Abstract
This study examined diagnostic predictors of prospectively observed suicide attempts in a personality disorder (PD) sample. During 2 years of follow-up, 58 participants (9%) reported at least 1 definitive suicide attempt. Predictors that were examined include 4 PD diagnoses and selected Axis I diagnoses (baseline and course). Multivariate logistic regression analyses indicated that baseline borderline personality disorder (BPD) and drug use disorders significantly predicted prospective suicide attempts. Controlling for baseline BPD diagnosis, proportional hazards analyses showed that worsening in the course of major depressive disorder (MDD) and of substance use disorders in the month preceding the attempt were also significant predictors. Therefore, among individuals diagnosed with PDs, exacerbation of Axis I conditions, particularly MDD and substance use, heightens risk for a suicide attempt.
Personality disorders (PDs) and Axis I disorders, particularly borderline personality disorder (BPD) and major depressive disorder (MDD), have long been established as risk factors for suicidal behavior (e.g., Friedman, Aronoff, Clarkin, Corn, & Hurt, 1983; McGlashan, 1986). However, because the base rates of suicide and suicide attempts are relatively low compared to the base rates of these disorders, diagnoses in and of themselves are of limited use in predicting suicidal events. Furthermore, it is not always clear whether improvement or deterioration of a psychiatric condition (particularly MDD) is the greater risk factor for suicidal behavior. Therefore, alternative means of investigating the predictive utility of psychiatric disorders, such as identifying high-risk combinations of co-occurring Axis I and Axis II disorders, or examining specific changes in the course of a disorder prior to a suicide event, may be more effective.
In reviewing suicide research, various types of suicide behaviors need to be distinguished, particularly because each type of behavior is associated with different risk factors. Generally accepted classifications of suicide behavior include completed suicide, suicide attempt, and suicide ideation (Beck, Beck, & Kovacs, 1975; O’Carroll et al., 1996). The consistent findings that men are at greater risk for suicide completion and women are at greater risk for suicide attempt(s) (Hirschfeld & Davidson, 1988) highlight the importance of identifying risk factors specific to the behavior. Nonetheless, because history of past suicide attempt(s) is one of the greater risk factors for suicide completion, research on suicide attempts inevitably informs clinical judgment with regard to suicide completion (e.g., Goldstein, Black, Nasrallah, & Winokur, 1991; Roy, 1982). Furthermore, the distinction between suicide attempts and suicide gestures (or parasuicide) has been advocated on the basis of differing intent to die. Specifically, those who make a suicide gesture (or parasuicide) do not intend to die but do aim either to draw attention through their actions, or to regulate their emotions (Kemperman, Russ, & Shearin, 1997), and have arguably different associated risk factors (Schneidman, 1985).
Several studies have examined risk factors for completed suicide among high-risk populations (e.g., psychiatric inpatient samples). McGlashan’s (1986) Chestnut Lodge study in which BPD patients were monitored for a mean of 15 years and Stone’s (1989) New York State Psychiatric Institute study in which BPD were monitored for a mean of 16 years found higher rates of suicide among BPD patients with co-occurring major depression. A recent 20-year prospective study found both PDs and MDD were unique significant risk factors for eventual suicide (Brown, Beck, Steer & Grisham, 2000). However, one 15-year follow-up study failed to find any difference in prevalence rates of affective disorders between BPD patients who committed suicide and nonsuicidal BPD controls (Paris, Nowlis, & Brown, 1989). Similarly, Kullgren (1988) found that rates of MDD did not differ between BPD patients who committed suicide and BPD inpatients who did not commit suicide within a month after discharge. Therefore, it remains uncertain as to whether MDD is an immediate or lifetime risk for suicide, and whether it remains a risk factor within the context of BPD.
Similarly, the question of whether co-occurrent BPD/MDD increases one’s risk for suicide attempts beyond the effect of each of these disorders independently, has also been debated. In a prospective follow-up of patients with BPD, other PDs, and no PD, those with BPD continued to be more suicidal 2 to 5 years later, despite no significant differences in rates of mood disorders (Mehlum, Friis, Vaglum, & Karterud, 1994). Among a large sample of patients with panic disorder who were monitored for 5 years, BPD and MDD were both significant risk factors for suicide behavior (Warshaw, Dolan, & Keller, 2000). Retrospective studies have generally found that patients with co-occurring MDD/BPD are more likely to have a history of suicide attempts than those with MDD only, or MDD with another personality disorder (Corbitt, Malone, Haas, & Mann, 1996; Kelly, Soloff, Lynch, Haas, & Mann, 2000). However, in a study of BPD patients, depressed mood, but not co-occurring affective disorder, was found to be associated with a history of suicidal behavior (Soloff, Lis, Kelly, Cornelius, & Ulrich, 1994). These results suggest that severity of depressed mood, as assessed subjectively and on a continuum, may be a better predictor of suicide behavior than the MDD diagnosis. Further efforts are necessary, particularly prospective studies, to determine whether MDD remains a significant risk factor when comorbid with BPD, and whether alternative ways of assessing depression may be more useful in predicting suicide attempts.
Other Axis I disorders have also been the focus of investigative efforts to identify risk factors for suicide attempts. These include studies of schizophrenia (Young, et al., 1998), panic disorder (e.g., Korn, Plutchik, & Van Praag, 1997), posttraumatic stress disorder (PTSD; e.g., Kessler, Borges, & Walters, 1999), and substance use disorders (e.g., O’Boyle & Brandon, 1998). However, for the most part, these disorders are examined independent of PD diagnoses.
Numerous studies have examined presence of Axis I disorders as predictors of suicide attempts, but have yielded inconsistent findings. No study, to the best of our knowledge, has examined course of Axis I disorders as predictors of suicide attempts. The examination of Axis I disorders (selected on the basis of empirically supported associations with suicidal behaviors) as dynamic variables would represent an innovative approach to approximating clinical presentations. We are specifically interested in worsening of Axis I conditions for its clinical relevancy; that is, patients are more likely to seek treatment when their conditions worsen rather than improve. Finally, our examination of these variables in a PD sample allows us to focus on a group that is at particularly high risk for suicidal behaviors.
This investigation examines prospective, longitudinal data in which suicide behaviors, Axis I symptomatology, and PD features were assessed at specified follow-up intervals, as part of a larger study examining the course of four PDs (including BPD). Our design allowed the advantage of examining immediate precipitants and the change in status of a particular Axis I disorder (as opposed to presence or absence of diagnosis) at the time of the suicide attempt. Furthermore, unlike many other studies of suicidal behavior, this sample was not restricted to inpatients or those who were admitted for a previous suicide attempt, but was recruited from a variety of treatment settings. Our first aim was to examine whether the diagnoses frequently associated with suicide behavior (i.e., BPD, MDD, panic disorder, PTSD, and substance use disorders) emerged as significant unique risk factors for suicide attempts. We predicted that these disorders at baseline would be associated with an increased likelihood of a suicide attempt during the 2-year follow-up. Our second aim examined whether worsening in the course of MDD, PTSD, substance use disorders (SUD), and panic disorder, would be a significant predictor for suicide attempts. We predicted that changes in these disorders would predict a suicide attempt.
Method
The Collaborative Longitudinal Personality Disorders Study (CLPS) is a multisite, naturalistic, prospective study of four PD groups: schizotypal (STPD), borderline (BPD), avoidant (AVPD), obsessive–compulsive (OCPD), and a comparison group of MDD without PD. The overall aims, design, assessment methodology, and demographic characteristics of the sample are detailed elsewhere (Gunderson et al., 2000). Following is an overview of the study participants and assessment procedures relevant to the investigation here.
Participants
Participants between the ages of 18 and 45 were recruited from treatment clinics affiliated with the four CLPS sites. Additional individuals who had been in current or past treatment were recruited from fliers and advertisements. Individuals with acute substance intoxication or withdrawal, active psychosis, an IQ of 85 or less, cognitive impairment, or a history of schizophrenia, schizophreniform, or schizoaffective disorders were excluded from participation on the basis of questionable ability to provide detailed and accurate information. Individuals were eligible to participate if they met diagnostic criteria as assessed by the Diagnostic Interview for DSM–IV Personality Disorders (DIPD–IV; Zanarini, Frankenburg, Sickel, & Yong, 1996) for at least one of the four personality disorders targeted in the CLPS (STPD, BPD, AVPD, OCPD), or if they met criteria for the comparison group, MDD as assessed by the Structured Clinical Interview for DSM–IV Axis I Disorders–patient version (SCID–I/P; First, Spitzer, Gibbon, & Williams, 1996) without PD. The DIPD–IV was the primary assessment of PD. However, to maximize accuracy of PD diagnoses, interviewers’ DIPD–IV diagnoses had to receive convergent support from one other method of Axis II assessment, either the self-report Schedule for Adaptive and Nonadaptive Personality (SNAP; Clark, 1993) or the clinician-rated personality assessment form (PAF; Shea, Glass, Pilkonis, Watkins, & Docherty, 1987). Interviewers had master’s or doctoral level training (or equivalent clinical experience) in a mental health related discipline. Each participant signed an informed consent, approved by the institutional review boards at their respective sites or institutions.
The total CLPS study group consisted of 668 participants who were interviewed at 6 months, 1 year, and 2 years following the baseline assessment. The 6-month and 1-year interviews each covered 6 months of follow-up, and the 2-year interview covered 1 year of follow-up. The examination here will focus only on the 621 participants (93% of sample) with at least 12 months of follow-up data (baseline, 6-month, and 1-year interviews). The majority of the sample, 578 participants (86.5% of sample) had 2 years of follow-up data at the time of analyses.
Measures
DIPD–IV
This semistructured interview consists of questions that assess each criterion of the 10 Diagnostic and Statistical Manual of Mental Disorders (DSM–IV; American Psychiatric Association, 1994) personality disorders. In this study, interrater and test–retest reliability of the DIPD–IV (kappa) for the four study PDs were .68 and .69 for BPD, .68 and .73 for AVPD, and .71 and .74 for OCPD, respectively. The interrater reliability sample was insufficient to calculate kappa for STPD; the test–retest kappa for STPD was .64 (Zanarini et al., 2000).
SCID-I/P
The SCID–I/P is a semistructured interview with demonstrated reliability used to diagnose major Axis I disorders as defined by the DSM–IV. In the CLPS, reliability of SCID–I/P diagnoses ranged from .57 to 1.00 depending on the disorder, with a median kappa of .76. Test–retest reliability ranged from .35 to .78, with a median kappa of .64. Interrater reliability kappa and test–retest kappa for specific Axis I disorders can be found in Zanarini et al. (2000). For the Axis I disorders examined here, the interrater reliability kappa and test–retest kappa are .80 and .61 for MDD, 1.0 and .77 for alcohol use disorder, 1.0 and .76 for drug use disorder, .65 and .65 for panic disorder, and .88 and .78 for PTSD, respectively.
Longitudinal Interval Follow-Up Evaluation
LIFE (Keller et al., 1987) is a semistructured interview rating system with demonstrated reliability for assessing the longitudinal course of psychiatric disorders and functioning including suicidal behaviors. Using information obtained from the interview, weekly psychiatric status ratings (PSRs) are made for each Axis I disorder present. In this study, PSRs for most disorders are based on a 3-point scale, indicating whether the individual meets full criteria (PSR3), is in partial remission (PSR2), or is in full remission from the given disorder (PSR1). Because MDD was among the central interests of study, it was rated on a 6-point scale (full criteria = PSR6, PSR5, partial remission = PSR4, PSR3, full remission = PSR2, PSR1) to allow finer distinctions within categories. Good to excellent interrater and test–retest reliabilities have been established for several Axis I disorders using a different sample in another longitudinal, naturalistic study with a similar assessment protocol (Warshaw, Dyck, Allsworth, Stout, & Keller, 2001; Warshaw, Keller, & Stout, 1994).
For suicidal behavior, number of attempts and gestures are recorded on a monthly basis. Detailed ratings of intent (categories include obviously no intent, only minimal intent, definite but very ambivalent, serious, very serious, and extreme) and medical threat (categories include no danger, minimal, mild, moderate, severe, and extreme) are made.
Data analyses
For the purposes of this study, suicide attempters were distinguished from gesturers on the basis of their LIFE ratings for suicide intent and medical threat. Participants who had at least “definite, but ambivalent” intent and whose attempts were rated to have at least a “mild effect” (medically) were included in the suicide attempt group. For the 15 participants with multiple attempts during the follow-up interval, only the first attempt was examined in analyses. Data from those who made suicidal gestures only (no or minimal intent, and no or minimal danger) were analyzed with nonattempters.1
To identify baseline diagnostic predictors of suicide attempt group, logistic regression analyses using model-building strategies recommended by Hosmer and Lemeshow (2000) were conducted. Because sex and past history of self-injurious behaviors are both empirically established and consistent risk factors for suicide attempts (Goldstein et al., 1991), these variables were entered as covariates after significant univariate predictors and a best-fitting model were identified.
Cox (1972) proportional hazards regression analyses using weekly PSR scores for the five selected Axis I disorders were conducted to determine whether change in Axis I symptomatology in the month preceding the first suicide attempt of the follow-up interval was a significant predictor of the attempt. Because PSR scores in the month preceding the attempts were examined, attempts made during the first month of the follow-up interval were not analyzable. Analyses with each Axis I disorder were limited to those participants who met criteria for that disorder either at baseline or at any time during the follow-up interval. Cox proportional hazards regression allows for the use of all available data, including censored observations (i.e., data from participants who did not make a suicide attempt) during the 2-year follow-up interval. Proportional hazard regression models were performed with sex, BPD, and the self-injurious behavior (SIB) criterion of BPD as covariates.
Results
Of the 621 participants who had at least 1 year of follow-up data,2 96 (15.5%) reported some suicidal behavior. Of those, 58 (9.3% of the follow-up sample) reported behaviors that met our criteria for suicide attempt, as defined by level of intent and medical threat. The mean age at intake was 33 (SD = 8.4) for suicide attempters and 32.8 (SD = 8.1) for nonattempters. The majority of suicide attempters were Caucasian (77.6%), female (77.6%), not married or living with a partner at intake (81%), not employed at time of intake (70.7%), and had at least some college education (69%). The only significant demographic difference between suicide attempters and nonattempters was sex, χ2(1, N = 621) = 5.2, p = .02. A higher proportion of women in our sample had suicide attempts (11.3%) than the proportion of men in our sample (5.8%). Among nonattempters, 76.8% were Caucasian, 62.4% were women, 74.5% were not married or living with a partner at intake, 59% were not employed at intake, and 74.5% had some college education.
Baseline Diagnoses
Table 1 shows numbers and percentages of participants in the attempt and nonattempt groups by selected diagnoses. Because participants had co-occurring disorders, the sum of participants across the diagnostic groups exceeded the sample size. Forty percent of our sample had more than one of the four study PDs. Among the five Axis I disorders examined here, 31% of our sample were diagnosed with more than one disorder. Detailed information on comorbidity rates in the overall sample is available in McGlashan et al. (2000).
Table 1.
Baseline Diagnoses as Univariate Predictors of Suicide Attempt Group
| Predictor (n/%) | SA (n = 58) n (%) |
No SA (n = 563) n (%) |
β | SE (β) | Wald χ2 | Odds ratio | 95% CI |
|---|---|---|---|---|---|---|---|
| STPD (92/14.8%) | 6 (10.3) | 86 (15.3) | −0.45 | .45 | 1.00 | 0.64 | 0.30–2.02 |
| BPD (220/35.4%) | 45 (77.6) | 175 (31.1) | 2.04 | .33 | 38.66*** | 7.67 | 1.32–6.61 |
| AVPD (304/48.9%) | 31 (53.4) | 273 (48.5) | 0.20 | .28 | 0.52 | 1.22 | 0.55–1.84 |
| OCPD (248/39.9%) | 14 (24.1) | 234 (41.6) | −0.80 | .32 | 6.37* | 0.45 | 0.30–1.16 |
| MDD (287/46.2%) | 28 (48.3) | 259 (46.1) | 0.09 | .28 | 0.10 | 1.09 | 0.61–2.03 |
| Panic disorder (121/19.5%) | 13 (22.4) | 108 (19.2) | 0.19 | .33 | 0.34 | 1.21 | 0.33–1.50 |
| PTSD (132/21.3%) | 21 (36.2) | 111 (19.8) | 0.84 | .29 | 8.13** | 2.31 | 0.65–2.46 |
| Alcohol (74/11.9%) | 11 (19.0) | 63 (11.2) | 0.61 | .36 | 2.93 | 1.85 | 0.58–3.13 |
| Drug (76/12.2%) | 17 (29.3) | 59 (10.5) | 1.26 | .31 | 15.56*** | 3.53 | 1.08–4.68 |
| Sex: F (397/63.9%) | 45 (77.6) | 352 (62.5) | 0.66 | .38 | 2.99 | 1.93 | 0.92–4.09 |
| SIB (155/25%) | 39 (67.2) | 116 (20.6) | 2.07 | .30 | 47.99*** | 7.91 | 1.72–7.20 |
Note. SA = suicide attempt; CI = confidence interval; STPD = schizotypal PD; BPD = borderline PD; AVPD = avoidant PD; OCPD = obsessive–compulsive PD; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; Alcohol = alcohol abuse/dependence; Drug = drug abuse/dependence; SIB = history of self-injurious behavior.
p < .05.
p < .01.
p < .001.
A majority of those who attempted suicide met criteria for BPD (77.6%), and conversely, 20.5% of BPD participants had made a suicide attempt during the 2-year interval. In contrast, only 10.2% of AVPD, 6.5% of STPD, and 5.6% of OCPD participants attempted suicide during the follow-up interval. Among the Axis I disorders, in descending proportional order: 17 (22.4%) participants with a baseline diagnosis of drug use disorder attempted suicide; 21 (15.9%) participants with a baseline diagnosis of PTSD attempted suicide; 11 (14.9%) participants with a baseline diagnosis of alcohol use disorder attempted suicide; 13 (10.7%) participants with a baseline diagnosis of panic disorder; and 28 (9.8%) participants with a baseline diagnosis of MDD attempted suicide.
Also depicted in Table 1 are results from the univariate logistic regression analyses that examine each disorder as a predictor for suicide attempt group. Five baseline diagnoses were significant (p < .10) and were considered for inclusion in a multivariate model (Hosmer & Lemeshow, 2000): BPD, drug use disorder, PTSD, OCPD, and alcohol use disorder (in ascending p values). Because BPD was clearly the strongest predictor, all other predictors were individually added to a model with BPD to ascertain whether they were orthogonal or redundant predictors with BPD. Of these, only drug use disorder had a significant additive effect. Furthermore, there were no significant interaction effects. When all disorders were entered simultaneously to determine predictive utility while controlling for all other disorders in addition to the covariates of past self-injurious behavior and sex, only BPD and drug use disorder remained significant (see Table 2).
Table 2.
Multivariate Logistic Regression Analyses With All Significant Univariate Predictors and Covariates of Sex and Past History of Self-Injury
| Predictor | β | SE (β) | Wald χ2 | Odds ratio | 95% CI |
|---|---|---|---|---|---|
| BPD | 1.03 | .41 | 6.36** | 2.80 | 1.26–6.24 |
| OCPD | −0.55 | .34 | 2.61 | .58 | 0.30–1.12 |
| PTSD | 0.18 | .33 | 0.29 | 1.19 | 0.63–2.27 |
| Drug | 0.79 | .37 | 4.74* | 2.21 | 1.08–4.53 |
| Alcohol | 0.35 | .42 | 0.70 | 1.42 | 0.63–3.21 |
| Sex | 0.68 | .37 | 3.33 | 1.97 | 0.95–4.08 |
| SIB | 1.26 | .36 | 12.02*** | 3.54 | 1.73–7.24 |
Note. CI = confidence interval; BPD = borderline PD; OCPD = obsessive–compulsive PD; PTSD = posttraumatic stress disorder; Drug = drug abuse/dependence; Alcohol = alcohol abuse/dependence; SIB = history of self-injurious behavior.
p < .05.
p < .01.
p < .001.
Course of Axis I Disorders
Results of the proportional hazards regression analyses yielded risk ratios indicating that worsening of MDD (RR = 1.60, p < .001), alcohol use (RR = 1.74, p < .01), and drug use (RR = 2.11, p < .001) were significant predictors of suicide attempt (see Table 3). PTSD and panic disorder did not emerge as significant predictors of suicide attempt. BPD and the SIB criterion were significant covariates in each of the proportional hazard regression analyses.
Table 3.
Proportional Hazards Analyses Examining Course of Axis I Disorders as Predictors of Suicide Attempt
| n (SA) | n censored (No SA) | χ2 | Risk Ratio | 95% CI | |
|---|---|---|---|---|---|
| MDD | 40 | 441 | 18.68*** | 1.60 | 1.29–2.00 |
| Panic disorder | 17 | 148 | 0.63 | 0.78 | 0.35–1.74 |
| PTSD | 28 | 159 | 0.38 | 1.19 | 0.77–1.84 |
| Alcohol | 28 | 227 | 6.34** | 1.74 | 1.13–2.68 |
| Drug | 29 | 205 | 14.12*** | 2.11 | 1.43–3.12 |
Note. Borderline personality disorder (BPD) and self-injurious behavior (SIB) covaried in each analyses. Risk ratios for BPD ranged between 2.00–10.33; risk ratios for SIB ranged between 2.29–3.73.
SA = suicide attempt; CI = confidence interval; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; Alcohol = alcohol abuse/dependence; drug = drug abuse/dependence.
p < .01.
p < .001.
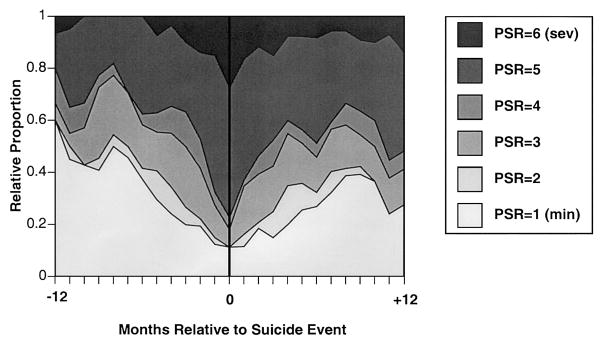
As an illustration, Figure 1 depicts PSR changes of MDD relative to the month of the suicide attempt. For participants who reported a suicide attempt and were monitored for MDD at any time during our follow-up interval, we designated the month of the attempt for that individual as Month 0. PSR ratings for MDD were then assembled relative to that time point, up to 12 months prior to the attempt and 12 months afterward. Figure 1 shows the proportion of PSRs at each level across the months before and after the suicide attempt. The depiction is group average data and does not necessarily represent the course of recovery for individual cases, but rather shows the general trends detected in the data by the proportional hazard regression analyses. MDD appears to worsen several months prior to the suicide attempt, but the worsening is the most dramatic in the month prior to the suicide attempt. There is an immediate improvement in MDD symptomalogy beginning in the month after the attempt and continuing for at least 6 months.
Figure 1.
Major depressive disorder psychiatric status rating (PSR) scores from PSR 1 (minimal) to PSR 6 (severe) in relation to month of suicide attempt.
Discussion
The main findings of this study were twofold: (a) baseline diagnoses of a drug use disorder and BPD were predictive of suicide attempts during the follow-up interval, and (b) worsening of depression and substance use was predictive of suicide attempts within the next month. Specifically, changes in the PSR scores for MDD, alcohol use disorder, and drug use disorder in the month preceding a suicide attempt were significant, relative to the general level of changes in all other months. Furthermore, the findings occur in the context of severe PD disturbance, even after taking into account other predictors of suicide attempt such as BPD and a past history of self-injurious behavior, which includes suicide attempts and gestures. This suggests that in addition to psychiatric diagnoses, proximate changes in the course of Axis I disorders may have important predictive utility.
Our findings that changes in SUDs and baseline diagnosis of a drug use disorder are associated with increased suicide risk is consistent with other empirical studies (e.g., Borges, Walters, & Kessler, 2000; Murphy, 1988). Contrary to hypothesis, baseline alcohol use disorder was not a significant predictor of suicide attempt group. One possible explanation for our finding is that the risk for suicide attempts associated with baseline alcohol use disorder was better accounted for by the other psychiatric disorders. In general, it is well supported that alcohol worsens the course of other psychiatric disorders, and thus may exert its influence as a risk factor indirectly.
With regard to baseline MDD, the lack of a significant finding is most likely attributed to the similarly high rates of baseline MDD among attempters (48.3%) and nonattempters (46.1%). Whereas the National Comorbidity Survey, which utilized a large community sample, reported a risk ratio of 12.9 for suicide attempts among participants with mood disorders (Kessler et al., 1999), the examination here is based on a high-risk, treatment-seeking population. Therefore, despite the lack of statistically significant differences in MDD between attempters and nonattempters in our sample, the high rate of baseline MDD (48%) and lifetime MDD (76%) among attempters remains striking and does not suggest that MDD lacks predictive or clinical utility. Rather, it suggests that in the presence of other psychiatric risk factors, a recent diagnosis of MDD does not appear to distinguish those who are likely to make a suicide attempt in a PD sample.
Panic disorder as a risk factor for suicide attempts has received inconsistent support in the literature, with the strongest evidence coming from earlier studies in which associated risk factors were not simultaneously examined (Johnson, Weissman, & Klerman, 1990; Weissman, Klerman, Markowitz, & Ouellette, 1989). Our lack of a significant finding with regard to panic disorder is consistent with more recent prospective studies (Brown et al., 2000; Warshaw et al., 2000), as well as reanalyses of the Epidemiologic Catchment Area (ECA) study in which panic disorder was not associated with an increased risk of suicide attempt after controlling for comorbid disorders (Hornig & McNally, 1995).
Our results also indicate that PTSD is not a significant predictor of suicide attempt after controlling for BPD. In the National Comorbidity Survey, individuals with PTSD were six times as likely as matched controls to attempt suicide, and PTSD had a stronger association with suicidality than any other anxiety disorder (Kessler et al., 1999). Many studies that implicated PTSD as a risk factor for suicide attempts did not assess for PDs (Kessler et al., 1999; Thompson et al., 1999). Because of the high rates of co-occurrence of these disorders, it is possible that much of the risk can be accounted for by BPD.
This is the first study to prospectively examine course of Axis I disorders as a risk factor for suicide attempts in the context of a PD sample. Our results have clinically relevant implications in that they suggest the consideration of both recent diagnosis of specific disorders and proximal course of specific disorders in determining one’s risk for a suicide attempt. The juxtaposition of the relative rarity of suicide attempts with the high frequency of individuals who present with severe and impairing psychiatric symptoms in medical and psychiatric settings, makes this a very difficult event to predict. However, given that most suicide victims do seek help from a health provider in the month preceding the suicide, it is essential to examine both lifetime as well as proximal risk factors (Vassilas & Morgan, 1993). In particular, our results highlight the importance of carefully monitoring symptoms of depression and substance use among high-risk individuals.
Whereas this study employed a prospective design, it necessarily relies on retrospective recall in which information was gathered on a 6-month or yearly basis. Therefore, it is quite possible that participants would recall the worsening of their Axis I symptoms to be concomitant with their suicide attempts. Furthermore, because interviewers are not blind as to whether the participant made a suicide attempt in that interval, it is possible that there could be biases in the probing of Axis I conditions. However, if a bias were to exist, it would be limited in scope because several of the investigated Axis I disorders were not found to be significant predictors in spite of their support in the literature. Furthermore, interviewers were unaware of the hypotheses of this study. An additional limitation of our study is the lack of reliability estimates for the suicide behavior assessment portion of the LIFE instrument. Finally, due to scoring rules of the LIFE, our data more accurately reflect suicide risk while in an Axis I episode, rather than changes in symptomatology (e.g., mild to moderate) when not in an episode.
This study focused exclusively on psychiatric disorders and course of disorders as risk factors for suicide attempts. Unfortunately, because of our exclusion criteria, we were not able to examine all Axis I disorders that have strong empirical associations with suicide, most notably schizophrenia and other psychotic disorders. Future investigations should integrate risk factors from various domains including demographic variables such as sex and marital status, recent life events (e.g., loss of employment, interpersonal loss), personality traits (e.g., social introversion, impulsivity), and past history (e.g., childhood sexual abuse, previous attempts). Accurate prediction of risk for suicide behavior will likely entail examining complex combinations of risk factors.
Acknowledgments
The Collaborative Longitudinal Personality Disorders Study is an ongoing, longitudinal, multisite, follow-along study of personality disorders that is funded by the National Institute of Mental Health. Award sites are Brown University Department of Psychiatry and Human Behavior, Providence, RI (MH-50837), Columbia University and New York State Psychiatric Institute, New York, NY (MH-50839), Harvard Medical School and McLean Hospital, Boston, MA (MH-50840), Texas A&M University, College Station, TX (MH-50838), Vanderbilt University, Nashville, TN (MH-50838), and Yale University School of Medicine, New Haven, CT (MH-50850). This work was further supported by NIMH K05 1654 to Thomas H. McGlashan.
Footnotes
Analyses were also conducted excluding data from the 37 participants who only reported suicide gestures; these results were consistent with the reported findings.
Using a Bonferroni-corrected p < .01, there were no demographic or baseline diagnostic differences between those who had at least 1 year of follow-up data by time of data analyses versus remaining others.
This article was approved by the publication committee of the Collaborative Longitudinal Personality Disorders Study, and was presented, in part, at the 2002 annual meeting of the American Psychiatric Association in Philadelphia.
Contributor Information
Shirley Yen, Department of Psychiatry and Human Behavior, Brown University.
M. Tracie Shea, Department of Psychiatry and Human Behavior, Brown University.
Maria Pagano, Department of Psychiatry and Human Behavior, Brown University.
Charles A. Sanislow, Department of Psychiatry, Yale University
Carlos M. Grilo, Department of Psychiatry, Yale University
Thomas H. McGlashan, Department of Psychiatry, Yale University
Andrew E. Skodol, Department of Psychiatry, New York State Psychiatric Institute and Columbia University
Donna S. Bender, Department of Psychiatry, New York State Psychiatric Institute and Columbia University
Mary C. Zanarini, Department of Psychiatry, McLean Hospital and Harvard Medical School
John G. Gunderson, Department of Psychiatry, McLean Hospital and Harvard Medical School
Leslie C. Morey, Department of Psychology, Texas A&M University
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Beck AT, Beck R, Kovacs M. Classification of suicidal behaviors: Quantifying intent and medical lethality. American Journal of Psychiatry. 1975;132:285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- Borges G, Walters EE, Kessler RC. Associations of substance use, abuse, and dependence with subsequent suicidal behavior. American Journal of Epidemiology. 2000;151:781–789. doi: 10.1093/oxfordjournals.aje.a010278. [DOI] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- Clark LA. Schedule for Nonadaptive and Adaptive Personality (SNAP) Minneapolis: University of Minnesota Press; 1993. [Google Scholar]
- Corbitt EM, Malone KM, Haas GL, Mann JJ. Suicidal behavior in patients with major depression and comorbid personality disorders. Journal of Affective Disorder. 1996;39:61–72. doi: 10.1016/0165-0327(96)00023-7. [DOI] [PubMed] [Google Scholar]
- Cox DR. Regression models and life tables. Journal of the Royal Statistical Society. 1972;34:187–220. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM–IV Axis I disorders—Patient version (SCID—I/P) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Friedman RC, Aronoff MS, Clarkin JF, Corn R, Hurt SW. History of suicidal behavior in depressed borderline inpatients. American Journal of Psychiatry. 1983;140:1023–1026. doi: 10.1176/ajp.140.8.1023. [DOI] [PubMed] [Google Scholar]
- Goldstein RB, Black DW, Nasrallah A, Winokur G. The prediction of suicide: Sensitivity, specificity, and predictive value of a multivariate model applied to suicide among 1,906 patients with affective disorders. Archives of General Psychiatry. 1991;48:418–422. doi: 10.1001/archpsyc.1991.01810290030004. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Shea MT, Skodol AE, McGlashan TH, Morey LC, Stout RL, et al. The Collaborative Longitudinal Personality Disorders study: Development, aims, design, and sample characteristics. Journal of Personality Disorders. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Davidson L. Clinical risk factors for suicide. Psychiatric Annals. 1988;18:628–635. [Google Scholar]
- Hornig CD, McNally RJ. Panic disorder and suicide attempt: A reanalysis of data from the Epidemiologic Catchment Area study. British Journal of Psychiatry. 1995;107:76–79. doi: 10.1192/bjp.167.1.76. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. 2. New York: Wiley; 2000. [Google Scholar]
- Johnson J, Weissman MM, Klerman GL. Panic disorder, comorbidity, and suicide attempts. Archives of General Psychiatry. 1990;47:805–808. doi: 10.1001/archpsyc.1990.01810210013002. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielson E, Endicott J, McDonald-Scott P, et al. The longitudinal interval follow-up evaluation. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kelly TM, Soloff PH, Lynch KG, Haas GL, Mann JJ. Recent life events, social adjustment, and suicide attempts in patients with major depression and borderline personality disorder. Journal of Personality Disorders. 2000;14:316–326. doi: 10.1521/pedi.2000.14.4.316. [DOI] [PubMed] [Google Scholar]
- Kemperman I, Russ MJ, Shearin E. Self-injurious behavior and mood regulation in borderline patients. Journal of Personality Disorders. 1997;11:146–157. doi: 10.1521/pedi.1997.11.2.146. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Borges B, Walters EE. Prevalence and risk factors of lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- Kjellander C, Bongar B, King A. Suicidality in borderline personality disorder. Crisis. 1998;19:125–135. doi: 10.1027/0227-5910.19.3.125. [DOI] [PubMed] [Google Scholar]
- Korn ML, Plutchik R, Van Praag HM. Panic-associated suicidal and aggressive ideation and behavior. Journal of Psychiatric Research. 1997;31:481–487. doi: 10.1016/s0022-3956(97)00019-8. [DOI] [PubMed] [Google Scholar]
- Kullgren G. Factors associated with completed suicide in borderline personality disorder. Journal of Nervous and Mental Disorders. 1988;176:40–44. doi: 10.1097/00005053-198801000-00005. [DOI] [PubMed] [Google Scholar]
- McGlashan TH. The Chestnut Lodge follow-up study: III. Long-term outcome of borderline personalities. Archives of General Psychiatry. 1986;43:2–30. doi: 10.1001/archpsyc.1986.01800010022003. [DOI] [PubMed] [Google Scholar]
- McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, et al. The Collaborative Longitudinal Personality Disorders study: Baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scandinavica. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- Mehlum L, Friis S, Vaglum P, Karterud S. The longitudinal pattern of suicidal behaviour in borderline personality disorder: A prospective follow-up study. Acta Psychiatrica Scandinavica. 1994;90:124–130. doi: 10.1111/j.1600-0447.1994.tb01567.x. [DOI] [PubMed] [Google Scholar]
- Murphy GE. Suicide and substance abuse. Archives of General Psychiatry. 1988;45:593–594. doi: 10.1001/archpsyc.1988.01800300091013. [DOI] [PubMed] [Google Scholar]
- O’Boyle M, Brandon EAA. Suicide attempts, substance abuse, and personality. Journal of Substance Abuse Treatment. 1998;15:353–356. doi: 10.1016/s0740-5472(97)00224-9. [DOI] [PubMed] [Google Scholar]
- O’Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, Silverman MM. Beyond the tower of Babel: A nomenclature for suicidology. Suicide and Life-Threatening Behavior. 1996;26:237–252. [PubMed] [Google Scholar]
- Paris J, Nowlis D, Brown R. Predictors of suicide in borderline personality disorder. Canadian Journal of Psychiatry. 1989;34:8–9. doi: 10.1177/070674378903400103. [DOI] [PubMed] [Google Scholar]
- Roy A. Risk factors for suicide in psychiatric patients. Archives of General Psychiatry. 1982;39:1089–1095. doi: 10.1001/archpsyc.1982.04290090071014. [DOI] [PubMed] [Google Scholar]
- Schneidman ES. Definitions of suicide. New York: Wiley; 1985. [Google Scholar]
- Shea MT, Glass DR, Pilkonis PA, Watkins J, Docherty JP. Frequency and implications of personality disorders in a sample of depressed inpatients. Journal of Personality Disorders. 1987;1:27–42. [Google Scholar]
- Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R. Risk factors for suicidal behavior in borderline personality disorder. American Journal of Psychiatry. 1994;151:1316–1323. doi: 10.1176/ajp.151.9.1316. [DOI] [PubMed] [Google Scholar]
- Stone MH. The course of borderline personality disorder. In: Tasman A, Hales RE, Frances AJ, editors. Annual review of psychiatry. Vol. 8. Washington, DC: American Psychiatric Press; 1989. pp. 103–122. [Google Scholar]
- Thompson MP, Kaslow NJ, Kingree JB, Puett R, Thompson NJ, Meadows L. Partner abuse and posttraumatic stress disorder as risk factors for suicide attempts in a sample of low-income, inner-city women. Journal of Traumatic Stress. 1999;12:59–72. doi: 10.1023/A:1024742215337. [DOI] [PubMed] [Google Scholar]
- Vassilas CA, Morgan HG. General practitioners’ contact with victims of suicide. British Medical Journal. 1993;307:300–301. doi: 10.1136/bmj.307.6899.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Dolan RT, Keller MB. Suicidal behavior in patients with current or past panic disorder: Five years of prospective data from the Harvard/Brown Anxiety Research program. American Journal of Psychiatry. 2000;157:1876–1878. doi: 10.1176/appi.ajp.157.11.1876. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: An ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. Journal of Psychiatric Research. 2001;35:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the Longitudinal Interval Follow-Up Evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Markowitz JS, Ouellette R. Suicidal ideation and suicide attempts in panic disorder and attacks. New England Journal of Medicine. 1989;321:1209–1214. doi: 10.1056/NEJM198911023211801. [DOI] [PubMed] [Google Scholar]
- Young AS, Nuechterlein KH, Mintz J, Ventura J, Gitlin M, Liberman RP. Suicide ideation and suicide attempts in recent-onset schizophrenia. Schizophrenia Bulletin. 1998;24:629–634. doi: 10.1093/oxfordjournals.schbul.a033354. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM–IV Personality Disorders (DIPD–IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, et al. The Collaborative Longitudinal Personality Disorders Study: Reliability of Axis I and II diagnoses. Journal of Personality Disorders. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]