Abstract
Attention-deficit/hyperactivity disorder (ADHD) has long been thought to reflect dysfunction of prefrontal-striatal circuitry, with involvement of other circuits largely ignored. Recent advances in systems neuroscience-based approaches to brain dysfunction enable the development of models of ADHD pathophysiology that encompass a number of different large-scale “resting state” networks. Here we review progress in delineating large-scale neural systems and illustrate their relevance to ADHD. We relate frontoparietal, dorsal attentional, motor, visual, and default networks to the ADHD functional and structural literature. Insights emerging from mapping intrinsic brain connectivity networks provide a potentially mechanistic framework for understanding aspects of ADHD, such as neuropsychological and behavioral inconsistency, and the possible role of primary visual cortex in attentional dysfunction in the disorder.
A systems neuroscience approach to ADHD
Attention-Deficit/Hyperactivity Disorder (ADHD), the most common neurodevelopmental disorder occurring in childhood, is characterized by developmentally excessive levels of inattention, impulsivity and hyperactivity [1]. The worldwide prevalence of ADHD has been estimated at 5.3% [2] although a national survey in the United States found parent-reported ADHD in 9.5% of school age children [3]. ADHD was once thought to be limited to childhood, but its continuation into adolescence and adulthood is no longer in doubt [4]. Yet, despite substantial economic impact and life-long psychosocial and psychiatric burden, ADHD remains among the most controversial of psychiatric diagnoses.
Based primarily on lesion studies in animals and humans, the imaging community initially embraced a prefrontal-striatal model of ADHD which expanded to include cerebellar involvement [5]. Prefrontal striatal circuits underpin executive function and dysfunction in such processes has long been considered an important neuropsychological correlate of ADHD [6]. This model has been largely supported by an ever-increasing number of structural and functional imaging studies [7,8], but divergent evidence such as involvement of occipital or temporal cortex [as noted by 9] has tended to be ignored, based on the initially reasonable assumption that unexpected results probably represent false positives. However, accumulating evidence suggests that the prefrontal-striatal model of ADHD should be extended to include other circuits and their interrelationships from the perspective of systems neuroscience [10,11]. We suggest that formulating a more inclusive brain model of ADHD is facilitated by the new paradigm of resting state functional magnetic resonance imaging (R-fMRI), which is increasingly revealing the intrinsic functional architecture of the brain [12]. Finally, we speculate that modulating neural networks through imaging-guided transcranial direct current electrical stimulation (tDCS) may provide novel therapeutic opportunities for disorders such as ADHD.
Resting state functional magnetic resonance imaging
Resting state functional imaging, i.e., imaging without a specific task (see Box 1), is not new. It dates from the earliest electroencephalography (EEG) and positron emission tomography studies [14]. What has only recently been appreciated is that large-scale neural systems exhibit synchronous intrinsic fluctuations at rates 10-100 times slower than the usual EEG frequencies [18]. These fluctuations persist during tasks, rest, wakefulness [18], sleep, or even anesthesia [19] and their correlations reflect the underlying connectivity of the brain's functional units. In other words, task-based imaging is no longer the only means of identifying neural networks because intrinsic relationships are continuously encoded in the spontaneous activity of the brain, and these can be most easily appreciated during rest [16,20]. The patterns formed by these relationships can be displayed as statistical maps that have the same appearance as task-evoked activation maps, but they do not represent the invariants associated with specific cognitions or behaviors [21]. Instead, they reflect correlations resulting from stochastic (i.e., probabilistic) neural activity transmitted differentially across synaptic connections that vary in strength based on the life experience of the individual [22].
Box 1. Mapping Intrinsic Functional Connectivity.
Functional magnetic resonance imaging (fMRI) without an explicit task, also known as resting state fMRI (R-fMRI), has facilitated delineating the intrinsic functional architecture of the brain based on the detection of patterns of coherence in low frequency (<0.1 Hz) spontaneous fluctuations in Blood Oxygenation Level Dependent (BOLD) signals [13,14]. Acquisition of R-fMRI data can be performed on any scanner capable of registering BOLD signals, as long as participants remain still and supine for upwards of five minutes, preferably with eyes open to minimize heterogeneity of arousal levels. The exploitation of R-fMRI has increased dramatically in recent years, driven by the wealth of information provided and by the ease of data collection across all clinical populations and throughout the entire lifespan. Although an ever increasing number of techniques are being developed to harness the voluminous information present in even brief records of R-fMRI data, the most commonly applied involve regression analyses of explicitly selected regions of interest (“seeds”), on the one hand, and data-driven independent component analyses (ICA) on the other [15]. These methods converge in detecting multiple large-scale neural systems, including the most frequently examined, the default network, that represent universal features of the adult brain architecture [16]. Resting state fMRI is reliable and reproducible, and the signals yielded are so robust as to allow aggregation of raw data across multiple scanners and populations even without prior coordination of data acquisition protocols [17]. This has advanced the goal of open sharing of primary data and analytical methods such as the 1000 Functional Connectomes Project (http://fcon_1000.projects.nitrc.org/) and the ADHD-200 Sample (http://fcon_1000.projects.nitrc.org/indi/adhd200/), and the Human Connectome Project http://www.humanconnectomeproject.org/.
The patterns of synchrony of these high-amplitude, albeit ultra-slow, fluctuations are extraordinarily robust across distinct populations, differences in scanner field strength, or scanning parameters [17], and are stable in test-retest designs [e.g., 23,24]. They have been validated in cross-species studies [19,25], in humans with electrocorticography [20], are exquisitely sensitive to age-factors during development [26] and to psychopathology [27]. Along with recent results applying resting state functional connectivity approaches to ADHD [28], these converging lines of evidence support our overarching hypothesis that ADHD results from dysregulated or aberrant interactions within and among large-scale neural systems.
Defining neural systems in the human brain
Neuronal connectivity can be defined at the microscale, i.e., in terms of single neurons, at the macroscale, the level of brain regions and their pathways, and at an intermediate level of minicolumns and their connection patterns [29]. Given currently available imaging methods and informatics capacity, the macroscale level is the most feasible for achieving a first draft of the human brain connectome [29] which is currently underway (http://www.humanconnectomeproject.org/).
Macroscale imaging based on the diffusion of water (diffusion tensor imaging) has begun to reveal the microstructure of major white matter tracts but is not yet capable of providing a comprehensive survey of brain networks. Classical lesion studies, which were the bases for identifying the systems underlying language, motor control and perception, have been updated with modern imaging methods and analytical techniques and continue to inform our understanding of neural systems [30].
Task-based functional imaging has also revealed many of the necessary elements of brain circuitry, but each individual contrast provides only a narrow-angle focus. When aggregated in meta-analyses, the results of thousands of such contrasts cumulatively delineate large-scale brain networks [16]. However, this objective is most efficiently achieved through R-fMRI, which captures the “full repertoire of functional networks utilized by the brain in action” [16]. Accordingly, R-fMRI methods have been used to identify the default network [31], the dorsal and ventral attentional networks [32], and motor, visual, and executive control systems [33] across labs [17] and clinical populations [27]. The remarkable replicability of neural networks in healthy young adults was recently demonstrated quantitatively in 1000 participants [12]. Those data were subdivided into a discovery set of 500 and a replication set of 500. Nearly all (97.4%) cortical vertices were assigned to the same seven cortical networks in the discovery and replication data sets. The parcellation of the human cerebral cortex based on all 1000 subjects is shown in Figure 1 and is freely available at (http://surfer.nmr.mgh.harvard.edu/fswiki/CorticalParcellation_Yeo2011). At this level of resolution, the seven major networks can be heuristically identified as sensorimotor and primary visual cortex, limbic, and dorsal attention, ventral attention, frontoparietal control and default networks. Although these are not the only relevant subdivisions of the cortex, they serve as reference networks that can be currently fruitfully examined in ADHD and other clinical conditions. As the field advances, we anticipate that these networks will be fractionated and designated in accordance with their functional ontologies, as illustrated later when we discuss the default network [34].
Figure 1. Coarse (7-network) parcellation of the human cerebral cortex obtained through clustering of R-fMRI data of 1,000 subjects.
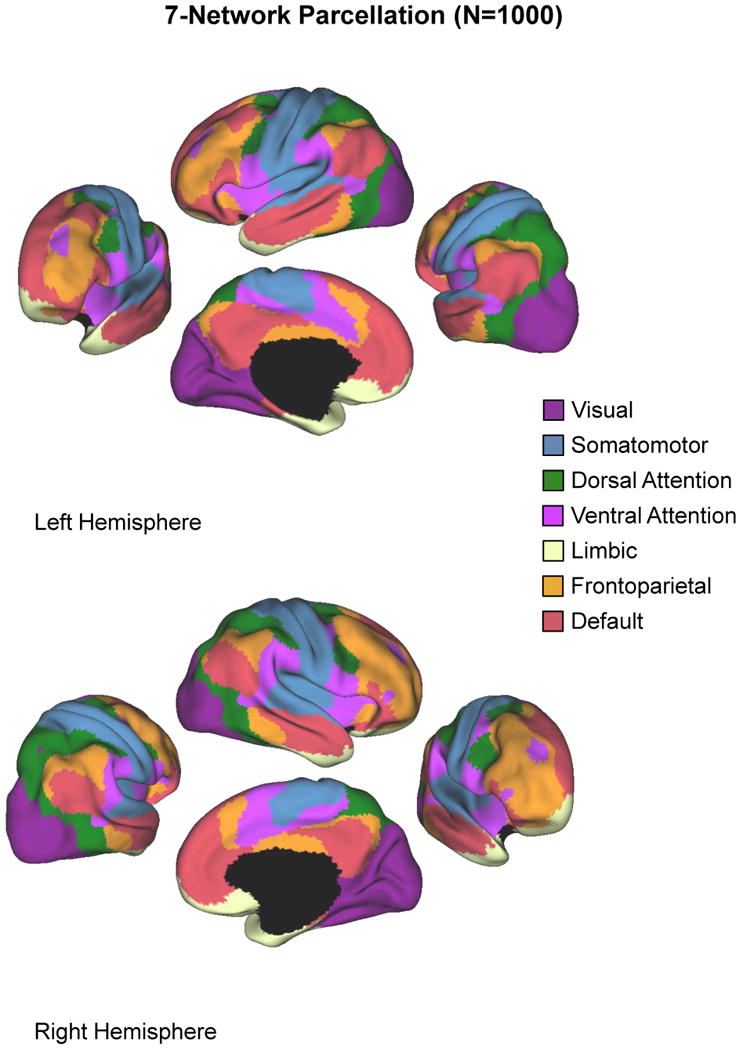
At this resolution, association cortex is distinguished from primary sensorimotor cortex. The association networks converged on and extended networks previously described in the resting-state literature, including the dorsal attention, ventral attention, frontoparietal control, and default networks. Adapted, with permission, from [12].
Candidate neural systems in ADHD
Recent conceptualizations of ADHD have taken seriously the distributed nature of neuronal processing [10,11,35,36]. Most of the candidate networks have focused on prefrontal-striatal-cerebellar circuits, although other posterior regions are also being proposed [10]. Until now, the evidence marshaled in support of a particular hypothesized circuit has consisted mostly of between-group differences in task-based fMRI activations [e.g., 36] or anatomic volumetric differences [8]. Such results provide indirect evidence of validity, but individually they only illuminate subsets of circuit components. Their generalizability is also usually limited to the specific construct of interest, the population sampled, and by idiosyncratic methodological factors. Fortunately, the neural substrates of functional circuits that are identified piece-wise through task-based fMRI studies are continuously represented in the brain in the form of intrinsic connectivity networks which are most easily measured during rest [16]. The recent compilation of reference networks for healthy young adults [12] raises questions of whether these circuits will provide a brain-based perspective for the process of characterizing brain behavior relationships across the lifespan and in clinical populations. Here, we briefly review the recent ADHD neuroimaging literature within the context of these reference resting state functional networks [12].
Fronto-parietal network
The frontoparietal control circuit (shown in Figure 1) includes the lateral frontal pole, anterior cingulate cortex (ACC), dorsolateral prefrontal cortex (dlPFC), anterior PFC (aPFC), lateral cerebellum, anterior insula, caudate and inferior parietal lobe [37]. This network is also known as the executive control circuit [38] because it underpins goal-directed executive processes and provides the flexibility to configure information processing in response to changing task demands [39]. Executive control systems guide decision making by integrating external information with internal representations.
In ADHD, the most studied executive control deficits have focused on motor inhibition. Multiple studies have found hypoactivation in frontostriatal and frontoparietal circuits during inhibitory tasks in children with ADHD [7,36]. Besides parietal areas, nearly all the remaining regions which have been implicated in the prefrontal-striatal-cerebellar model of ADHD [8,40] are components of the frontoparietal circuit: ACC, aPFC, dlPFC, frontal pole, cerebellum, and caudate. For example, the dorsal ACC has been reported as hypoactivated in ADHD during go/no go, response inhibition and attentional tasks [11,36,41-43]. Similarly, dlPFC and ventrolateral PFC are hypoactivated in various tasks ranging from working memory to time discrimination [36,43-45]. Involvement of the frontoparietal network has also been confirmed by resting state studies in ADHD [46-49].
The frontoparietal network has been situated both spatially and conceptually as an intermediate system between two other major networks in the brain, the default network and the dorsal attentional network [37], which we take up next.
The dorsal and ventral attentional networks
Figure 1 shows the reference dorsal and ventral attentional networks [32], which form key components of the attentional regulatory systems of the brain [50]. The ventral attentional network, closely related to circuits referred to as the salience network [38] or the cingulo-opercular network [51], is involved in monitoring for salient, i.e., behaviorally relevant, stimuli and for interrupting ongoing activity when appropriate. The ventral attentional network is anchored by the temporoparietal junction, the supramarginal gyrus, frontal operculum, and anterior insula [50].
The network most likely to be affected by the ventral is the dorsal attentional network, which mediates goal-directed, top-down executive control processes, particularly in reorienting attention during visual attentional functioning. Its key nodes are the intraparietal sulcus (BA 40) and the frontal eye fields (BA 6), which are the main regions involved in attention shifting and in controlling spatial attention [50].
The literature does not support clear involvement of the ventral attentional network in ADHD, but it is also not yet possible to discard its potential participation. By contrast, abnormalities in precentral and parietal regions associated with the dorsal attentional network clearly emerge in ADHD [7,36,52]. For example, during the performance of executive and response inhibition tasks, bilateral parietal regions (BA7, BA40) were among the main areas in which controls demonstrated significantly greater probability of activation relative to ADHD subjects, along with motor regions (BA6) [7]. More recent studies have shown greater activation of the parietal cortex of ADHD patients during response inhibition [53,54]. In addition, abnormal patterns of parietal activity have been reported during working memory [55-57] and attentional tasks [52,58-63].
Visual network
The visual cortex and the lateral temporal MT+ region are related with the superior parietal lobule and intraparietal sulcus, which are part of the dorsal attentional network. MT+ also is coupled with frontal regions such as precentral cortex and the frontal eye fields. MT+ is strongly functionally correlated with primary visual areas such as V1 and V3 [12].
The occipital cortex has not previously been considered to be relevant to ADHD, even though neuroimaging studies in ADHD have found repeated differences in medial occipital cortex (BA18, BA19) [7,53,58,64,65]. Occipital cortex interacts with the dorsal attentional network to maintain attention [66] and suppress attention to irrelevant stimuli [67]. Failing to ignore extraneous stimuli is one of the core symptoms of ADHD. A recent structural neuroimaging study in medication-naïve adults with ADHD found significant bilateral reduction of gray matter volume only in early visual cortex [68]. In a 33-year follow-up of childhood ADHD, persistence of the diagnosis was associated with decreased cortical thickness in medial occipital cortex among other regions (see Figure 2) [9]. In functional studies, children with ADHD show deactivation of parietal and occipital regions during spatial tasks [64,65] whereas adults with ADHD show occipital hyperactivations on inhibition, working memory and attentional tasks [53,58,69]. A resting state study in children with ADHD found decreased small-world network nodal efficiency in multiple brain regions including visual cortex [49]. These findings suggest that visual function and its regulation by attentional processes should be further investigated in ADHD.
Figure 2. Cortical thickness analysis reveals occipital involvement in ADHD.
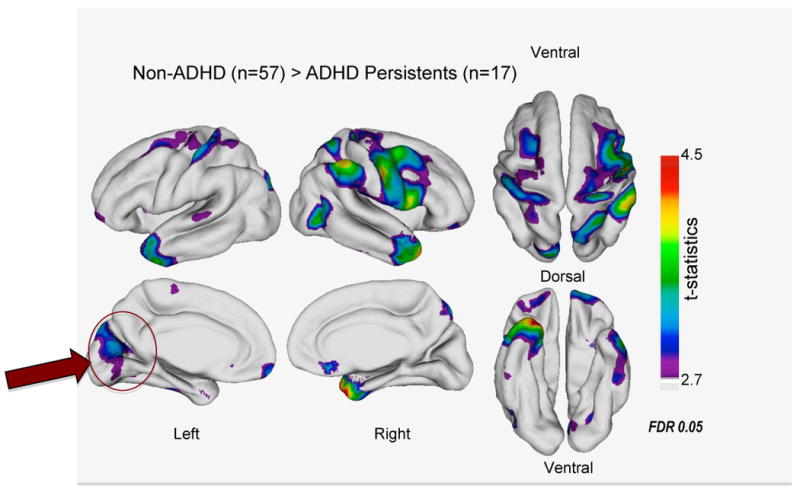
In a 33-year longitudinal follow-up study, adults with ADHD persisting from childhood showed significantly decreased cortical thickness in multiple regions, including medial occipital cortex (arrow) relative to non-ADHD controls. Reproduced, with permission, from [9].
Motor network
The first brain network identified by characterizing intrinsic functional connectivity was the motor system [18]. As recently reviewed, R-fMRI analyses detect synchrony in spontaneous low-frequency fluctuations between primary motor cortex, primary sensory cortex, second sensory cortex, supplementary motor area (SMA), ventral premotor cortex, putamen, thalamus, and cerebellum [70].
Remarkably, despite the incontrovertible salience of motoric hyperactivity in children with ADHD, there have been few neuroimaging studies of the motor system in ADHD [e.g., 36,71,72,73]. When performing simple motor tapping, children with ADHD exhibited decreased activation in primary motor cortex relative to controls [71]. Intra-subject variability, which is generally increased in ADHD [74], was positively related to pre-SMA activation in children with ADHD, whereas in healthy controls variability was inversely related to pre-SMA activation [72]. In a study of adults with ADHD during paced and unpaced tapping, hypoactivations in ADHD were found both in timing related circuits as well as in motor and premotor cortex [73]. In a non-imaging study that directly probed the motor system, intracortical inhibition was measured with short-interval paired-pulse transcranial magnetic stimulation [75]. Children with ADHD were found to have markedly reduced cortical inhibition which was correlated with deficiencies in motor performance [75]. This recent literature suggests that continued examination of the motor system in ADHD would be productive.
The default network
The most studied intrinsic functional connectivity system is known as the brain's default network (see Figure 1), because its high amplitude fluctuations, which are consistently diminished during cognitive tasks and increased during rest, were described as representing the brain's physiological baseline [14,31]. As shown in Figure 3, the default network contains two hubs, the anterior medial PFC (aMPFC) and posterior cingulate cortex (PCC) and two subcomponent systems, the dorsomedial prefrontal cortex (dMPFC) subsystem and the medial temporal lobe (MTL) subsystem [34]. In a tour-de-force model of how to combine task-based and resting state data, Andrews-Hanna et al. established that the dMPFC subsystem is activated when subjects perform self-referential cognitive processes anchored in the present; the MTL subsystem is preferentially activated by cognitions regarding projecting one's self into the future [34]. Beyond its roles in typically developing individuals, the default network is implicated across the full range of psychiatric disorders [38].
Figure 3. Fractionation of the default network.
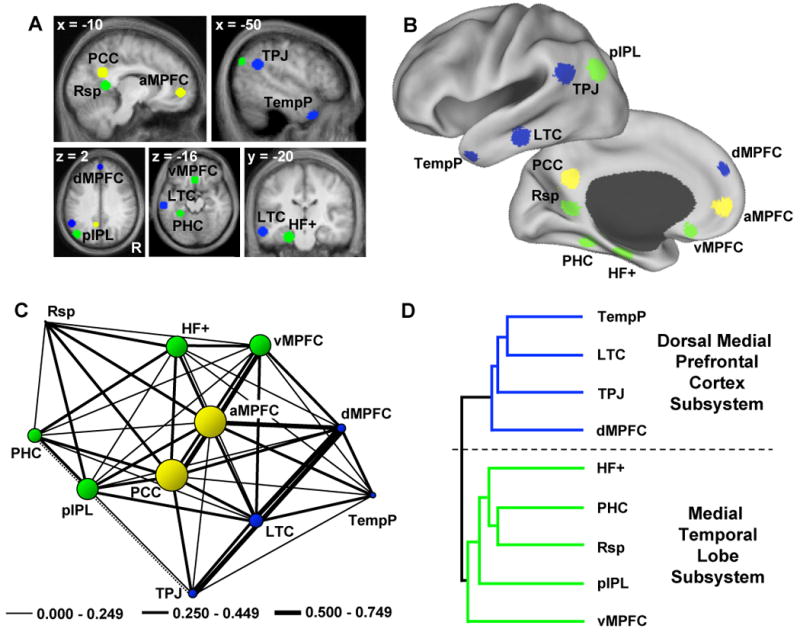
Default network core hubs are shown in yellow, the dorsomedial prefrontal cortex subsystem is shown in blue, and the regions comprising the medial temporal lobe subsystem are in green. (a) Shows the 11 seeds defined a priori using functional connectivity approaches. (b) The 11 seeds projected onto an inflated brain. (c) The correlation strengths among the regions within the default network are shown using network centrality measures. The size of the circle represents the centrality of a given node. The anterior medial prefrontal cortex (aMPFC) and posterior cingulate cortex (PCC) are the core hubs of the network and both are significantly connected to every other node. Negative correlations are shown with a dotted line. (d) Represents the two clusters resulting from centrality analyses. dMPFC: dorsomedial prefrontal cortex; TPJ: temporoparietal junction; LTC: lateral temporal cortex; TempP: temporal pole; vMPFC: ventromedial prefrontal cortex; pIPL: posterior inferior parietal lobe; Rsp: retrosplenial cortex; PHC: parahippocampal cortex; HF+: hippocampal formation. Reproduced, with permission, from [34].
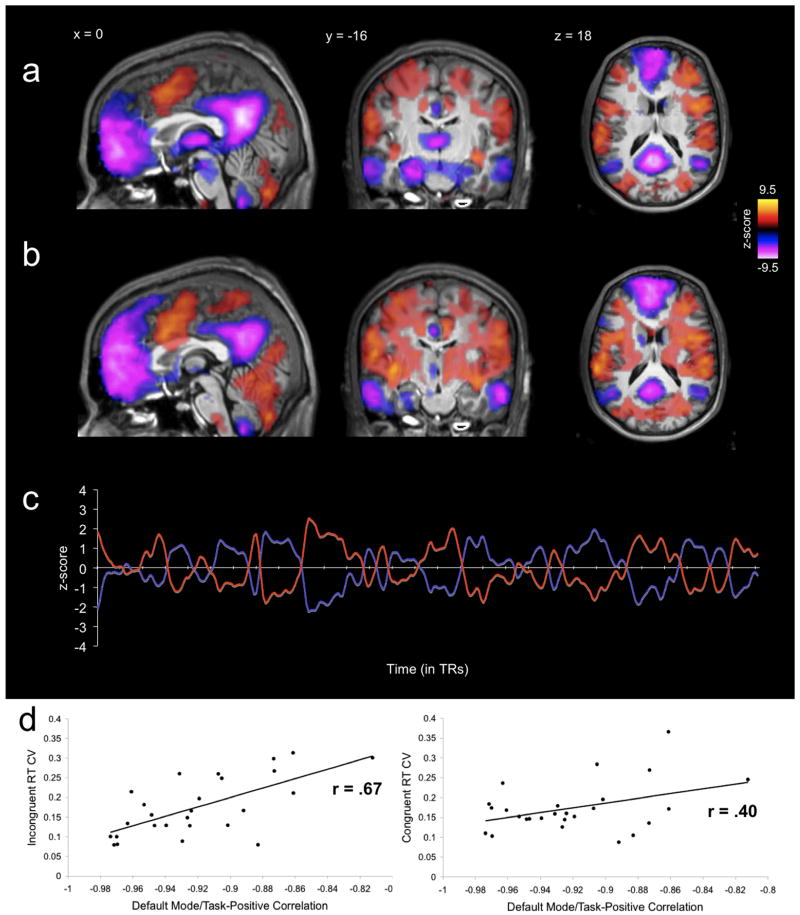
Intriguingly, default network fluctuations are 180° out of phase with fluctuations in networks that become activated during externally-oriented tasks, presumably reflecting competition between opposing processes for processing resources [76]. Stronger negative correlation between default and frontoparietal control networks and greater coherence within networks is related to better behavioral performance, as shown in Figure 4 [76]. This is consistent with the finding that diminished suppression of default network activity is associated with attentional lapses [77] and with the suggestion that inter-individual differences in performance are related to the efficiency of interactions among brain regions [78].
Figure 4. Anticorrelations between neural networks.
(a) Mid-sagittal, coronal and axial views of anticorrelated networks extracted through region-of-interest based functional connectivity analyses by. The “task positive network” shown in yellow-orange includes the frontoparietal network; the default network is shown in purple.
(b) Mid-sagittal, coronal and axial views of anticorrelated networks extracted through independent component analyses showing substantial overlap of the two methods. The frontoparietal network is shown in yellow-orange and the default network in purple.
(c) Time series of default and frontoparietal networks for one participant with Pearson r= - 0.97 during performance of slow event-related Eriksen Flanker task. The strength of this relationship was negatively related to intra-subject variability of response times across participants.
Reproduced, with permission, from [76].
In 2007 Sonuga-Barke and Castellanos suggested that ADHD could be considered a default network disorder [79]. They reasoned that the default network in ADHD might be refractory to regulation by other neural systems, thus producing intrusions or disruptions of ongoing cognition and behavior which would manifest as periodic lapses in on-task performance, a hallmark of ADHD [74]. Decreased default network coherence has been found in ADHD [80] and decreased default network suppression has been related to increased intra-individual variability in a small sample of children with ADHD [81]; ongoing studies will test the hypothesis that intercorrelation between the default network and cognitive control networks [76] underpins ADHD attentional lapses.
In the meantime, an interesting result has been obtained by comparing healthy young subjects scanned after rested wakefulness and after 24 hours of full sleep deprivation [82]. Sleep deprivation produced an increase in intra-subject variability and degraded attentional performance. These were paralleled by decreases in default network functional connectivity and weaker anticorrelation between the default network and anti-correlated regions [76,82]. Determining whether similar effects are found in participants with ADHD is likely to be informative.
Treatment with methylphenidate was found to normalize default network suppression in ventromedial PFC and PCC in 16 youth with ADHD each scanned twice [83]. An interaction among methylphenidate, motivational level (high and low incentives) and diagnosis was found in default network suppression during a go/no-go task [84]. Control children deactivated the default network under both high and low incentive conditions, similarly to the children with ADHD who were scanned on methylphenidate. By contrast, children with ADHD scanned while off medication only deactivated the default network during the high incentive condition [84]. The authors concluded that the normalization of default network suppression by either methylphenidate or increased incentives points to dysregulation of the default network rather than to its fundamental impairment. On the other hand, abnormalities residing in the default network are suggested by the emergence of significantly greater gray matter volume in precuneus/PCC in a structural meta-analysis of ADHD [8]. Taken together, these findings suggest that the interplay of default, cognitive control and limbic networks is likely a key factor in suboptimal neural functioning in ADHD.
A counter-argument to the above analysis could be that we have simply proposed that the entire brain is involved in ADHD. While such an argument is not without merit, in that global volumetric reductions have been consistently related to the disorder [5], we believe it is far more likely that interactions among the candidate functional networks we have identified will form distinguishable neurobiological patterns that can provide the bases for meaningful subtyping of this heterogeneous condition
Concluding remarks
Functional connectivity reveals replicable brain networks that are likely to be relevant to our understanding of brain-behavior relationships in disorders such as ADHD. Characterizing the spatial extents of such networks [21] or their intra- or inter-network coherence for individuals has become feasible [76,92-94]. What is now needed is to relate such brain network profiles [12] to neuropsychological and clinical measures [95]. The networks we have mentioned are unlikely to be exhaustive or equally relevant to all individuals with ADHD, but they provide a straightforward framework for converging attempts to parse the pertinent dimensions of symptoms and constructs, in keeping with the U.S. National Institute of Mental Health Research Domains Criteria project (http://www.nimh.nih.gov/research-funding/rdoc/nimh-research-domain-criteria-rdoc.shtml). Brain networks are situated in the conceptual “sweet spot” between genes and behaviors, and represent the most tractable opportunities to formulate hypotheses linking these multiple levels (see also Box 3).
Box 3. Questions for future research.
Is increased response time intra-individual variability in ADHD ascribable to abnormalities within a single system, such as the default network, or to the interrelationships among default, executive control and limbic-motivational networks?
Can imbalances between dorsal attentional network and/or frontoparietal network on the one hand, and the default network, on the other, be redressed through intracranial direct current electrical stimulation? Are these networks useful units to examine the effects of pharmacological and behavioral treatments? Are they relevant to lack of response to treatments?
How do the seven large intrinsic connectivity networks map onto striatal [98], thalamic [99], and cerebellar [100] connectivity circuits?
What is the appropriate resolution level to examine cortico-striato-thalamo-cortical and cortico-thalamo-cerebellar circuitry in ADHD? Are the seven large networks overly inclusive?
Do visual network abnormalities in ADHD relate to its linkage to the dorsal attentional network? Are they primary or compensatory? How are they related to inattention symptoms?
Can neurobiological subtypes of ADHD be established on the basis of neural network profiles?
Can such neural network profiles be used to track treatment response?
How will ADHD-related differences in neural network profiles change across development in cross-sectional and longitudinal studies?
How do the default network subcomponent functions (self-related processing in the present vs. the future) relate to ADHD symptoms? Is the medial temporal subcomponent associated with future prospection associated with faulty decision making in ADHD and related disorders?
However, in the absence of manipulation, neuroimaging methods remain correlational, and unable to inform on causal mechanisms. Nevertheless, imaging pre- and post-treatment can reveal biomarkers linked to causal pathways. Besides pharmacological and behavioral treatments for ADHD, novel approaches such as transcranial direct current electrical stimulation (tDCS) should be considered (see Box 2). Non-invasive tDCS can produce transient increases or decreases in cortical excitability which target specific regions and circuits and their interactions [89-91,96]. Despite substantial evidence that tDCS modulates neural processes, its clinical benefits have not been demonstrated convincingly, even for chronic pain [97]. We suggest that future tDCS studies could use R-fMRI to select candidate patients and circuits, and that imaging be used to document the appropriate placement of stimulating electrodes. Evidence of short-term improvement in symptoms and corresponding changes in the circuits targeted could then be used to justify more prolonged treatment regimens, with the goal of determining whether transcranial electrical stimulation holds therapeutic promise in ADHD.
Box 2. Transcranial direct current stimulation.
Transcranial direct current stimulation (tDCS) is a noninvasive neurostimulating technique which uses small electrodes as pathways for delivering low amplitude electric current to cerebral regions of interest. This technique is considered a promising tool for clinical populations because of its safe application in humans [86].
Transcranial DCS is performed through a battery-powered device that emits a constant current through two electrodes. Each device has a positively charged electrode (anode) and a negatively charged electrode (cathode). The applied current is diminished substantially in crossing the scalp, but sufficient electricity flows into the brain to produce neuronal effects. Application of anodal direct current increases and cathodal direct current decreases underlying cortical excitability. The extent of neuronal effects depends on the duration of stimulation, size of the electrodes, and current density [87,88].
Recent pre- and post-tDCS R-fMRI sessions lead to the suggestion that neurostimulation may have therapeutic relevance for ADHD. Real but not sham tCDS applied to left and right dlPFC produced decreases in default network synchrony and increases in anticorrelated network coherence [89]. Stimulation over primary motor cortex modulated functional connectivity of cortico-striatal and thalamo-cortical circuits [90]. Real vs. sham anodal tDCS of dlPFC significantly enhanced default and frontoparietal network synchrony, which may underlie reports of improvements in cognitive performance [91].
Glossary
- Electrocorticography (ECoG)
electroencephalography with the electrodes applied directly to the exposed surface of the brain to record electrical activity from the cerebral cortex. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure. ECoG is the “gold standard” for defining epileptogenic zones in clinical practice. ECoG data have served to validate R-fMRI findings as relevant to neuronal processes, and not simply ascribable to hemodynamic or physiological epiphenomena
- Anticorrelations
are negative correlations, in which one value increases as the other decreases. These are observed in R-fMRI data even in the absence of regression with the global signal as a nuisance covariate, but doing so enhances their detection. The neurophysiological significance of cerebral anticorrelations remains unknown but they are generally observed between competing neural systems such as the default network and the frontoparietal control network
- Systems neuroscience
a subdiscipline of neuroscience and systems biology that studies the function of neural circuits and systems. It is an umbrella term, encompassing a number of areas of study concerned with how nerve cells behave when connected together to form neural networks
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. American Psychiatric Association; 2000. [Google Scholar]
- 2.Polanczyk G, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control. Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children --- United States, 2003 and 2007. MMWR Morb Mortal Wkly Rep. 2010;59:1439–1443. [PubMed] [Google Scholar]
- 4.Simon V, et al. Prevalence and correlates of adult attention-deficit hyperactivity disorder: meta-analysis. Br J Psychiatry. 2009;194:204–211. doi: 10.1192/bjp.bp.107.048827. [DOI] [PubMed] [Google Scholar]
- 5.Krain AL, Castellanos FX. Brain development and ADHD. Clin Psychol Rev. 2006;26:433–444. doi: 10.1016/j.cpr.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Castellanos FX, et al. Characterizing cognition in ADHD: beyond executive dysfunction. Trends Cogn Sci. 2006;10:117–123. doi: 10.1016/j.tics.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Dickstein SG, et al. The neural correlates of attention deficit hyperactivity disorder: an ALE meta-analysis. J Child Psychol Psychiatry. 2006;47:1051–1062. doi: 10.1111/j.1469-7610.2006.01671.x. [DOI] [PubMed] [Google Scholar]
- 8.Nakao T, et al. Gray matter volume abnormalities in ADHD: Voxel-based meta-analysis exploring the effects of age and stimulant medication. Am J Psychiatry. 2011 doi: 10.1176/appi.ajp.2011.11020281. [DOI] [PubMed] [Google Scholar]
- 9.Proal E, et al. Brain gray matter deficits at 33-year follow-up in adults with attention-deficit/hyperactivity disorder established in childhood. Arch Gen Psychiatry. 2011;68:1122–1134. doi: 10.1001/archgenpsychiatry.2011.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makris N, et al. Towards conceptualizing a neural systems-based anatomy of attention-deficit/hyperactivity disorder. Dev Neurosci. 2009;31:36–49. doi: 10.1159/000207492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bush G. Attention-deficit/hyperactivity disorder and attention networks. Neuropsychopharmacology. 2010;35:278–300. doi: 10.1038/npp.2009.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yeo BT, et al. The organization of the human cerebral cortex estimated by functional connectivity. J Neurophysiol. 2011;106:1125–1165. doi: 10.1152/jn.00338.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lowe MJ. A historical perspective on the evolution of resting-state functional connectivity with MRI. MAGMA. 2010;23:279–288. doi: 10.1007/s10334-010-0230-y. [DOI] [PubMed] [Google Scholar]
- 14.Raichle ME, Snyder AZ. A default mode of brain function: a brief history of an evolving idea. Neuroimage. 2007;37:1083–1090. doi: 10.1016/j.neuroimage.2007.02.041. [DOI] [PubMed] [Google Scholar]
- 15.Margulies DS, et al. Resting developments: a review of fMRI post-processing methodologies for spontaneous brain activity. MAGMA. 2010;23:289–307. doi: 10.1007/s10334-010-0228-5. [DOI] [PubMed] [Google Scholar]
- 16.Smith SM, et al. Correspondence of the brain's functional architecture during activation and rest. Proc Natl Acad Sci U S A. 2009;106:13040–13045. doi: 10.1073/pnas.0905267106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biswal BB, et al. Toward discovery science of human brain function. Proc Natl Acad Sci U S A. 2010;107:4734–4739. doi: 10.1073/pnas.0911855107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat Rev Neurosci. 2007;8:700–711. doi: 10.1038/nrn2201. [DOI] [PubMed] [Google Scholar]
- 19.Vincent JL, et al. Intrinsic functional architecture in the anaesthetized monkey brain. Nature. 2007;447:83–86. doi: 10.1038/nature05758. [DOI] [PubMed] [Google Scholar]
- 20.Keller CJ, et al. Intrinsic functional architecture predicts electrically evoked responses in the human brain. Proc Natl Acad Sci U S A. 2011;108:10308–10313. doi: 10.1073/pnas.1019750108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mennes M, et al. Inter-individual differences in resting state functional connectivity predict task-induced BOLD activity. Neuroimage. 2010;50:1690–1701. doi: 10.1016/j.neuroimage.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deco G, et al. Emerging concepts for the dynamical organization of resting-state activity in the brain. Nat Rev Neurosci. 2011;12:43–56. doi: 10.1038/nrn2961. [DOI] [PubMed] [Google Scholar]
- 23.Shehzad Z, et al. The resting brain: unconstrained yet reliable. Cereb Cortex. 2009;19:2209–2229. doi: 10.1093/cercor/bhn256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Dijk KR, et al. Intrinsic functional connectivity as a tool for human connectomics: theory, properties, and optimization. J Neurophysiol. 2010;103:297–321. doi: 10.1152/jn.00783.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Margulies DS, et al. Precuneus shares intrinsic functional architecture in humans and monkeys. Proc Natl Acad Sci U S A. 2009;106:20069–20074. doi: 10.1073/pnas.0905314106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Power JD, et al. The development of human functional brain networks. Neuron. 2010;67:735–748. doi: 10.1016/j.neuron.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang D, Raichle ME. Disease and the brain's dark energy. Nat Rev Neurol. 2010;6:15–28. doi: 10.1038/nrneurol.2009.198. [DOI] [PubMed] [Google Scholar]
- 28.Konrad K, Eickhoff SB. Is the ADHD brain wired differently? A review on structural and functional connectivity in attention deficit hyperactivity disorder. Hum Brain Mapp. 2010;31:904–916. doi: 10.1002/hbm.21058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sporns O, et al. The human connectome: A structural description of the human brain. PLoS Comput Biol. 2005;1:e42. doi: 10.1371/journal.pcbi.0010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Glascher J, et al. Distributed neural system for general intelligence revealed by lesion mapping. Proc Natl Acad Sci U S A. 2010;107:4705–4709. doi: 10.1073/pnas.0910397107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Buckner RL, et al. The brain's default network: anatomy, function, and relevance to disease. Ann N Y Acad Sci. 2008;1124:1–38. doi: 10.1196/annals.1440.011. [DOI] [PubMed] [Google Scholar]
- 32.Fox MD, et al. Spontaneous neuronal activity distinguishes human dorsal and ventral attention systems. Proc Natl Acad Sci U S A. 2006;103:10046–10051. doi: 10.1073/pnas.0604187103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Damoiseaux JS, et al. Consistent resting-state networks across healthy subjects. Proc Natl Acad Sci U S A. 2006;103:13848–13853. doi: 10.1073/pnas.0601417103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andrews-Hanna JR, et al. Functional-anatomic fractionation of the brain's default network. Neuron. 2010;65:550–562. doi: 10.1016/j.neuron.2010.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Durston S, et al. Differentiating frontostriatal and fronto-cerebellar circuits in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2011;69:1178–1184. doi: 10.1016/j.biopsych.2010.07.037. [DOI] [PubMed] [Google Scholar]
- 36.Rubia K. “Cool” inferior frontostriatal dysfunction in attention-deficit/hyperactivity disorder versus “hot” ventromedial orbitofrontal-limbic dysfunction in conduct disorder: a review. Biol Psychiatry. 2011;69:e69–e87. doi: 10.1016/j.biopsych.2010.09.023. [DOI] [PubMed] [Google Scholar]
- 37.Vincent JL, et al. Evidence for a frontoparietal control system revealed by intrinsic functional connectivity. J Neurophysiol. 2008;100:3328–3342. doi: 10.1152/jn.90355.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Menon V. Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci. 2011;15:483–506. doi: 10.1016/j.tics.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Liston C, et al. Anterior cingulate and posterior parietal cortices are sensitive to dissociable forms of conflict in a task-switching paradigm. Neuron. 2006;50:643–653. doi: 10.1016/j.neuron.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 40.Valera EM, et al. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007;61:1361–1369. doi: 10.1016/j.biopsych.2006.06.011. [DOI] [PubMed] [Google Scholar]
- 41.Durston S, et al. Neural and behavioral correlates of expectancy violations in attention-deficit hyperactivity disorder. J Child Psychol Psychiatry. 2007;48:881–889. doi: 10.1111/j.1469-7610.2007.01754.x. [DOI] [PubMed] [Google Scholar]
- 42.Konrad K, et al. Dysfunctional attentional networks in children with attention deficit/hyperactivity disorder: evidence from an event-related functional magnetic resonance imaging study. Biol Psychiatry. 2006;59:643–651. doi: 10.1016/j.biopsych.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 43.Smith AB, et al. Reduced activation in right lateral prefrontal cortex and anterior cingulate gyrus in medication-naive adolescents with attention deficit hyperactivity disorder during time discrimination. J Child Psychol Psychiatry. 2008;49:977–985. doi: 10.1111/j.1469-7610.2008.01870.x. [DOI] [PubMed] [Google Scholar]
- 44.Schneider M, et al. Anatomical and functional brain imaging in adult attention-deficit/hyperactivity disorder (ADHD)--a neurological view. Eur Arch Psychiatry Clin Neurosci. 2006;256 1:i32–i41. doi: 10.1007/s00406-006-1005-3. [DOI] [PubMed] [Google Scholar]
- 45.Vaidya CJ, Stollstorff M. Cognitive neuroscience of Attention Deficit Hyperactivity Disorder: current status and working hypotheses. Dev Disabil Res Rev. 2008;14:261–267. doi: 10.1002/ddrr.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao Q, et al. Abnormal neural activity in children with attention deficit hyperactivity disorder: a resting-state functional magnetic resonance imaging study. NeuroReport. 2006;17:1033–1036. doi: 10.1097/01.wnr.0000224769.92454.5d. [DOI] [PubMed] [Google Scholar]
- 47.Zang YF, et al. Altered baseline brain activity in children with ADHD revealed by resting-state functional MRI. Brain Dev. 2007;29:83–91. doi: 10.1016/j.braindev.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 48.Cao X, et al. Abnormal resting-state functional connectivity patterns of the putamen in medication-naive children with attention deficit hyperactivity disorder. Brain Res. 2009;1303:195–206. doi: 10.1016/j.brainres.2009.08.029. [DOI] [PubMed] [Google Scholar]
- 49.Wang L, et al. Altered small-world brain functional networks in children with attention-deficit/hyperactivity disorder. Hum Brain Mapp. 2009;30:638–649. doi: 10.1002/hbm.20530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Corbetta M, et al. The reorienting system of the human brain: from environment to theory of mind. Neuron. 2008;58:306–324. doi: 10.1016/j.neuron.2008.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dosenbach NU, et al. A dual-networks architecture of top-down control. Trends Cogn Sci. 2008;12:99–105. doi: 10.1016/j.tics.2008.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stevens MC, et al. An FMRI auditory oddball study of combined-subtype attention deficit hyperactivity disorder. Am J Psychiatry. 2007;164:1737–1749. doi: 10.1176/appi.ajp.2007.06050876. [DOI] [PubMed] [Google Scholar]
- 53.Dillo W, et al. Neuronal correlates of ADHD in adults with evidence for compensation strategies--a functional MRI study with a Go/No-Go paradigm. Ger Med Sci. 2010;8:Doc09. doi: 10.3205/000098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karch S, et al. Neural correlates (ERP/fMRI) of voluntary selection in adult ADHD patients. Eur Arch Psychiatry Clin Neurosci. 2010;260:427–440. doi: 10.1007/s00406-009-0089-y. [DOI] [PubMed] [Google Scholar]
- 55.Wolf RC, et al. Regional brain activation changes and abnormal functional connectivity of the ventrolateral prefrontal cortex during working memory processing in adults with attention-deficit/hyperactivity disorder. Hum Brain Mapp. 2009;30:2252–2266. doi: 10.1002/hbm.20665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Burgess GC, et al. Attentional control activation relates to working memory in attention-deficit/hyperactivity disorder. Biol Psychiatry. 2010;67:632–640. doi: 10.1016/j.biopsych.2009.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bayerl M, et al. Disturbed brain activation during a working memory task in drug-naive adult patients with ADHD. NeuroReport. 2010;21:442–446. doi: 10.1097/WNR.0b013e328338b9be. [DOI] [PubMed] [Google Scholar]
- 58.Schneider MF, et al. Impairment of fronto-striatal and parietal cerebral networks correlates with attention deficit hyperactivity disorder (ADHD) psychopathology in adults - a functional magnetic resonance imaging (fMRI) study. Psychiatry Res. 2010;183:75–84. doi: 10.1016/j.pscychresns.2010.04.005. [DOI] [PubMed] [Google Scholar]
- 59.Rubia K, et al. Temporal lobe dysfunction in medication-naive boys with attention-deficit/hyperactivity disorder during attention allocation and its relation to response variability. Biol Psychiatry. 2007;62:999–1006. doi: 10.1016/j.biopsych.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 60.Tamm L, et al. Parietal attentional system aberrations during target detection in adolescents with attention deficit hyperactivity disorder: event-related fMRI evidence. Am J Psychiatry. 2006;163:1033–1043. doi: 10.1176/ajp.2006.163.6.1033. [DOI] [PubMed] [Google Scholar]
- 61.Rubia K, et al. Methylphenidate normalises activation and functional connectivity deficits in attention and motivation networks in medication-naive children with ADHD during a rewarded continuous performance task. Neuropharmacology. 2009;57:640–652. doi: 10.1016/j.neuropharm.2009.08.013. [DOI] [PubMed] [Google Scholar]
- 62.Cubillo A, et al. Reduced activation and inter-regional functional connectivity of fronto-striatal networks in adults with childhood Attention-Deficit Hyperactivity Disorder (ADHD) and persisting symptoms during tasks of motor inhibition and cognitive switching. J Psychiatr Res. 2010;44:629–639. doi: 10.1016/j.jpsychires.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 63.Banich MT, et al. The neural basis of sustained and transient attentional control in young adults with ADHD. Neuropsychologia. 2009 doi: 10.1016/j.neuropsychologia.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Silk T, et al. Dysfunction in the fronto-parietal network in attention deficit hyperactivity disorder (ADHD): An fMRI study. Brain Imaging and Behavior. 2008;2:123–131. [Google Scholar]
- 65.Vance A, et al. Right parietal dysfunction in children with attention deficit hyperactivity disorder, combined type: a functional MRI study. Mol Psychiatry. 2007;12:826–832. doi: 10.1038/sj.mp.4001999. [DOI] [PubMed] [Google Scholar]
- 66.Shulman GL, et al. Interaction of stimulus-driven reorienting and expectation in ventral and dorsal frontoparietal and basal ganglia-cortical networks. J Neurosci. 2009;29:4392–4407. doi: 10.1523/JNEUROSCI.5609-08.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Capotosto P, et al. Frontoparietal cortex controls spatial attention through modulation of anticipatory alpha rhythms. J Neurosci. 2009;29:5863–5872. doi: 10.1523/JNEUROSCI.0539-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ahrendts J, et al. Visual cortex abnormalities in adults with ADHD: A structural MRI study. World J Biol Psychiatry. 2010 doi: 10.3109/15622975.2010.518624. [DOI] [PubMed] [Google Scholar]
- 69.Hale TS, et al. Atypical brain activation during simple & complex levels of processing in adult ADHD: an fMRI study. J Atten Disord. 2007;11:125–140. doi: 10.1177/1087054706294101. [DOI] [PubMed] [Google Scholar]
- 70.Deco G, Corbetta M. The dynamical balance of the brain at rest. Neuroscientist. 2011;17:107–123. doi: 10.1177/1073858409354384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mostofsky SH, et al. Atypical motor and sensory cortex activation in attention-deficit/hyperactivity disorder: a functional magnetic resonance imaging study of simple sequential finger tapping. Biol Psychiatry. 2006;59:48–56. doi: 10.1016/j.biopsych.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 72.Suskauer SJ, et al. fMRI of intrasubject variability in ADHD: anomalous premotor activity with prefrontal compensation. J Am Acad Child Adolesc Psychiatry. 2008;47:1141–1150. doi: 10.1097/CHI.0b013e3181825b1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Valera EM, et al. Neural substrates of impaired sensorimotor timing in adult attention-deficit/hyperactivity disorder. Biol Psychiatry. 2010;68:359–367. doi: 10.1016/j.biopsych.2010.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Castellanos FX, et al. Varieties of attention-deficit/hyperactivity disorder-related intra-individual variability. Biol Psychiatry. 2005;57:1416–1423. doi: 10.1016/j.biopsych.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gilbert DL, et al. Motor cortex inhibition: a marker of ADHD behavior and motor development in children. Neurology. 2011;76:615–621. doi: 10.1212/WNL.0b013e31820c2ebd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kelly AMC, et al. Competition between functional brain networks mediates behavioral variability. Neuroimage. 2008;39:527–537. doi: 10.1016/j.neuroimage.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 77.Weissman DH, et al. The neural bases of momentary lapses in attention. Nat Neurosci. 2006;9:971–978. doi: 10.1038/nn1727. [DOI] [PubMed] [Google Scholar]
- 78.Rypma B, et al. Neural correlates of cognitive efficiency. Neuroimage. 2006;33:969–979. doi: 10.1016/j.neuroimage.2006.05.065. [DOI] [PubMed] [Google Scholar]
- 79.Sonuga-Barke EJ, Castellanos FX. Spontaneous attentional fluctuations in impaired states and pathological conditions: A neurobiological hypothesis. Neurosci Biobehav Rev. 2007;31:977–986. doi: 10.1016/j.neubiorev.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 80.Castellanos FX, et al. Cingulate-precuneus interactions: a new locus of dysfunction in adult attention-deficit/hyperactivity disorder. Biol Psychiatry. 2008;63:332–337. doi: 10.1016/j.biopsych.2007.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fassbender C, et al. A lack of default network suppression is linked to increased distractibility in ADHD. Brain Res. 2009;1273:114–128. doi: 10.1016/j.brainres.2009.02.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.De Havas JA, et al. Sleep deprivation reduces default mode network connectivity and anti-correlation during rest and task performance. Neuroimage. 2011 doi: 10.1016/j.neuroimage.2011.08.026. [DOI] [PubMed] [Google Scholar]
- 83.Peterson BS, et al. An FMRI study of the effects of psychostimulants on default-mode processing during Stroop task performance in youths with ADHD. Am J Psychiatry. 2009;166:1286–1294. doi: 10.1176/appi.ajp.2009.08050724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Liddle EB, et al. Task-related default mode network modulation and inhibitory control in ADHD: effects of motivation and methylphenidate. J Child Psychol Psychiatry. 2011;52:761–771. doi: 10.1111/j.1469-7610.2010.02333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gordon EM, et al. Effect of dopamine transporter genotype on intrinsic functional connectivity depends on cognitive state. Cereb Cortex. 2011 doi: 10.1093/cercor/bhr305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Utz KS, et al. Electrified minds: transcranial direct current stimulation (tDCS) and galvanic vestibular stimulation (GVS) as methods of non-invasive brain stimulation in neuropsychology--a review of current data and future implications. Neuropsychologia. 2010;48:2789–2810. doi: 10.1016/j.neuropsychologia.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 87.DaSilva AF, et al. Electrode positioning and montage in transcranial direct current stimulation. J Vis Exp. 2011 doi: 10.3791/2744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zaghi S, et al. Noninvasive brain stimulation with low-intensity electrical currents: putative mechanisms of action for direct and alternating current stimulation. Neuroscientist. 2010;16:285–307. doi: 10.1177/1073858409336227. [DOI] [PubMed] [Google Scholar]
- 89.Pena-Gomez C, et al. Modulation of large-scale brain networks by transcranial direct current stimulation evidenced by resting-state functional MRI. Brain Stimul. 2011 doi: 10.1016/j.brs.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Polania R, et al. Modulating cortico-striatal and thalamo-cortical functional connectivity with transcranial direct current stimulation. Hum Brain Mapp. 2011 doi: 10.1002/hbm.21380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Keeser D, et al. Prefrontal transcranial direct current stimulation changes connectivity of resting-state networks during fMRI. J Neurosci. 2011;31:15284–15293. doi: 10.1523/JNEUROSCI.0542-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cox CL, et al. Your resting brain CAREs about your risky behavior. PLoS ONE. 2010;5:e12296. doi: 10.1371/journal.pone.0012296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Di Martino A, et al. Autistic traits in neurotypical adults are related to cingulo-insular functional connectivity. Am J Psychiatry. 2009;166:891–899. doi: 10.1176/appi.ajp.2009.08121894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Koyama MS, et al. Resting-state functional connectivity indexes reading competence in children and adults. J Neurosci. 2011;31:8617–8624. doi: 10.1523/JNEUROSCI.4865-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Chabernaud C, et al. Dimensional brain-behavior relationships in children with Attention-Deficit/Hyperactivity Disorder. Biol Psychiatry. 2011 doi: 10.1016/j.biopsych.2011.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Alon G, et al. Non-invasive electrical stimulation of the brain (ESB) modifies the resting-state network connectivity of the primary motor cortex: A proof of concept fMRI study. Brain Res. 2011;1403:37–44. doi: 10.1016/j.brainres.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 97.O'Connell NE, et al. Non-invasive brain stimulation techniques for chronic pain. A report of a Cochrane systematic review and meta-analysis. Eur J Phys Rehabil Med. 2011;47:309–326. [PubMed] [Google Scholar]
- 98.Di Martino A, et al. Functional connectivity of human striatum: a resting state fMRI study. Cereb Cortex. 2008;18:2735–2747. doi: 10.1093/cercor/bhn041. [DOI] [PubMed] [Google Scholar]
- 99.Zhang D, et al. Intrinsic functional relations between human cerebral cortex and thalamus. J Neurophysiol. 2008;100:1740–1748. doi: 10.1152/jn.90463.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Buckner RL, et al. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:2322–2345. doi: 10.1152/jn.00339.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]