Abstract
Purpose
To report our results on urinary continence after bladder neck preservation (BNP) and posterior urethral reconstruction (PUR) during robot-assisted laparoscopic radical prostatectomy (RALP).
Materials and Methods
Data from 107 patients who underwent RALP were compared on the basis of whether the patients underwent BNP and PUR, BNP only, or the standard technique (ST). In group A (n=31 patients), ST was performed by using Ven velthoven continuous suturing for urethrovesical anastomosis. In group B (n=28 patients), ST with only PUR was performed. In group C (n=48 patients), both the BNP and PUR techniques were used. "Recovery of continence" was defined as the use of 1 pad (50 ml) or less within 24 hours.
Results
The three groups were comparable in terms of patient demographics. The mean operative time and the mean blood loss decreased significantly from group A to group C (p=0.021 for mean operative time and p=0.004 for the mean blood loss). Mean catheterization time was 8.9, 7.8, and 7.1 days in each group (p=0.047). Early return of urinary continence at 3 months was observed in group B (89.2%) and group C (90.6%) compared with group A (71%). However, continence at 6 months was comparable in the 3 groups (87.5% in group A, 92.8% in group B, and 92.3% in group C). Rates of positive surgical margins decreased from 30.2% in group A to 20% in group B and 12% in group C.
Conclusions
BNP and PUR during RALP showed a favorable impact on the early postoperative recovery of continence while not affecting positive surgical margins.
Keywords: Prostatectomy, Prostatic neoplasms, Urinary incontinence
INTRODUCTION
Robot-assisted laparoscopic radical prostatectomy (RALP) has been rapidly accepted as a viable option for the minimally invasive surgical treatment of localized prostate cancer. Since the introduction of the da Vinci Robotic Surgical System (Intuitive Inc., Surgical, CA, USA) in 2001, various reports on RALP have claimed comparable or superior outcomes to open and laparoscopic surgery in oncological and functional aspects [1].
The recovery of potency and continence are important factors for the quality of life of patients undergoing RALP. The recovery of continence depends on various factors, and among these, the surgical technique is considered most critical. Urinary incontinence is usually temporary in most patients. The recovery rate is satisfactory, with rates of 85% to 97% by 1 year after radical prostatectomy, but complete recovery may require a much longer time in some patients [2-6]. In this study, we compared the outcomes of bladder neck preservation (BNP) using lateral bladder neck dissection (LBND) and the posterior urethral reconstruction (PUR) techniques for early recovery of continence during RALP. The effects on the early recovery of continence and positive surgical margins (+SMs) were evaluated and compared when the BNP technique using LBND and the PUR technique were used.
MATERIALS AND METHODS
The study subjects included 107 patients who underwent RALP owing to localized prostate cancer within the period from January 2008 to August 2010. The following techniques for early recovery of continence were performed chronologically, and recovery of continence was observed during this period. In group A, standard RALP techniques with Ven velthoven continuous suturing for urethrovesical anastomosis (UVA) were performed in 31 patients. In group B, standard RALP techniques with PUR and Ven velthoven continuous suturing for UVA were performed in 28 patients. In group C, standard RALP techniques using LBND as the BNP technique with PUR and Ven velthoven continuous suturing for UVA were performed in 48 patients.
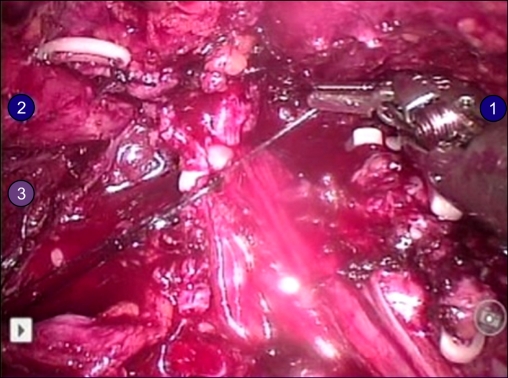
The Ven velthoven technique requires continuous suturing of the urethra using monofilament 3-0 double arm sutures from 6 to 12 o'clock of the urethral lumen. The PUR technique requires identification of the posterior portion of the rhabdosphincter and the anterior leaflet of Denovilliers fascia. Using one arm of the continuous suture, the posterior part of the rhabdosphincter is anchored with continuous sutures of three to four bites to the remaining portion of the Denovilliers fascia. The other arm of the continuous suture is then placed to approximate between the posterior bladder neck and the posterior urethra and then tied to the other arm of the continuous suture (Fig. 1). Another arm of the continuous suture is used to perform Ven velthoven continuous suturing for UVA. Lateral bladder neck dissection for the BNP technique requires precise identification of the detrusor muscle fibers at the critical junction of the lateral bladder neck, prostate base, and the fat pad.
FIG. 1.
Posterior urethral reconstruction. The posterior urethral reconstruction (PUR) technique requires identification of the posterior portion of the rhabdosphincter and the anterior leaflet of Denovilliers fascia. With the use of one arm of the continuous suture, the posterior part of the rhabdosphincter is anchored with continuous sutures of three to four bites to the remaining portion of the Denovilliers fascia.
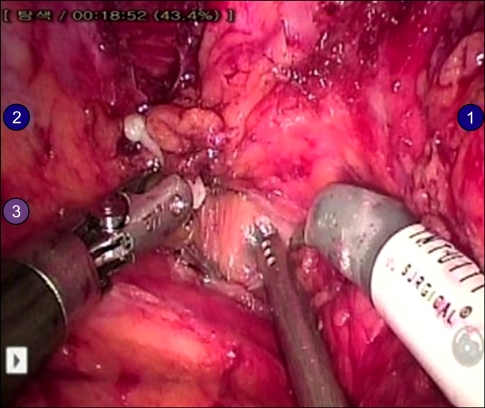
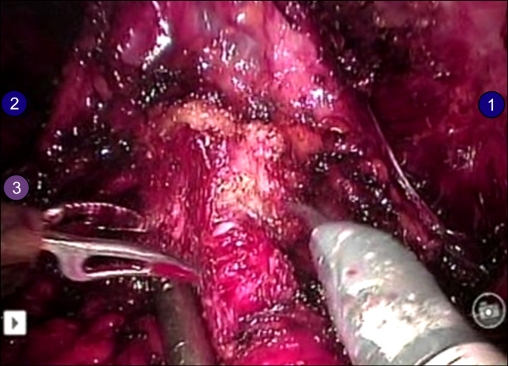
Meticulous dissection is performed just medially to the fat pad of Whitmore encountering adipose tissue and the lateral border of the bladder neck, while appreciating the ventrolateral and dorsal longitudinal muscles, until the dissection reaches the prostate base and the anterior surface of the seminal vesicle. After the bilateral dissection of the lateral bladder neck, which exposes the anterior surface of the seminal vesicle, the detrusor muscles in the posterior bladder neck are well appreciated medially from the anterior surface of the seminal vesicles and the bladder neck is then approached at the midline. The dissection is continued until distinct musculus sphincter vesicae are identified and preserved, and then the bladder neck is divided (Figs. 2, 3).
FIG. 2.
Bladder neck preservation technique using lateral bladder neck dissection. The picture shows the left side of the lateral bladder neck dissection. The lateral bladder neck dissection technique requires precise identification of the detrusor muscle fibers at the critical junction of the lateral bladder neck, prostate base, and the fat pad of Whitmore. Meticulous dissection is performed just medially to the fat pad of Whitmore encountering adipose tissue and the lateral border of the bladder neck while appreciating the ventrolateral and dorsal longitudinal muscles until the dissection reaches the prostate base and the anterior surface of the seminal vesicle.
FIG. 3.
Bladder neck transection. The figure shows a well-preserved bladder neck at the medial aspect between the prostate and the bladder neck.
The medical records of the patients were collected, and the preoperative and postoperative clinical course and recovery of continence in the three groups were compared. Digital rectal examination, prostate biopsy, magnetic resonance imaging, and bone scan were performed before RALP in all patients. Perioperative parameters such as operative time, blood loss, catheterization time, pathology data, and positive surgical margin rate (+SMR) were reviewed from our surgical database. Urinary continence was evaluated by using the International Continence Society questionnaire. Postoperative continence was assessed through a questionnaire survey administered 1 day after catheter removal, and at intervals of 1 month, 3 months, and 6 months after RALP. Postoperative continence was defined as lack of incontinence or the use of less than one diaper (50 ml) per day for security. Postoperative cystograms were performed in all patients on the 7th postoperative day. In the case of leakage, catheterization was maintained for an additional 5 to 10 days and the cystogram was repeated. The variables before and after the operation among the patient groups were compared by using one-way analysis of variance test and Fisher's exact test, and p values of less than 0.05 were considered statistically significant. SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis.
RESULTS
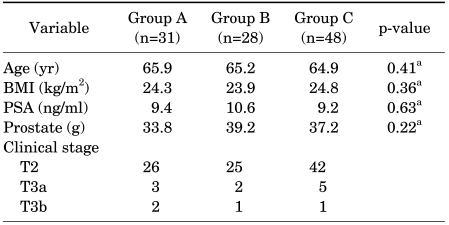
The mean age of the patients in groups A, B, and C was 65.9, 65.2, and 64.9 years, respectively (p=0.41), and the mean preoperative prostate-specific antigen values were 9.4, 10.6, and 9.2 ng/ml, respectively (p=0.63). The mean body mass index values were 24.3, 23.9, and 24.8 kg/m2, respectively, (p=0.36), and the mean prostate sizes were 33.8, 39.2, and 37.2 g, respectively (p=0.22) (Table 1). The Gleason grade was similar in the 3 groups: 6.89 in group A, 6.68 in group B, and 6.61 in group C (p=0.37). Also, the International Prostate Symptom Score was comparable in the 3 groups: 18.6 in group A, 18.8 in group B, and 17.9 in group C (p=0.47).
TABLE 1.
Preoperative patient characteristics
BMI, body mass index; PSA, prostate-specific antigen.
a: Student's t-test.
The tumor stages in the 3 groups were comparable (p=0.39). The preoperative stages were as follows: 26 patients in T2, 3 in T3a, and 2 in T3b for group A; 25 patients in T2, 2 in T3a, and 1 in T3b for group B; and 42 patients in T2, 5 in T3a, and 1 in T3b for group C.
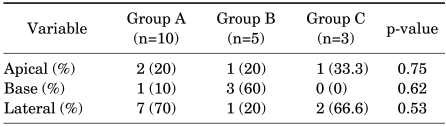
The mean operative times were 226.3, 192.1, and 170.9 minutes, respectively (p=0.021), and the mean blood loss was 188, 121.3, and 106.8 ml, respectively (p=0.004). The catheterization time was 8.9, 7.8, and 7.1 days in each group (p=0.047). In the postoperative cystogram, two cases of urine leakage were reported in group A, whereas no cases were observed in groups B and C. The postoperative +SMRs were 10 patients in group A (31.2%), 5 patients in group B (17.9%), and 3 patients in group C (6.3%) (Table 2). In group A, seven patients had +SMs in the lateral, two in the base, and one in the apical area of the prostate. In group B, one patient had +SMs in the lateral, three in the base, and one in the apical area of the prostate. In group C, two patients had +SMs in the lateral and one in the apical area of the prostate (Table 3).
TABLE 2.
Intraoperative and postoperative outcomes
EBL, estimated blood loss.
a: one-way ANOVA test.
TABLE 3.
Positive surgical margins according to the location of the prostate
Values are presented as number (%).
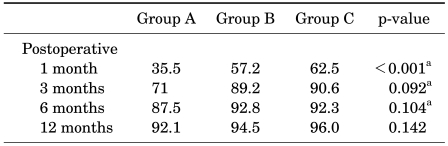
Continence was assessed by recording pad usage 1 day after catheter removal and 3, 6, and 12 months postoperatively. Recovery of continence was reported as follows: 11 patients by 1 month (35.5%), 22 patients by 3 months (71.0%), and 27 patients by 6 months (87.5%) in group A; 16 patients by 1 month (57.2%), 25 patients by 3 months (89.2%), and 26 patients by 6 months (92.8%) in group B; and 30 patients by 1 month (62.5%), 36 patients by 3 months (90.6%), and 29 patients by 6 months (92.3%) in group C (Table 4). Early return of continence at 3 months of follow-up was observed in groups B and C compared with group A. Continence at 1 year was comparable in the 3 groups: 92.1% in group A, 94.5% in group B, and 96.0% in group C.
TABLE 4.
Return of continence according to operative methods
Recovery of continencewas defined as the use of 1 pad (50 ml) or less within 24 hours.
a: one-way analysis of variance test.
DISCUSSION
Recent advances in video-endoscopic equipment and the development of minimally invasive surgical techniques have reduced the rates of mortality and complications from radical prostatectomy. In particular, the da Vinci Robotic Surgical System (Intuitive Inc., Sunnyvale, CA, USA), which was introduced in 2001, offers a stable and magnified operative field, enables meticulous dissection and the preservation of the bladder neck, and enhances nerve-sparing and suturing for UVA during RALP. Despite these improvements, however, temporary postoperative incontinence is blamed for lowering the quality of life of patients after RALP. Therefore, to achieve early return of continence, various authors have introduced numerous techniques with variable outcomes [7,8]. In the current study, patients treated with BNP using LBND and the PUR techniques showed an advantage with respect to early continence. Nevertheless, no statistically significant difference was observed at 6 and 12 months postoperatively among the 3 groups.
Since the adaptation of the running, bidirectional monofilament anastomosis to UVA in 2003, several modifications have been introduced to enhance watertight cooptation of UVA. A technique reported by Rocco et al. [9] arose from a theory based on the functional anatomy and restores the posterior aspect of the rhabdosphincter with radical prostatectomy, from which recovery of continence is expected. Data from open radical prostatectomy using Rocco's technique reported 74% recovery of continence. In addition, in a study that followed up 100 patients for 13.3 months, Duthie et al. [10] reported 68% recovery of continence by 12 months with the improvements in the surgical technique. In the current study, we experienced the additive effects of PUR when compared with the Ven velthoven continuous suturing technique. This technique allows approximating the bladder neck closer to the urethra and thus enables tension-free UVA and prevents leakage at the UVA site.
Rebuck et al. [11] compared the outcomes of RALP with the Ven velthoven continuous suturing technique and reported a reduction in incontinence from 26.2% to 14.3% to 2.3% with the progress in the surgical technique, as shown in the cystogram. In addition, the recovery time was shortened as the staff gained more experience in this technique. He also observed a decreased rate of urine leakage and the early recovery of continence when the highly experienced staff used the technique. In our prior experience, we moved to the continuous suturing technique for UVA from the interrupted sutures in the early days of laparoscopic radical prostatectomy because the Ven velthoven continuous suturing technique was shown confer a better continence rate.
Controversy exists in the current literature regarding BNP. The BNP technique was first described by Curto and Gaston in 2006. Using the BNP technique in 1400 cases from 2001 to 2010, Asimakopoulos et al. [12] reported 80% recovery of continence immediately after catheter removal and 73% recovery of continence in the remaining patients by 3 months. In South Korea, Jeong et al. [13] reported the methodology and outcome of typical RALP using both Rocco's and the BNP technique. In his study, 91% recovery of continence was observed in the patient group that underwent surgery using the BNP technique. In our study, Group C showed a significant benefit in early recovery of continence. Also, more than 90% recovery of continence was observed in all the groups 6 months after RALP. However, when the outcomes were compared at 1, 3, and 6 months after RALP, early recovery of continence was confirmed in group C in which both Rocco's and the BNP techniques were used. We assume that the PUR technique restores the normal anatomic position and reinforces the backbone in the axis of the pelvic anatomy.
Regarding +SMs, some reports showed that the +SMR was high in the group with the BNP technique, but our study showed no differences. When performing the BNP technique by LBND, it is crucial to identify the detrusor muscle fibers at the critical junction of the lateral bladder neck, the prostate base, and the fat pad laterally. The meticulous dissection must be utilized just medially to the fat pad of Whitmore to avoid inadvertent bleeding from the lateral venous plexus while appreciating the ventrolateral and dorsal longitudinal bladder muscles medially, until the dissection reaches the prostate base and the anterior surface of the seminal vesicle. Clear visualization and identification of the surgical landmarks and meticulous dissection will reduce the +SMR.
When both Rocco's and the BNP techniques were used as in group C, the early return of continence was observed. In addition, there was no sign of leakage at the site of UVA when both techniques were used. It is possible that recovery was achieved earlier due to the absence of leakage, which is thought to have an adverse effect on the healing of the UVA and recovery of continence. The PUR technique helps to reduce the tension between the urethra and the bladder, leading to more stable and watertight UVA.
There are several limitations to our study. The study was performed in a retrospective manner and the patients were not randomly assigned. Also, because operative methods were performed chronologically, there may have been some contribution of the learning curve, because cases accumulated with the BNP and the PUR techniques. However, patients with large prostates or prominent median lobes were not spared from performing the BNP technique and a single surgeon performed all the procedures in this study. Even though our study did not address the impact of these factors on postoperative outcomes, continence and +SMs did not vary across the study groups.
CONCLUSIONS
Posterior urethral reconstruction reduced the risk of urine leakage and proved to have good outcomes on early continence. When both bladder neck preservation using lateral bladder neck dissection and the posterior urethral dissection techniques were used, a much better outcome was observed in the early recovery of continence at the 3 month follow-up. Also, bladder neck preservation did not influence +SMs. Further studies of these surgical techniques are expected to achieve better quality of life for patients undergoing RALP.
Footnotes
The authors have nothing to disclose.
References
- 1.Cho JW, Kim TH, Sung GT. Laparoscopic radical prostatectomy versus robot-assisted laparoscopic radical prostatectomy: a single surgeon's experience. Korean J Urol. 2009;50:1198–1202. [Google Scholar]
- 2.Rassweiler J, Sentker L, Seemann O, Hatzinger M, Rumpelt HJ. Laparoscopic radical prostatectomy with the Heilbronn technique: an analysis of the first 180 cases. J Urol. 2001;166:2101–2108. [PubMed] [Google Scholar]
- 3.Eden CG, Cahill D, Vass JA, Adams TH, Dauleh MI. Laparoscopic radical prostatectomy: the initial UK series. BJU Int. 2002;90:876–882. doi: 10.1046/j.1464-410x.2002.03049.x. [DOI] [PubMed] [Google Scholar]
- 4.Guillonneau B, el-Fettouh H, Baumert H, Cathelineau X, Doublet JD, Fromont G, et al. Laparoscopic radical prostatectomy: oncological evaluation after 1,000 cases a Montsouris Institute. J Urol. 2003;169:1261–1266. doi: 10.1097/01.ju.0000055141.36916.be. [DOI] [PubMed] [Google Scholar]
- 5.Salomon L, Anastasiadis AG, Katz R, De La Taille A, Saint F, Vordos D, et al. Urinary continence and erectile function: a prospective evaluation of functional results after radical laparoscopic prostatectomy. Eur Urol. 2002;42:338–343. doi: 10.1016/s0302-2838(02)00360-3. [DOI] [PubMed] [Google Scholar]
- 6.Peyromaure M, Ravery V, Boccon-Gibod L. The management of stress urinary incontinence after radical prostatectomy. BJU Int. 2002;90:155–161. doi: 10.1046/j.1464-410x.2002.02824.x. [DOI] [PubMed] [Google Scholar]
- 7.Burnett AL, Mostwin JL. In situ anatomical study of the male urethral sphincteric complex: relevance to continence preservation following major pelvic surgery. J Urol. 1998;160:1301–1306. [PubMed] [Google Scholar]
- 8.Rocco F, Carmignani L, Acquati P, Gadda F, Dell'Orto P, Rocco B, et al. Restoration of posterior aspect of rhabdosphincter shortens continence time after radical retropubic prostatectomy. J Urol. 2006;175:2201–2206. doi: 10.1016/S0022-5347(06)00262-X. [DOI] [PubMed] [Google Scholar]
- 9.Rocco B, Gregori A, Stener S, Santoro L, Bozzola A, Galli S, et al. Posterior reconstruction of the rhabdosphincter allows a rapid recovery of continence after transperitoneal videolaparoscopic radical prostatectomy. Eur Urol. 2007;51:996–1003. doi: 10.1016/j.eururo.2006.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Duthie JB, Pickford JE, Gilling PJ. Robot-assisted laparoscopic prostatectomy: a 2010 update. N Z Med J. 2010;123:30–34. [PubMed] [Google Scholar]
- 11.Rebuck DA, Haywood S, McDermott K, Perry KT, Nadler RB. What is the long-term relevance of clinically detected postoperative anastomotic urine leakage after robotic-assisted laparoscopic prostatectomy. BJU Int. 2011;108:733–738. doi: 10.1111/j.1464-410X.2010.09939.x. [DOI] [PubMed] [Google Scholar]
- 12.Asimakopoulos AD, Annino F, D'Orazio A, Pereira CF, Mugnier C, Hoepffner JL, et al. Complete periprostatic anatomy preservation during robot-assisted laparoscopic radical prostatectomy (RALP): the new pubovesical complex-sparing technique. Eur Urol. 2010;58:407–417. doi: 10.1016/j.eururo.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 13.Jeong W, Araki M, Park SY, Lee YH, Kumon H, Hong SJ, Rha KH. Robot-assisted laparoscopic radical prostatectomy in the Asian population: modified port configuration and ultradissection. Int J Urol. 2010;17:297–300. doi: 10.1111/j.1442-2042.2010.02480.x. [DOI] [PubMed] [Google Scholar]