster reflection in diabetes self-management.) For visual data such as photos, a web application can provide a much richer interaction environment than can text messages or even a phone call. At the same time, a mobile phone provides an early perfect tool for capturing such data, enabling quicker and richer data acquisition than is possible through traditional journaling.
Each of the three modalities for providing coaching feedback has its own benefits and downsides. Telephone calls are highly interactive, enabling in-depth discussions and problem solving. Consequently, they can be very effective for helping patients to develop self-management skills. However, phone calls are labor intensive for healthcare providers and require coordination of patients’ and clinicians’ busy schedules. SMS can be effective for routine troubleshooting—adjusting the dose of a medication, providing tips for changes in specific daily activities, etc.—but they are less well suited for helping newly diagnosed patients to learn how to manage their illness or to find solutions for persistent self-management problems. Online interactions through forums and secure messaging, such as those used by Mamykina et al., might provide a happy medium in this regard. Although they can belabor intensive, the asynchronous nature of web-based communication makes such interactions more flexible than telephone calls. The ability to share multimedia content and links to educational and problem-solving resources makes such web-based clinician-patient communication very well suited for facilitating self-management skills while also supporting brief interactions when those are sufficient for ongoing health management.
Mobile phones enable effective remote coaching interventions that can help chronic disease patients to learn a range of complex skills that they need to manage their condition. Phones serve this purpose both by enabling patients to collect data about their activities and physiological measures and, in SMS coaching interventions, by providing a way for them to receive concrete, tailored feedback about how to manage their illness more effectively.
5.2.2 Remote symptom monitoring
In addition to remote coaching, mobile phones are commonly used to monitor patients’ health and to alert the healthcare team if dangerous symptoms develop. Timely detection of such symptoms and worrisome physiological parameters is key to prevention of potentially serious deterioration in patients’ health. Thus, many interventions use data captured with mobile phones to look for such indicators and to alert appropriate healthcare providers.
Depending on the condition, symptom-monitoring applications can take advantage of sensing, self-report, or a combination of the two. For monitoring patients with heart disease, for example, physiological data are key and remote monitoring applications often connect to devices that can measure and upload these data automatically. For instance, Villalba et al.’s [54,55] system combines a mobile phone application and a variety of Bluetooth-connected devices—a blood pressure cuff, respiration and ECG sensors embedded in an instrumented shirt, accelerometers, and a digital scale—to enable chronic heart failure patients to collect data about their health status. Patients’ data are automatically uploaded to a server and are continuously monitored for signs of decompensation. If decompensation is detected, the patient’s physician is immediately notified by pager and email. Similarly, Rubel et al. [7]’s system uses a mobile phone connected to a portable device with an electrocardiogram. Heart disease patients use the system—called PAM—to monitor the condition of their heart over time. Every time a patient records an ECG reading, the PEM software compares the new reading to the person’s baseline and recent history. ECG readings outside the patient’s normal range generate alerts, and if the system determines that a heart attack is imminent both the patient’s physician and the nearest emergency call center are immediately notified.
Patients can also report their symptoms using self-report questionnaires built into a phone application. For example, an application developed by researchers in the UK [56–59] facilitates monitoring of toxicity symptoms in cancer patients undergoing chemotherapy. The system uses phone-based questionnaires to assess six toxicity indicators: nausea, vomiting, mucositis, hand-foot symptom, diarrhea, and fatigue. Patients’ responses are uploaded to a server, and if the software determines that reported symptoms are potentially alarming, the system generates “amber” or “red” alerts to the patient’s healthcare team.
Patients who use these symptom monitoring systems consistently report feeling reassured with the knowledge that their health is being monitored [43,58] and with the fast response from the healthcare team in cases when the system detects that something might be wrong [30,58]. In addition, Scherr et al.’s [6,60] work with chronic heart failure patients has shown that such systems can have measurable positive effects on health and clinical care. CHF patients in Scherr’s [60] study used a mobile phone application, a Bluetooth-enabled blood pressure monitor, and a digital scale to transmit their blood pressure, weight, and medication dosages every day. Study physicians had access to the data through a secure website, and data that fell outside of a predetermined range generated automatic alerts that were sent to the physicians. Scherr et al.’s results show that the study group that used the intervention had both fewer hospitalizations than the controls over a six-month period and that their hospitalizations were significantly shorter (median of 6.5 days for the intervention group vs. 10 days for the controls).
The design of symptom-monitoring systems remains challenging. To be effective, symptoms need to be assessed and monitored regularly, but this need must be balanced against the burden of monitoring. For example, excessive reminders to report symptoms can be negatively perceived [e.g., 21], potentially leading to system abandonment. Similarly, sensitivity is needed to balance clinician burden. For example, in Logan et al.’s [30] work on remote monitoring of hypertensive diabetic patients, physicians were very concerned about the negative impact of such systems on their workload (as well as the legal liability that this new data stream might introduce). Thus, they requested that the symptom reports be sent to their offices only by fax. Although remote-monitoring systems can be hugely beneficial, especially for life-threatening conditions, such burden and workflow issues need to be carefully considered.
5.2.3 Automated feedback
To increase patients’ access to health expertise and to make it available when patients most need it, automated systems can encode the types of feedback clinicians could provide if they were given the patients’ tracked data. The types and complexity of such feedback vary greatly. At the simple end, for Holtz and Whitten’s [43] intervention for self-management of asthma, users log their peak flow readings using SMS, and the system sends back one of three possible responses:(1) that the patient’s peak flow value is OK, (2) that the patient should follow her asthma action plan, or (3) that the patient should call her physician. At the complex end, Larsen et al.’s [57] and Kearney et al.’s [56] chemotherapy symptom management system provides sophisticated and tailored automated feedback. Depending on the symptoms that the patient reports, the system suggests specific strategies for managing those symptoms. For example, if the patient reports diarrhea, she might be told to drink fluids, use rehydration sachets, or take an anti-diarrheal medication, depending on reported severity [57]. As another complex example, Morris et al. have developed a system for managing stress and negative emotions [61,62]. Throughout the day, the phone prompts users to report how they are feeling. Users who indicate intense negative emotions, such as anger or anxiety, are prompted with an option to do an appropriate coping exercise drawn from cognitive psychology. For example, the application can present the user with an animated breathing exercise or ask a set of questions aimed at deescalating the user’s intense anger. Morris et al.’s data from a field study of this application indicate that using the system helped their participants significantly reduce their anger, anxiety, and sadness ratings over the course of the study [62].
The feedback that a phone-based intervention provides can be further customized by taking into account not only the information that the user is tracking but also the user’s health profile and other relevant information. In Haug et al.’s [2] ”SMS Coach” smoking cessation intervention, for example, individuals are prompted over SMS with weekly questionnaires that assess their smoking status and intention to quit. The system combines these data with the information about the user’s stage of change, smoking history, self-efficacy, and reasons for smoking to select customized motivational and educational messages that are sent to each person three times a week. A similar intervention by Obermayer et al. [1] uses user profiles to send coping messages at times of the day when individuals trying to quit reported that they were most likely to smoke (e.g., after dinner).
Automated feedback can make it easier for patients to get timely and relevant health management guidance that does not depend on the availability of healthcare professionals. However, to be effective, automated feedback needs to be sufficiently tailored. For example, Obermayer et al.’s [1] participants reported that the coping messages they were receiving were not customized enough for the situations in which they were tempted to smoke, and Haug et al.’s [2] participants desired more diverse feedback than the intervention provided. How to design highly customized and effective types of automated feedback remains an important open research question. Even simple representations of progress and goal attainment, however, can enhance motivation and facilitate the difficult behavior change process.
5.3 Leveraging social influence
Effective health management depends not only on the patients and their clinicians but also on the patients’ social environment [63]. For example, Wang and Fenske [64] found that chronic disease patients who received support from family and friends engaged in significantly more self-care behaviors than those who did not. Similarly, in a study of predictors of women’s continued exercise after cardiac rehabilitation, of all the examined factors only social support predicted exercise persistence [65]. Support from family and friends has been associated with lower hospital readmission rates [66,67], as well as longer survival times in patients with heart failure [68]. In addition, epidemiological studies by Christakis and Fowler [69,70] have indicated that the structure of individuals’ social networks influences not only their health risks (e.g., probability of becoming obese), but also their ability to adopt health-promoting behaviors, such as quitting smoking.
For such reasons, a number of recent mobile-phone interventions leverage social influence to promote health behavior change and effective management of chronic diseases. These interventions have pursued this strategy in three different ways: (1) by facilitating social support or competition among individuals who share the same health goal (i.e., peer-to-peer influence), (2) by facilitating social support from family and friends, and (3) by leveraging peers who have succeeding in accomplishing similar health goals (i.e., peer modeling). We review these intervention types next.
5.3.1 Peer-to-peer influence
Several mobile-phone interventions try to facilitate social influence among people who are working on the same health goal—such as increasing physical activity or managing diabetes. These systems have used two types of social influence to further this goal: social support (i.e., providing encouragement, reassurance, and empathy) and competition.
Consolvo et al.’s application Houston [71] uses peer-to-peer social support to help individuals to be more physically active. Individuals use Houston to share their daily step counts and progress toward their daily step goals with a group of friends (“fitness buddies”) and to send messages of encouragement to each other. Users can also annotate their step count records with additional information (e.g., that a person went hiking or had the flu) to make it easier for their fitness buddies to understand the context of a particular daily step count. To help users manage how they share their information, Houston provides controls to make it possible for a user to share a step count record with only certain buddies, with everyone, or with no one. Results from a pilot evaluation of Houston revealed that messages of social support were very motivating and that competition among buddies was often seen as helpful. Study participants who used the social version of Houston were significantly more likely to reach their daily step goals than participants who used a version of Houston that supported step count tracking but did not support sharing. However, in spite of its benefits, sharing sometimes also introduced discomfort, especially when a participant was not being very active [71].
Rodger et al.’s [72] text messaging intervention uses a similar peer-to-peer support strategy. Their system for smoking cessation used user profiles to connect individuals in the intervention with unfamiliar “quit buddies” who shared similar characteristics. However, Rodger et al. provide no detail about how well this part of the intervention worked, or how and to what extent system-assigned buddies interacted.
Franklin et al.’s [44,53] Sweet Talk system implements an impersonal version of peer social support. In Sweet Talk, an individual in the intervention can send a message that is anonymously forwarded to all other participants in the intervention. Sweet Talk users used this mechanism to send tips, success stories, or purely social messages [53]. The purpose of this intervention component, Franklin et al. [44] write, was to create a sense of community while protecting the group from text-bullying through moderation of forwarded messages. Franklin et al.’s [53] analysis of messages sent by participants during a six-month randomized controlled trial showed that the community building aspect of the intervention was at least partly successful. Messages intended to be forwarded to others—with tips, frustrations with diabetes self-management, personal experiences, etc.—were the second most common type of message that study participants created, right after submissions of blood glucose readings, indicating that the participants found such social messages to be valuable.
In contrast to Consolvo’s, Rodger’s, and Franklin’s systems that encourage social support, Gasser’s [39] Mobile Lifestyle Coach application attempted to use competition as a way to encourage individuals to be physically active and eat healthily. In the competitive, social version of the application, users were assigned into teams of five. The mobile phone interface made an individual’s progress toward her daily goal visible to the whole team, and the progress of the team—shown as each member’s individual progress as well as in cumulative terms—was displayed alongside the progress of the opposing team. Gasser et al. report that individuals in the competitive, social condition of their study did not do any better than the participants who took part in the condition that tested the individual version of the system. Although in this case the element of competition did not help, it also did not seem to hurt or be perceived negatively. This result contrasts with results in studies by Consolvo et al. [71] and Lin et al. [73], both of which found that, although liked by some users, competition hurt other participants’ motivation. Such mixed results suggest that if competition is going to be used as a motivation tool in mobile health technologies, it should be an optional element of these systems.
5.3.2 Social support from family and friends
An alternative form of social influence can come through support from family and friends. For example, Obermayer et al.’s [1] intervention for smoking cessation enabled individuals participating in the intervention to nominate a “support person” from their personal social networks who could provide social support during the quitting process. Using the web component of the intervention system, a support person could monitor the progress of the quitter and send messages of encouragement and support that were forwarded to the quitter’s phone via SMS. Interestingly, only a minority of participants in either Obermayer et al.’s [1] original study or in Riley et al.’s [74] follow-up study of the system chose to nominate a support person. It is not clear whether this lack of interest in having a support person was due to some aspect of this particular intervention or if it reflects a general weakness of this approach to facilitating social support. A similar result reported by Franklin et al. [53]—that none of the participants in their study of Sweet Talk nominated a friend or family member to receive their goal messages—suggests that sharing with people who are not pursuing the same health goal, even those close to the person, might be perceived as problematic or at least not very helpful. Future work is needed to understand the desires and needs of patients for such social support in mobile-phone health interventions.
5.3.3 Peer Modeling
In addition to motivating individuals through encouragement, praise, and competition, some mobile-phone health interventions provide users with support through modeling and exchange of information, such as tips and pointers to health-related resources, from successful peers. The social cognitive theory has shown that such social learning practices area key ingredient of successful behavior change [63]. As such, social learning strategies are particularly useful for helping individuals to adopt health-promoting behaviors, such as healthy diets.
Whittaker et al. [75] have used modeling in a smoking cessation SMS intervention for Maori youth. For the intervention, Whittaker et al. created a set of 30-second videos featuring “role models” who have successfully quit smoking. In the video clips, role models talk about their experiences with quitting and encourage viewers that they too can quit. Participants in Whittaker et al.’s intervention were sent text messages with links to these motivational video clips. They could then click on the links and watch the videos directly on their mobile phones. The participants in the intervention were overwhelmingly positive about the videos, stating that the use of video made the stories more real and made it easier for them to relate to the role models. An important aspect of the success of Whittaker et al.’s intervention was that the role models were selected from the local Maori community, making it easier for participants to identify with them. The use of video was key in conveying this aspect of the intervention. While video imposes additional technical requirements that could potentially limit the reach of an intervention, for modeling interventions the immediacy provided by video can greatly enhance the connection that users feel with peer models.
Grimes et al. [76,77] used a related strategy in their intervention for improving diet in a low-income African American community. Grimes et al.’s EatWell application enabled users to use their mobile phones to call a system where they could record and listen to “memories” about eating healthily in their local community. Users left stories about their successes and challenges and tips about healthy recipes and local places where one could get tasty but healthy meals. As with Whittaker et al.’s intervention, the local nature of EatWell was key to its acceptance by users. The tips that were exchanged through EatWell were both highly relevant because they were about local food establishments and stores, and were perceived as being culturally appropriate and helpful because they were coming from other community members with similar eating patterns and tastes. Whittaker et al.’s and Grimes et al.’s results indicate that mobile-phone health interventions can effectively facilitate social learning to encourage health-promoting behaviors. Insofar as social learning is strengthened by tailoring the intervention to local and cultural resources, technologies such as GPS and geo-tagged social networking updates (e.g., Twitter) could enable researchers to customize their phone-based interventions to specific user groups and context seven further.
Results from studies reviewed in this section suggest that mobile-phone interventions that incorporate social influence can be both effective and well liked by users. However, they also indicate that precisely how the social component is designed can significantly affect the usefulness and acceptability of an intervention. A careful design process and preliminary testing of a new system in small-scale field studies is, therefore, necessary for this type of phone intervention.
5.4 Increasing the accessibility of health information
One of the chief advantages of using mobile phones for health interventions is that intervention content can be delivered to individuals without any effort on their own part. By using text messages, for example, an intervention can be “pushed” to individuals’ phones, providing reminders, health information, motivational messages, and other kinds of content that can help them manage their health. Such interventions can not only provide information at the right time—for example, a reminder shortly before a person should take her medications—but can also help individuals to maintain persistent awareness of and commitment to their health goals [78], facilitating long-term behavior change and health management. In this way, mobile-phone health interventions can make it easier for individuals to manage their health more consistently and, thus, more effectively.
Recent mobile-phone health interventions have used the push model of delivering health-related information in three main ways: through informational messages about how to manage health more effectively, through reminders, and through glanceable displays. We review these intervention types next.
5.4.1 Informational messages
A common way of using mobile phones for health is to send individuals information relevant to their health goals or the management of their condition. Such informational messages fall into two primary categories: tips and educational content. Tips provide individuals with concrete strategies they can use to manage their condition or engage in health behavior change. Smoking cessation interventions, for example, might send tips on how to avoid weight gain [72] or offer coping strategies for specific situations, such as “if you typically experience cravings after breakfast, try getting up from the table and taking a walk” [1, p. 72]. A weight loss intervention would send users tips on diet and exercise, such as a reminder to drink more water [79]. Although in most cases such tips are drawn from a database of predefined messages, in some interventions users can contribute their own tips [e.g., 53]. Results suggest text messages with health tips are seen as being helpful. Gerber et al. [79] report, for instance, that 79% of women in their weight loss study thought that the tips that they were sent during the intervention could help them lose weight.
Along with concrete tips, messages sent in health interventions often include more general educational information related to the target condition. Messages sent in a smoking intervention can include information about symptoms of withdrawal or information aimed at strengthening a person’s decision to quit, such as the amount of money she would save if she were to stop smoking [1]. Similarly, Wangberg et al.’s [3] intervention sent text messages to parents of children with diabetes with information about diabetes management and the nature of the disease. As with tips, educational messages can have positive impact. For instance, participants in Wangberg et al.’s study expressed that the information they received during the intervention made it easier for them to talk with their adolescent children about diabetes.
Informational messages are a light weight health intervention that can help individuals to learn to better manage their health and stay engaged with their health goals. However, although informational messages can be helpful, Fjeldsoe et al.’s [80] comprehensive review of text messaging interventions for behavior change showed that tailored messages are more effective than generic messages. Participant comments in the studies were viewed support these findings. For example, participants in Obermayer et al.’s [1] smoking cessation intervention wanted feedback that was customized to their own high-risk situations. In addition, Fjeldsoe et al. found that interventions where users actively communicated with the healthcare team or with each other worked better than interventions where they just passively received information. For such reasons, informational messages would ideally be a part of a comprehensive intervention and not a full intervention in their own right.
5.4.2 Reminders
Another simple type of intervention that takes advantage of the push model is to send users reminders. Such reminders have been used in a variety of applications, from those where the sole intervention is the reminder to those where the reminders are one component of a comprehensive health intervention.
As the sole intervention type, one particularly important application of reminders is to increase medication adherence. For example, Curioso and colleagues [81] developed an SMS reminder system to increase HIV patients’ adherence to antiretroviral therapy (ART)—a type of treatment where extremely high levels of adherence (over 95%) are paramount to both immediate and long-term effectiveness. Similarly, Strandbygaard and colleagues [82] have used daily SMS reminders to increase adherence to asthma treatment. Although such reminders can be very effective—Strandbygaard et al. report that the participants in the intervention arm of their trial had 17.8% higher adherence to anti-asthmatic medications after 12 weeks than the controls—the results are not always positive. For example, daily SMS reminders used to increase adherence of French soldiers to malaria chemoprophylaxis did not result in increased compliance [83].
Another common use of reminders is to increase the consistency of health-promoting behaviors that individuals often forget to do. For instance, reminders are commonly used to increase the attendance of medical appointments. Even a single text message sent 24 to 48 hours prior to an appointment can significantly reduce the number of appointment no-shows. SMS reminders have been successfully used to increase appointment attendance in primary care [4,33], in family planning clinics [84], for chronic disease follow-up appointments [34], and for ophthalmology appointments [32]. Similarly, Armstrong et al. [5] showed that a text-messaging reminder can significantly increase regular application of sunscreen. In a study with 70 participants over six weeks, adherence to sunscreen application in the group that received daily SMS reminders was nearly twice as high (56%) as in the control group (30%) even though there was no difference between the two groups at baseline. Castaño and Martínez [85] used SMS reminders to help sexually active adolescents to regularly take their oral birth control. For such easy health-promoting behaviors, where the main barrier to doing them regularly is forgetting to do them, reminder interventions using SMS can be an excellent fit.
In multifaceted interventions, reminders are often paired with tracking applications, where individuals monitor their behaviors or physiological states. Many remote coaching and automated feedback interventions use reminders to ensure that participants are uploading their data regularly. Diabetes management interventions, for example, have reminders that are triggered if a patient does not upload her glucose readings in a certain amount of time [40,47,51]. Similarly, asthma [43] and hypertnsion [30] management interventions send patients reminders if they have not uploaded their peak flow or blood pressure readings regularly.
Although most health interventions use text messaging as the mechanism for delivering reminders, reminding functionality can also be a component of a native phone application. For example, if users of UbiFit [28] do not journal any physical activities in 24 hours and no activities are automatically detected, the system prompts them and asks whether they want to add anything to the exercise journal. These reminders area part of the UbiFit application itself, and they discreetly wait on the phone’s screen for the next time the user picks up the phone.
Literature suggests that reminders can be well received by users. Participants in the UbiFit studies [8,28] were very positive about reminders to journal their activities, partially because the reminders were not obtrusive—there was no sound and the user just saw the reminder next time she used the phone. Even the more obtrusive text-messaging reminders can be well liked [5,43]. However, the design of reminders is important. Users object to reminders that are perceived as being unnecessarily too frequent [21]. The content of the reminders matters as well. For instance, during the participatory design of their reminder system for medication adherence, Curioso and colleagues [81] found that their users wanted the reminders to be motivational (reminding them not only what they need to do but also why they are doing it), direct, and privacy-preserving (e.g., using code words instead of direct references to sensitive health conditions, in case someone were to see the recipient’s phone). Although the content and frequency of reminders varies from intervention to intervention, such findings suggest that minimizing disruptiveness (both of users’ time and potentially social relationships) is an important consideration for the design of effective reminder-based health interventions. At the same time, Curioso et al.’s findings indicate that thoughtfully designed reminders have a potential to do more than just remind individuals: they can also motivate, increasing the probability of being effective.
5.4.3 Glanceable displays
Informational messages and reminders are both push interventions in the narrow sense—they are delivered to the user’s phone on a schedule determined to maximize the likelihood that the delivered information will be effective. In contrast, recent work on glanceable displays aims to make health-related information visible every time a user picks up the phone. Glanceable displays provide users with an overview of their health in formation that can be interpreted at a glance and that is visible throughout the day. In this way, glanceable displays support persistent awareness of health goals and increase the likelihood that users will engage in health-promoting behavior.
For example, a key component of the UbiFit application [8,28] is the feedback about users’ physical activities that is displayed on the background screen (i.e., wallpaper) of the users’ mobile phones (Figure 1). UbiFit uses a stylized image of a garden to display physical activities that users perform each week. Different types of flowers represent different types of physical activity—walking, cardiovascular exercise, strength training, flexibility training, and other. The user gets a flower for every ten minutes of walking or cardiovascular exercise, and for each session of one of the other types of physical activities (e.g. stretching or strength training). The garden is automatically updated either when the sensing device detects an activity or when the user manually journals a new activity. If users meet their weekly activity goals, a large butterfly appears in the garden. Up to three smaller butterflies represent goal attainment for the previous three weeks.
Figure 1.
UbiFit’s glanceable display on the phone’s background screen. Different types of flowers represent different types of physical activities that the user performed this week (walking, cardio, strength training, and stretching). The butterflies indicate if the weekly activity goal was met this week (the large butterfly) and during the previous three weeks.
Through the use of the garden display on the background screen, UbiFit enables users to see at a glance how active they have been this week, how varied their activities have been, and whether they have attained their weekly goals. Because the garden is visible each time they use the phone, users have frequent encounters with feedback about their physical activity. This exposure causes cognitive activation of physical activity goals—making it more likely that users will continue to be active and notice opportunities to engage in physical activity [78,86].
A three-month trial of UbiFit demonstrated the power of this approach. Participants who had the background display managed to maintain their level of physical activity over the course of the three-month study—including the winter holiday season—while the activity of participants without the display, who used the same journaling application, significantly decreased during this period [8]. Study interviews revealed that seeing the garden display throughout the day kept physical activity in the front of participants’ minds. These results suggest that glanceable displays are a promising avenue for facilitating health behavior change. Chiu et al.’s [87] Playful Bottle system for motivating water intake uses a related approach—they have created a mobile game that provides feedback in the form of a tree that slowly loses its leaves if the user does not drink enough water. Stylized representations such as those used in UbiFit and Playful Bottle could be an effective way of presenting health information on displays that are likely to be seen by people other than the user. They also open another avenue of intervention personalization, potentially enabling users to pick “themes” that most resonate with them. One participant in the UbiFit trial, for instance, suggested that for him the system would have been much more motivating if it had used robots instead of flowers to represent different types of physical activity.
By increasing the accessibility of health information, these interventions support individuals’ ability to stay engaged with their health throughout the day. For a class of health-promoting activities that require high consistency in order to be effective—such as adoption of new healthy habits or adherence to a critical medication regimen—this persistent engagement with health is paramount. Yet, a remaining challenge is how to maximize the effectiveness of the pushed health information while minimizing the burden on the individuals using them.
5.5 Utilizing entertainment
Few people would refer to managing their health as ”fun.” Yet, a growing number of recent phone-based health interventions have begun to leverage some form of entertainment to engage individuals with their health goals.
One common form of this strategy is to make reminders and informational messages more engaging by interspersing them with other interesting or amusing non-health-related content. For instance, both Armstrong et al.’s [5] text messaging intervention for sun screen application and Rodgers et al.’s [72] smoking cessation intervention sent their participants messages with fun content—such as weather forecasts, jokes, sports scores, or interesting local news—in addition to health messages. Such messages were well received, keeping individuals interested in the intervention. In addition, participants in Whittaker et al.’s [75] smoking cessation intervention for Maori youth explicitly suggested that the intervention could be improved by including jokes, quizzes, and other such content. Although the inclusion of general interest content can give health interventions a lighter touch, future work will need to investigate whether certain types of non-health content work better than others to keep users engaged and whether there are health/non-health content ratios that optimize user engagement while minimizing the burden created by the inclusion of additional messages.
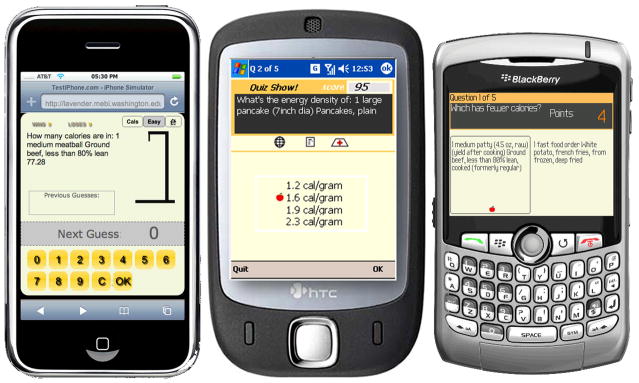
The second approach to leveraging entertainment that has recently emerged uses mobile phone-based video games to support health management. In human-computer interaction there is an established literature on exertion games—games that require players to invest significant physical effort as a part of game play [e.g., 88,89]. However, the idea that mobile phones can be used for games that promote health management is very recent. In two recent papers, DeShazo et al. [31,90] describe a set of simple phone games that teach patients with diabetes how to estimate carbohydrate content and caloric value of various foods (Figure 2). They have adapted familiar games of Hangman, QuizShow, and Countdown to include questions about food relevant to diabetes and to slowly scaffold users’ knowledge about nutrition. In Hangman, for example, users are given six chances to guess how many carbohydrates are contained in a given food before the stickman is hanged. To make them more effective, all games can be personalized based on whether users are vegetarian or not, what their educational goals are (i.e., to learn to estimate carbohydrates, calories, or energy density), and what their current skill level is. DeShazo et al.’s [31] early results indicate that players perceive the phone games to be enjoyable and that they think that playing the games has increased their knowledge about nutrition.
Figure 2.
DeShazo et al.’s phone-based games for teaching nutritional skills to diabetic patients. Users are asked to estimate nutritional content of various foods. Correct answers earn users points in the games.
Grimes et al. [91] have taken a similar approach with their OrderUP! game for helping African Americans learn to eat more healthily. In the game, users play a waiter at a restaurant and try to recommend, from the given choices, the healthiest food option for restaurant patrons. The healthier recommendations the users make and the more quickly they do it, the longer they get to keep the job in the game. As with Grimes et al.’s [76] EatWell system, the food options in OrderUP! were customized to the food choices that were popular and readily available in the community that the game was targeting. A three-week trial of the game showed that participants found the game to be enjoyable as well as educational. Participants expressed that playing the game both helped them learn about the healthfulness of the foods they typically ate and that it influenced their food choices. However, the participants thought that the educational value of the game was limited by the lack of feedback about why certain foods in the game were healthier than others.
One particularly attractive feature of games like those developed by DeShazo et al. and Grimes et al. is that they enable individuals to use microbreaks—brief periods of free time during the day (e.g., while waiting for a bus or at the grocery store)—to increase their self-management knowledge while engaging in an entertaining, relaxing activity. Both of these games could be played in just a few minutes. The use of such frequent breaks to improve health management skills could have far reaching positive health outcomes.
The use of phone-based video games for health is in its infancy but is quickly developing. The 2011 meeting of the Games for Health conference (www.gamesforhealth.org), for instance, has a full day of presentations on mobile serious games, many of which are about health. This space is wide open for innovative research that could not only support individuals in managing their health but also do so in an enjoyable, immersive way.
6 Discussion
In this paper, we identified five strategies that have been used in mobile-phone health interventions and the different ways in which those strategies have been implemented in interventions developed in health sciences and human-computer interaction. Recent technological advances are creating opportunities for further developments in interventions based on each of these strategies. In this section, we briefly review what we see as the main directions for future work in this important area of health research.
Most mobile-phone interventions based on monitoring of health information focus only on capturing information about the health activities and states that are directly tied to individuals’ health goals, such as the amount of physical activity or peak flow in asthma management. Yet, both in health behavior change and chronic disease management, understanding the context that influences these activities and states can be very important for developing effective health management practices. Mobile phones can make it possible to capture such contextual information to help individuals—and their healthcare providers—to better understand the concrete circumstances that influence their health and to develop strategies to address those patterns. By automatically associating captured information about health-relevant activities and states with location, time of day, and other information contained on the phone, such as calendar events or recent emails and phone calls, phone-based interventions could help individuals construct a rich understanding of the range of factors that influence their health and health-related behavior. Similarly, toolkits like My Experience [92] and Open Data Kit [93] can help make the very capture of self-report data smarter. By triggering questionnaires about health-related activities and states not only at predetermined times but also based on users’ location, detected activities and physiological measures, and other factors that the phone can sense, phone-based interventions can capture self-report data at the times that are most critical to individuals’ health goals (e.g., by capturing a user’s emotional state when initial signs of stress are detected). Such information, in turn, combined with a variety of sensing data, could enable truly effective just-in-time interventions. Although their potential has been recognized for several years [17,18], mobile phone technology is only now getting to the point where such interventions are technically feasible.
Improvements in phone technologies are also opening new opportunities for facilitating involvement of clinicians. The quality of photo and video available on modern mobile phones make it possible to use these devices as ubiquitous and inexpensive telemonitoring terminals. Schreier et al.’s [24] intervention for remote monitoring of psoriasis is a good example of the kinds of clinical interactions that mobile phones make possible. Recent developments of sophisticated medical devices that interface with mobile phones, such as AliveCor’s iPhoneECG system (www.alivecor.com) or Mobisante’s MobiUS smartphone-based ultrasound system (mobisante.com), could enable phone-based consultations for a range of conditions, greatly facilitating specialist care in areas where local healthcare resources are lacking.
Mobile-phone interventions are just beginning to explore the potential of leveraging social networks. In combination with lightweight tagging and automatically added location data, social networking tools like Twitter and Facebook can enable a whole class of new applications that use mobile phones to seek and share advice, expertise, support, and local resources for health management. Such applications could enable creation of ad hoc social networks of people with similar health goals or concerns, helping individuals to connect with others and to get health- related information and advice that is highly customized to their locations, cultural backgrounds, and health situations. Additionally, such looser social networks might avoid some of the social frictions that arise with changes in intensity of sharing in more tightly knit networks, such as those utilized by the Houston system [71].
Similarly, location and other contextual information, such as the user’s calendar, could be used to alert individuals to opportunities for healthy activities and local resources relevant to their health situation (e.g., nearby restaurants that serve healthy food or a suggestion to take a walk after a long meeting). If such prompts are made suitably unobtrusive and diverse—potentially by drawing on information mined from social networking tools—they could provide a dynamic way to keep individuals engaged with their health goals over extended periods of time, further building on benefits provided by reminders and glanceable displays.
As we already mentioned, the field of mobile-phone games for health is only starting. Future work should investigate both new types of games (e.g., augmented reality games that superimpose relevant health information on real world objects) and new ways to motivate health through gaming. For instance, Berkovsky et al. [94] has investigated providing in-game rewards for performance of physical activity and Harris et al. [90] have experimented with tethering health educational content to standard, non-health games such as Sudoku. Exploring other strategies for motivating health behavior and education through games and other forms of entertainment should be an important direction of future work.
Lastly, the vast majority of phone-based interventions we identified for this review focus on only three areas: chronic disease management, supporting health behavior change, and monitoring of symptoms and critical events. Although all three areas are extremely important, other aspects of health management could benefit from mobile phone-based solutions. Key among them, we believe, is personal health information management [95]. The ability to access their health information from anywhere, to easily collect and group care-related information as the information is first encountered, and to have relevant health-related information integrated with other daily tools (e.g., calendar), could greatly benefit patients, especially those who are undergoing treatment for complex conditions such as cancer. The work in this area is just beginning. As of mid 2011, Microsoft just announced a mobile-optimized website for Microsoft HealthVault—the preeminent third party personal health record—but robust mobile phone applications that use HealthVault are yet to be developed. Even the few patient portals that currently provide mobile access—such as Spectrum Health’s MySpectrum portal—support patients’ personal health information management needs in only limited ways. For instance, patient portals typically do not allow patients to enter their own data or annotate their records. Some of our own ongoing work attempts to fill this gap [96,97], but much more work is needed in this area.
7 Limitations
The review presented in this paper has two main limitations that are important to acknowledge. The first limitation is that the review is largely based on research literature from health sciences and human-computer interaction and does not survey the many commercial mobile-phone health interventions that have been developed in recent years. One reason for this choice is that unlike for research literature there is no systematic way to get a comprehensive overview of commercial products. The other reason, however, is that our goal was to provide an overview of the design space of phone-based intervention and that in the commercial products we found we did not identify any intervention strategies that were not also represented in the research literature. Of course, given the sheer number of commercial systems in this area, it is certainly possible that we overlooked products that break new ground in spite of our efforts to be comprehensive.
The other limitation is that the large majority of systems we reviewed here are intended to be used by patients or other individuals who are working on their own health goals. We did not review phone-based systems that help individuals to manage the health of another person, such as a child or an elderly family member. There is exciting new work in this area [e.g., 98] which is likely to lead to the development of novel intervention strategies which are currently not used in phone-based interventions for patients themselves. We suspect that at least some of those new strategies will be applicable to personal health applications as well, further contributing to our understanding of how to develop effective phone-based interventions that can help individuals to manage their health more effectively, consistently, and enjoyably.
Acknowledgments
This research was supported by a grant from the National Library of Medicine (grant number R01 LM009143) to Wanda Pratt.
Contributor Information
Predrag Klasnja, Email: klasnja@uw.edu.
Wanda Pratt, Email: wpratt@uw.edu.
References
- 1.Obermayer JL, Riley WT, Asif O, Jean-Mary J. College smoking-cessation using cell phone text messaging. J Am Coll Health. 2004;53(2):71–78. doi: 10.3200/JACH.53.2.71-78. [DOI] [PubMed] [Google Scholar]
- 2.Haug S, Meyer C, Schorr G, Bauer S, John U. Continuous individual support of smoking cessation using text messaging: A pilot experimental study. Nicotine & Tobacco Research. 2009;11(8):915–923. doi: 10.1093/ntr/ntp084. [DOI] [PubMed] [Google Scholar]
- 3.Wangberg SC, Arsand E, Andersson N. Diabetes education via mobile text messaging. J Telemed Telecare. 2006;12 (Suppl 1):55–56. doi: 10.1258/135763306777978515. [DOI] [PubMed] [Google Scholar]
- 4.Fairhurst K, Sheikh A. Texting appointment reminders to repeated non-attenders in primary care: randomised controlled study. Qual Saf Health Care. 2008;17(5):373–376. doi: 10.1136/qshc.2006.020768. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong AW, Watson AJ, Makredes M, Frangos JE, Kimball AB, Kvedar JC. Text-message reminders to improve sunscreen use: a randomized, controlled trial using electronic monitoring. Arch Dermatol. 2009;145(11):1230–1236. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- 6.Scherr D, Zweiker R, Kollmann A, Kastner P, Schreier G, Fruhwald FM. Mobile phone-based surveillance of cardiac patients at home. J Telemed Telecare. 2006;12(5):255–261. doi: 10.1258/135763306777889046. [DOI] [PubMed] [Google Scholar]
- 7.Rubel P, Fayn J, Nollo G, Assanelli D, Li B, Restier L, et al. Toward personal eHealth in cardiology. Results from the EPI-MEDICS telemedicine project. J Electrocardiol. 2005;38(4 Suppl):100–106. doi: 10.1016/j.jelectrocard.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Consolvo S, Klasnja P, McDonald DW, Avrahami D, Froehlich J, LeGrand L, et al. Proc UbiComp2008. ACM; 2008. Flowers or a robot army?: Encouraging awareness & activity with personal, mobile displays; pp. 54–63. [Google Scholar]
- 9.Mohan P, Marin D, Sultan S, Deen A. MediNet: personalizing the self-care process for patients with diabetes and cardiovascular disease using mobile telephony. Conf Proc IEEE Eng Med Biol Soc. 2008;2008:755–758. doi: 10.1109/IEMBS.2008.4649262. [DOI] [PubMed] [Google Scholar]
- 10.Krishna S, Boren SA. Diabetes self-management care via cell phone: a systematic review. J Diabetes Sci Technol. 2008;2(3):509–517. doi: 10.1177/193229680800200324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pew Internet & American Life Project. Internet, broadband, and cell phone statistics. 2010 Available from: http://www.pewinternet.org/Reports/2010/Internet-broadband-and-cell-phone-statistics.aspx?r=1.
- 12.Ventä L, Isomursu M, Ahtinen A, Ramiah S. Proc UbiComm’08. IEEE Computer Society; 2008. “My Phone is a Part of My Soul”-How people bond with their mobile phones; pp. 311–317. [Google Scholar]
- 13.IDC. IDC Woldwide quarterly mobile phone tracker. 2010 Available from: http://www.idc.com/getdoc.jsp?containerId=IDC_P8397.
- 14.Patel SN, Kientz JA, Hayes GR, Bhat S, Abowd GD. Proc UbiComp2006. Springer-Verlag; 2006. Farther than you may think: An empirical investigation of the proximity of users to their mobile phones; pp. 123–140. [Google Scholar]
- 15.Fogg BJ. The future of persuasion is mobile. In: Fogg BJ, Eckles D, editors. Mobile persuasion: 20 perspectives on the future of behavior change. Stanford, CA: Stanford Captology Media; 2007. pp. 5–11. [Google Scholar]
- 16.Demiris G, Afrin LB, Speedie S, Courtney KL, Sondhi M, Vimarlund V, et al. Patient-centered Applications: Use of Information Technology to Promote Disease Management and Wellness. A White Paper by the AMIA Knowledge in Motion Working Group. J Am Med Inform Assoc. 2008;15(1):8–13. doi: 10.1197/jamia.M2492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Intille SS. Ubiquitous computing technology for just-in-time motivation of behavior change. Stud Health Technol Inform. 2004;107(Pt 2):1434–1437. [PubMed] [Google Scholar]
- 18.Patrick K, Griswold WG, Raab F, Intille SS. Health and the mobile phone. Am J Prev Med. 2008;35(2):177–181. doi: 10.1016/j.amepre.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.International Telecommunications Union. The world in 2010: ICT facts and figures. 2010 Available from: http://www.itu.int/ITU-D/ict/material/FactsFigures2010.pdf.
- 20.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 21.Anhøj J, Møldrup C. Feasibility of collecting diary data from asthma patients through mobile phones and SMS (short message service): response rate analysis and focus group evaluation from a pilot study. J Med Internet Res. 2004;6(4):e42. doi: 10.2196/jmir.6.4.e42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown B, Chetty M, Grimes A, Harmon E. CHI ‘06 Extended Abstracts. ACM; 2006. Reflecting on health: a system for students to monitor diet and exercise; pp. 1807–1812. [Google Scholar]
- 23.Mamykina L, Mynatt E, Davidson P, Greenblatt D. Proc CHI 2008. ACM; 2008. MAHI: investigation of social scaffolding for reflective thinking in diabetes management; pp. 477–486. [Google Scholar]
- 24.Schreier G, Hayn D, Kastner P, Koller S, Salmhofer W, Hofmann-Wellenhof R. A mobile-phone based teledermatology system to support self-management of patients suffering from psoriasis. Conf Proc IEEE Eng Med Biol Soc. 2008:5338–5341. doi: 10.1109/IEMBS.2008.4650420. [DOI] [PubMed] [Google Scholar]
- 25.Smith BK, Frost J, Albayrak M, Sudhakar R. Integrating glucometers and digital photography as experience capture tools to enhance patient understanding and communication of diabetes self-management practices. Personal Ubiquitous Computing. 2007;11(4):273–286. [Google Scholar]
- 26.Denning T, Andrew A, Chaudhri R, Hartung C, Lester J, Borriello G, et al. Proc HotMobile ‘09. ACM; 2009. BALANCE: towards a usable pervasive wellness application with accurate activity inference; pp. 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee G, Tsai C, Griswold WG, Raab F, Patrick K. CHI ‘06 extended abstracts. ACM; 2006. PmEB: a mobile phone application for monitoring caloric balance; pp. 1013–1018. [Google Scholar]
- 28.Consolvo S, McDonald DW, Toscos T, Chen MY, Froehlich J, Harrison B, et al. Proc CHI 2008. ACM; 2008. Activity sensing in the wild: a field trial of ubifit garden; pp. 1797–1806. [Google Scholar]
- 29.Mattila E, Pärkkä J, Hermersdorf M, Kaasinen J, Vainio J, Samposalo K, et al. Mobile diary for wellness management--Results on usage and usability in two user studies. IEEE Transactions on Information Technology in Biomedicine. 2008;12(4):501–512. doi: 10.1109/TITB.2007.908237. [DOI] [PubMed] [Google Scholar]
- 30.Logan AG, McIsaac WJ, Tisler A, Irvine MJ, Saunders A, Dunai A, et al. Mobile Phone-Based Remote Patient Monitoring System for Management of Hypertension in Diabetic Patients. Am JHypertens. 2007;20(9):942–948. doi: 10.1016/j.amjhyper.2007.03.020. [DOI] [PubMed] [Google Scholar]
- 31.DeShazo J, Harris L, Turner A, Pratt W. Grounded in theory, user-centered, and someplace else: Designing and remotely testing mobile diabetes video games. J Telemed Telecare. 2010;16(7):378–382. doi: 10.1258/jtt.2010.091012. [DOI] [PubMed] [Google Scholar]
- 32.Koshy E, Car J, Majeed A. Effectiveness of mobile-phone short message service (SMS) reminders for ophthalmology outpatient appointments: observational study. BMC Ophthalmol. 2008;8:9. doi: 10.1186/1471-2415-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leong KC, Chen WS, Leong KW, Mastura I, Mimi O, Sheikh MA, et al. The use of text messaging to improve attendance in primary care: a randomized controlled trial. Fam Pract. 2006;23(6):699–705. doi: 10.1093/fampra/cml044. [DOI] [PubMed] [Google Scholar]
- 34.Liew S-M, Tong SF, Lee VKM, Ng CJ, Leong KC, Teng CL. Text messaging reminders to reduce non-attendance in chronic disease follow-up: a clinical trial. Br J Gen Pract. 2009 doi: 10.3399/bjgp09X472250. Available from: http://www.ncbi.nlm.nih.gov.offcampus.lib.washington.edu/pubmed/19712544. [DOI] [PMC free article] [PubMed]
- 35.Kopp J. Self-monitoring: A literature review of research and practice. Social Work Research & Abstracts. 1988;24:8–20. [Google Scholar]
- 36.Mace FC, Kratochwill TR. Theories of reactivity in self-monitoring. Behavior Modification. 1985;9(3):323–343. [Google Scholar]
- 37.McFall RM. Parameters of self-monitoring. In: Stuart RB, editor. Behavioral self-management: Strategies, techniques and outcomes. New York: Brunner/Mazel, Publishers; 1977. [Google Scholar]
- 38.Nelson RO. Assessment and therapeutic functions of self-monitoring. In: Hersen M, Eisler RM, Miller PM, editors. Progress in behavior modification. New York: Academic Press; 1977. [Google Scholar]
- 39.Gasser R, Brodbeck D, Degen M, Luthiger J, Wyss R, Reichlin S. Proc Persuasive Tech ‘06. Springer-Verlag; 2006. Persuasiveness of a Mobile Lifestyle Coaching Application Using Social Facilitation; pp. 27–38. [Google Scholar]
- 40.Kollmann A, Riedl M, Kastner P, Schreier G, Ludvik B. Feasibility of a mobile phone-based data service for functional insulin treatment of type 1 diabetes mellitus patients. J Med Internet Res. 2007;9(5):e36. doi: 10.2196/jmir.9.5.e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Walters D, Sarela A, Fairfull A, Neighbour K, Cowen C, Stephens B, et al. A mobile phone-based care model for outpatient cardiac rehabilitation: the care assessment platform (CAP) BMC Cardiovasc Disord. 2010;10(1):5. doi: 10.1186/1471-2261-10-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tsai CC, Lee G, Raab F, Norman GJ, Sohn T, Griswold W, et al. Usability and feasability of PmEB: A mobile phone application for monitoring real time caloric balance. Mobile Networks and Applications. 2007;12(2–3):173–184. [Google Scholar]
- 43.Holtz B, Whitten P. Managing asthma with mobile phones: a feasibility study. Telemed J E Health. 2009;15(9):907–909. doi: 10.1089/tmj.2009.0048. [DOI] [PubMed] [Google Scholar]
- 44.Franklin VL, Waller A, Pagliari C, Greene SA. “Sweet Talk”: text messaging support for intensive insulin therapy for young people with diabetes. Diabetes Technol Ther. 2003;5(6):991–996. doi: 10.1089/152091503322641042. [DOI] [PubMed] [Google Scholar]
- 45.Choudhury T, Borriello G, Consolvo S, Haehnel D, Harrison B, Hemigway B, et al. The Mobile Sensing Platform: An embedded activity recognition system. IEEE Pervasive Computing. 2008;7(2):32–41. [Google Scholar]
- 46.Saponas TS, Lester J, Froehlich J, Fogarty J, Landay JA. iLearn on the iPhone: Real-time human activity classification on commodity mobile phones. Seattle, WA: University of Washington; 2008. [Google Scholar]
- 47.Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management: the NICHE pilot study. J Eval Clin Pract. 2008;14(3):465–469. doi: 10.1111/j.1365-2753.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- 48.Truong KN, Hayes GR. Ubiquitous computing for capture and access. Foundations and Trends in Human-Computer Interaction. 2009;2(2):95–171. [Google Scholar]
- 49.Klasnja P, Consolvo S, Choudhury T, Beckwith R, Hightower J. Exploring Privacy Concerns about Personal Sensing. In: Tokuda H, Beigl M, Friday A, Brush AJB, Tobe Y, editors. Pervasive Computing. Berlin, Heidelberg: Springer Berlin Heidelberg; 2009. pp. 176–183. [Google Scholar]
- 50.Farmer A, Gibson O, Hayton P, Bryden K, Dudley C, Neil A, et al. A real-time, mobile phone-based telemedicine system to support young adults with type 1 diabetes. Inform PrimCare. 2005;13:171–178. doi: 10.14236/jhi.v13i3.594. [DOI] [PubMed] [Google Scholar]
- 51.Kim S-I, Kim H-S. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform. 2008;77(6):399–404. doi: 10.1016/j.ijmedinf.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 52.Park M-J, Kim H-S, Kim K-S. Cellular phone and Internet-based individual intervention on blood pressure and obesity in obese patients with hypertension. Int J of Med Inform. 2009;78(10):704–710. doi: 10.1016/j.ijmedinf.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 53.Franklin VL, Greene A, Waller A, Greene SA, Pagliari C. Patients’ engagement with “Sweet Talk”-a text messaging support system for young people with diabetes. J Med Internet Res. 2008;10(2):e20. doi: 10.2196/jmir.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Villalba E, Salvi D, Ottaviano M, Peinado I, Arredondo MT, Akay A. Wearable and mobile system to manage remotely heart failure. IEEE Trans Inf Technol Biomed. 2009;13(6):990–996. doi: 10.1109/TITB.2009.2026572. [DOI] [PubMed] [Google Scholar]
- 55.Villalba E, Ottaviano M, Arredondo MT, Martinez A, Guillen S. Wearable monitoring system for heart failure assessment in a mobile environment. Computers in Cardiology. 2006;33:237–240. [Google Scholar]
- 56.Kearney N, McCann L, Norrie J, Taylor L, Gray P, McGee-Lennon M, et al. Evaluation of a mobile phone-based, advanced symptom management system (ASyMS©) in the management of chemotherapy-related toxicity. Support Care Cancer. 2008;17(4):437–444. doi: 10.1007/s00520-008-0515-0. [DOI] [PubMed] [Google Scholar]
- 57.Larsen ME, Rowntree J, Young AM, Pearson S, Smith J, Gibson OJ, et al. Chemotherapy side effect management using mobile phones. Conf Proc IEEE Eng Med Biol Soc. 2008:5152–5155. doi: 10.1109/IEMBS.2008.4650374. [DOI] [PubMed] [Google Scholar]
- 58.McCann L, Maguire R, Miller M, Kearney N. Patients’ perceptions and experiences of using a mobile phone-based advanced symptom management system (ASyMS) to monitor and manage chemotherapy related toxicity. Eur J Cancer Care (Engl) 2009;18(2):156–164. doi: 10.1111/j.1365-2354.2008.00938.x. [DOI] [PubMed] [Google Scholar]
- 59.Weaver A, Young AM, Rowntree J, Townsend N, Pearson S, Smith J, et al. Application of mobile phone technology for managing chemotherapy-associated side-effects. Ann Oncol. 2007;18(11):1887–1892. doi: 10.1093/annonc/mdm354. [DOI] [PubMed] [Google Scholar]
- 60.Scherr D, Kastner P, Kollmann A, Hallas A, Auer J, Krappinger H, et al. Effect of home-based telemonitoring using mobile phone technology on the outcome of heart failure patients after an episode of acute decompensation:randomized controlled trial. J Med Internet Res. 2009;11(3):e34. doi: 10.2196/jmir.1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Morris M, Guilak F. Mobile Heart Health: Project Highlight. IEEE Pervasive Computing. 2009;8(2):57–61. [Google Scholar]
- 62.Morris M, Kathawala Q, Leen TK, Gorenstein EE, Guilak F, Labhard M, et al. Mobile therapy: Case study evaluations of a cell phone application for emotional self-awareness. J Med Internet Res. 2010;12(2):e10. doi: 10.2196/jmir.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- 64.Wang CY, Fenske MM. Self-care of adults with non-insulin-dependent diabetes mellitus: influence of family and friends. Diabetes Educ. 1996;22(5):465–470. doi: 10.1177/014572179602200506. [DOI] [PubMed] [Google Scholar]
- 65.Moore SM, Dolansky MA, Ruland CM, Pashkow FJ, Blackburn GG. Predictors of women’s exercise maintenance after cardiac rehabilitation. J Cardiopulm Rehabil. 2003;23(1):40–49. doi: 10.1097/00008483-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 66.Chin MH, Goldman L. Factors contributing to the hospitalization of patients with congestive heart failure. Am J Public Health. 1997;87(4):643–648. doi: 10.2105/ajph.87.4.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schwarz KA, Elman CS. Identification of factors predictive of hospital readmissions for patients with heart failure. Heart Lung. 2003;32(2):88–99. doi: 10.1067/mhl.2003.15. [DOI] [PubMed] [Google Scholar]
- 68.Coyne JC, Rohrbaugh MJ, Shoham V, Sonnega JS, Nicklas JM, Cranford JA. Prognostic importance of marital quality for survival of congestive heart failure. Am J Cardiol. 2001;88(5):526–529. doi: 10.1016/s0002-9149(01)01731-3. [DOI] [PubMed] [Google Scholar]
- 69.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 70.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Consolvo S, Everitt KM, Smith I, Landay JA. Proc CHI 2006. ACM Press; 2006. Design requirements for technologies that encourage physical activity; pp. 457–466. [Google Scholar]
- 72.Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin R-B, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. Tob Control. 2005;14(4):255–261. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lin JL, Mamykina L, Lindtner S, Delajoux G, Strub HB. Proc UbiComp 2006. Springer; 2006. Fish’n’Steps: Encouraging physical activity with an interactive computer game; pp. 261–278. [Google Scholar]
- 74.Riley W, Obermayer J, Jean-Mary J. Internet and Mobile Phone Text Messaging Intervention for College Smokers. J Am Coll Health. 2008;57(2):245–248. doi: 10.3200/JACH.57.2.245-248. [DOI] [PubMed] [Google Scholar]
- 75.Whittaker R, Maddison R, McRobbie H, Bullen C, Denny S, Dorey E, et al. A multimedia mobile phone-based youth smoking cessation intervention: findings from content development and piloting studies. J Med Internet Res. 2008;10(5):e49. doi: 10.2196/jmir.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Grimes A, Bednar M, Bolter JD, Grinter RE. Proc CSCW 2008. ACM; 2008. EatWell: sharing nutrition-related memories in a low-income community; pp. 87–96. [Google Scholar]
- 77.Grimes A, Landry BM, Grinter RE. Proc CSCW 2010. ACM; 2010. Characteristics of shared health reflections in a local community; pp. 435–444. [Google Scholar]
- 78.Bargh JA, Gollwitzer PM, Lee-Chai A, Barndollar K, Trötschel R. The automated will: Nonconscious activation and pursuit of behavioral goals. J of Pers Soc Psychol. 2001;81(6):1014–1027. [PMC free article] [PubMed] [Google Scholar]
- 79.Gerber BS, Stolley MR, Thompson AL, Sharp LK, Fitzgibbon ML. Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study. Health Informatics J. 2009;15(1):17–25. doi: 10.1177/1460458208099865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med. 2009;36(2):165–173. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 81.Curioso WH, Quistberg DA, Cabello R, Gozzer E, Garcia PJ, Holmes KK, et al. AMIA Annual Sym Proc. American Medical Informatics Association; 2009. “It’s time for your life”: How should we remind patients to take medicines using short text messages? pp. 129–133. [PMC free article] [PubMed] [Google Scholar]
- 82.Strandbygaard U, Thomsen SF, Backer V. A daily SMS reminder increases adherence to asthma treatment: a three-month follow-up study. Respir Med. 2010;104(2):166–171. doi: 10.1016/j.rmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 83.Ollivier L, Romand O, Marimoutou C, Michel R, Pognant C, Todesco A, et al. Use of short message service (SMS) to improve malaria chemoprophylaxis compliance after returning from a malaria endemic area. Malar J. 2009;8:236. doi: 10.1186/1475-2875-8-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mackenzie H. A text messaging trial in family planning clinics. Stud Health Technol Inform. 2009;146:154–159. [PubMed] [Google Scholar]
- 85.Castaño PM, Martínez RA. Harnessing technology for adolescent health promotion. Adolesc Med State Art Rev. 2007;18(2):400–406. xiii. [PubMed] [Google Scholar]
- 86.Fitzsimons GM, Bargh JA. Automatic self-regulation. In: Vohs KD, Baumeister RF, editors. Handbook of self-regulation: Research, theory, and applications. New York: The Guilford Press; 2004. pp. 151–170. [Google Scholar]
- 87.Chiu M-C, Chang S-P, Chang Y-C, Chu H-H, Chen CC-H, Hsiao F-H, et al. Proc UbiCom 2009. ACM; 2009. Playful bottle: a mobile social persuasion system to motivate healthy water intake; pp. 185–194. [Google Scholar]
- 88.Mueller F, Gibbs M. Proc OzCHI ‘06. ACM; 2006. A table tennis game for three players; pp. 321–324. [Google Scholar]
- 89.Mueller F, Gibbs MR, Vetere F. Proc CHI 2009. ACM; 2009. Design influence on social play in distributed exertion games; pp. 1539–1548. [Google Scholar]
- 90.Harris L, DeShazo JP, Pratt W. Health Informatics: A patient centered approach to Diabetes. MIT Press; 2010. Diabetes and Obesity: Can Video Games Help? In: Hayes BM, Aspray W, editors; pp. 131–149. [Google Scholar]
- 91.Grimes A, Kantroo V, Grinter RE. Proc UbiCom 2010. ACM; 2010. Let’s play!: mobile health games for adults; pp. 241–250. [Google Scholar]
- 92.Froehlich J, Chen MY, Consolvo S, Harrison BL, Landay JA. Proc MobiSys ‘07. ACM Press; 2007. MyExperience: A system for in situ tracing and capturing of user feedback on mobile phones; pp. 57–70. [Google Scholar]
- 93.Anokwa Y, Hartung C, Brunette W, Borriello G, Lerer A. Open source data collection in the developing world. Computer. 2009;42(10):97–99. [Google Scholar]
- 94.Berkovsky S, Freyne J, Coombe M, Bhandari D, Baghaei N. Proc OzCHI ‘09. ACM; 2009. Physical activity motivating games: you can play, mate! pp. 273–276. [Google Scholar]
- 95.Pratt W, Unruh K, Civan A, Skeels MM. Personal health information management. Communications of the ACM. 2006;49(1):51–55. [Google Scholar]
- 96.Klasnja P, Civan Hartzler A, Unruh KT, Pratt W. Proc CHI 2010. ACM Press; 2010. Blowing in the wind: Unanchored patient information work during cancer care; pp. 193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Klasnja P, Hartzler A, Powell C, Phan G, Pratt W. AMIA Ann Sym Proc. American Medical Informatics Association; 2010. HealthWeaver Mobile: Designing a mobile tool for managing personal health information during cancer care; pp. 392–396. [PMC free article] [PubMed] [Google Scholar]
- 98.Liu LS, Hirano SH, Tentori M, Cheng KG, George S, Park SY, et al. Proc CSCW 2011. ACM; 2011. Improving communication and social support for caregivers of high-risk infants through mobile technologies; pp. 475–484. [Google Scholar]