Abstract
Objective
This article describes the method and intake findings of the Brown Longitudinal Obsessive Compulsive Study, the first comprehensive prospective investigation of the naturalistic course of obsessive-compulsive disorder (OCD) in a large clinical sample using longitudinal research methodology.
Method
Intake data, collected between June 2001 and October 2004, are presented for 293 adult participants in a prospective, naturalistic study of OCD. Participants had a primary diagnosis of DSM-IV OCD and had sought treatment for the disorder.
Results
Our findings indicate that OCD typically has a gradual onset and a continuous course regardless of age at onset. There is a substantial lag between the onset of the disorder and initiation of treatment. OCD, which almost always coexists with other psychiatric symptoms, leads to serious social and occupational impairment. Compared with participants with late-onset OCD, early-onset participants had higher rates of lifetime panic disorder, eating disorders, and obsessive-compulsive personality disorder. The groups also differed on the types of obsessive-compulsive symptoms that were first noticed, as well as on rates of current obsessions and compulsions.
Conclusion
The demographics, clinical characteristics, comorbidity rates, and symptom presentation of the sample are consistent with those reported for cross-sectional studies of OCD, including the DSM-IV Field Trial. The current sample has a number of advantages over previously collected prospective samples of OCD in that it is large, diagnostically well characterized, recruited from multiple settings, and treatment seeking. This unique data set will contribute to the identification of meaningful phenotypes in OCD based on stability of symptom dimensions, prospective course patterns, and treatment response.
Obsessive-compulsive disorder (OCD) is a neuropsychiatric condition characterized by recurrent, intrusive thoughts (obsessions) and repetitive behaviors that the individual feels driven to perform (compulsions). Obsessions and compulsions can cause significant functional impairment. In fact, the World Health Organization characterizes OCD as among the 10 most disabling of all medical and psychiatric conditions in the industrialized world.1
In spite of increased recognition of the public health significance of OCD over the last decade, surprisingly little is known about the long-term course and prognosis of this disorder. Long-term, prospective, observational studies, using sound longitudinal designs, for other major anxiety disorders, the mood disorders, eating disorders, and personality disorders have contributed valuable new information regarding prognosis, patterns of remission and relapse, the factors that affect these patterns, and the underutilization of effective treatments. Previous prospective studies of OCD2–7 have been hampered by at least 1 of the following methodological limitations: lack of standardized longitudinal measures, small sample sizes limiting power for course analyses, limited study duration, the stringent inclusion criteria of clinical trials (e.g., excluding participants with comorbid major depression), and a lack of consensus on definitions of relapse, remission, and recovery. A careful and systematic prospective study of symptom course and outcome over time in OCD, using validated longitudinal measures and a large sample, would be an important step toward advancing our knowledge of the prognosis and predictors of course in this common and often disabling disorder.
The Brown Longitudinal Obsessive Compulsive Study (BLOCS) is the first comprehensive study to prospectively investigate the naturalistic course and outcome of OCD in a large clinical sample, using a methodology of longitudinal research successfully employed in other large, naturalistic follow-up studies.8,9 The specific aims of the project are to: (1) comprehensively describe the long-term patterns of course of OCD; (2) identify clinically meaningful predictors of remission and relapse; (3) prospectively describe the amount of psychiatric treatment received; and (4) assess the relationship between psychosocial function, quality of life, and obsessive-compulsive symptom severity over the follow-up period. Progress in each of these content areas will not only provide new information about course of illness in OCD and longitudinal aspects of treatment but will also help refine data supporting the existence of homogeneous subtypes in OCD.
This article describes the method and intake findings of the BLOCS, including sample demographics, clinical characteristics, comorbidities, and symptom presentation. In addition, adults with early-onset OCD (EOCD) were compared with those with late-onset OCD (LOCD) on each of the intake study variables. Results of recent investigations suggest that patients with EOCD have a more severe clinical presentation (more chronic course, poorer treatment response)6,10–12 and are more likely to have family members affected by OCD than those with LOCD.13,14 Differences between these age at onset categories suggest a potential distinct subtype of the disorder with prepubertal onset.
We predicted that our sample’s demographics, clinical characteristics, comorbidity rates, and symptom presentation would be consistent with those reported for cross-sectional studies of OCD such as the DSM-IV Field Trial.15 We also hypothesized that the EOCD group would have higher rates of tic disorders and family history of OCD.
METHOD
Participants
Subjects were the first 293 consecutive adult participants in an ongoing, 5-year, National Institute of Mental Health–funded, naturalistic follow-up study of the course of OCD, recruited between June 2001 and October 2004. This report includes data from the intake assessment only. Inclusion criteria were age 19 or older, a primary diagnosis of DSM-IV OCD (defined as the disorder that participants considered their biggest problem overall across their lifetime), having sought treatment for OCD, and willingness to participate in annual interviews. While individuals with organic mental disorders and mental retardation were excluded from the study (N = 2), there were no exclusions for comorbid Axis I or II disorders. Participants were recruited from psychiatric treatment settings, including consecutive admissions to an outpatient OCD specialty clinic, inpatient units of a private psychiatric hospital, community mental health centers, 2 general outpatient psychiatric clinics, and the private practices of 3 experts in cognitive-behavioral therapy for OCD. Seventy-nine percent of those screened met the inclusion criteria and were enrolled in the study.
Eighty-one percent of the sample currently met full DSM-IV criteria for OCD. The remaining 19% had met full OCD criteria in the past: 17% were in partial remission (symptoms consume less than 1 hour per day; mild distress and/or functional impairment), and 2% were in full remission (no distress or functional impairment). At the time of the intake interview, 91% of the sample was participating in outpatient treatment, 4% were inpatient, and 5% were not in treatment.
Procedures
The study was approved by the institutional review boards of Brown University and Butler Hospital, and all subjects signed statements of informed consent prior to enrollment. The participants were compensated $25 for participating in the intake interview.
Participants were interviewed in person by trained research assistants and completed a semistructured clinical interview, rater-administered assessments, and self-report questionnaires. Narrative summary reports describing psychiatric symptoms were prepared for all participants, and DSM-IV diagnoses were assigned. Each case was presented to experts in OCD (M.C.M. and J.L.E.) at a weekly conference to review diagnoses and psychosocial impairment and to ensure ongoing consistency in ratings. Prior to data entry, interview data were reviewed by senior staff members for clinical and clerical accuracy.
Measures
The Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Version (SCID-I/P)16 and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II)17 were used at intake. The SCID-I/P is a semistructured, rater-administered interview designed to diagnose DSM-IV psychiatric disorders, including mood disorders, psychotic disorders, substance use disorders, anxiety disorders, somatoform disorders, and eating disorders. Additional SCID-like modules based on DSM-IV criteria were included to assess the rates of tic disorders, impulse-control disorders, and childhood disorders. The SCID-II is a structured interview for personality disorders described on DSM-IV Axis II.
The Butler Hospital OCD Database, a semistructured, rater-administered questionnaire, was used to collect detailed information on participant demographics and clinical features of OCD. Participants were asked to recall information such as ages at onset of minor (subclinical) and major symptoms, age at first received treatment, retrospective assessment of course of illness, and psychiatric treatments received. This instrument has been used in previous phenomenological studies at this site.18–20
OCD symptom severity was assessed with the Yale-Brown Obsessive Compulsive Scale (YBOCS).21 The YBOCS is a reliable and valid 10-item rater-administered measure of current severity of obsessions and compulsions. The scale is widely accepted as the major outcome measure for OCD. Higher scores on the YBOCS indicate greater severity, with total scores ranging from 0 to 40. Prior to the YBOCS, interviewers administered the YBOCS Symptom Checklist (YBOCS-SC) to gather information on specific current symptoms. The YBOCS-SC comprises 15 separate categories of obsessions and compulsions. (Since the aggressive obsession category contains items that refer to both a fear of aggressive impulses [e.g., “I have violent or horrific images in my mind”] and pathological doubt [e.g., “I fear that I’ll harm others because I’m not careful enough”], this category will be presented as 2 subcategories: aggressive obsessions and pathological doubt.)
The delusionality of OCD-related beliefs was evaluated with the rater-administered Brown Assessment of Beliefs Scale (BABS),22 both dimensionally (higher scores indicate a greater degree of delusionality) and categorically, based on empirically derived cutoff points for both “poor insight” and “delusional.” Scores range from 0 to 24. The rater-administered Modified Hamilton Rating Scale for Depression,23 a modified version of the widely accepted Hamilton Rating Scale for Depression (HAM-D),24 assessed current severity of depressive symptoms. The validity of the Modified HAM-D has been established by comparing it with the original HAM-D.23 We used the 25-item scoring method. Family history of OCD in first-degree relatives (probable diagnoses) was obtained by asking participants if any of their relatives have/had similar problems and by rephrasing the SCID questions for OCD.
The current psychosocial functioning of participants was quantified using 2 interviewer-rated DSM-IV-TR Axis V 100-point scales, the Global Assessment of Functioning (GAF),25 and the Social and Occupational Functioning Assessment Scale (SOFAS).25 The GAF is used to rate overall psychological, social, and occupational functioning, excluding physical and environmental impairment. The SOFAS assesses an individual’s level of social and occupational functioning not directly influenced by the overall severity of psychiatric symptoms.
Interviewer Training
All interviewers had at least a bachelor’s degree and were trained to reliability. Prior to the inception of subject enrollment, the interviewers attended training sessions for each of the study instruments. The interviewers viewed and rated sample tapes, and discrepancies between raters were discussed. In addition, the interviewers rated several live mock participants, observed by a psychologist, and again, discrepancies among raters were discussed for each interview. After didactic training, new raters observed more experienced SCID interviewers. A psychologist and SCID trainer then observed the first 5 interviews of newly trained raters in order to provide feedback. These initial interviews were audiotaped to allow for interrater reliability ratings. Prior to the independent administration of study instruments, newly trained interviewers were required to demonstrate a high degree of interrater reliability with both trainers and other raters (intraclass correlation coefficients > .85 for YBOCS total score and SCID diagnoses). As indicated earlier, the consistency of ongoing ratings was assured through both the presentation of diagnostic and impairment data to OCD experts at weekly conferences and the review of all collected interview data by senior staff members prior to data entry. In an effort to minimize interviewer drift, interrater reliability exercises were also performed periodically on a random sample of taped interviews.
Data Analysis
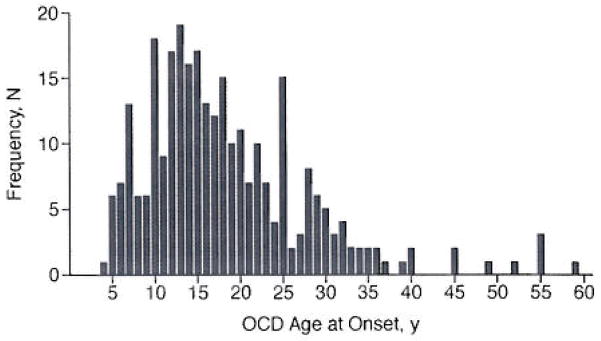
Means, standard deviations, percentages, and frequencies were calculated to describe demographics, comorbidity rates, and clinical symptoms. EOCD subjects were compared with LOCD subjects on study variables. Like previous studies,11,26,27 age at onset was defined as the age at which a participant’s obsessions and/or compulsions began to cause clinically significant distress or impairment. We did not define onset by the age at which minor obsessive-compulsive symptoms were first experienced12,28 because of the high prevalence of subclinical obsessive-compulsive symptoms in the general public that do not develop into clinical symptoms. The distribution of ages at onset for the overall sample is presented in Figure 1. Although the distribution is positively skewed (mean = 18.49 years; median = 16.00 years; mode = 13.00 years), age 18 was used as the cutoff point between EOCD and LOCD as in previous studies of age at onset.10,26,29 Besides being generally accepted as the onset age of adulthood, an age of 18 years is considered a threshold for strong familial aggregation of OCD13,14 and is a hypothesized marker for different etiologic variants of the disorder. Between-group differences for the EOCD versus LOCD cases were explored using χ2 analysis for categorical variables and analysis of variance for continuous variables. All tests were 2-tailed; an α level of .05 determined statistical significance. Due to risk of type I error with multiple post hoc comparisons, Bonferroni correction was applied when testing for differences between EOCD and LOCD groups on each of the YBOCS-SC categories. Statistical analyses were performed using SAS statistical software version 8e for Windows (SAS, Cary, N.C.).
Figure 1.
Distribution of Ages at Onset of OCD for Overall Sample (N = 293)
Abbreviation: OCD = obsessive-compulsive disorder.
RESULTS
Aside from the expected differences in symptom severity (YBOCS, Modified HAM-D, BABS) and functioning (GAF, SOFAS) measures, the 238 participants in episode did not differ from the 55 out of episode on demographics, lifetime comorbidity, or OCD age at onset. In addition, when the sample was divided by recruitment site, there were no differences on any of these variables, with the exception of inpatients, who reported poorer functioning on the GAF and SOFAS, as would be expected. As a result, analyses were performed on the entire sample (N = 293).
Regarding demographic features, the sample is predominantly white (96%) and 55% female. Forty-six percent of the participants are college-educated, and 44% are married (36% never married). Forty-one percent of the sample was unemployed at the time of the intake interview, with 27% unable to work due to psychopathology and 14% receiving disability benefits largely due to OCD. Means and standard deviations for intake clinical characteristics arc presented in Table 1. On average, individuals in the sample first received treatment more than 17 years after initially experiencing obsessive-compulsive symptoms and 11 years after meeting diagnostic criteria for OCD. Eighty-one percent of the sample reported a gradual onset (≥ 3 months) of major obsessive-compulsive symptoms, and 17% reported a sudden onset (≤ 1 month). Regarding the overall course of symptoms, 67% rated the course as continuous (with mild variation in intensity of symptoms but with no remission), 23% as waxing and waning (with periods of at least 3 months’ duration of only subclinical symptoms), 8% as episodic (with periods of complete remission of 3 months or more), and 2% as deteriorative (OCD continues to worsen even with treatment). Thirty-one percent of subjects reported having at least 1 first-degree relative with a probable diagnosis of OCD.
Table 1.
Clinical Characteristics of Participants (N = 293)
| Characteristic | Mean | SD | Range |
|---|---|---|---|
| Age, y | |||
| At intake | 40.49 | 12.9 | 19–75 |
| First experienced minor symptoms | 12.36 | 8.2 | 3–60 |
| At onset of OCD | 18.49 | 9.9 | 4–62 |
| First received treatment | 29.86 | 11.9 | 8–69 |
| Duration of illness, y | 22.02 | 13.3 | 0–69 |
| Symptom severity scores at intake (possible score range) | Mean | SD | Actual Score Range |
|
|
|||
| YBOCS (0–40) | 20.26 | 8.4 | 0–37 |
| Modified HAM-D (0–72) | 10.48 | 9.0 | 0–39 |
| BABS (0–24) | 6.37 | 5.0 | 0–24 |
| GAF (0–100) | 52.17 | 12.0 | 18–90 |
| SOFAS (0–100) | 55.45 | 14.3 | 28–90 |
| OCD severity categories based on YBOCS (possible score range) | N | % | Actual Score Range |
|
|
|||
| Subclinical (0–7) | 24 | 8.2 | 0–7 |
| Mild (8–15) | 57 | 19.5 | 8–15 |
| Moderate (16–23) | 86 | 29.4 | 16–23 |
| Severe (24–31) | 109 | 37.2 | 24–31 |
| Extreme (32–40) | 17 | 5.8 | 32–37 |
Abbreviations: BABS = Brown Assessment of Beliefs Scale, GAF = Global Assessment of Functioning. Modified HAM-D = Modified Hamilton Rating Scale for Depression. OCD = obsessive-compulsive disorder, SOFAS = Social and Occupational Functioning Assessment Scale. YBOCS = Yale-Brown Obsessive Compulsive Scale.
The overall severity of current OCD on the YBOCS was in the moderate range, with the vast majority of participants scoring in the moderate and severe categories (see Table 1). Based on mean scores, the sample presented with mild depression on the Modified HAM-D and good insight on the BABS. Twelve percent of the participants at intake had poor insight with respect to their OCD-related beliefs; only 2% were delusional. Both the GAF and SOFAS mean scores demonstrated serious impairment in social and occupational functioning. While 52% of the sample reported a history of suicidal ideation, 15% noted at least 1 suicide attempt.
Tables 2 and 3 present the rates of lifetime and current comorbid Axis I disorders and the rates of comorbid Axis II disorders, respectively, in the overall sample. While 58% of the participants did not meet criteria for any other current Axis I condition besides OCD, 91% met lifetime criteria for at least 1 other Axis I disorder, with major depressive disorder (MDD), social phobia, alcohol abuse/dependence, panic disorder, and specific phobia as the most common comorbid conditions. Thirty-eight percent met criteria for at least 1 Axis II disorder. Obsessive-compulsive personality disorder (OCPD) and avoidant personality disorder were the most common comorbid personality disorders in this sample.
Table 2.
Lifetime and Current Comorbidity of DSM-IV Axis I Disorders in Participants With Primary OCD (N = 293)
| DSM-IV Diagnosis | Lifetime
|
Current
|
||
|---|---|---|---|---|
| N | % | N | % | |
| OCD only | 27 | 9.2 | 170 | 58.0 |
| Any mood disordera | 217 | 74.1 | 48 | 16.4 |
| Major depressive disorder | 197 | 67.2 | 44 | 15.0 |
| Bipolar disorder | 8 | 2.7 | 2 | 0.7 |
| Dysthymia | 23 | 7.8 | 0 | 0.0 |
| Depressive disorder NOS | 4 | 1.4 | 2 | 0.7 |
| Any psychotic disorder | 8 | 2.7 | 6 | 2.0 |
| Any anxiety disordera | 154 | 52.6 | 111 | 38.0 |
| Panic disorder | 54 | 18.4 | 21 | 7.2 |
| Agoraphobia without panic disorder | 4 | 1.4 | 4 | 1.4 |
| Social phobia | 81 | 27.6 | 55 | 18.8 |
| Specific phobia | 53 | 18.1 | 43 | 14.7 |
| Posttraumatic stress disorder | 19 | 6.5 | 10 | 3.4 |
| Generalized anxiety disorder | 22 | 7.5 | 22 | 7.5 |
| Any substance use disordera | 75 | 25.6 | 17 | 5.8 |
| Alcohol abuse/dependence | 68 | 23.2 | 13 | 4.4 |
| Drug abuse/dependence | 39 | 13.3 | 4 | 1.4 |
| Any eating disordera | 30 | 10.2 | 5 | 1.7 |
| Anorexia nervosa | 9 | 3.1 | 0 | 0.0 |
| Bulimia nervosa | 9 | 3.1 | 3 | 1.0 |
| Binge eating disorder | 4 | 1.4 | 1 | 0.3 |
| Eating disorder NOS | 9 | 3.1 | 1 | 0.3 |
| Any somatoform disorder | 22 | 7.5 | 18 | 6.1 |
| Hypochondriasis | 4 | 1.4 | 3 | 1.0 |
| Body dysmorphic disorder | 18 | 6.1 | 15 | 5.1 |
| Any tic disorderb | 41 | 14.0 | 16 | 5.5 |
| Attention-deficit/hyperactivity disorder | 30 | 10.2 | 8 | 2.7 |
| Separation anxiety disorder | 22 | 7.5 | 0 | 0.0 |
| Any impulse-control disorderc | 44 | 15.0 | 33 | 11.3 |
The total is less than the sum of the individual disorders because some subjects had more than 1 disorder in a given category.
Includes DSM-IV and DSM-III-R diagnoses of Tourette’s disorder, chronic motor or vocal tic disorder, transient tic disorder, and tic disorder NOS.
Includes nail biting, skin picking, trichotillomania, pathological gambling, pyromania, and kleptomania.
Abbreviations: NOS = not otherwise specified, OCD = obsessive-compulsive disorder.
Table 3.
Comorbidity of DSM-IV Axis II Disorders in Participants With Primary OCD (N = 288)a
| Personality Disorder | N | % |
|---|---|---|
| Obsessive-compulsive | 71 | 24.7 |
| Avoidant | 44 | 15.3 |
| Borderline | 18 | 6.3 |
| Depressive | 10 | 3.5 |
| Paranoid | 5 | 1.7 |
| Schizotypal | 3 | 1.0 |
| Antisocial | 3 | 1.0 |
| Dependent | 3 | 1.0 |
| Schizoid | 2 | 0.7 |
| Passive-aggressive | 2 | 0.7 |
| Histrionic | 2 | 0.7 |
| Narcissistic | 0 | 0.0 |
Data were missing from 5 subjects.
Abbreviation: OCD = obsessive-compulsive disorder.
Participants were asked to identify the first minor (subclinical) obsessive-compulsive symptom (obsession or compulsion) that they noticed. Approximately 53% of respondents identified an obsession as their first symptom, with the rest reporting a compulsion first. Table 4 lists frequencies for the first minor symptoms noticed according to YBOCS-SC category. The table also includes the percentage of subjects for each YBOCS-SC category for whom the first minor symptom noticed was also the current principal symptom (defined as the single obsession and compulsion that they “would most like to get rid of”) at the intake interview. Symmetry obsessions, contamination obsessions, miscellaneous compulsions, and checking compulsions were the most common minor symptoms. Aggressive obsessions and hoarding obsessions and compulsions were the most enduring symptoms. That is, of those who named an aggressive obsession as their first noticed symptom, 62% identified this type of symptom as their current principal obsession, and 75% of participants who named hoarding obsessions or compulsions as their first symptom also reported this as their current principal obsessive-compulsive symptom.
Table 4.
Frequency of First Minor Symptom Noticed (by YBOCS-SC category) and Overlap With Current Principal Obsession or Compulsiona
| YBOCS-SC Category | First Minor Symptom
|
First Minor Symptom Is the Current Principal Obsession or Compulsionb |
||
|---|---|---|---|---|
| N | % | N | % | |
| Obsessions (N = 132)c | ||||
| Aggressive (any) | 25 | 18.9 | 19 | 76.0 |
| Aggressive | 13 | 9.8 | 8 | 61.5 |
| Pathological doubt | 12 | 9.1 | 6 | 50.0 |
| Contamination | 30 | 22.7 | 17 | 56.7 |
| Sexual | 2 | 1.5 | 1 | 50.0 |
| Hoarding | 8 | 6.1 | 6 | 75.0 |
| Religious | 15 | 11.4 | 8 | 53.3 |
| Symmetry | 34 | 25.8 | 14 | 41.2 |
| Somatic | 7 | 5.3 | 4 | 57.1 |
| Miscellaneous | 11 | 8.3 | 5 | 45.5 |
| Compulsions (N = 119)d | ||||
| Cleaning | 19 | 16.0 | 7 | 36.8 |
| Checking | 25 | 21.0 | 10 | 40.0 |
| Repeating | 21 | 17.6 | 7 | 33.3 |
| Counting | 5 | 4.2 | 0 | 0.0 |
| Ordering | 19 | 16.0 | 7 | 36.8 |
| Hoarding | 4 | 3.4 | 3 | 75.0 |
| Miscellaneous | 26 | 21.8 | 9 | 34.6 |
N = 251. Data were missing from 42 subjects. Participants were asked to name the first minor (subclinical) obsessive-compulsive symptom (obsession or compulsion) that they noticed.
Defined as the single obsession or compulsion that the participant “would most like to get rid of.” Percentages are based on frequency of corresponding first noticed symptom.
132 participants (52.6% of respondents) reported an obsession as the first minor symptom noticed. Percentages are based on N = 132.
119 participants (47.4% of respondents) reported a compulsion as the first minor symptom noticed. Percentages are based on N = 119.
Abbreviation: YBOCS-SC = Yale-Brown Obsessive Compulsive Scale Symptom Checklist.
Most participants reported multiple current obsessions and compulsions on the YBOCS-SC. Participants endorsed symptoms in a mean ± SD 3.29 ± 1.7 out of 8 possible obsession categories and in 3.43 ± 1.8 out of 7 possible compulsion categories. Table 5 lists the frequencies of current obsessions and compulsions by YBOCS-SC category (based on having any symptoms in a particular category). Among the obsession categories, contamination, particularly the concern with dirt or germs and fear of illness due to contamination, was most frequently endorsed. Next were the miscellaneous obsessions, namely thoughts about lucky and unlucky numbers and the fear of losing things. This was followed by the aggressive obsessions subcategory pathological doubt, which includes the fear of being responsible for a disaster. Regarding compulsions, the most frequently endorsed category was checking, particularly checking that one did not make a mistake and checking some aspect of one’s body, followed by cleaning, especially excessive handwashing, and the miscellaneous compulsions, including mental rituals (such as compulsive prayer, mental arithmetic, and reviewing) and the need to tell, ask, or confess.
Table 5.
Frequency of Current Obsessions and Compulsions by YBOCS-SC Category
| YBOCS-SC Category | Overall Sample (N = 293)
|
EOCD (N = 159)
|
LOCD (N = 134)
|
χ2 | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Obsessions | |||||||
| Aggressive (any) | 208 | 71.0 | 125 | 78.6 | 83 | 61.9 | 9.82* |
| Aggressive | 133 | 45.4 | 86 | 54.1 | 47 | 35.1 | 10.61* |
| Pathological doubt | 164 | 56.0 | 97 | 61.0 | 67 | 50.0 | 3.58 |
| Contamination | 169 | 57.7 | 99 | 62.3 | 70 | 52.2 | 2.99 |
| Sexual | 39 | 13.3 | 26 | 16.4 | 13 | 9.7 | 2.79 |
| Hoarding | 86 | 29.4 | 52 | 32.7 | 34 | 25.4 | 1.89 |
| Religious | 77 | 26.3 | 53 | 33.3 | 24 | 17.9 | 8.93* |
| Symmetry | 140 | 47.8 | 79 | 49.7 | 61 | 45.5 | 0.51 |
| Somatic | 77 | 26.3 | 47 | 29.6 | 30 | 22.4 | 1.93 |
| Miscellaneous | 167 | 57.0 | 102 | 64.2 | 65 | 48.5 | 7.26 |
| Compulsions | |||||||
| Cleaning | 176 | 60.1 | 100 | 62.9 | 76 | 56.7 | 1.16 |
| Checking | 202 | 68.9 | 120 | 75.5 | 82 | 61.2 | 6.92 |
| Repeating | 165 | 56.3 | 103 | 64.8 | 62 | 46.3 | 10.13* |
| Counting | 76 | 25.9 | 45 | 28.3 | 31 | 23.1 | 1.01 |
| Ordering | 127 | 43.3 | 70 | 44.0 | 57 | 42.5 | 0.07 |
| Hoarding | 83 | 28.3 | 51 | 32.1 | 32 | 23.9 | 2.41 |
| Miscellaneous | 176 | 60.1 | 109 | 68.6 | 67 | 50.0 | 10.44* |
p < .003 (with Bonferroni correction: .05/17).
Abbreviations: EOCD = early-onset OCD (age at onset < 18 years), LOCD = late-onset OCD (age at onset ≥ 18 years), OCD = obsessive-compulsive disorder, YBOCS-SC = Yale-Brown Obsessive Compulsive Scale Symptom Checklist.
Early-Onset OCD vs. Late-Onset OCD
Mean ± SD age at onset for the EOCD group (age at onset < 18 years) (N = 159) was 11.81 ± 3.5 years versus 26.64 ± 9.1 years for the LOCD group (age at onset ≥ 18 years) (N = 134). The age at onset groups did not differ on any demographic variables (gender, race, marital status, education, employment) other than age at interview. The LOCD group (43.7 ± 12.1 years) was older at intake compared with the EOCD group (37.9 ± 13.0 years), F = 15.08, df = 1.289; p < .001.
With regard to clinical data, the EOCD and LOCD groups did not differ in how they rated the onset of major obsessive-compulsive symptoms (sudden vs. gradual) and the overall course of symptoms. When analyses were restricted to participants currently in episode for OCD, it was found that OCD severity, depression symptoms, level of insight, global functioning, social and occupational functioning, and the number of participants currently disabled due to OCD did not differ between the 2 age at onset groups. Significantly more subjects in the EOCD group (36% vs. 26%, χ2 = 3.78, df = 1, p = .050) reported having at least 1 first-degree relative with a probable diagnosis of OCD.
In terms of lifetime comorbidity, there were significantly higher rates of panic disorder in the EOCD group compared with the LOCD group (22% vs. 13%, χ2 = 4.38, df = 1, p = .036). Rates of any eating disorder were also significantly higher in the EOCD group (14% vs. 5%, χ2 = 6.35, df = 1, p= .012). The groups did not differ in the rates of any other comorbid Axis I disorder. On Axis II, the groups differed on the rates of comorbid OCPD, with the EOCD group showing significantly higher rates than the LOCD group (32% vs. 16%, χ2 = 9.82, df = 1, p = .002).
While the groups did not differ in the first minor obsession noticed, they differed in the first minor compulsion noticed, χ2 = 14.35, df = 6, p = .026. The EOCD group was more likely to report repeating rituals, ordering compulsions, and miscellaneous compulsions as the first compulsions experienced. Meanwhile, the LOCD group was more likely to report hoarding as the first compulsion experienced.
Regarding rates of current symptoms on the YBOCS-SC, as noted in Table 5, the EOCD group was significantly more likely than the LOCD group to report aggressive obsessions, religious obsessions, repeating compulsions, and miscellaneous compulsions (after Bonferroni correction). We used current symptoms so that EOCD versus LOCD comparisons would not be confounded by duration of illness. In fact, there was no correlation between duration of illness and either the number of current obsession categories (r = .03, df = 291, p = .601) or current compulsion categories (r = .01, df = 291, p = .826) endorsed on the YBOCS-SC.
DISCUSSION
The BLOCS is the first long-term, comprehensive, prospective study of OCD with validated, longitudinal measures. This report presents the study’s intake findings. Based on the report of participants ascertained as adults, OCD typically has a gradual onset and a continuous course regardless of age at onset. There is a substantial lag between the onset of the disorder and initiation of treatment. Obsessive-compulsive disorder, which almost always coexists with other psychiatric symptoms, leads to serious social and occupational impairment.
As predicted, the demographics, clinical features, and symptom presentation of this sample are consistent with those of samples in previous cross-sectional studies of OCD as well as other studies on OCD phenomenology, indicating that participants in the BLOCS are representative of a typical clinical sample of OCD. Specifically, the mean age at intake, higher percentage of women, low rates of minorities, and mean YBOCS total score at intake were all comparable with those of the DSM-IV Field Trial.15 The distribution of obsessions and compulsions (by YBOCS-SC categories) in our sample strongly resembles that reported for 624 affected individuals in the OCD Collaborative Genetics Study.30 The percentage of participants who never married, the mean age at which treatment was first received, and the number of years between onset of symptoms and treatment mirrored those reported by Rasmussen and Tsuang.18 The mean age at onset of OCD, duration of illness, percentage of participants with a chronic course, and GAF scores were similar to those reported by Eisen and colleagues.2 In addition, our sample’s mean BABS score was akin to that of Ravi Kishore and colleagues,31 and the percentages of participants with poor insight32 and classified as delusional33 using the BABS corresponded to previous reports. The 14% of the current sample who reported receiving disability benefits due to OCD is consistent with community findings from the National Epidemiologic Catchment Area study34 in which 18% of individuals with OCD were receiving disability payments, a rate more than 4 times higher than for individuals without an Axis I diagnosis.
As predicted, the comorbidity rates of the BLOCS sample were in line with past research. In terms of lifetime Axis I comorbidity, only 9% of participants had OCD alone, suggesting that OCD rarely occurs in the absence of additional neuropsychiatric disorders. This percentage corresponds to a study of comorbidity in OCD by LaSalle and colleagues35 in which only 8% of 334 SCID-diagnosed participants had OCD alone. The very high rate of lifetime MDD in our sample (67%) is particularly noteworthy and very likely accounts for the report of suicidal ideation in half the sample, with attempted suicide in 15%. Our study’s lifetime Axis I comorbidity rates were strongly consistent with those of LaSalle et al.,35 with the exception of surprisingly low rates in the BLOCS sample of dysthymia, agoraphobia without panic disorder, generalized anxiety disorder (GAD), and eating disorders. However, our rates of lifetime dysthymia and GAD match those of Nestadt et al.36 and Antony et al.,37 respectively. In a study of 1078 cases of OCD diagnosed by general physician evaluation,38 rates of lifetime agoraphobia and eating disorders coincided with those reported here.
Our study reports a relatively low rate of lifetime bipolar disorder (3%) compared with recent studies. Hantouche et al.39 found a comorbidity rate of 11%, but this rate was based on self-ratings rather than a diagnostic interview. Perugi et al.40 reported a 56% lifetime rate of comorbid bipolar disorder, using structured interviews, in a sample with current DSM-IV OCD and MDD. It is possible that our inclusion criterion of primary OCD may account for our lower rate of OCD and bipolar disorder comorbidity.
In terms of current Axis I comorbidity, our rates were similar to those of Denys et al.41 and Eisen et al.2 Our rates of Axis II comorbidity were highly consistent with those of Samuels and colleagues,42 with OCPD and avoidant personality disorder as the most prevalent personality disorders by far.
Do adults with EOCD represent a distinct subgroup? In our comparisons of EOCD and LOCD participants in episode, the groups did not differ in terms of severity of OCD, level of insight, and functional impairment. Similar to Nestadt et al.13 and Pauls et al.,14 we found greater familial loading for OCD in the EOCD group. However, we measured family history for the disorder based on participant report rather than direct interview of relatives. This potential reporting bias may explain why our estimate of the likelihood of affected first-degree relatives was considerably lower than that reported in the family studies.
Tic disorders did not occur with greater frequency in the EOCD group than in the LOCD group, contrary to our hypothesis. This difference from previous reports12,28,43 is most likely due to the low frequency of tic disorders overall in our study. The inclusion of children and recruitment from child psychiatric settings in 2 of the studies28,43 quite likely contributed to substantially higher rates of tic disorders in those samples. Similarly, our rate of attention-deficit/hyperactivity disorder in the overall sample (10%) was low in comparison with the 30% reported in a literature review,44 yet the review was based on samples of juvenile OCD rather than patients ascertained as adults.
Several studies12,28,35,43 have reported more lifetime psychiatric comorbidity in participants with EOCD than in those with LOCD. In our sample, we found significantly higher rates of eating disorders, panic disorder, and OCPD in the EOCD group. It should be noted that we had a relatively small number of participants with comorbid eating disorders, so this finding may not be reliable. While it is not clear why panic disorder would be more prevalent in the EOCD group, a high rate of panic disorder in EOCD subjects (41%) was also found in a family study of OCD,45 although an LOCD comparison group was not used. It should be noted that the comorbidity in this family study may have been due to ascertainment bias, since all of the probands had participated in a double-blind, placebo-controlled medication trial. In a long-term, follow-up study of 55 individuals with OCD that had its onset in childhood or adolescence,46 26% of the sample met criteria for OCPD using the SCID-II when interviewed 11 years (mean follow-up) later. Although this study also did not have an LOCD comparison group, the data suggest a possible association between EOCD and OCPD in later life.
The EOCD group reported significantly higher rates of current symptoms than the LOCD group in the following categories: aggressive obsessions, religious obsessions, repeating rituals, and miscellaneous compulsions. The greater prevalence of “taboo” obsessions in the EOCD group, such as aggressive and religious obsessions, around puberty suggests that the hormonal and psychological changes associated with this developmental phase may be involved in their pathogenesis. In a previous study,12 early-onset subjects were more likely than late-onset subjects to report hoarding, repeating compulsions, and miscellaneous compulsions on the YBOCS-SC. Millet et al.43 reported a higher frequency of hoarding among early-onset subjects, although these data were collected using questionnaires instead of clinical interviews. The rates of aggressive, sexual, and contamination obsessions in our EOCD sample mirrored those reported for a small sample of EOCD probands in a family study.47
The BLOCS data set will allow for prospective exploration of important questions concerning course and treatment. The current sample has a number of advantages over previous prospective samples in that it is large (N = 293), diagnostically well characterized (with OCD being the primary diagnosis of participants), recruited from multiple settings, and treatment seeking (to allow for research on treatment response over time). Another major advantage of the BLOCS over previous studies is the use of a reliable and valid semistructured instrument designed specifically for the collection of longitudinal data. The Longitudinal Interval Follow-up Evaluation (LIFE)48,49 was administered at all follow-up timepoints to collect detailed information on symptomatic status, diagnostic status, and behavioral and pharmacologic treatment received. As part of the LIFE, psychiatric status ratings (PSRs),48 were assigned at follow-up visits to each of a participant’s diagnoses for each week since the previous visit. These PSRs are then used to identify patterns of remission and relapse over time. With this methodology, we will also explore how ongoing comorbid symptomatology affects the course of OCD.
In future studies using the BLOCS sample, we will explore approaches to identifying meaningful phenotypes in OCD based on stability of symptom dimensions, prospective course patterns, and treatment response. This work can potentially lead to better understanding of the relationship between specific symptom patterns in the disorder and neurobiological correlates.
There are several limitations to this study. Despite our attempts to gather a representative clinical sample of OCD, the generalizability of the results is limited by the fact that individuals self-selected to participate in the research study and by the small number of minority participants enrolled. The findings also cannot extend to non–treatment-seeking cases in the community. Data on age at onset, and thus comparisons between early- and late-onset groups, and retrospective descriptions of the course of symptoms were limited by participant recall. In addition, as stated, family history of OCD was not obtained from direct family interviews but instead was based on participants’ perceptions of relatives.
Additional research on OCD’s clinical features is needed in community populations to better understand the presentation of the disorder in nonclinical settings. Special attention to the vastly understudied area of course and outcome of OCD in minority subjects is needed. Since the literature on early course patterns of pediatric OCD is scant, longitudinal study of children is also strongly recommended, as this would allow for more accurate documentation and corroboration of onset age and initial symptoms.
Acknowledgments
Supported by a grant (R01 MH060218) to Dr. Rasmussen from the National Institute of Mental Health, Bethesda, Md.
Footnotes
The authors report no additional financial or other relationships relevant to the subject of this article.
References
- 1.Murray CJ, Lopez AD. The Global Burden of Disease. Boston, Mass: Harvard University Press; 1996. [Google Scholar]
- 2.Eisen JL, Goodman WK, Keller MB, et al. Patterns of remission and relapse in obsessive-compulsive disorder: a 2-year prospective study. J Clin Psychiatry. 1999;60:346–351. doi: 10.4088/jcp.v60n0514. [DOI] [PubMed] [Google Scholar]
- 3.Leonard HL, Swedo SE, Lenane MC, et al. A 2- to 7-year follow-up study of 54 obsessive-compulsive children and adolescents. Arch Gen Psychiatry. 1993;50:429–439. doi: 10.1001/archpsyc.1993.01820180023003. [DOI] [PubMed] [Google Scholar]
- 4.Orloff LM, Battle MA, Baer L, et al. Long-term follow-up of 85 patients with obsessive-compulsive disorder. Am J Psychiatry. 1994;151:441–442. doi: 10.1176/ajp.151.3.441. [DOI] [PubMed] [Google Scholar]
- 5.Ravizza L, Barzega G, Bellino S, et al. Drug treatment of obsessive-compulsive disorder (OCD): long-term trial with clomipramine and selective serotonin reuptake inhibitors (SSRIs) Psychopharmacol Bull. 1996;32:167–173. [PubMed] [Google Scholar]
- 6.Skoog G, Skoog I. A 40-year follow-up of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56:121–127. doi: 10.1001/archpsyc.56.2.121. [DOI] [PubMed] [Google Scholar]
- 7.Steketee G, Eisen J, Dyck I, et al. Predictors of course in obsessive-compulsive disorder. Psychiatry Res. 1999;89:229–238. doi: 10.1016/s0165-1781(99)00104-3. [DOI] [PubMed] [Google Scholar]
- 8.Keller MB, Lavori PW, Mueller TI, et al. Time to recovery, chronicity, and levels of psychopathology in major depression: a 5-year prospective follow-up of 431 subjects. Arch Gen Psychiatry. 1992;49:809–816. doi: 10.1001/archpsyc.1992.01820100053010. [DOI] [PubMed] [Google Scholar]
- 9.Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. Am J Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- 10.Albert U, Picco C, Maina G, et al. Phenomenology of patients with early and adult onset obsessive-compulsive disorder [in Italian] Epidemiol Psichiatr Soc. 2002;11:116–126. doi: 10.1017/s1121189x00005571. [DOI] [PubMed] [Google Scholar]
- 11.Fontenelle LF, Mendlowicz MV, Marques C, et al. Early- and late-onset obsessive-compulsive disorder in adult patients: an exploratory clinical and therapeutic study. J Psychiatr Res. 2003;37:127–133. doi: 10.1016/s0022-3956(02)00087-0. [DOI] [PubMed] [Google Scholar]
- 12.Rosario-Campos MC, Leckman JF, Mercadante MT, et al. Adults with early-onset obsessive-compulsive disorder. Am J Psychiatry. 2001;158:1899–1903. doi: 10.1176/appi.ajp.158.11.1899. [DOI] [PubMed] [Google Scholar]
- 13.Nestadt G, Samuels J, Riddle M, et al. A family study of obsessive-compulsive disorder. Arch Gen Psychiatry. 2000;57:358–363. doi: 10.1001/archpsyc.57.4.358. [DOI] [PubMed] [Google Scholar]
- 14.Pauls DL, Alsobrook JP, Goodman W, et al. A family study of obsessive-compulsive disorder. Am J Psychiatry. 1995;152:76–84. doi: 10.1176/ajp.152.1.76. [DOI] [PubMed] [Google Scholar]
- 15.Foa EB, Kozak MJ, Goodman WK, et al. DSM-IV field trial: obsessive-compulsive disorder. Am J Psychiatry. 1995;152:90–96. doi: 10.1176/ajp.152.1.90. [DOI] [PubMed] [Google Scholar]
- 16.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I/P, version 2.0) New York, NY: Biometrics Research, New York State Psychiatric Institute; 1996. [Google Scholar]
- 17.First MB, Gibbon M, Spitzer RL, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 18.Rasmussen SA, Tsuang MT. Clinical characteristics and family history in DSM-III obsessive-compulsive disorder. Am J Psychiatry. 1986;143:317–322. doi: 10.1176/ajp.143.3.317. [DOI] [PubMed] [Google Scholar]
- 19.Rasmussen SA, Eisen JL. Clinical features and phenomenology of obsessive compulsive disorder. Psychiatr Ann. 1989;19:67–73. [Google Scholar]
- 20.Rasmussen SA, Eisen JL. The epidemiology and differential diagnosis of obsessive compulsive disorder. J Clin Psychiatry. 1994;55:5–10. [PubMed] [Google Scholar]
- 21.Goodman WK, Price LH, Rasmussen SA, et al. The Yale Brown Obsessive Compulsive Scale, 1: development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 22.Eisen JL, Phillips KA, Baer L, et al. The Brown Assessment of Beliefs Scale: reliability and validity. Am J Psychiatry. 1998;155:102–108. doi: 10.1176/ajp.155.1.102. [DOI] [PubMed] [Google Scholar]
- 23.Miller IW, Bishop S, Norman WH, et al. The Modified Hamilton Rating Scale for Depression: reliability and validity. Psychiatry Res. 1985;14:131–142. doi: 10.1016/0165-1781(85)90057-5. [DOI] [PubMed] [Google Scholar]
- 24.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 26.Sobin C, Blundell ML, Karayiorgou M. Phenotypic differences in early- and late-onset obsessive-compulsive disorder. Compr Psychiatry. 2000;41:373–379. doi: 10.1053/comp.2000.9009. [DOI] [PubMed] [Google Scholar]
- 27.Sobin C, Blundell M, Weiller F, et al. Phenotypic characteristics of obsessive-compulsive disorder ascertained in adulthood. J Psychiatr Res. 1999;33:265–273. doi: 10.1016/s0022-3956(98)00061-2. [DOI] [PubMed] [Google Scholar]
- 28.Diniz JB, Rosario-Campos MC, Shavitt RG, et al. Impact of age at onset and duration of illness on the expression of comorbidities in obsessive-compulsive disorder. J Clin Psychiatry. 2004;65:22–27. doi: 10.4088/jcp.v65n0104. [DOI] [PubMed] [Google Scholar]
- 29.Fyer AJ, Lipsitz JD, Mannuzza S, et al. A direct interview family study of obsessive-compulsive disorder, 1. Psychol Med. 2005;35:1611–1621. doi: 10.1017/S0033291705005441. [DOI] [PubMed] [Google Scholar]
- 30.Samuels JF, Riddle MA, Greenberg BD, et al. Am J Med Genetics, Pan B:Neuropsychiatric Genetics. Vol. 141. The OCD Collaborative Genetics Study: methods and sample description; pp. 201–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ravi Kishore V, Samar R, Janardhan Reddy YC, et al. Clinical characteristics and treatment response in poor and good insight obsessive-compulsive disorder. Eur Psychiatry. 2004;19:202–208. doi: 10.1016/j.eurpsy.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 32.Eisen JL, Rasmussen SA, Phillips KA, et al. Insight and treatment outcome in obsessive-compulsive disorder. Compr Psychiatry. 2001;42:494–497. doi: 10.1053/comp.2001.27898. [DOI] [PubMed] [Google Scholar]
- 33.Eisen JL, Phillips KA, Coles ME, et al. Insight in obsessive compulsive disorder and body dysmorphic disorder. Compr Psychiatry. 2004;45:10–15. doi: 10.1016/j.comppsych.2003.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leon AC, Portera L, Weissman MM. The social costs of anxiety disorders. Br J Psychiatry. 1995;166:19–22. [PubMed] [Google Scholar]
- 35.LaSalle VH, Cromer KR, Nelson KN, et al. Diagnostic interview assessed neuropsychiatric disorder comorbidity in 334 individuals with obsessive-compulsive disorder. Depress Anxiety. 2004;19:163–173. doi: 10.1002/da.20009. [DOI] [PubMed] [Google Scholar]
- 36.Nestadt G, Samuels J, Riddle MA, et al. The relationship between obsessive-compulsive disorder and anxiety and affective disorders: results from the Johns Hopkins OCD Family Study. Psychol Med. 2001;31:481–487. doi: 10.1017/s0033291701003579. [DOI] [PubMed] [Google Scholar]
- 37.Antony M, Downie F, Swinson R. Diagnostic issues and epidemiology in obsessive-compulsive disorder. In: Swinson R, Antony M, Rachman S, et al., editors. Obsessive-Compulsive Disorder: Theory, Research, and Treatment. New York, NY: Guilford Press; 1998. pp. 3–32. [Google Scholar]
- 38.Fireman B, Koran LM, Leventhal JL, et al. The prevalence of clinically recognized obsessive-compulsive disorder in a large health maintenance organization. Am J Psychiatry. 2001;158:1904–1910. doi: 10.1176/appi.ajp.158.11.1904. [DOI] [PubMed] [Google Scholar]
- 39.Hantouche EG, Angst J, Demonfaucon C, et al. Cyclothymic OCD: a distinct form? J Affect Disord. 2003;75:1–10. doi: 10.1016/s0165-0327(02)00461-5. [DOI] [PubMed] [Google Scholar]
- 40.Perugi G, Toni C, Frare F, et al. Obsessive-compulsive-bipolar comorbidity: a systematic exploration of clinical features and treatment outcome. J Clin Psychiatry. 2002;63:1129–1134. [PubMed] [Google Scholar]
- 41.Denys D, Tenney N, van Megen HJ, et al. Axis I and II comorbidity in a large sample of patients with obsessive-compulsive disorder. J Affect Disord. 2004;80:155–162. doi: 10.1016/S0165-0327(03)00056-9. [DOI] [PubMed] [Google Scholar]
- 42.Samuels J, Nestadt G, Bienvenu OJ, et al. Personality disorders and normal personality dimensions in obsessive-compulsive disorder. Br J Psychiatry. 2000;177:457–462. doi: 10.1192/bjp.177.5.457. [DOI] [PubMed] [Google Scholar]
- 43.Millet B, Kochman F, Gallarda T, et al. Phenomenological and comorbid features associated in obsessive-compulsive disorder: influence of age of onset. J Affect Disord. 2004;79:241–246. doi: 10.1016/S0165-0327(02)00351-8. [DOI] [PubMed] [Google Scholar]
- 44.Geller DA, Biederman J, Griffin S, et al. Comorbidity of juvenile obsessive-compulsive disorder with disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 1996;35:1637–1646. doi: 10.1097/00004583-199612000-00016. [DOI] [PubMed] [Google Scholar]
- 45.Carter AS, Pollock RA, Suvak MK, et al. Anxiety and major depression comorbidity in a family study of obsessive-compulsive disorder. Depress Anxiety. 2004;20:165–174. doi: 10.1002/da.20042. [DOI] [PubMed] [Google Scholar]
- 46.Wewetzer C, Jans T, Muller B, et al. Long-term outcome and prognosis of obsessive-compulsive disorder with onset in childhood or adolescence. Eur Child Adolesc Psychiatry. 2001;10:37–46. doi: 10.1007/s007870170045. [DOI] [PubMed] [Google Scholar]
- 47.Eapen V, Robertson MM, Alsobrook JP, II, et al. Obsessive compulsive symptoms in Gilles de la Tourette syndrome and obsessive compulsive disorder: differences by diagnosis and family history. Am J Med Genet. 1997;74:432–438. doi: 10.1002/(sici)1096-8628(19970725)74:4<432::aid-ajmg15>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 48.Keller MB, Lavori PW, Friedman B, et al. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 49.Warshaw MG, Keller MB, Stout RL. Reliability and validity of the Longitudinal Interval Follow-Up Evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]