Abstract
Background
Despite the importance of understanding the long-term outcome for children of alcohol dependent (AD) women, the available literature is largely based on offspring of AD fathers and few have utilized prospective designs that include child, adolescent and young adult assessments. Multiplex AD families in which multiple cases of AD are present provide an ideal setting for understanding developmental variants of the adult phenotype.
Method
Offspring from multiplex AD families identified through the mother or control families were evaluated multiple times during childhood and followed to young adulthood. Familial risk status and the presence of specific child/adolescent disorders were used as predictors of substance use disorder outcome by young adulthood.
Results
Offspring who were members of maternal multiplex families had elevated rates of child and young adulthood disorders. High risk offspring of alcohol dependent women were at increased risk for externalizing (Conduct Disorder and ADHD) and internalizing disorders (Major Depressive Disorder (MDD) and Anxiety Disorders). By young adulthood, offspring from these multiplex families had significantly greater odds of developing alcohol abuse or dependence (odds ratio [OR] = 3.63 [CI 1.36–9.64] and drug abuse or dependence (OR = 4.23 [CI 1.73–10.32]). The prospective design of the study revealed that specific childhood disorders (Conduct Disorder, ADHD, MDD) increased the odds of subsequent development of substance use disorder (SUD).
Conclusions
Multiplex familial risk for alcohol dependence is a significant predictor of substance use disorders by young adulthood. Familial risk and an earlier childhood disorder may set the stage for later development of SUD.
Keywords: high-risk, psychopathology, alcohol dependence, substance use disorders, women
It is now well-known that offspring of alcohol dependent (AD) parents are themselves more likely to develop alcohol and drug dependence by young adulthood (Bohman, 1978; Cloninger et al., 1981; Goodwin et al., 1973; Kendler et al., 2008). Multiple studies show that children of alcohol and drug dependent individuals have an increased risk for developing externalizing disorders including elevations in Conduct Disorder (CD), oppositional Defiant Disorder (ODD), and Attention Deficit Hyperactivity Disorder (ADHD) (Kuperman et al 2005; Ohannessian et al 2004; Hill and Muka, 1996; Hill et al 1999; Hill et al 2008; Earls and Powell, 1988; Reich et al 1993; Kuperman et al 1999; Merikangas et al 2000). Elevations in internalizing disorders have also been noted, particularly for overanxious disorder (Reich et al 1993) and affective disorders (Hill and Muka, 1996; Hill et al 1999; Hill et al 2008).
Prevalence estimates for child and adolescent disorders among offspring of AD parents is complicated by the array of disorders examined (e.g., only Conduct Disorder or ADHD) in some studies (Biederman et al 2006; Elkins et al 2007) versus a full-spectrum of disorders including internalizing psychopathology in others (Schuckit et al 2000). In the few longitudinal studies that exist, age at study entry and follow up are quite varied and follow up often does not extend into young adulthood (Biederman et al 2006; Elkins et al 2007). Many studies that have examined the effects of childhood psychopathology on later development of substance use disorders have not controlled for family history of substance use disorders (Elkins et al 2007; Hofmann et al 2009), or if family history data was collected was limited because it was based on a single informant (Goldstein et al 2007). Some large-scale epidemiological surveys that have assessed prodromal childhood risk factors for later development of substance use disorders have relied on retrospective report of childhood disorders (Goldstein et al 2007; Hofmann et al 2009).
Few studies have the benefit of studying offspring from families where multiple cases of alcohol dependence or related phenotypes are present. Offspring from unselected families of alcohol dependent parents differ from offspring from multiplex families in which there are multiple cases of alcohol dependence (AD), the latter having an even greater risk for developing AD (Hill et al 2008) with an earlier age of onset to begin regular drinking (Hill et al 2000). Offspring from multiplex families have now been studied in the Collaborative Study on the Genetics of Alcoholism (COGA) study (Kuperman et al 2005; Ohannessian et al 2004) and from our samples (Hill and Muka, 1996; Hill et al 1999; Hill et al 2008). Multiplex families provide a distinct advantage for attempts to understand possible developmental variants of adult substance use disorder phenotypes. With the high rate of alcohol dependent individuals seen in these families, it is quite likely that genes with a substantial contribution to AD susceptibility are likely to be segregating within these families. Additionally, with the recognition that genes can have pleiotropic effects, there is now increased interest in identifying phenotypes of adolescence that may portend development of adult disorders. Dick et al (2006) has identified Conduct Disorder of adolescence as one such variant of substance use disorder risk that may be related to GARBA2 variation.
Although the offspring of alcohol dependent parents are known to have increased risk for developing substance use disorders, identification of the moderating and mediating factors that influence the likelihood that adolescents will develop alcohol and drug abuse and dependence in young adulthood is not well documented. Among the factors that have been identified is the age at which the individual begins drinking (Robins and Pryzbeck, 1985; Ghodosian and Power, 1987; Grant and Dawson, 1997; Dawson et al 2007), which in turn appears to be related to having a more extraverted personality (Hill et al 2000) and a family history of alcohol dependence. Early onset to begin drinking appears to be part of a generalized tendency to exhibit disinhibited behavior including an earlier onset to begin smoking, to engage in sexual behavior, and to use illegal drugs (McGue et al 2001). Undercontrolled or externalizing behaviors of childhood and adolescence are often seen in offspring from alcohol dependent families (Kuperman et al., 1999; Hill and Muka, 1996; Ohannessian et al., 2004) and increase the risk for substance use disorders during adulthood. What appears to be lacking is a description of the relative importance of externalizing and internalizing disorders of childhood/adolescence on young adult outcome. Also, lacking is information concerning the extent to which the predictors remain significant when evaluated against familial genetic loading for substance use disorders.
Only a few studies have investigated the diagnostic outcome of children with alcohol dependent mothers or those from families with high familial maternal loading for AD (Kendler et al 1994; Hill and Muka, 1996; Leib et al 2002; Walden et al 2007; Hill et al 2008; Slutske et al 2008). Hill and Muka (1996) found that the relative risk for childhood psychopathology among the offspring of alcoholic mothers was 1.76 (95% confidence interval = 1.01 to 3.09), comparable to the elevated risk observed in family studies of alcohol dependent fathers (Hill et al., 1999). Hill et al (2008) recently reported that risk to offspring of alcohol dependent mothers is especially high when presence of any psychiatric disorder is considered (OR = 3.97, q < 0.001), and particularly so for externalizing disorders (OR = 5.34, q < 0.001).
Currently, the prevalence of psychiatric disorder by young adulthood among offspring of women who are alcohol dependent is not well documented. It appears that these offspring are at greater risk of developing alcohol dependence and other substance use disorders (Hill et al 2008). Also, though there is general agreement that such high risk offspring are more prone to experience a variety of emotional disorders during childhood and adolescence, significant gaps in our knowledge of the specific risk factors that antedate the development of substance use disorders persists. An ongoing prospective study of offspring who were evaluated at approximately yearly intervals in childhood and adolescence and biennially in young adulthood provided the opportunity to relate previous child/adolescent psychopathology to young adult outcome. A survival analysis framework was chosen for analysis of the data to allow appropriate correction for the differing ages of the participants at the time of the last follow-up.
Methods
Description of the Family Study
The present report is based on offspring currently enrolled in prospective family study. The offspring are from either maternal multiplex AD families (high-risk) or control families (low-risk). These offspring were evaluated multiple times during childhood at approximately yearly intervals and every two years during young adulthood. Including the most recent follow up visit, 85% of the offspring entered into the study have been retained.
Inclusion Criteria for High-Risk Families
The high-risk families were identified through a proband pair of alcohol dependent sisters. One member of the proband pair was in a substance abuse treatment facility in the Pittsburgh area at the time of recruitment. Determination that this individual had a sibling similarly affected with alcohol dependence was made using structured screening instruments. Both members of the proband pair were screened using the Diagnostic Interview Schedule (DIS) (Robins et al., 1981) to determine the presence of alcohol dependence (AD) and other Axis I (DSM-III) psychopathology (Feighner Criteria [Feighner et al 1972]). Each multiplex family required the screening of approximately 100 families to meet the present goals, and for the broader goals of family studies ongoing in our laboratory that include a search for developmental neurobiological markers (Hill et al., 2009a,b) and gene finding efforts (Hill et al., 2004).
Exclusion Criteria for High-Risk Families
The DIS was administered to all available relatives (adult probands, their siblings and parents. Unavailable or deceased relatives were diagnosed by family-history reports. Targeted families were excluded if the proband or her first-degree relatives showed evidence of primary recurrent Major Depressive Disorder (MDD), Bipolar Disorder (BD), Primary Drug Dependence (PDD) (i.e., drug dependence preceded alcohol dependence by 1 or more years) or Schizophrenia by DSM-III criteria, the diagnostic system in place at the time the studies were initiated. Presence of Axis II disorders was not used as either an exclusionary or inclusionary condition. No attempt was made to limit the psychiatric disorders in “marrying in” spouses who represent the parents of the children/adolescents reported here. However, available spouses were diagnosed using the same methods (DIS) as members of the “target” families. Presence of alcohol dependence in mothers and fathers may be seen in Table 1.
Table 1.
| A. Maternal and paternal diagnoses of Alcohol Dependence by Risk Group and Method of Diagnosis. | ||||||||
|---|---|---|---|---|---|---|---|---|
| High Risk | Low Risk | |||||||
| Mothers | Fathers | Mothers | Fathers a | |||||
| Alcohol Dependent |
Not AD |
Alcohol Dependent |
Not AD |
Alcohol Dependent |
Not AD |
Alcohol Dependent |
Not AD |
|
|
DIS In Person Interview |
88 | 11 | 6 | 17 | 2 | 85 | 9 | 36 |
|
Spouse Family History b |
0 | 4 | 54 | 26 | 0 | 6 | 5 | 41 |
| Total | 88 85.4% |
15 14.6% |
60 58.3% |
43 41.7% |
2 2.2% |
91 97.8% |
14 15.4% |
77 84.6% |
| b. Parental Pairs Concordant and Discordant for Alcohol Dependence by Risk group | |||||
|---|---|---|---|---|---|
| Parental Pairs | |||||
| High Risk | Low Risk | ||||
| Neither AD | 9 a | 8.7% | Neither AD | 76 | 83.5% |
| One AD | 40 | 38.8% | One AD b | 14 | 15.4% |
| Both AD | 54 | 52.4% | Both AD b | 1 | 1.1% |
No information was available for 2 fathers either by family history or direct interview.
Could not distinguish whether the parent also had drug dependence by family history
Offspring of the female AD proband pairs were included in the study, as well as their female and male siblings’ offspring some of whom were not alcohol dependent nor were their spouses (co-parent of child).
The low risk control group was chosen from the general population (same census tracks as high risk families). Some of the parents met criteria for alcohol dependence though none had a second alcohol dependent sibling that would have qualified the family to be multiplex for alcohol dependence.
Selection of Control Families
Selection of control families was based on availability of families with children between the ages of 8–18. Each control family was selected on basis of residence within a census track from which a high risk family had been selected with an attempt made to yoke each control family to a high risk family in the study. Random phone calls were made to homes within the census track to determine if the family had available children and were interested in participating in the study. Those expressing an interest were sent a letter of introduction. Parents were screened for absence of alcohol and drug dependence using the DIS but other psychopathology was free to vary (Table 1).
Child/Adolescent Assessment for DSM-III Diagnoses
Each child/adolescent and his/her parent were separately administered the Schedule for Affective Disorders and Schizophrenia (K-SADS) (Chambers et al., 1985) by trained, Masters’ level, clinical interviewers and an advanced resident in child psychiatry at each annual evaluation. Using DSM-III criteria that have been used throughout the follow-up, K-SADS interviewers and the resident independently provided scores for each diagnosis. A best-estimate diagnosis based on these four blinded interviews was completed in the presence of a third clinician who facilitated discussion to resolve diagnostic disagreements if needed.
Young Adult Assessment for DSM-IV Diagnoses
Offspring who had reached their 19th birthday were evaluated by Master’s level clinical interviewers using the Composite International Diagnostic Interview (CIDI; Janca et al 1992) to determine the presence or absence of a DSM-IV Axis I diagnosis. The CIDI-SAM (Substance Abuse Module; Cottler et al. 1989) was also administered in order to determine quantity, frequency, and pattern of drug and alcohol use. Interrater reliability for interviewers on the diagnostic instruments used in this study exceeded 90%.
Participants
The present report is based on analysis of data for 196 offspring who were evaluated during childhood and adolescence (ages 8 to 18). High risk offspring from maternal multiplex families (N = 103) (46 male and 57 female), or low-risk offspring (N = 93) selected for minimal familial substance use disorders (53 male and 40 female) were assessed at approximately annual intervals multiple times (Table 2a). The present report is based on a total of 1,119 assessments. To date, 116 have been evaluated during young adulthood (19–30 years of age) (Table 2b). The study has ongoing approval from the University of Pittsburgh Institutional Review Board. All participants provided informed consent at each follow-up visit. Children provided assent with parental consent.
Table 2.
| a. Age at First and Last Follow Up Visit and Number of Evaluations for High and Low-Risk Offspring Recruited in Childhood (N=196) | ||
|---|---|---|
| High-Risk (N = 103) |
Low-Risk (N = 93) |
|
| Gender | ||
| Male | 46 | 53 |
| Female | 57 | 40 |
|
Average Age at initial assessment* |
11.20 ± 2.77 | 11.48 ± 2.73 |
| Average Age at Last assessment | 19.54 ± 5.43 | 19.59 ± 4.51 |
|
Average Number of Child and Young Adult Evaluations |
5.15 ± 2.84 | 6.33 ± 2.79 |
|
Average Number of Child Evaluations |
4.12 ± 2.43 | 5.20 ± 2.71 |
| b. Demographic Characteristics of High and Low-Risk Offspring Currently Followed to Young Adulthood (N=116) | ||
|---|---|---|
| High-Risk (N= 58 ) |
Low-Risk (N= 58) |
|
| Gender | 20 | 32 |
| Male | 38 | 26 |
| Female | ||
|
Average Age at initial assessment |
11.62 ± 2.78 | 12.60 ± 2.33 |
|
Average Age at Last assessment* |
23.53 ± 2.98 | 22.38 ± 2.54 |
|
Average Number of Child and Young Adult Evaluations |
6.24 ± 2.74 | 6.74 ± 2.51 |
|
Average Number of Child Evaluations |
4.43 ± 2.49 | 4.93 ± 2.42 |
|
Average Number of Young Adult Evaluations |
1.81 ± 0.76 | 1.81 ± 0.66 |
High risk offspring range = 8–18; Low- Risk Offspring = 8–17
High Risk offspring range = 19–30; Low-Risk offspring 19–28
Statistical Analyses
The first goal of the analyses was to evaluate the effects of familial risk status on the odds that offspring would develop specific psychiatric disorders by young adulthood. Because the offspring varied in age at entry into the study and at their last follow up visit, survival analyses were performed. Appropriate adjustment for varying age at follow up can be made through censoring of data inherent in survival methods (Kaplan-Meier or Cox Regression (Parmar and Machin, 1995). Kaplan-Meier (nonparametric) survival-analyses were used to determine the proportion of offspring in each risk group who had developed a given psychiatric disorder at each age during the observation period (Kaplan and Meier, 1958). Cox Regression analyses were performed to obtain β and the exponent of β using SPSS (Version 17) to estimate the odds associated with variables of interest. (The exponent of β is computationally equivalent to the odds ratio.)
The second goal of the statistical analysis was to determine the impact of having specific child/adolescent diagnoses on subsequent development of substance use disorders in young adulthood controlling for familial risk status. To do this, stepwise Cox regression models (Cox and Oakes, 1984) were used to estimate the influence of potential moderators (presence of specific childhood disorders) that might influence the relationship between familial risk and the incidence rate of a psychiatric outcome in young adulthood (SPSS version 16; SPSS, Chicago, Illinois). The Cox models were run evaluating each possible predictor (Conduct Disorder, ADHD, MDD, and Anxiety Disorders) and each outcome: (1) Alcohol Abuse and Dependence; (2) Drug Abuse and Dependence; (3) Alcohol or Drug Abuse and Dependence (substance use disorder [SUD]). Models were tested controlling for risk to evaluate the increase in the odds of developing each of these three outcomes in association with the predictors.
A third goal was to test the childhood predictors within each gender to determine if the predictor was equally salient in both males and females. Finally, our fourth goal was to test the childhood predictors of young adult outcome within each risk group to determine if childhood disorders identified as significant predictors within one risk group were equally predictive within the other.
Results
Effects of Familial Risk Status
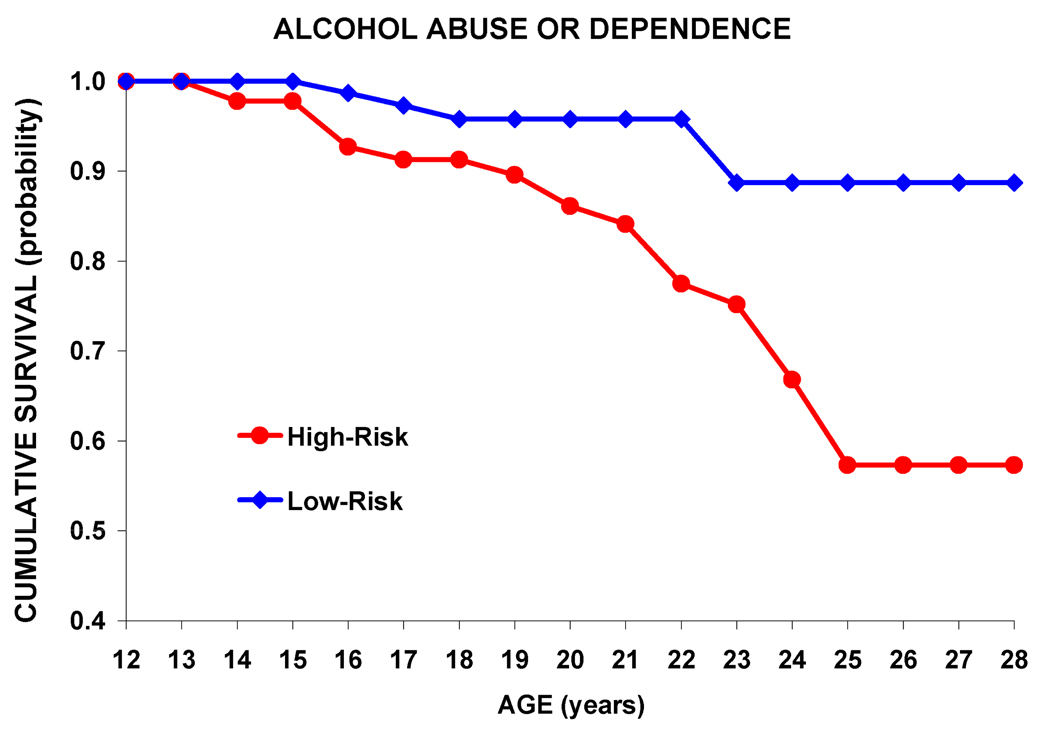
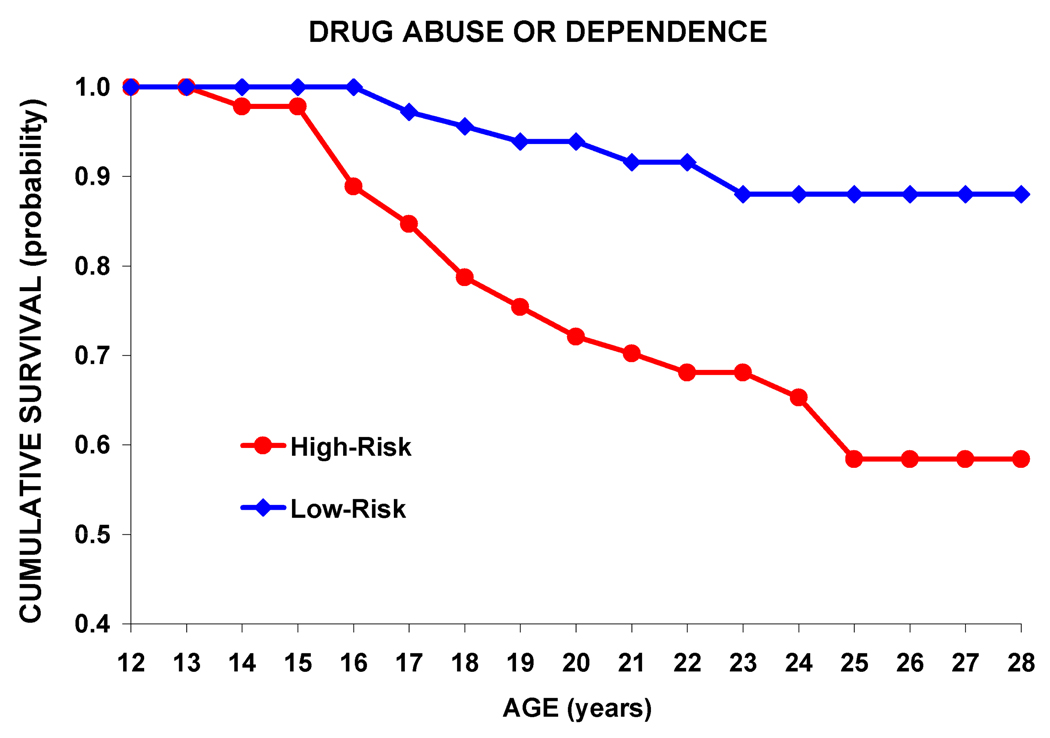
Analyses were performed contrasting high and low risk offspring for four different outcomes: alcohol abuse, drug abuse, alcohol dependence and drug dependence adjusting for the participant’s age at last visit through use of survival analyses. For participants who received a positive substance use disorder diagnosis before the age of 18, the diagnosis was made using information from the K-SADS instrument, and therefore, was determined by DSM-III criteria. If a positive diagnosis occurred after the age of 19, the diagnosis was obtained from administration of the CIDI interview and was based on DSM-IV criteria. Offspring from multiplex AD families had a significantly earlier onset for Alcohol Abuse and Alcohol Dependence (Figure 1) and Drug Abuse and Drug Dependence (Figure 2). Comparison of Figures 1 and 2 shows a steeper slope for drug abuse/dependence than alcohol abuse/dependence for high risk offspring, suggesting that drug abuse/dependence occurs earlier than does alcohol abuse/dependence.
Figure 1.
Kaplan-Meier survival curves for Alcohol Abuse and Alcohol Dependence for the high-risk and low-risk offspring. An earlier onset for development of either abuse or dependence is seen in offspring from families of alcohol dependent women (Tarone-Ware χ2 = 7.14, df = 1, p =0.008).
Figure 2.
Kaplan-Meier survival curves for drug abuse and dependence for the high-risk and low-risk offspring An earlier onset for development of either Drug Abuse or Drug Dependence is seen in offspring from families of alcohol dependent women (Tarone-Ware χ2 = 12.70, df = 1, p = <0.001.
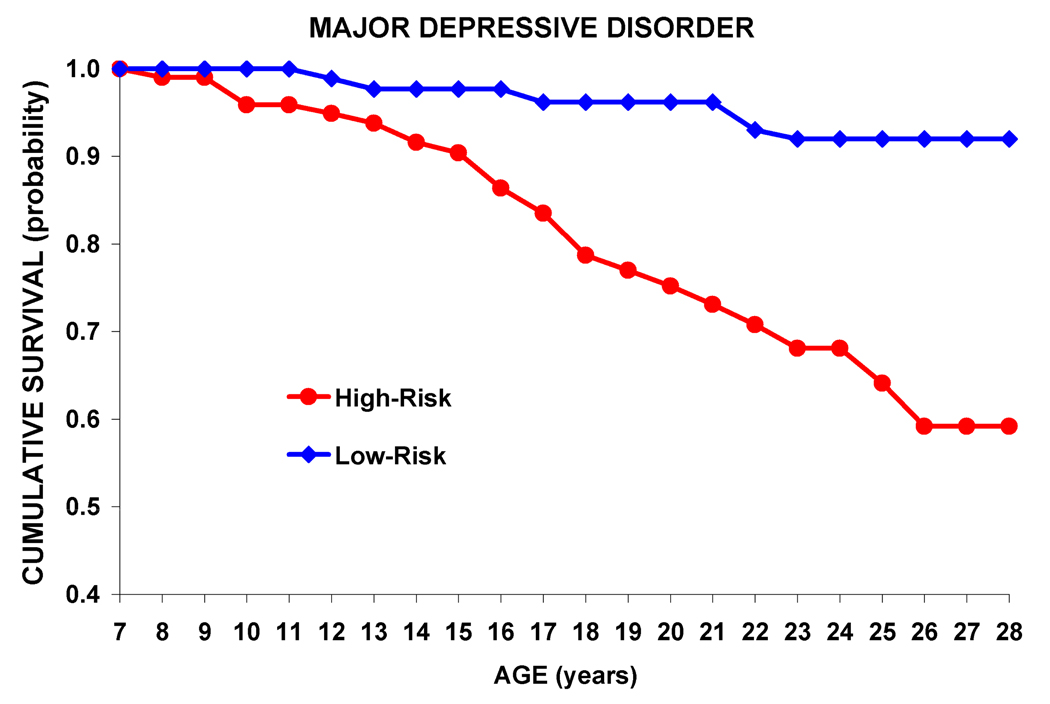
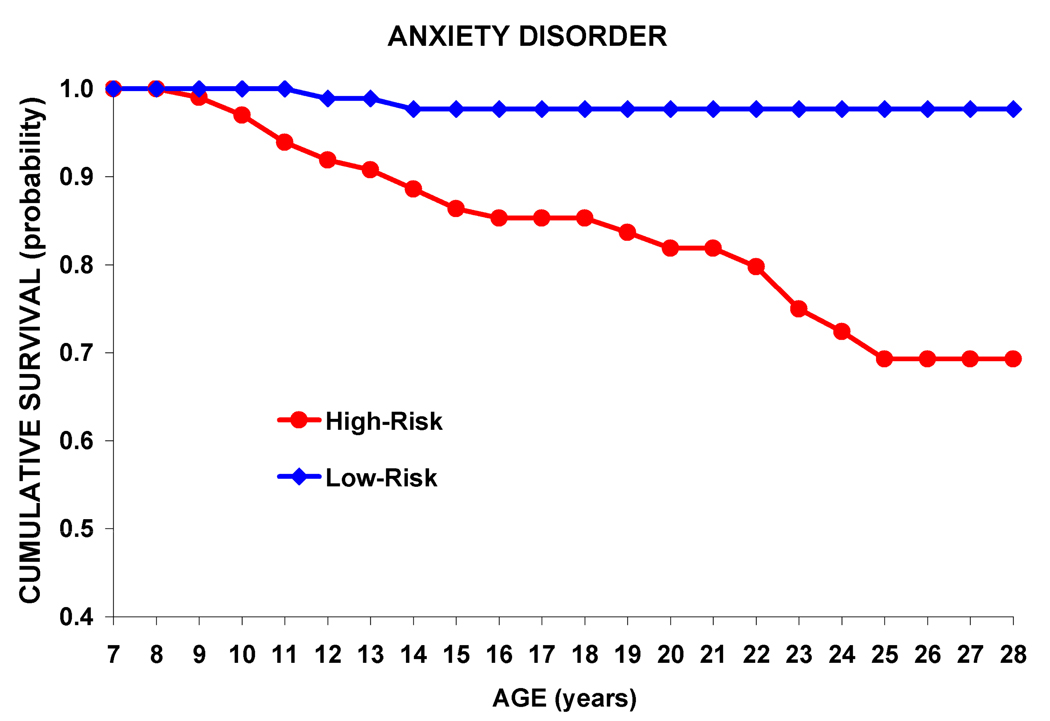
An earlier onset for development of Major Depressive Disorder (Figure 3) and for developing an Anxiety Disorders (Figure 4) is also seen among high risk offspring. Major depressive disorder (MDD) and Anxiety Disorders diagnoses were based on a DSM-III (K-SADS) diagnosis if present before age 18 and based on a DSM-IV (CIDI) diagnosis for those over age 19. As may be seen, MDD affected approximately 25 % of the high risk offspring by age 21.
Figure 3.
Kaplan-Meier survival curves for onset of Major Depressive Disorder for high-risk and low-risk offspring shows a significantly earlier onset for the high-risk offspring (Tarone-Ware χ2 = 13.91, df = 1, p = <0.001).
Figure 4.
Kaplan-Meier survival curves for onset of Anxiety Disorders for high-risk and low-risk offspring shows high risk offspring with significantly earlier onset (Tarone-Ware χ2 = 14.42, df = 1, p = <0.001).
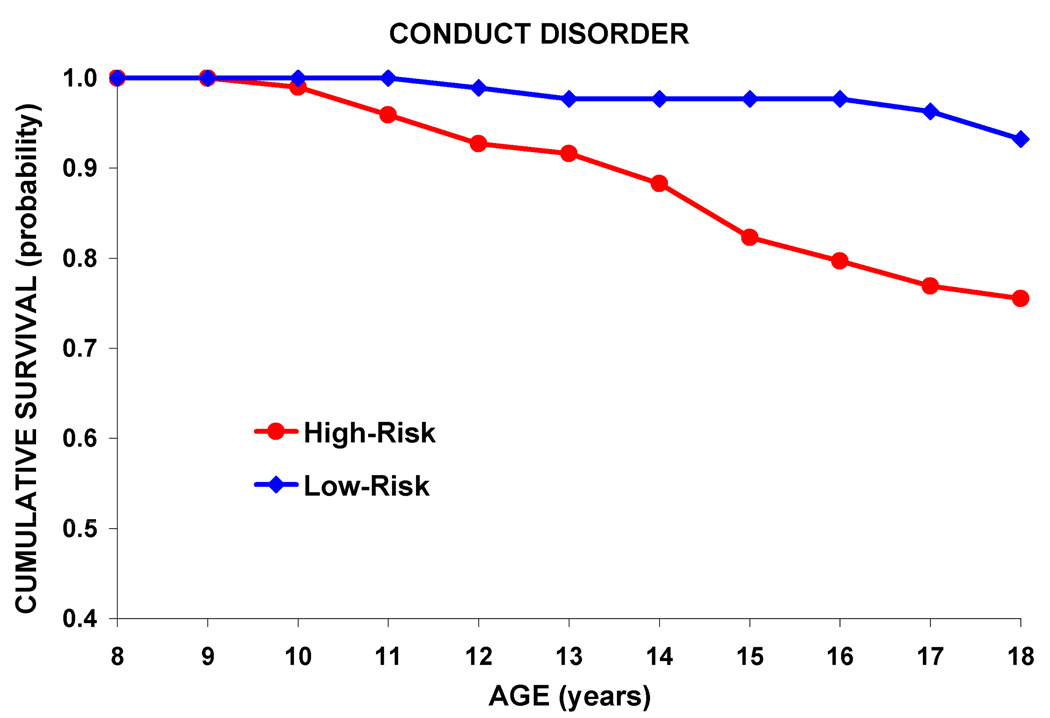
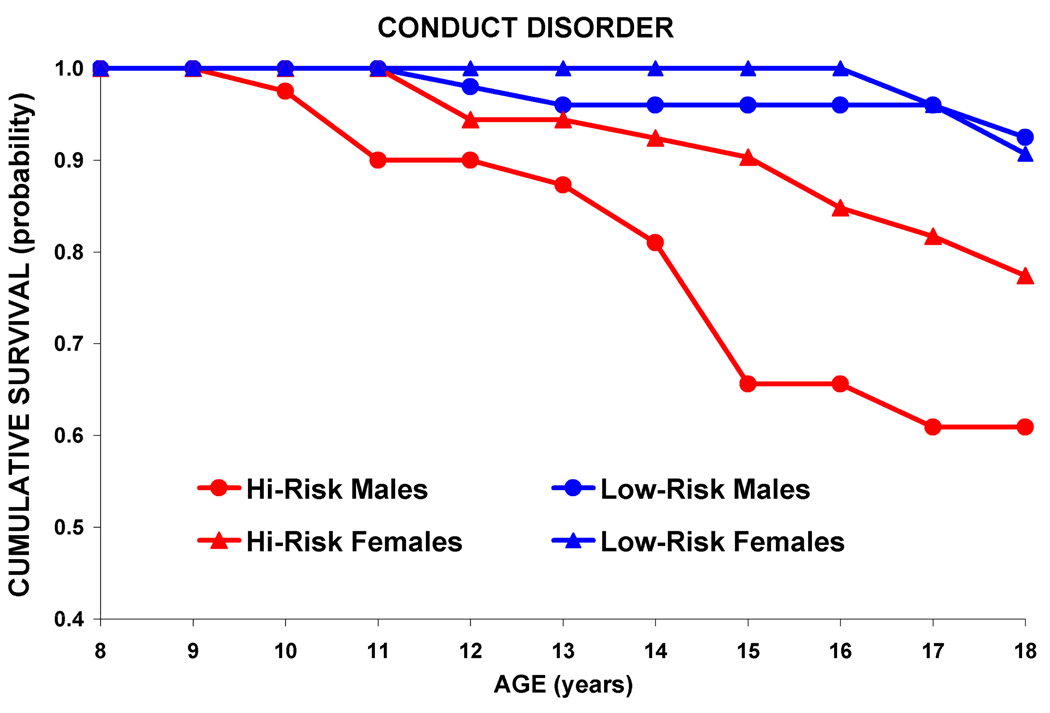
A greater proportion of high risk offspring had Conduct Disorder with over 20% affected by age 19 (Figure 5). The presence or absence of Conduct Disorder and ADHD was based on approximately yearly administration of the K-SADS interviews during childhood. (Because ADHD is considered a lifetime diagnosis, survival rates were not obtained for ADHD.) This greater proportion of high risk offspring with Conduct Disorder can be seen in both males and females (Figure 6).
Figure 5.
Kaplan-Meier survival curves for Conduct Disorder during childhood and adolescence for the high-risk and low-risk groups. The high-risk offspring have a significantly earlier onset than the low-risk controls (Tarone-Ware χ2 = 11.44, p = 0.001],
Figure 6.
Survival curves illustrating effect of gender and familial risk status on age of onset for Conduct Disorder. A significant relationship was seen for both males (Wald = 28.86, df =1, p =<0.001) and females (Wald = 17.74, df =1, p =<0.001) for Conduct Disorder.
Risk group differences by psychiatric diagnosis may be seen in Table 3.
Table 3.
Effect of Familial Risk Status on Odds of Developing a Child/Adolescent or Young Adult Diagnosis.
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
|---|---|---|---|---|---|---|
| Alcohol Abuse | 3.41 | 3.60 | 1 | 0.058 | 0.96 | 12.14 |
| Drug Abuse | 3.43 | 4.76 | 1 | 0.029 | 1.13 | 10.37 |
|
Alcohol Dependence |
2.62 | 2.76 | 1 | 0.097 | 0.84 | 8.14 |
|
Drug Dependence |
5.17 | 9.00 | 1 | 0.003 | 1.77 | 15.15 |
|
Drug Abuse or Dependence |
4.23 | 10.04 | 1 | 0.002 | 1.73 | 10.32 |
|
Alcohol Abuse or Dependence |
3.63 | 6.67 | 1 | 0.01 | 1.36 | 9.64 |
| ADHD | 2.24 | 4.53 | 1 | 0.033 | 1.07 | 4.71 |
| Conduct | 4.46 | 9.03 | 1 | 0.003 | 1.84 | 13.02 |
|
Anxiety Disorders |
10.46 | 10.06 | 1 | 0.002 | 2.45 | 44.64 |
|
Major Depressive Disorder |
6.11 | 11.20 | 1 | 0.001 | 2.12 | 17.63 |
Effects of Childhood Disorders on Subsequent Substance Use Disorders
Childhood ADHD and Conduct Disorder-- Effects on SUD Outcome
A series of Cox Regression analyses were performed to determine the effect of particular childhood disorders on outcome (Tables 4a, 4b, 4c). The presence of an externalizing disorder in childhood was an antecedent predictor of subsequent Alcohol Abuse or Dependence, Drug Abuse or Dependence, or presence of either (SUD) based on data collected at an average follow up interval of 5.04 ± 4.12 years. The presence of childhood ADHD significantly decreased survival time for Alcohol Abuse or Dependence, Drug Abuse or Dependence, or SUD by young adulthood. Analyses performed controlling for the gender of the offspring did not alter this relationship between ADHD and SUD (Wald = 20.30, df =1, p = <0.001) indicating that both girls and boys with ADHD were more likely to develop SUD.
Table 4.
| a. Effect of Childhood Disorder on ODDS of Developing Alcohol Abuse or Alcohol Dependence by Young Adulthood | ||||||
|---|---|---|---|---|---|---|
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
| ADHD | 7.16 | 23.15 | 1 | 0.000 | 3.21 | 15.97 |
| Conduct | 4.97 | 16.18 | 1 | 0.000 | 2.28 | 10.86 |
| Anxiety Disorders |
1.13 | 0.05 | 1 | NS | 0.39 | 3.30 |
| Major Depressive Disorder |
2.16 | 3.46 | 1 | 0.063 | 0.96 | 4.85 |
| b. Effect of Childhood Disorder on ODDS of Developing Drug Abuse or Drug Dependence by Young Adulthood | ||||||
|---|---|---|---|---|---|---|
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
| ADHD | 4.43 | 15.21 | 1 | 0.000 | 2.10 | 0.35 |
| Conduct Disorder |
8.71 | 35.59 | 1 | 0.000 | 4.28 | 17.74 |
| Anxiety Disorders |
1.35 | 0.37 | 1 | NS | 0.52 | 3.52 |
| Major Depressive Disorder |
2.42 | 5.29 | 1 | 0.021 | 1.14 | 5.14 |
| c. Effect of Childhood Disorder on ODDS of Developing Substance Use Disorder (Alcohol or Drug Abuse or Drug Dependence) by Young Adulthood | ||||||
|---|---|---|---|---|---|---|
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
| ADHD | 4.44 | 19.84 | 1 | 0.000 | 2.31 | 8.56 |
| Conduct Disorder |
8.73 | 48.06 | 1 | 0.000 | 4.73 | 16.10 |
| Anxiety Disorders |
1.66 | 1.65 | 1 | NS | 0.77 | 3.59 |
| Major Depressive Disorder |
2.58 | 8.36 | 1 | 0.004 | 1.36 | 4.90 |
Having a diagnosis of childhood Conduct Disorder resulted in an earlier onset for Alcohol Abuse or Dependence, Drug Abuse or Dependence, and increased the risk for all four conditions (Alcohol Abuse, Alcohol Dependence, Drug Abuse, Drug Dependence) or SUD (Tables 4a, 4b, 4c). Controlling for the gender of the offspring did not alter this relationship indicating that Conduct Disorder in girls as well as boys is associated with earlier development of SUD (Wald = 48.46, df =1, p =<0.001).
Childhood MDD and Anxiety Disorders -- Effects on SUD Outcome
The presence of a childhood internalizing disorder (MDD or Anxiety Disorder) on the subsequent development of SUD was evaluated with an average interval of 3.19 ± 3.69 years. As may be seen in Table 4 (a–c), the presence of an antecedent diagnosis of MDD influenced the likelihood of developing Alcohol Abuse or Alcohol Dependence with marginal statistical significance. However, a childhood diagnosis of MDD significantly influenced the risk of developing Drug Abuse or Dependence and the likelihood of developing SUD. In contrast to childhood MDD, having an Anxiety Disorder in childhood did not significantly predict Alcohol Abuse or Dependence, Drug Abuse or Dependence, or either (SUD diagnosis). However, a childhood history of either Anxiety Disorder or MDD was significantly associated with later development of Drug Abuse and Dependence (Wald = 4.39, df =1, p =0.036), and with development of SUD (Wald = 5.73, df =1, p =0.017).
Childhood ADHD, Conduct Disorder, Risk, and SUD Outcome
Models were run to test the contribution of specific childhood disorders to Substance Use Disorder outcome that also included the familial risk variable as a covariate in the model. These analyses made it possible to adjust for the potential influence of familial risk group membership on the relationship between having a specific prior childhood disorder and SUD outcome. The odds of developing SUD in association with the presence of specific childhood externalizing disorders is shown in Table 5 relative to the odds associated with high or low familial risk status without consideration of whether or not the offspring had a childhood disorder. These results demonstrate that externalizing problems of childhood and adolescence are associated with a dramatic increase in risk for SUD by young adulthood in these offspring of AD mothers. Moreover, the effects of these externalizing disorders as predictors of later SUD are substantial because they remain significant even when familial risk is entered into the Cox Regression models.
Table 5.
Effect of Childhood Externalizing Disorders on Odds of Developing a Child/Adolescent or Young Adult Diagnosis Controlling for Risk Status.
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
|---|---|---|---|---|---|---|
| Alcohol Abuse or Dependence |
||||||
| Risk* | 3.33 | 5.81 | 1 | 0.016 | 1.25 | 8.84 |
| ADHD | 6.84 | 21.20 | 1 | <0.001 | 3.02 | 15.51 |
| Risk | 2.72 | 3.84 | 1 | 0.05 | 1.00 | 7.42 |
| Conduct | 3.93 | 11.12 | 1 | 0.001 | 1.76 | 8.78 |
| Risk | 2.81 | 4.22 | 1 | 0.04 | 1.05 | 7.51 |
| ADHD and Conduct |
5.88 | 18.43 | 1 | <0.001 | 2.62 | 13.21 |
|
Drug Abuse or Dependence |
||||||
| Risk | 3.89 | 8.89 | 1 | 0.003 | 1.59 | 9.52 |
| ADHD | 4.01 | 12.96 | 1 | <0.001 | 1.88 | 8.54 |
| Risk | 2.70 | 4.43 | 1 | 0.035 | 1.07 | 6.79 |
| Conduct | 6.70 | 25.35 | 1 | <0.001 | 3.20 | 14.05 |
| Risk | 3.19 | 6.41 | 1 | 0.01 | 1.30 | 7.85 |
| ADHD and Conduct |
6.89 | 24.91 | 1 | <0.001 | 3.23 | 14.70 |
| SUD a | ||||||
| Risk | 4.67 | 13.80 | 1 | <0.001 | 2.07 | 10.54 |
| ADHD | 4.16 | 17.55 | 1 | <0.001 | 2.14 | 8.10 |
| Risk | 3.31 | 7.92 | 1 | 0.005 | 1.44 | 7.61 |
| Conduct | 6.63 | 34.25 | 1 | <0.001 | 3.52 | 12.48 |
| Risk | 3.87 | 10.54 | 1 | 0.001 | 1.71 | 8.76 |
| ADHD or Conduct |
7.49 | 36.40 | 1 | <0.001 | 3.89 | 14.40 |
Odds for familial risk are shown along with the odds for each childhood variable evaluated in the model.
SUD was defined by the presence of either Alcohol Abuse or Alcohol Dependence or Drug Abuse or Drug Dependence.
Childhood MDD, Anxiety Disorders, Risk and SUD Outcome
When analyses were run controlling for familial risk group membership, the presence of MDD in childhood/adolescence did not significantly affect survival time for Alcohol Abuse and Alcohol Dependence, Drug Abuse and Drug Dependence or all four conditions (SUD), though a trend was seen for SUD ((Wald = 2.81, df =1, p =0.09). Similarly, presence of an anxiety disorder in childhood/adolescence did not significantly influence survival time for Alcohol Abuse and Alcohol Dependence, Drug Abuse and Drug Dependence or all four conditions (SUD). Using a broader phenotype of prior Major Depressive Disorder or an Anxiety Disorder in childhood or adolescence, we also did not find an association between internalizing disorders of childhood and reduced survival time for SUD by young adulthood when familial risk status was entered into the model.
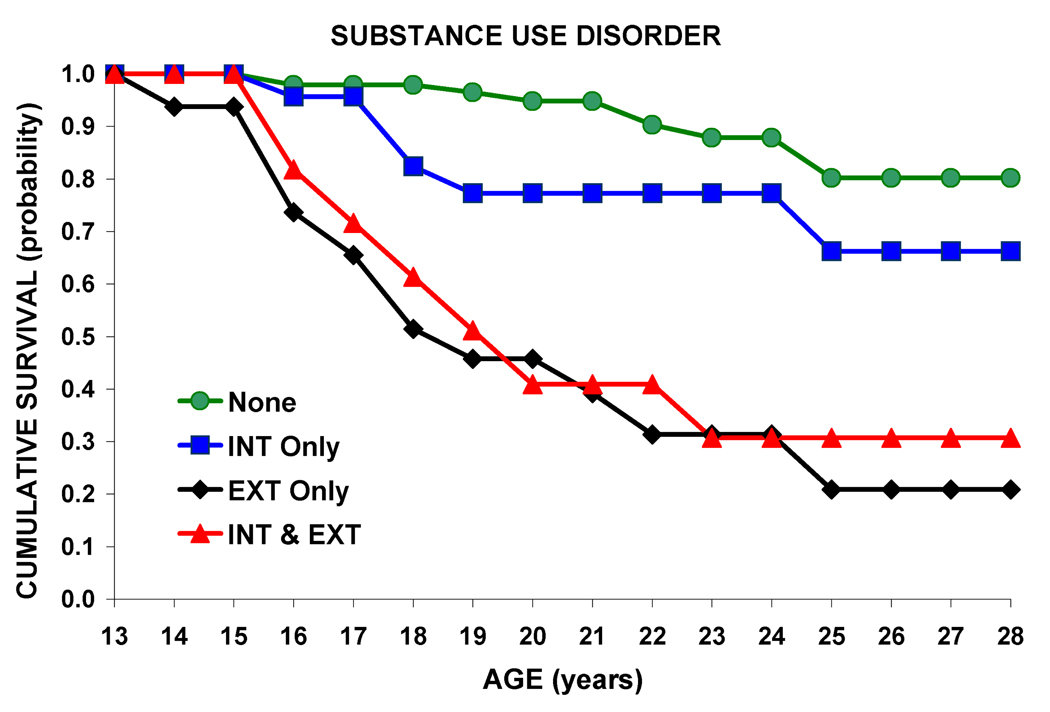
Childhood Internalizing and Externalizing Disorders and SUD Outcome
Externalizing disorders, defined by the presence of childhood ADHD or Conduct Disorder, reduced survival time significantly (Wald = 31.94 df =1, p = .000). Because it is not uncommon for individuals to have both externalizing and internalizing disorders, an analysis was completed to evaluate their separate and joint effects on SUD outcome. Presence of both internalizing and externalizing disorder together decreased the age of onset for SUD by young adulthood (Wald = 30.34 df =1, p =0 .001) as seen in Figure 7.
Figure 7.
Survival curves for Substance Use Disorder outcome in association with no childhood diagnosis, internalizing disorders only, externalizing disorders, or both internalizing or externalizing disorders. Both internalizing and externalizing disorder together decreased the age of onset for SUD by young adulthood (Wald = 30.34 df =1, p =0 .001
Gender of Offspring as a Moderating Variable
Gender did not significantly influence the age of onset of SUD among the 196 individuals, though as expected familial risk was highly significant (Wald = 15.04, df =1, p =<0.001). To illustrate, by an average of 19.5 years, 15 of the 46 males (32.6%) and 20 of the 57 female high risk offspring (35.1%) met criteria for SUD. In short, risk for Substance Use Disorders by young adulthood appears to be increased for both daughters and sons from multiplex families of maternal alcoholics.
Both female and male offspring from maternal multiplex AD families are at increased risk for Conduct Disorder with 26.1% and 15.8% diagnosed by age 19 (Figure 7). Female and male offspring from multiplex families are also at increased for ADHD with 28.3% of males and 17.5 % of females with ADHD. Because Conduct Disorder and ADHD are highly predictive of later development of SUD, it would appear that gender equality for these disorders may set the stage for the similar rates of SUD seen in male and female offspring from these maternal AD families.
To test the impact of gender on relationship between these disorders and SUD outcome, analyses were performed using ADHD and Conduct Disorder as predictors of SUD within each gender. A significant relationship was seen for both males (Wald = 28.86, df =1, p =<0.001) and females (Wald = 17.74, df =1, p =<0.001) for Conduct Disorder. The odds ratio for developing SUD in association with a prior diagnosis of Conduct disorder in males was 15.2 (95% CI: 5.6, 41) and for females 6.05 (95% CI: 2.6, 13.9). For ADHD, a significant effect was seen for males (Wald = 6.23, df =1, p =0.013) and for females (Wald = 15.81, df =1, p =<0.001). The odds ratio for developing SUD in association with a prior diagnosis of ADHD for males was 3.69 (95% CI: 1.3, 10.3) and was greater for females 5.80 (95% CI: 2.4, 13.8).
Early Young Adulthood
Although the young adult follow up is not completed, it was instructive to determine the rates of illness among a group of 118 offspring who had their most recent follow up visit some time between the ages of 18–22 years. Obtaining estimates of diagnostic prevalence for those currently transitioning from adolescence to young adulthood is of considerable interest because it often represents a time when youngsters leave the parental home for college or to live on their own away from parental supervision. Using this strategy we find that high risk offspring have significantly elevated rates of Alcohol Abuse/ Alcohol Dependence, Drug Abuse/Drug Dependence, Anxiety Disorders and MDD in comparison to low risk offspring (Table 6).
Table 6.
Diagnosis in Early Young Adulthood (Ages 18–22) – Effect of Familial Risk Status
| High- Risk |
% | Low- Risk |
% | Chi Square | df | p value | |
|---|---|---|---|---|---|---|---|
|
Drug Abuse or Dependence |
17 | 29.8% | 5 | 8.2% | 9.09 | 1 | 0.002 |
|
Alcohol Abuse or Dependence |
10 | 8.5% | 3 | 2.5% | 4.79 | 1 | 0.028 |
|
Anxiety Disorders |
14 | 24.6% | 1 | 1.6% | 13.95 | 1 | 0.000 |
|
Major Depressive Disorder |
19 | 33.3% | 4 | 6.6% | 13.46 | 1 | 0.000 |
Effects of Childhood Disorders on Outcome within the High Risk Group
Because of the significant colinearity between being a member of a high risk family and having one or more psychiatric disorders of childhood and/or adolescence, it was interest to determine if the predictors identified within the entire sample would also predict SUD outcome within the high risk group. This analysis showed that Conduct Disorder and ADHD were highly significant predictors of later development of SUD, but the presence of MDD or Anxiety Disorders were not (Table 7). The effects of these child/adolescent predictors appear to be similar within the high risk sample and in the larger full sample of high and low risk individuals, but with one exception. MDD had been a significant predictor of outcome in the full sample (Table 4 a, b, c) but was not a significant predictor within the sample of high risk offspring from these multiplex families selected through a female proband.
Table 7.
| a. Effect of Childhood Disorder on ODDS of Developing Alcohol Abuse or Alcohol Dependence by Young Adulthood – High Risk Only | ||||||
|---|---|---|---|---|---|---|
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
| ADHD | 9.05 | 20.65 | 1 | 0.000 | 3.50 | 23.40 |
| Conduct | 4.03 | 9.89 | 1 | 0.002 | 1.69 | 9.60 |
| Conduct or ADHD |
||||||
| MDD or Anxiety Disordersa |
1.13 | 0.08 | 1 | NS | 0.46 | 2.70 |
| b. Effect of Childhood Disorder on ODDS of Developing Drug Abuse or Drug Dependence by Young Adulthood – High Risk Only | ||||||
|---|---|---|---|---|---|---|
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
| ADHD | 4.52 | 12.53 | 1 | 0.000 | 1.96 | 10.42 |
| Conduct Disorder |
6.15 | 19.21 | 1 | 0.000 | 2.73 | 13.85 |
| Conduct or ADHD |
7.12 | 19.22 | 1 | 0.000 | 2.96 | 17.12 |
| MDD or Anxiety Disordersa |
1.28 | 0.52 | 1 | NS | 0.65 | 2.51 |
| C. Effect of Childhood Disorder on ODDS of Developing Substance Use Disorder (Alcohol or Drug Abuse or Drug Dependence) by Young Adulthood – High Risk Only | ||||||
|---|---|---|---|---|---|---|
| Odds Ratio |
Wald | df | p value | Confidence Interval |
||
| ADHD | 4.86 | 18.06 | 1 | 0.000 | 2.34 | 10.08 |
| Conduct Disorder |
6.55 | 28.60 | 1 | 0.000 | 3.29 | 13.03 |
| Conduct or ADHD |
8.67 | 31.60 | 1 | 0.000 | 4.08 | 18.42 |
| MDD or Anxiety Disordersa |
1.28 | 0.52 | 1 | NS | 0.65 | 2.51 |
MDD or Anxiety Disorders alone did not significantly predict outcome in the high risk group.
Discussion
This is one of a few studies that have prospectively assessed the onset of internalizing and externalizing disorders as well as Substance Use Disorders from childhood/adolescence into young adulthood. This follow up is unique in having followed offspring from multiplex AD families identified through a pair of female alcohol dependent individuals. As such, this is the first report documenting the temporal order of psychopathology in offspring from families with a high density of maternal AD. The present findings indicate that offspring from high-risk families with maternal AD (mother and/or multiple maternal relatives are alcoholic) have a significantly earlier age of onset of a variety of psychiatric conditions compared to offspring from control families.
This report adds to the existing literature by providing prospective evidence for elevated risk for developing internalizing disorders including mood-related disorders among young adult offspring of AD individuals (Earls and Powell, 1988; Hill and Muka 1996; Reich et al., 1993, Hill et al., 2008). A 6-fold increase in the odds for developing MDD was seen among those with a history of maternal familial AD. Previously, Dawson and Grant, (1998) reported that among adults over the age of 18, the odds for developing MDD increases with the percentage of first degree relatives with alcohol dependence. For women with 50% of relatives affected, the odds ratio (OR) was reported to be 4.77 [CI 4.06–5.61].
Although the high risk offspring showed an increased OR for developing an Anxiety Disorder in childhood (10.46), the presence of Anxiety Disorders in childhood did not predict later development of substance use disorder diagnoses. This is in contrast to findings of (Hofmann et al 2009) reporting on findings from the National Comorbidity Survey in which anxiety disorders were associated with increased odds for development of substance use disorders. The present results may differ from the Hoffman et al (2009) study because the present study utilized individuals selected for a high degree of familial loading for AD. Because familial risk is such an important predictor of young adult outcome, the effect of Anxiety Disorders of childhood may not have been manifest. While presence of Anxiety Disorders of childhood did not increase the odds for developing a substance use disorder by young adulthood in the present study, presence of MDD did elevate the OR over two-fold. Other studies have reported that depression during adolescence is concurrently associated with increased substance use (Needham, 2007) and longitudinally predicts increased use in young adulthood (Crum et al 2008; Marmorstein 2009a).
The present results find a two-fold increase in risk for ADHD associated with being the offspring from a mutliplex AD family. Our results are consistent with other prospective longitudinal studies that find ADHD often precedes young adult SUD (Mannuzza et al., 1993; Elkins et al 2007; Biederman et al., 2008). Importantly, the presence of ADHD is associated with an increased likelihood of subsequent development of SUD (OR= 4.44). The present report also finds that ADHD is a significant predictor of SUD even among the all female offspring sample. Our finding is in accord with a previous report showing an odds ratio of 4.0 at 5 year follow up for girls with ADHD and later development of substance dependence (Beiderman et al 2006). Also, ADHD is a significant prospective predictor of SUD even after taking into account a diagnosis of Conduct Disorder (Elkins et al 2007).
The present analyses show that the presence of childhood Conduct Disorder increases the risk for young adult SUD in offspring of female alcoholics, a relationship previously reported for offspring of male alcoholics (Schuckit et al (2008). Similarly, presence of ADHD in childhood increased the likelihood of having a SUD diagnosis by young adulthood. Whether the presence of externalizing disorders of childhood and adolescence sets the stage for later development of SUD through increased exposure to peers with similar problems and predilection for substance use is unknown. It is also possible that externalizing disorders of childhood are one pleiotropic manifestation of a genetic predisposition to SUD that is expressed in an alternate manner in childhood and adolescence. In comparison to other childhood behavioral disorders, Conduct Disorder is one of the most powerful predictors of SUD (Ohannessian et al., 1995) and has been reported to be a better predictor of SUD outcome than having a family history of psychopathology, having divorced parents, or family income (Schuckit et al 2008). Two studies have reported that presence of either Oppositional Defiant Disorder or Conduct Disorder in childhood increased the likelihood of developing a SUD in young adulthood though these studies did not assess the possible conjoint effects of familial risk for AD or other SUD (Nock et al., 2006, 2007). The present results based on offspring from maternal alcohol dependent families finds ADHD and Conduct Disorder in childhood significantly decreased survival time for SUD.
The present results demonstrated that offspring from multiplex families selected through an AD woman, have a 4–5 five fold odds of developing SUD by young adulthood. This compares with odds of 2–3 fold seen in community based samples where offspring of alcohol and drug dependent parents have been investigated (Marmorstein et al 2009b). Importantly, both male and female offspring from multiplex maternal AD families were equally as likely to meet criteria for SUD by adulthood (32.6 % and 35.1%, for males and females, respectively). This compares with DSM-IIIR reported rates of 35.4% and 17.9% for males and females in the National Comorbidity Survey (Kessler et al 1994). Both male and female high risk offspring frequently met DSM-III criteria for Conduct Disorder (26.1 and 15.8% in males and females, respectively). This compares to 12% for males and 7% for females reported in national surveys (Nock et al 2006). The increased risk for Conduct Disorder seen among high risk offspring in this study may set the stage for increased risk for developing SUD along with other psychiatric disorders of adulthood. Using a large community sample, Robins and Price (1991) showed that Conduct Disorder increased the prevalence of 10 adult disorders spanning both internalizing and externalizing disorders. It is especially interesting to note that the presence of Conduct Disorder in childhood increased the risk for future SUD even in our sample of very high risk families (multiplex for AD).
A previous report found sons of male alcoholics to be at increased risk for exhibiting conduct symptoms in comparison to female offspring (Schuckit et al., 2008). The present observation of nearly equivalent rates of Conduct Disorder in boys and girls may be the result of the ascertainment strategy used to select these maternal high risk families. Families selected through the presence of two alcohol dependent sisters are at an especially high risk for developing alcohol dependence. Also, it has often been noted that threshold for alcohol dependence may differ by gender because societal pressures reduce the likelihood that women will engage in heavy drinking (Hill, 2000). Those who exceed that threshold may be more extreme than are males who become heavy drinkers. Also, higher prevalence ratios of ASPD are seen in female than male alcoholics (Helzer et al., 1991). Therefore, both male and female offspring in this study may have exhibited Conduct Disorder as a result of an increased liability for adult ASPD in their mothers, a condition that is often preceded by adolescent conduct problems.
In addition to varying rates of disorder by gender of the offspring, the gender of the parent appears to be an important consideration. A meta-analysis (Prescott, 2001) addressing sex differences in alcoholism transmission reported a 40% increase in risk for alcoholism among relatives of female alcoholics in comparison to male alcoholics. Additionally, several studies utilizing population-based samples have examined the influence of parental gender. Utilizing a sample of 1,030 same-sex twins from the Virginia Twin registry and their parents, Kendler et al. (1994) reported that alcoholism was transmitted to daughters equally as often from alcoholic mothers (n=33) as alcoholic fathers (N=82). Similarly, Lieb et al. (2002) using a representative sample of German 14–17 year olds and adjusting for the number of parents who were alcohol dependent (one or both) reported that progression to hazardous level of drinking over a four year follow up was equally likely in offspring of affected mothers as fathers. One limitation of the Lieb et al (2002) study was the relative infrequent occurrence of alcohol dependence in mothers (7.5%). In another population-based sample 1,514 adolescent twins were identified through Minnesota birth records and evaluated at ages 11, 14, and 17 for substance use. Having either a mother or father with a substance use disorder was reported to accelerate substance use involvement in their offspring (Walden et al., 2007). Similarly, Slutske et al. (2008) studying 1,224 male and female offspring of twins in Australia reported that having either a father or mother with alcohol dependence increased the odds (OR = 2.7, 95% CI: 1.2, 6.2) that offspring would have a history of AD. Because the sample was population-based, only 18% of the offspring had parental AD, however. One strength of the present study was that, by study design, a reasonably high proportion of the offspring were children of female alcohol dependent cases.
One limitation of the present analyses includes the varying definitions of the Substance Use Disorders for those diagnosed in childhood and adolescence (DSM-III) and those receiving a DSM-IV diagnosis from the age-appropriate CIDI interview that was administered for those seen after age 19. Another limitation was that some predictors and outcomes both occurred in close proximity during childhood and adolescence during the 8–18 year old portion of the study while for others the childhood predictor (Conduct Disorder or ADHD) occurred several years before the young adult SUD outcome This would tend to introduce variation in the predictor/outcome relationship because conditions more proximal might be expected to have greater influence than those separated in time. This may be of more limited concern because there is good reason to believe Conduct Disorder and ADHD are persistent disorders that once diagnosed rarely remit.
Another limitation was the varying methods used to assess mothers and fathers. The diagnostic status of the mothers was determined using direct interviews to obtain DSM diagnoses and obtain family history information concerning her parents and siblings. While biological fathers were interviewed in person and similar information obtained where possible, often family history information was obtained from mothers concerning the biological father and his family. Because diagnostic status was more often determined through family history for the biological fathers of these offspring, the influence of genetic loading for psychiatric problems and their possible influence on the offspring could not be directly evaluated as it was for mothers. Additionally, these alcohol dependent women from multiplex AD families demonstrate a significant amount of nonrandom mating with similarly affected SUD men. As a result, the offspring of these alcohol dependent women were more likely to have both parents affected.
Another potential limitation is the representativeness of the sample. Selection of families through a proband pair of alcohol dependent women, one of whom was in treatment at the time of identification, by study design, results in a sample that may not be representative of families of alcohol dependent individuals in the general population. However, the strength of this approach is that a significant number of offspring have the outcome variable of interest to relate to child/adolescent precursors. Population-based samples provide the distinct advantage of drawing on large and often representative samples. However, the base rate of alcohol dependence and other substance use disorders especially among mothers is often reported to be quite low limiting the number of variables that can be assessed at one time.
A further limitation of the study is the myriad of factors associated with familial risk status. Familial risk encompasses not only the overall genetic susceptibility for AD and other SUD, but also can include correlated endophenotypes of risk such as cognitive alteration as indexed by P300 amplitude (Hill et al 2009b) that appear to alter this vulnerability. Additionally, offspring with multiplex familial AD risk often grow up in a family where the nuclear and extended family is affected with Substance Use Disorders. Importantly, alcohol and drug dependent mothers often fail to stop their use of substances during pregnancy so that these effects may contribute to increase risk for offspring psychopathology. Although analysis of these exposures is beyond the scope of the present report, separate genetic and exposure conditions appear to contribute to childhood disorders (Hill et al 2000b). Although it difficult to distinguish between genetically mediated factors and those as a result of familial environmental effects in family-based studies, the observations presented here suggest that intergeneration transmission of psychopathology through the maternal line places offspring at very high risk for experiencing psychopathology. This is underscored by the high rate of Drug Abuse and Drug Dependence and MDD seen in early young adulthood. Because the follow up is ongoing, not all offspring have been followed during young adulthood and so the complete picture of this relationship is not currently known.
In spite of these limitations, it should be pointed out that this is the first prospective study to evaluate the same multiplex offspring multiple times during childhood as well as several times in young adulthood in relating survival to familial risk. This extensive follow-up has provided prospectively collected data for improved estimation of the onset of specific psychiatric disorders that precede the onset of Substance Use Disorders. Future research is needed to evaluate whether early intervention programs focused on decreasing childhood externalizing and internalizing symptoms reduce the likelihood of substance use disorders in adulthood.
The present results suggest that prevention efforts designed to interrupt the intergenerational transmission of substance use disorders in families of female alcohol dependent individuals may require new approaches. Women with substance use disorders who become mothers more often have partners similarly affected. If the partner is the biological father of the child, the expectation would be that genetic risk factors for externalizing disorders would be elevated in offspring where both parents are affected. The biological father can also provide a negative environment through his continued use of substances. Even If the partner with whom the child lives is not the biological father there is increased environmental pressure for engaging in substance use possibly as result of modeling behavior or just increased availability. Previous work (Hill and Muka, 1996) has suggested that presence of a SUD male “custodial” parent appears to elevate the risk for offspring childhood disorders. The present findings suggest that offspring of mothers with AD are at especially high risk of developing childhood disorders and young adult substance use disorders. The challenge is in finding ways to decrease the intergenerational transmission.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Biederman J, Petty CR, Dolan C, Hughes S, Mick E, Monuteaux MC, Faraone SV. The long-term longitudinal course of oppositional defiant disorder and conduct disorder in ADHD boys: findings from a controlled 10-year prospective longitudinal follow-up study. Psychol Med. 2008;38:1027–1036. doi: 10.1017/S0033291707002668. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Klein KL, Price JE, Faraone SV. Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled. five-year prospective study. Biological Psychiatry. 2006;60:1098–1105. doi: 10.1016/j.biopsych.2006.02.031. [DOI] [PubMed] [Google Scholar]
- Bohman M. Some genetic aspects of alcoholism and criminality. A population of adoptees. Arch Gen Psychiatry. 1978;35:269–276. doi: 10.1001/archpsyc.1978.01770270019001. [DOI] [PubMed] [Google Scholar]
- Chambers W, Puig-Antich J, Hirsch M, Paez P, Ambrosini P, Tabrizi MA, et al. The assessment of affective disorders in children and adolescents by semistructured interview: test–retest reliability of the schedule for affective disorders and schizophrenia for school-age children, present episode version. Arch Gen Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. (1985) [DOI] [PubMed] [Google Scholar]
- Cloninger CR, Bohman M, Sigvardsson S. Inheritance of alcohol abuse. Cross-fostering analysis of adopted men. Arch Gen Psychiatry. 1981;38:861–868. doi: 10.1001/archpsyc.1981.01780330019001. [DOI] [PubMed] [Google Scholar]
- Cottler LB, Robins LN, Helzer JE. The reliability of the CIDI-SAM: a comprehensive substance abuse interview. British Journal of Addiction. 1989;84:801–814. doi: 10.1111/j.1360-0443.1989.tb03060.x. [DOI] [PubMed] [Google Scholar]
- Cox DR, Oakes D. Analysis of Survival Data. London: Chapman and Hall; 1984. [Google Scholar]
- Crum RM, Green KM, Storr CL, Chan YF, Ialongo N, Stuart EA, Anthony JC. Depressed mood in childhood and subsequent alcohol use through adolescence and young adulthood. Arch Gen Psychiatry. 2008;65:702–712. doi: 10.1001/archpsyc.65.6.702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Li TK. Impact of age at first drink on stress-reactive drinking. Alcohol Clin Exp Res. 2007;31:69–77. doi: 10.1111/j.1530-0277.2006.00265.x. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF. Family history of alcoholism and gender: Their combined effects on DSM-IV alcohol dependence and major depression. J Stud Alc. 1998:97–106. doi: 10.15288/jsa.1998.59.97. [DOI] [PubMed] [Google Scholar]
- Dick DM, Bierut L, Hinrichs A, Fox L, Bucholz KK, Kramer J, Kuperman S, Hesselbrock V, Schuckit M, Almasy L, Tischfield J, Porjesz B, Begleiter H, Nurnberger J, Jr, Xuei X, Edenberg HJ, Foroud T. The role of GABRA2 in risk for conduct disorder and alcohol and drug dependence across developmental stages. Behav Genet. 2006;36:577–590. doi: 10.1007/s10519-005-9041-8. [DOI] [PubMed] [Google Scholar]
- Earls F, Powell J. Patterns of substance use and abuse in inner-city adolescent medical patients. Yale J Biol Med. 1988;61:233–242. (1988) [PMC free article] [PubMed] [Google Scholar]
- Earls F, Reich W, Jung KG, Cloninger CR. Psychopathology in children of alcoholic and antisocial parents. Alcohol Clin Exp Res. 1988;12:481–487. doi: 10.1111/j.1530-0277.1988.tb00230.x. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64:1145–1152. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Feighner JP, Robins E, Guze SB, Woodruff RA, Jr, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Arch Gen Psychiatry. 1972;26:57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- Ghodsian M, Power C. Alcohol consumption between the ages of 16 and 23 in Britain: A longitudinal study. Br J Addiction. 1987;82:175–180. doi: 10.1111/j.1360-0443.1987.tb01457.x. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Dawson DA, Saha TD, Ruan WJ, Compton WM, Grant BF. Antisocial behavioral sydromes and DSM-IV alcohol use disorders: Results from the National Epdiemiolgic survey on alcohol and related Conditions. Alcoholism: Clinical and Experimental Research. 2007;31:814–828. doi: 10.1111/j.1530-0277.2007.00364.x. [DOI] [PubMed] [Google Scholar]
- Goodwin DW, Schulsinger F, Hermansen L, Guze SB, Winokur G. Alcohol problems in adoptees raised apart from alcoholic biological parents. Arch Gen Psychiatry. 1973;28:238–243. doi: 10.1001/archpsyc.1973.01750320068011. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. J Subst Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Helzer J, Burnam A, McEvoy LT. Alcohol Abuse and Dependence. In: Robins LN, Regier DA, editors. Psychiatric Disorders in America. New York, New York: Free Press; 1991. pp. 81–115. [Google Scholar]
- Hill SY. Goldman MB, Hatch MC. Women and Health. New York: Academic Press; 2000. Addictive Disorders; pp. 1042–1053. [Google Scholar]
- Hill SY, Lowers L, Locke-Wellman Shen S. Maternal smoking and drinking during pregnancy and the risk for child and adolescent psychiatric disorders. J Stud Alc. 2000b;61:661–668. doi: 10.15288/jsa.2000.61.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill SY, Locke J, Lowers L, Connolly J. Psychopathology and achievement in children at high risk for developing alcoholism. J Am Acad Child Adolesc Psychiatry. 1999;38:883–891. doi: 10.1097/00004583-199907000-00019. [DOI] [PubMed] [Google Scholar]
- Hill SY, Muka D. Childhood psychopathology in children from families of alcoholic female probands. J Am Acad Child Adolesc Psychiatry. 1996;35:725–733. doi: 10.1097/00004583-199606000-00012. [DOI] [PubMed] [Google Scholar]
- Hill SY, Shen S, Lowers L, Locke J. Factors predicting the onset of adolescent drinking in families at high risk for developing alcoholism. Biol Psychiatry. 2000;48:265–275. doi: 10.1016/s0006-3223(00)00841-6. [DOI] [PubMed] [Google Scholar]
- Hill SY, Shen S, Lowers L, Locke-Wellman J, Matthews AG, McDermott M. Psychopathology in offspring from multiplex alcohol dependence families with and without parental alcohol dependence: a prospective study during childhood and adolescence. Psychiatry Res. 2008;160:155–166. doi: 10.1016/j.psychres.2008.04.017. (2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill SY, Shen S, Zezza N, Hoffman EK, Perlin M, Allan W. A genome-wide search for alcoholism susceptibility genes. Am J Med Genet Part B (Neuropsychiatr Genet) 2004;128B:102–113. doi: 10.1002/ajmg.b.30013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill SY, Wang S, Kostelnik B, Carter H, Holmes B, McDermott M, Zezza N, Stiffler S, Keshavan MS. Disruption of orbitofrontal cortex laterality in offspring from multiplex alcohol dependence families. Biological Psychiatry. 2009a;65:129–136. doi: 10.1016/j.biopsych.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill SY, Steinhauer SR, Locke-Wellman J, Ulrich R. Childhood risk factors for young adult substance dependence outcome in offspring from multiplex alcohol dependence families. Biological Psychiatry. 2009b;66:750–757. doi: 10.1016/j.biopsych.2009.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Richey JA, Kashdan TB, McKnight PE. Anxiety disorders moderate the association between externalizing problems and substance use disorders: Data from the National Comorbidity Survey-Revised. Journal of Anxiety Disorders. 23:529–534. doi: 10.1016/j.janxdis.2008.10.011. [DOI] [PubMed] [Google Scholar]
- Janca A, Robins LN, Cottler LB, Early TS. Clinical observation of assessment using the Composite International Diagnostic Interview (CIDI). An analysis of the CIDI field trials B wave II at the St. Louis site. Br J Psychiatry. 1992;160:815–818. doi: 10.1192/bjp.160.6.815. [DOI] [PubMed] [Google Scholar]
- Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53 457-48. [Google Scholar]
- Kendler KS, Neale MC, Heath AC, Kessler RC, Eaves LJ. A twin-family study of alcoholism in women. Am J Psychiatry. 1994;151:707–715. doi: 10.1176/ajp.151.5.707. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Schmitt E, Aggen SH, Prescott CA. Genetic and environmental influences on alcohol, caffeine, cannabis, and nicotine use from early adolescence to middle adulthood. Arch Gen Psychiatry. 2008;65:674–682. doi: 10.1001/archpsyc.65.6.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the the United States. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kuperman S, Schlosser SS, Lidral J, Reich W. Relationship of child psychopathology to parental alcoholism and antisocial personality disorder. J Am Acad Child Adolesc Psychiatry. 1999;38:686–692. doi: 10.1097/00004583-199906000-00015. [DOI] [PubMed] [Google Scholar]
- Kuperman S, Chan G, Kramer JR, Bierut L, Bucholz KK, Fox L, Hesselbrock V, Nurnberger JI, Jr, Reich T, Schuckit MA. Relationship of age of first drink to child behavioral problems and family psychopathology. Alcohol Clin Exp Res. 2005;29:1869–1876. doi: 10.1097/01.alc.0000183190.32692.c7. [DOI] [PubMed] [Google Scholar]
- Lieb R, Merikangas KR, Hofler M, Pfister H, Isensee H, Wittchen HU. Parental alcohol use disorders and alcohol use and disorders in offspring: a community study. Psycholog Med. 2002;32:63–78. doi: 10.1017/s0033291701004883. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993;50:565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR. Longitudinal association between alcohol problems and depressive symptoms: Early adolescence through early adulthood. Alcoholism: Clinical and Experimental Research. 2009a;33 doi: 10.1111/j.1530-0277.2008.00810.x. 499-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, McGue M. Alcohol and illicit drug dependence among parents: associations with offspring externalizing disorders. Psychological Medicine. 2009b;39:149–155. doi: 10.1017/S0033291708003085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGue M, Iacono WG, Legrand LN, Malone S, Elkins I. Origins and consequences of age at first drink. I. Associations with substance-use disorders, disinhibitory behavior and psychopathology, and P3 amblitude. Alcoholism: Clinical and Experimental Research. 2001;8:1156–1165. [PubMed] [Google Scholar]
- Merikangas KR, Avenevoli S. Implications of genetic epidemiology for the prevention of substance use disorders. Addictive Behavior. 2000;25:807–820. doi: 10.1016/s0306-4603(00)00129-5. [DOI] [PubMed] [Google Scholar]
- Needham BL. Gender differences in trajectories of depressive symptomatology and substance use during the transition from adolescence to young adulthood. Social Science and Medicine. 2007;65:1166–1179. doi: 10.1016/j.socscimed.2007.04.037. [DOI] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol Med. 2006;36:699–710. doi: 10.1017/S0033291706007082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: results from the National Comorbidity Survey Replication. J Child Psychol Psychiatry. 2007;48:703–713. doi: 10.1111/j.1469-7610.2007.01733.x. (2007) [DOI] [PubMed] [Google Scholar]
- Ohannessian CM, Stabenau JR, Hesselbrock VM. Childhood and adulthood temperament and problem behaviors and adulthood substance use. Addict Behav. 1995;20:77–86. doi: 10.1016/0306-4603(94)00047-3. (1995) [DOI] [PubMed] [Google Scholar]
- Ohannessian CM, Hesselbrock VM, Kramer J, Kuperman S, Bucholz KK, Schuckit MA, Nurnberger JI. The relationship between parental alcoholism and adolescent psychopathology: a systematic examination of parental comorbid psychopathology. J Abnorm Psychol. 2004;32:519–533. doi: 10.1023/b:jacp.0000037781.49155.a6. (2004) [DOI] [PubMed] [Google Scholar]
- Parmar MKB, Machin D. Survival Analysis. West Sussex, England: John Wiley and Sons, Ltd; 1995. [Google Scholar]
- Prescott CA. The genetic epidemiology of alcoholism: Sex differences and future directions. In: Agarwal DP, Seitz HK, editors. Alcohol in Health and Disease. New York: Marcel Dekker; 2001. pp. 125–149. [Google Scholar]
- Reich W, Earls F, Frankel O, Shayka JJ. Psychopathology in children of alcoholics. J Am Acad Child Adolesc Psychiatry. 1993;32:995–1002. doi: 10.1097/00004583-199309000-00017. [DOI] [PubMed] [Google Scholar]
- Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38:381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- Robins LN, Price RK. Adult diosrders predicted by childhood conduct problems: results from the NIMH Epidemiologic Catchment Area project. Psychiatry. 1991;54:116–132. doi: 10.1080/00332747.1991.11024540. [DOI] [PubMed] [Google Scholar]
- Robins LN, Przybeck TR. Age of onset of drug use as a factor in drug and other disorders. In: Jones CL, Battles RJ, Washington DC, editors. Etiology of Drug Abuse: Implications for Prevention. US Government Printing Office; 1985. pp. 178–192. (NIDA Research Monograph No 56, DHHS Publication No ADM 85-1335) [Google Scholar]
- Schuckit MA, Smith TL, Radziminski S, Heyneman EK. Behavioral symptoms and psychiatric diagnoses among 162 children in in nonalcoholic or alcoholic families. American Journal of Psychiatry. 2000;157:1881–1883. doi: 10.1176/appi.ajp.157.11.1881. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL, Pierson J, Trim R, Danko GP. Externalizing disorders in the offspring from the San Diego prospective study of alcoholism. J Psychiatr Res. 2008;42:644–652. doi: 10.1016/j.jpsychires.2007.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS, D'Onofrio BM, Turkheimer E, Emery RE, Harden KP, Heath AC, Martin NG. Searching for an environmental effect of parental alcoholism on offspring alcohol use disorder: a genetically informed study of children of alcoholics. J Abnorm Psychol. 2008;117:534–551. doi: 10.1037/a0012907. (2008) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walden B, Iacono WG, McGue M. Trajectories of change in adolescent substance use and symptomatology: impact of paternal and maternal substance use disorders. Psychol Addict Behav. 2007;21:35–43. doi: 10.1037/0893-164X.21.1.35. [DOI] [PubMed] [Google Scholar]