Abstract
Stent assisted coiling on intracranial broad neck aneurysm has been considered as an effective technique and has made the complex aneurysms amenable to coiling. However, stent navigation and application themselves often have the problems especially when the parent vessel angle (entrance between afferent and efferent vessel) is over 90 degrees. We report here a case of a ruptured broad neck basilar top aneurysm that was successfully coiled using two self-expandable stents (Enterprise and Neuroform) placed in a fashion of modified Y-configured stents with waffle cone technique.
Keywords: Subarachnoid hemorrhage, Complex aneurysm, Modified Y-configured stent
INTRODUCTION
Treatment of intracranial aneurysm with detachable coils is associated with lower morbidity and mortality rate compared with traditional microsurgical clipping7,8). However, endovascular aneurysm coiling still has limitations especially on the treatment of broad neck aneurysm because of the distal flow obliteration by the coil herniation into the parent vessel. Many devices and techniques have been introduced to overcome these limitations including three-dimensional (3D) coils, techniques using multiple catheters, and balloon remodeling technique, etc.6,9,13).
The introduction of stent-assisted coiling method in this situation has added an attractive therapeutic approach. In selected cases, stent-assisted coiling offers an advantage over traditional coiling and balloon remodeling technique. The stent can not only prevent coil herniation but provide as a matrix of durable membrane formation in the lumen of aneurysm neck. The stent is typically placed within the afferent to efferent vessel's lumen before coiling. However, some broad neck aneurysms, such as the ones located at bifurcation, are not amenable to treatment with a single stent. There is limited information on the use and efficacy of stent treatment of such aneurysms. In case of the bifurcation broad neck aneurysm, Y-configuration using two stents often is necessary to cover the full lumen of the aneurysm neck for preserving the patency of the parent vessel.
We present a case where stent-assisted coiling with a 'modified Y-configured stents with waffle cone technique' that was utilized for the management of ruptured broad neck basilar top aneurysm of acute angle between afferent and efferent parent artery (over 90 degrees).
CASE REPORT
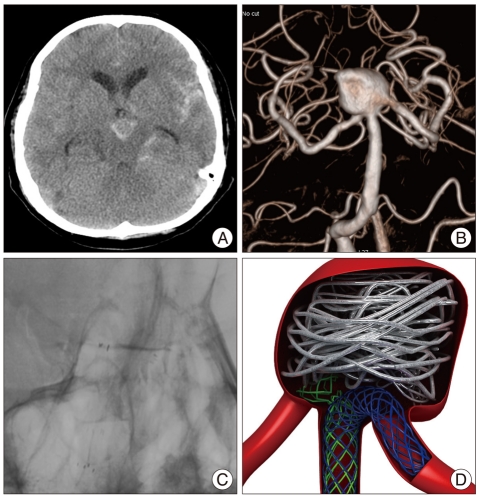
A 68-year-old woman with subarachnoid hemorrhage in Hunt and Hess Grade II was admitted the initial brain computed tomography (CT) scan revealed thick subarachnoid blood around basal and prepontine cistern (Fig. 1A). 3D-CT angiography and catheter based cerebral angiography showed a large aneurysm on the top of the basilar artery (Fig. 1B). Because of the large neck size and intolerable dome and neck ratio, the authors decided to place a stent before coiling. Pre-treatment with antiplatelet agent was not done. The procedure was performed under intravenous sedation using propofol and alfentanyl. A 6Fr guide catheter was placed within the right vertebral artery. During the procedure an activated clotting time was maintained between 250 and 300 seconds. First, 4.5 mm×28 mm Enterprise stent (Cordis Neurovascular, Miami, FL, USA) was placed from the left posterior cerebral artery to the basilar artery. We tried to deploy second stent of 4.5 mm×20 mm Neuroform stent (Boston Scientific/Target, Fremont, CA, USA) from right posterior cerebral artery to basilar artery, but it was found to be very difficult to navigate to the proper position through a cell of the Enterprise previously placed by the acute angle between the right P1 and the basilar artery. Therefore, we decided the second stent used as a waffle cone stent and the distal stent markers placed on the proximal portion of the aneurysm to make the right P1 preservation during the coiling (Fig. 1C). Ultimately, we planned a vascular remodeling by modified Y-configured stents with waffle cone technique (Fig. 1D).
Fig. 1.
A : Initial brain computed tomography showing spontaneous subarachnoid hemorrhage in basal and prepontine cistern. B : 3D angiogram shows a broad neck basilar top aneurysm involving both P1 segments and basilar artery. C : Unsubstraction image showing 4.5 mm×28 mm Enterprise stent placed in the distal basilar artery and proximal left PCA and 4.5 mm×20 mm Neuroform stent is deployed into aneurysm sac. D : 3D computer illustration graph shows a Enterprise stent placed in the distal basilar artery and proximal left PCA and Neuroform stent is located into aneurysm neck.
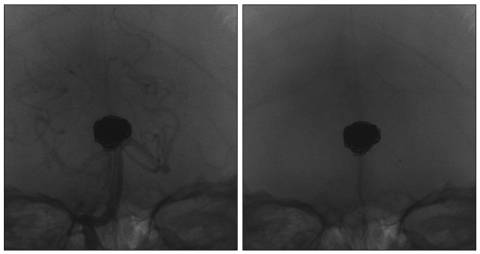
After stent deployment, coiling was performed safely with a microcatheter (Excelsior SL-10; Boston Scientific, Fremont, CA, USA) placed in the aneurysm through the cell and the stem of the stents. Near complete occlusion of the aneurysm was made (Fig. 2). After the procedure, the patient received clopidogrel (75 mg daily) and aspirin (100 mg daily) for 4 weeks, after then only aspirin monotherapy has been continued. The femoral puncture site was closed by a closure device and heparin was not reversed at the end of the procedure.
Fig. 2.
Immediate postembolization angiogram and fluoroscopic image showing the complete embolization under 4.5 mm×28 mm Enterprise stent placed in the distal basilar artery and proximal left PCA and 4.5 mm×20 mm Neuroform stent is deployed into aneurysm sac.
An unsubtracted image showed the stent and in place. The patient was discharged from the hospital 14 days after admission without any neurological deficits.
DISCUSSION
The successful treatment of an intracranial aneurysm require an isolation of the aneurysm from the parent vessel. However, endovascular coiling on the broad neck aneurysms has always been very difficult to treat because of the risk of coil protrusion in the parent vessel and subsequent thrombus formation and the distal flow obliteration. Several techniques and endovascular devices have been developed for the treatment of broad neck aneurysms, such as a balloon-assisted neck remodeling, 3D coils, and multiple catheter technique, etc.6,9,13).
Currently, the development of a flexible and self-expandable intracranial stents (Neuroform, Enterprise) has increased the options for the treatment of complex aneurysms. The efficacy and safety of intracranial stents for endovascular treatment of broad neck intracranial aneurysms have been evaluated in several studies. In associated with coiling, the development of a stent within the parent vessel has some advantages : it enables dense packing in aneurysm; it induces significant intra-aneurysmal flow modification that may lead to spontaneous thrombosis, and it may provide a framework for endothelial growth resulting in permanent separation of the aneurysm from parent vessel lumen2).
In stent assisted coiling, most authors report that the premedication of antiplatelet drugs have been strongly recommended to prevent the thromboembolic events enhanced by stent positioning1,2,11). However, in the cases of ruptured aneurysms, the procedures should be performed as early as possible, so the recommended premedication with dual antiplatelets of clopidogrel and aspirin for more than three days could not be applied in most cases. Katsaridis et al.4) reported a series of 44 patients treated with stent and coiling for ruptured intracranial aneurysms who were not pretreatment with antiplatelet agents without serious complications such as a aneurysm bleeding, aneurysm recanalization and/or thromboembolic events. Also, Kim5), the senior author of this report previously eported the safety of the stent assisted coiling in the acute stage on the ruptured aneurysms without dual antiplatelets premedication.
However, some broad neck aneurysms, such as the ones located at parent vessel bifurcation, are not amenable to treatment with a single stent. It is interesting that some reports on unconventional use of the stent have provided intelligent technical solutions to difficult endovascular cases. Thorell et al.12) and Perez-Arjona and Fessler10) reported on a Y-configuration deployment of two Neuroform stents applied in the treatment of a broad neck basilar top aneurysm; Y-configuration stenting was technically successful in most reports; however, difficulty in stent deployment was encountered in several cases during delivery of the second stent. The friction within the system and acute angle prevented the delivery of the stent with mere utilization of the stabilizer. Moreover, stent navigation over the microguidewire carries significant risk of a ruptured aneurysm and technically very difficulty with acute angle (over 90 degrees). For aneurysms involving bilateral P1 segments, stent placement in any side of P1 is not enough for retaining the coils in the aneurysm sac and preservation of the parent vessels.
In this situation, the modified waffle-cone technique has become a feasible method. Horowitz et al.3) described the use of a waffle cone arrangement in the management of broad neck bifurcation aneurysms. This technique involves the deployment of a single Neuroform stent placed in the basilar artery. The distal component of the stent is allowed to fan out as it is extruded into the bifurcation at the neck of the aneurysm. However, there are disadvantages of this technique. First, placement of the stent into the aneurysm exposes to potential risk of perforation, which is especially true for the smaller aneurysms. Second, flow direction into the aneurysm via stent may predispose to more rapid rates of recanalization.
In this report, we described the modified Y-configured stents with waffle cone technique for the first time using an open cell stent through closed cell stent system. In our opinion, it enables to make a waffle cone shape with narrower base when a Neuroform stent is deployed through an Enterprise stent which offers the closed strut system because closed strut system hold a Neuroform stent at the point of penetration. Moreover, it may prevent the injury of aneurysm base by the end of the stent when stent strut spreads out. Furthermore, this technique has not been described before for the treatment of ruptured broad neck aneurysm arising from the basilar top.
CONCLUSION
Successful endovascular treatment of ruptured broad neck aneurysm from basilar top is technically feasible with the modified Y-configured stents with waffle cone technique. More clinical data with longer follow-up are needed to help establish the role of this technique in ruptured intracranial aneurysms.
References
- 1.Biondi A, Janardhan V, Katz JM, Salvaggio K, Riina HA, Gobin YP. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms : strategies in stent deployment and midterm follow-up. Neurosurgery. 2007;61:460–468. doi: 10.1227/01.NEU.0000290890.62201.A9. discussion 468-469. [DOI] [PubMed] [Google Scholar]
- 2.Fiorella D, Albuquerque FC, Deshmukh VR, McDougall CG. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms : results at initial (3-6-mo) follow-up. Neurosurgery. 2005;56:1191–1202. doi: 10.1227/01.neu.0000159645.86823.af. discussion 1201-1202. [DOI] [PubMed] [Google Scholar]
- 3.Horowitz M, Levy E, Sauvageau E, Genevro J, Guterman LR, Hanel R, et al. Intra/extra-aneurysmal stent placement for management of complex and wide-necked-bifurcation aneurysms : eight cases using the waffle cone technique. Neurosurgery. 2006;58:ONS258–ONS262. doi: 10.1227/01.NEU.0000204713.24945.D2. discussion ONS262. [DOI] [PubMed] [Google Scholar]
- 4.Katsaridis V, Papagiannaki C, Violaris C. Embolization of acutely ruptured and unruptured wide-necked cerebral aneurysms using the neuroform2 stent without pretreatment with antiplatelets : a single center experience. AJNR Am J Neuroradiol. 2006;27:1123–1128. [PMC free article] [PubMed] [Google Scholar]
- 5.Kim YJ. Early experiences of neuroform stent-assisted coiling in ruptured intracranial aneurysms. Interv Neuroradiol. 2007;13:31–44. doi: 10.1177/159101990701300104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kwon OK, Kim SH, Oh CW, Han MH, Kang HS, Kwon BJ, et al. Embolization of wide-necked aneurysms with using three or more microcatheters. Acta Neurochir (Wien) 2006;148:1139–1145. doi: 10.1007/s00701-006-0876-4. discussion 1145. [DOI] [PubMed] [Google Scholar]
- 7.Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms : a randomised trial. Lancet. 2002;360:1267–1274. doi: 10.1016/s0140-6736(02)11314-6. [DOI] [PubMed] [Google Scholar]
- 8.Molyneux AJ, Kerr RS, Yu LM, Clarke M, Sneade M, Yarnold JA, et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms : a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. Lancet. 2005;366:809–817. doi: 10.1016/S0140-6736(05)67214-5. [DOI] [PubMed] [Google Scholar]
- 9.Moret J, Cognard C, Weill A, Castaings L, Rey A. [Reconstruction technic in the treatment of wide-neck intracranial aneurysms. Long-term angiographic and clinical results Apropos of 56 cases.] J Neuroradiol. 1997;24:30–44. [PubMed] [Google Scholar]
- 10.Perez-Arjona E, Fessler RD. Basilar artery to bilateral posterior cerebral artery 'Y stenting' for endovascular reconstruction of wide-necked basilar apex aneurysms : report of three cases. Neurol Res. 2004;26:276–281. doi: 10.1179/016164104225013969. [DOI] [PubMed] [Google Scholar]
- 11.Sedat J, Chau Y, Mondot L, Vargas J, Szapiro J, Lonjon M. Endovascular occlusion of intracranial wide-necked aneurysms with stenting (Neuroform) and coiling : mid-term and long-term results. Neuroradiology. 2009;51:401–409. doi: 10.1007/s00234-009-0502-2. [DOI] [PubMed] [Google Scholar]
- 12.Thorell WE, Chow MM, Woo HH, Masaryk TJ, Rasmussen PA. Y-configured dual intracranial stent-assisted coil embolization for the treatment of wide-necked basilar tip aneurysms. Neurosurgery. 2005;56:1035–1040. discussion 1035-1040. [PubMed] [Google Scholar]
- 13.Vallée JN, Pierot L, Bonafé A, Turjman F, Flandroy P, Berge J, et al. Endovascular treatment of intracranial wide-necked aneurysms using three-dimensional coils : predictors of immediate anatomic and clinical results. AJNR Am J Neuroradiol. 2004;25:298–306. [PMC free article] [PubMed] [Google Scholar]