Abstract
Although posterior segmental fixation technique is becoming increasingly popular, surgical treatment of craniovertebral junctional disorders is still challenging because of its complex anatomy and surrounding critical neurovascular structures. Basilar invagination is major pathology of craniovertebral junction that has been a subject of clinical interest because of its various clinical presentations and difficulty of treatment. Most authors recommend a posterior occipitocervical fixation following transoral decompression or posterior decompression and occipitocervical fixation. However, both surgical modalities inadvertently sacrifice C0-1 and C1-2 joint motion. We report two cases of basilar invagination reduced by the vertical distraction between C1-2 facet joint. We reduced the C1-2 joint in an anatomical position and fused the joint with iliac bone graft and C1-2 segmental fixation using the polyaxial screws and rods C-1 lateral mass and the C-2 pedicle.
Keywords: Atlantoaxial instability, Basilar invagination, Vertical reduction
INTRODUCTION
Cervical spinal diseases associated with atlantoaxial instability (AAI) and basilar invagination (BI) are rare, and because of the anatomical characteristic of the upper cervical spine, the decision making for treatment and surgical treatments are difficult. If the diagnosis and treatment are overlooked in cases with AAI and (or) BI, the autonomic center could be compromised and result in catastrophic consequences such as labile blood pressures, arrhythmias, or sudden death due to high cervical myelopathy and brain stem compression at the foramen magnum level16). The novel technique applied the polyaxial screws and rods C1 lateral mass and the C2 pedicle described by Harms and Melcher6) is considered to be a breakthrough for the treatment of diseases associated with AAI. In addition, Goel has reported the method to correct the craniospinal alignment by the distraction of the C1-2 facet joint in patients with BI et al.5). We report our experience of 2 cases of AAI associated with BI treated simultaneously by the distraction using the direct manipulation of C1-2 screws and subsequently the insertion of an autograft as facet joint spacer by the modified method of Harms and Goel.
CASE REPORT
Case 1
History and examination
A 45-year-old male patient was admitted for diffuse neck pain developed from 3 years ago. There was no history of special trauma or rheumatoid arthritis. In the physical examination, abnormal findings were not detected, and in the neurologic examination, motor weakness or sensory changes were not detected. In cervical spine X-ray and computed tomography (CT), the atlanto-dental interval (ADI) was observed to be increased by 10 mm at the neutral and flexion position, the protrusion of the tip of odontoid to the McRae line11) just above, which was the finding suspicious to be BI, and thus various radiologic criteria diagnosing BI were measured (Fig. 1A). The odontoid tip was located below the Chamberlain line2), the apex of odontoid tip was located above the McGregor line10) by 3.5 mm, which did not meet the criteria of BI. Nonetheless, in the Clark station3), the anterior ring of the atlas was located in the station II, and it was 32 mm by the Redlund-Johnell criterion14), 11 mm by the Ranawat criterion13), and findings satisfying the criteria of BI were observed. In cervical spine magnetic resonance imaging, on T2 weighted images, high signal changes of the spinal cord at the C1-2 level was not shown, but behind the spinal cord, compression finding was detected. In CT angiogram, the findings of the high riding vertebral artery, abnormal course of vertebral artery, and narrow C2 pedicle were not observed. Evaluating the findings, we diagnosed this patient as idiopathic AAI associated with BI, and surgery was performed to correct the two pathologies simultaneously.
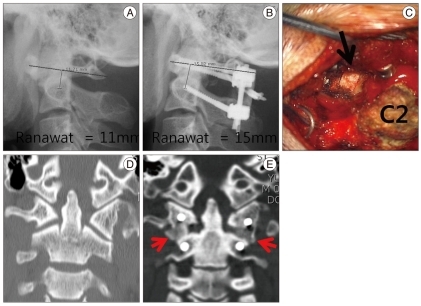
Fig. 1.
Case 1 image findings. A : Preoperative X-ray showing increased atlantodental interval about 10 mm and Ranawat criterion being 11 mm. B : Postoperative X-ray showing C1-2 fixation as well as vertical reduction of basilar invagination. C : Intraoperative photograph showing an autograft iliac bone spacer inserted in the C1-2 facet joint (arrow). D and E : Compared with preoperative computed tomography (CT), postoperative CT showing distracted joint space in which autograft iliac bone spacer (arrow) have been placed.
Operation
Under the intraoperative electrophysiologic monitoring system (IOM), intentional sacrifice of bilateral C2 ganglions were performed to obtain enough space for C1 screw entry point and bone fusion surface. Subsequently, by the application of Harms and Melcher6) technique, polyaxial screws were inserted to the bilateral C1 lateral masses and the C2 pedicles. The C1-2 joint was slightly distracted using a distractor, and the articular cartilages were removed widely using a curette and a high speed burr. The C1-2 joint was slightly distracted carefully under IOM to avoid overdistraction and subsequent stretching injury of the spinal cord and 8 mm iliac bone autograft were inserted bilaterally as joint spacers to maintain the vertical reduction, subsequently interlaminar fusion was performed using autograft iliac bone blocks and cables (Fig. 1C).
Postoperative course
After surgery, special neurological defects or occipital neuralgia caused by the resection of C2 ganglion were not seen and troublesome neck pain became tolerable immediately after surgery. In postsurgical cervical spine X-ray and CT, the Clark station, the Redlund-Johnell criterion and the Ranawat criterion were station I, 39 mm, and 15 mm, respectively, and they were restored to normal ranges (Fig. 1B, D, E).
Case 2
History and examination
A 69-year-old female patient was brought to emergency room because of sudden stuporous mentality. There was severe brain swelling with hemorrhagic infarction of the left cerebellar hemisphere on brain CT. In cervical spine X-ray, ADI was 9 mm and AAI findings were shown together with cervical kyphotic deformity. The tip of odontoid process was protruded above the McRae line11) by 5 mm. The odontoid tip was located above the Chamberlain line2) by 8 mm, and the apex of odontoid tip was located above the McGreger line10) by 11 mm. In the Clark station3), the anterior ring of the atlas was located in the station II, it was 32 mm by the Redlund-Johnell criterion14), 10 mm by the Ranawat cirterion13), and except the Redlund-Johnell criterion, the findings corresponding to the criteria of BI were evident (Fig. 2A, C, E).
Fig. 2.
Case 2 image findings. A : Preoperative X-ray showing severe kyphosis with degenerative spondylotic change and increased ADI about 9 mm and BI. B : Postoperative X-ray showing correction of cervical kyphosis and reduction of BI as well as C1-4 fixation. C-F : Compared with preoperative CT, postoperative CT showing decompressed craniovertebral junction and distracted joint space in which in which autograft iliac bone spacer (arrow) have been placed. ADI : atlanto-dental interval, BI : basilar invagination, CT : computed tomography.
Operation
Concerning the injury of cervicomedullary junction due to the neck flexion position during the emergency decompression of posterior inferior cerebellar artery infarction, correction of the high cervical deformity and decompression were performed first. To prevent hardware failures caused by C1 laminectomy for cervicomedullary decompression, kyphosis correction and poor bone quality, except the fusion extension using C3 and 4 lateral mass screws, surgery for AAI and BI was performed by the method identical to the case 1. After the surgery for the cervical spinal area, as planned, suboccipital decompression and extraventricular drainage were performed sequentially.
Postoperative course
After surgery, the mentality of patient was recovered slowly, and distinct motor weakness findings were not shown. In postsurgical cervical spine X-ray, the Clark station, the Redlund-Johnell criterion, and the Ranawat criterion were station I, 41 mm, and 17 mm, respectively, and they were restored to normal ranges (Fig. 2B, D, F).
DISCUSSION
In patients with anomalies including instability in the craniovertebral junction, because of the proprietary characteristic of the area such as the presence of the occipital bone, clivus, foramen magnum, upper cervical vertebrae, their associated ligaments, vertebral artery, and spinal cord, factors that should be considered in the surgical decision making are numerous and complex13). Among them, for AAI and BI cases with the symptom of the protruded odontoid tip compressing the spinal cord or the brain stem in the ventral side, the choice treatment was to perform first anterior transoral odontoidectomy and occipitocervical fusion or cervical traction and thus performing the release of the ligaments around the odontoid process, and subsequently to perform posterior fusion4,12,17,18).
During the past three decades, particularly in the past 10 years, there have been significant improvements in atlantoaxial fusion techniques, and various methods of atlantoaxial fixation have been described in the literature7,9). Due to such development, in BI, posterior only surgery was attempted. Goel et al.5) have reported that in selected case of BI, posterior only surgery was feasible by intraoperative cervical traction followed by the distraction of C1-2 facet joint, and subsequently, firm lateral mass fixation. Aryan et al.1) have reported that for cases with significant instability or vertical settling, allograft spacers were inserted to the C1-2 joint space. In addition, Jian et al.8) have reported that BI with AAI was treated by the direct posterior distraction technique between occiput and C2 pedicle screws.
After the report of a novel technique using the polyaxial screws and rods C1 lateral mass and C2 pedicle described by Harms and Melcher6), the direct manipulation of C1 and C2 using the instrumentation as the reduction device became feasible. Similar to the 2 cases reported by us, in BI associated with AAI, although the ventral spinal cord compression was not severe, after placing the instrumentation, the C1-2 facet joint was released, and autograft iliac bone spacers were inserted by distracting C1 and C2 screw. Cervical traction was not necessary preoperatively or even during the operation, because intraoperative C1-2 reduction was possible using C1-2 segmental screw construct. The procedure has several advantages; 1) vertical reduction of BI can eliminate the necessity of additional posterior decompressive procedure such as C1 laminectomy and posterior fossa decompression, 2) increase of the fusion bed using the facet graft could enhance fusion rate, 3) reduction of the risk of trans-oral surgery, 4) minimization of cervical traction prior to surgery or during surgery, and 5) preservation of occipito-atlantal motion avoiding occipito-cervical fusion.
C2 root resection is necessary to expose enough space of C1-2 facet joint and perform the entire operation under direct vision. Ames et al.1) have reported that there was no cerebrospinal fluid leakage and only one case of neuropathic pain postoperatively after sacrificing the C2 roots in 102 patients, however, routine sacrifice of C2 roots is controversial and long term follow up is mandatory to analyze the clinical effect of C2 nerve root resection.
Direct distraction of C1-2 facet joint can be used to reduce basilar invagination and to expose room for bone graft insertion within the joint cavity, which could provide remarkable stability to the region by itself. Exposed C1-2 facet joint surface provides a wide space for bone fusion. However, in cases of more severe ventral compression combined with irreducible BI, this procedure must be warranted by further investigation and transoral decompression might be necessary before or after posterior surgery.
Considering the spinal cord damage caused by overdistraction, the IOM should be observed carefully during the distraction performed after the facet release, and it is thought that the size of graft should be determined by considering the level of height restoration in advance. In addition, to prevent injury of spinal cord and medulla oblongata caused by the posterior shifting of the odontoid process, distraction should be performed while fixating C2 screws with a screwdriver8).
CONCLUSION
We report experiences of AAI cases without severe ventral compression and associated with BI. The stabilization of AAI and the vertical reduction of BI were performed simultaneously by performing distraction of C1-2 facet joint with C1-2 screws, and inserting autograft iliac bone as facet joint spacers. These cases show the importance to determine the presence or absence of vertical instability and reducibility in cases with BI. Stabilization and fusion in a reduced and anatomical position can reduce the level of fixation, result in sound bone fusion using interfacetal bone graft and maintain the occipitoatlantal joint motion.
References
- 1.Aryan HE, Newman CB, Nottmeier EW, Acosta FL, Jr, Wang VY, Ames CP. Stabilization of the atlantoaxial complex via C-1 lateral mass and C-2 pedicle screw fixation in a multicenter clinical experience in 102 patients : modification of the Harms and Goel techniques. J Neurosurg Spine. 2008;8:222–229. doi: 10.3171/SPI/2008/8/3/222. [DOI] [PubMed] [Google Scholar]
- 2.Chamberlain WE. Basilar Impression (Platybasia) : a Bizarre Developmental Anomaly of the Occipital Bone and Upper Cervical Spine with Striking and Misleading Neurologic Manifestations. Yale J Biol Med. 1939;11:487–496. [PMC free article] [PubMed] [Google Scholar]
- 3.Clark CR, Goetz DD, Menezes AH. Arthrodesis of the cervical spine in rheumatoid arthritis. J Bone Joint Surg Am. 1989;71:381–392. [PubMed] [Google Scholar]
- 4.Dickman CA, Locantro J, Fessler RG. The influence of transoral odontoid resection on stability of the craniovertebral junction. J Neurosurg. 1992;77:525–530. doi: 10.3171/jns.1992.77.4.0525. [DOI] [PubMed] [Google Scholar]
- 5.Goel A, Kulkarni AG, Sharma P. Reduction of fixed atlantoaxial dislocation in 24 cases : technical note. J Neurosurg Spine. 2005;2:505–509. doi: 10.3171/spi.2005.2.4.0505. [DOI] [PubMed] [Google Scholar]
- 6.Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine (Phila Pa 1976) 2001;26:2467–2471. doi: 10.1097/00007632-200111150-00014. [DOI] [PubMed] [Google Scholar]
- 7.Hong JT, Yi JS, Kim JT, Ji C, Ryu KS, Park CK. Clinical and radiologic outcome of laminar screw at C2 and C7 for posterior instrumentation--review of 25 cases and comparison of C2 and C7 intralaminar screw fixation. World Neurosurg. 2010;73:112–118. doi: 10.1016/j.surneu.2009.06.010. discussion e15. [DOI] [PubMed] [Google Scholar]
- 8.Jian FZ, Chen Z, Wrede KH, Samii M, Ling F. Direct posterior reduction and fixation for the treatment of basilar invagination with atlantoaxial dislocation. Neurosurgery. 2010;66:678–687. doi: 10.1227/01.NEU.0000367632.45384.5A. discussion 687. [DOI] [PubMed] [Google Scholar]
- 9.Kuroki H, Rengachary SS, Goel VK, Holekamp SA, Pitkänen V, Ebraheim NA. Biomechanical comparison of two stabilization techniques of the atlantoaxial joints : transarticular screw fixation versus screw and rod fixation. Neurosurgery. 2005;56:151–159. doi: 10.1227/01.neu.0000144838.01478.35. discussion 151-159. [DOI] [PubMed] [Google Scholar]
- 10.McGreger M. The significance of certain measurements of the skull in the diagnosis of basilar impression. Br J Radiol. 1948;21:171–181. doi: 10.1259/0007-1285-21-244-171. [DOI] [PubMed] [Google Scholar]
- 11.McRae DL, Barnum AS. Occipitalization of the atlas. Am J Roentgenol Radium Ther Nucl Med. 1953;70:23–46. [PubMed] [Google Scholar]
- 12.Menezes AH, VanGilder JC, Graf CJ, McDonnell DE. Craniocervical abnormalities. A comprehensive surgical approach. J Neurosurg. 1980;53:444–455. doi: 10.3171/jns.1980.53.4.0444. [DOI] [PubMed] [Google Scholar]
- 13.Ranawat CS, O'Leary P, Pellicci P, Tsairis P, Marchisello P, Dorr L. Cervical spine fusion in rheumatoid arthritis. J Bone Joint Surg Am. 1979;61:1003–1010. [PubMed] [Google Scholar]
- 14.Redlund-Johnell I, Pettersson H. Radiographic measurements of the cranio-vertebral region. Designed for evaluation of abnormalities in rheumatoid arthritis. Acta Radiol Diagn (Stockh) 1984;25:23–28. doi: 10.1177/028418518402500105. [DOI] [PubMed] [Google Scholar]
- 15.Riew KD, Hilibrand AS, Palumbo MA, Sethi N, Bohlman HH. Diagnosing basilar invagination in the rheumatoid patient. The reliability of radiographic criteria. J Bone Joint Surg Am. 2001;83-A:194–200. doi: 10.2106/00004623-200102000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Slätis P, Santavirta S, Sandelin J, Konttinen YT. Cranial subluxation of the odontoid process in rheumatoid arthritis. J Bone Joint Surg Am. 1989;71:189–195. [PubMed] [Google Scholar]
- 17.Subin B, Liu JF, Marshall GJ, Huang HY, Ou JH, Xu GZ. Transoral anterior decompression and fusion of chronic irreducible atlantoaxial dislocation with spinal cord compression. Spine (Phila Pa 1976) 1995;20:1233–1240. doi: 10.1097/00007632-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Wang C, Yan M, Zhou HT, Wang SL, Dang GT. Open reduction of irreducible atlantoaxial dislocation by transoral anterior atlantoaxial release and posterior internal fixation. Spine (Phila Pa 1976) 2006;31:E306–E313. doi: 10.1097/01.brs.0000217686.80327.e4. [DOI] [PubMed] [Google Scholar]