SUMMARY
In this series of patients, the underlay or overlay positioning of a graft achieves successful outcome for both repair of perforation and hearing function, with better hearing gain in the underlay group. In myringoplasty, the two most common techniques for positioning the graft relative to the remnant of both the tympanic membrane and the annulus are the "overlay" and the "underlay" techniques. 115 patients who underwent myringoplasty for tympanic membrane perforation secondary to chronic otitis media and/or trauma were included, and hearing function was evaluated. We prefer an overlay technique in subtotal perforations, in those involving the anterior and antero-inferior parts of the ear drum with respect to the handle of the malleus and in revision surgery. We reserve an underlay technique for smaller perforations and for those limited to the posterior part of the tympanic membrane. Of 115 cases, 63 underwent an overlay myringoplasty and 52 underlay myringoplasty. In the former group, five cases were anatomically unsuccessful, whereas in the second group there were three failures. The air bone gap improved significantly in both groups with a better hearing gain in the underlay group.
KEY WORDS: Tympanic membrane perforation, Surgery, Healing, Hearing function
RIASSUNTO
Le due principali tecniche di miringoplastica sono l'underlay e l'overlay, che differiscono per i rapporti che l'innesto contrae con l'anulus e i residui della membrana del timpano. Abbiamo valutato la guarigione e i risultati funzionali di 115 pazienti sottoposti a miringoplastica per otite media cronica e perforazione post-traumatica della membrana timpanica. La miringoplastica overlay è stata preferibilmente effettuata per le perforazioni subtotali, per quelle che interessano i quadranti anteriori e nelle revisioni. La tecnica underlay è stata impiegata, invece, per il trattamento delle perforazioni più piccole e per quelle dei quadranti posteriori. Nella nostra casistica 63 pazienti sono stati sottoposti a miringoplastica con tecnica overlay e 52 con tecnica underlay. Abbiamo registrato 5 insuccessi nel primo gruppo e 3 nel secondo. Il guadagno uditivo è stato significativo in entrambi i gruppi sebbene maggiore nel gruppo di pazienti trattati con tecnica underlay. Concludendo nella nostra casistica, mediante le miringoplastiche underlay e overlay abbiamo ottenuto un'alta percentuale di successo sia come guarigione che come guadagno uditivo, quest'ultimo più accentuato nel gruppo underlay.
Introduction
Perforation of the tympanic membrane primarily results from middle ear infections, trauma or iatrogenic causes. Up to 80% of these perforations heal spontaneously 1; for the remaining, surgical repair, known as myringoplasty, is usually proposed. Introduced by Berthold 2, myringoplasty was further developed by Wullstein 3 and Zollner 4. The principal indications are recurrent otorrhea, the desire to swim without having to waterproof the ear and to improve conductive hearing loss.
Several factors may affect surgical outcome such as the surgical approach (endaural, postaural) and technique (underlay vs. overlay), site of perforation and type of graft utilized.
The surgical technique is better is still matter of debate. The two classical techniques that have been developed are the "underlay" and the "overlay" procedures. The former is widely used and relatively simple to perform as the graft is placed entirely medial to the remaining drum and malleus. This technique is ideal to repair small and easily visualized perforations, blunting and lateralization of the graft are avoided, the drum heals at the correct level relative to the annulus and the ossicles and it is quick and easy to perform. On the other hand, its disadvantages are that the middle ear space is reduced and adhesions may occur, there is increased failure because of a limited bed size for the graft supplying poor vascularity, exposure of the middle ear is relatively limited and it is not the ideal technique for perforations extending into the anterior annulus since placement of the graft is difficult. In contrast, the overlay technique is more challenging and typically reserved for total perforations, anterior perforations, or failed underlay surgery. In the overlay technique, the graft is placed lateral to the annulus and any remaining fibrous middle layer after the squamous layer has to be carefully removed. In this technique, there is an excellent visualization of the anterior meatal recess, which is important in cases of anterior perforations reaching the anterior annulus. In addition, the healing rate is high because the drum is essentially replaced intact and the middle ear space is not reduced. The most serious disadvantages are blunting of the anterior meatal recess, the lateralization of the graft and the iatrogenic cholesteatoma; moreover, this technique is more laborious and the healing time is longer.
However, there is still uncertainty about the prognostic factors in myringoplasty, and there are significant variations in the reported success rates for achieving an intact tympanic membrane after surgery. Furthermore, it is now becoming apparent that re-perforation following myringoplasty may occur several years after the initial surgery 5. The aim of this study was to investigate differences in the success of the two myringoplasty techniques of using the temporalis fascia, and to assess the advantages and disadvantage of both techniques.
Materials and methods
The charts of all patients who underwent ear surgery at our institution from January 2004 to December 2008 were reviewed with institutional review board approval. All cases with cholesteatoma, tympanosclerosis, ossicular chain disorders and revision or combined procedures, e.g. mastoidectomy and ossiculoplasty, were excluded.
The review was conducted on 115 ears with a tympanic membrane perforation. Patients were selected regardless of type of procedure, sex, age, cause of perforation, side, size, location and hearing level.
We treated 115 ears in a general population of 54 female patients and 61 male patients with a median age of 36.2 years (range 10-74 years; SD 14.7). The cause of perforation was infection in 104 (90.4%) cases and trauma in the remaining 11 patients. All the ears at the time of surgery were dry.
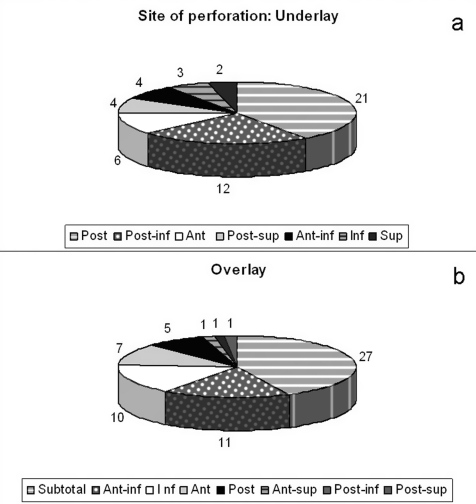
The underlay technique was used in 52 patients (28 males, 24 females) with age ranging from 10 to 69 years (mean 33.4; SD 15.1). The primary causes of disease were infection (46 cases, 88.5%) and trauma (6 cases). In 3 patients we performed revision surgery for residual perforation. The right ear was involved in 30 cases (57.7%) and the left ear in the remaining 22 patients. In relation to the handle of the malleus, perforation was noted in the posterior (21 ears, 40.4%), postero-inferior (12 ears, 23.0%), anterior (6 ears, 11.5%), postero-superior (4 ears, 7.7%), antero-inferior (4 ears, 7.7%), inferior (3 ears, 5.7%) and superior (2 ears, 3.8%) parts of the tympanic membrane (Fig. 1a).
Fig. 1.
Distribution according to site of perforation in the underlay (a) and overlay (b) groups.
The overlay technique was used in 63 patients (33 males, 30 females) with age ranging from 15 to 74 years (mean 38.5; SD 14.0). The leading causes of disease were infection (58 cases, 92.0%) and trauma (5 cases). In 8 patients we performed a revision surgery for a residual perforation. The right ear was involved in 28 cases (44.4%) and the left ear in the remaining 35 subjects. In relation to the handle of the malleus, perforation involved more than 50% of the tympanic membrane (sub-total) in 27 ears (42.8%) and was noted in the antero-inferior (11 ears, 17.4%), inferior (10 ears, 15.8%), anterior (7 ears, 11.1%), posterior (5 ears, 40.4%), antero-superior, postero-inferior and postero-superior (1 ear each, 1.5%) (Fig. 1b). Four patients were lost to follow-up and were not included in the analysis.
Outcomes were measured for healing, complications and post-operative hearing. Healing was categorized as perforated or healed. Functional results were recorded at the last follow-up examination. Audiological evaluation was carried out using a tonal audiometric test. Air conduction (AC) and bone conduction (BC) pure-tone average (PTA) values were calculated as the mean of 0.5-, 1-, 2- and 4 kHz thresholds. Air-bone gaps (ABG) were obtained from ACPTA and BCPTA thresholds. Finally, postoperative hearing gain was calculated from the ABG before the operation minus the ABG of the last follow-up examination. A hearing gain of at least 10 dB was considered clinically relevant. A high-frequency PTA of 1, 2, and 4 kHz was computed from preoperative and postoperative BC thresholds to evaluate sensorineural hearing loss (SNHL). Preoperative variables that could affect outcomes were also evaluated, including age and sex of patients, cause of tympanic membrane disease, and the size and location of the perforation.
Statistical analysis
The distribution of age, pre-operative ACPTA and preoperative BCPTA was estimated using a Kolmogorov- Smirnov test. Given the normal distribution of values, differences between "overlay" and "underlay" patients were assessed using a two-tailed, two-sample Student's t-test. Differences between postoperative and preoperative results were analyzed with a paired t-test. Categorical variables were studied with a chi-square test. To investigate correlations between the surgical technique and outcome measures, a logistic regression analysis was performed, with adjustment for age and gender. Odds ratios are reported with their 95% confidence interval (CI). Statistical significance was accepted at a level of p < 0.05. Statistical analysis was performed with the software package EPI INFO, version 3.3.2 (Atlanta, GA, USA).
Results
The underlay and the overlay groups were matched for age and gender. Without regard to the technique, surgery was associated with successful healing in 92.7% of cases, and in hearing improvement in 75.7% of patients.
Underlay group
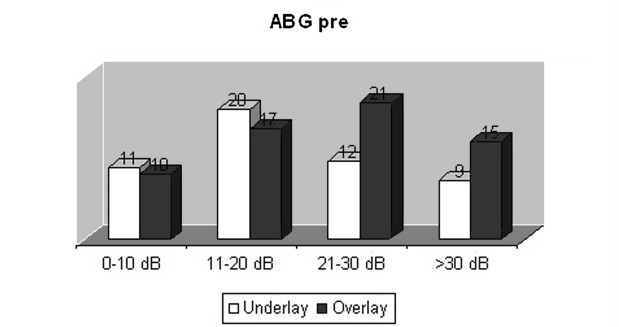
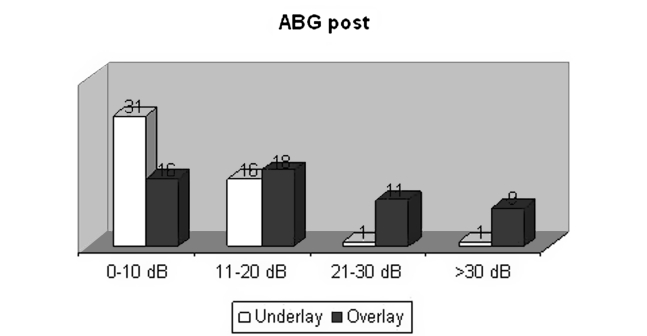
The underlay technique resulted in a 94.2% (49 cases) success rate: postoperative perforation was noted in three cases; in all three patients, the perforation involved the anterior parts of the tympanic membrane. Some patients developed granulation tissue during the healing process, which resolved with topic applications of boric acid and antibiotics. Preoperatively, the mean ACPTA was 37.9 dB, the BCPTA was 18.3 dB and the ABGPTA was 19.1 dB: for 11 patients, the ABGPTA was ≤ to 10 dB (22.4%), for 18 was from 11 to 20 dB (36.7%), for 11 from 21 to 30 dB (36.7%) and for 9 was > 30 dB (18.3%) (Fig. 2). At follow up examination (on average 17.6 months), the mean ACPTA was 26.6 dB, the BCPTA was 16.6 dB and the ABGPTA was 9.9 dB: for 31 patients the ABGPTA was ≤ 10 dB (63.2%), for 16 was from 11 to 20 dB (32.6%), for 1 from 21 to 30 dB (0.6%) and for 1 > 30 dB (0.6%) (Fig. 3). The BCPTA at 1, 2 and 4 kHz decreased after surgery to 19.2 dB from a preoperative level of 20.6 dB. Paired T-test showed a significant ABGPTA reduction after surgery (mean pre-op ABGPTA = 19.57 ± 10.24 dB; mean post-op ABGPTA = 9.93 ± 6.6 dB; p < 0.001). Hearing improvement was achieved in 44 patients (89.8%): the mean hearing gain was 11.2 dB with a range between 1-30; in 1 patient hearing function remained stable; only 4 patients (8.2%) experienced worsening of the hearing threshold of 8.5 dB on average. At the last examination, 63.2% of patients showed an ABGPTA less than 10 dB, and 95.9% less than 20 dB. Surgery did not cause any acoustic trauma in this group and the BCPTA decreased by an average of 1.4 dB.
Overlay group
The overlay technique resulted in a 91.5% (54 cases) success rate: postoperative perforation was noted in five cases; in three patients, the perforation was subtotal and in the remaining two it involved the antero-inferior part of the tympanic membrane. The development of granulation tissue during the healing process was greater than with the underlay technique and the healing period was also longer. These patients were also treated effectively with topical medications. In this group, we noted an anterior blunting and/or a graft lateralization in 4 cases (6.3%). Concerning hearing function, preoperatively the mean ACPTA was 42.7 dB, the BCPTA was 19.8 dB and the ABGPTA was 22.3 dB: for 8 patients, the ABGPTA was ≤ 10 dB (14.8%), for 16 was from 11 to 20 dB (29.6%), for 17 from 21 to 30 dB (31.4%) and for 13 was> 30 dB (24.0%) (Fig. 2). At follow up examination (on average 21.8 months), the mean ACPTA was 38.4 dB, the BCPTA was 20.6 dB and the ABGPTA was 17.5 dB: for 16 patients, the ABGPTA was ≤ 10 dB (29.6%), for 18 was from 11 to 20 dB (33.3%), for 11 from 21 to 30 dB (20.3%) and for 9 was> 30 dB (16.6%) (Fig. 3). Moreover, we observed a very slight decrease of the BCPTA at 1, 2 and 4 kHz after surgery (22 dB preoperatively and 23.3 postoperatively). Paired T-test showed a significant reduction in ABGPTA after surgery (mean pre-op ABGPTA = 22.33 ± 10.27 dB; mean post-op ABGPTA = 17.57 ± 10.22 dB; p = 0.02). Hearing improvement was achieved in 40 patients (74%): the mean hearing gain was 10,3 dB with a range between 1-31; in 1 patient, hearing function remained stable; 13 patients (24%) experienced worsening of the hearing threshold by a mean of 12.7 dB. At the last examination, 29.6% of patients showed an ABGPTA< 10 dB and 62.9% < 20 dB. A slight decrease of 1.3 dB was observed for the BCPTA.
Fig. 2.
Preoperative distribution of ABG in four classes for each study group.
Fig. 3.
Postoperative distribution of the ABG in four classes for each study group.
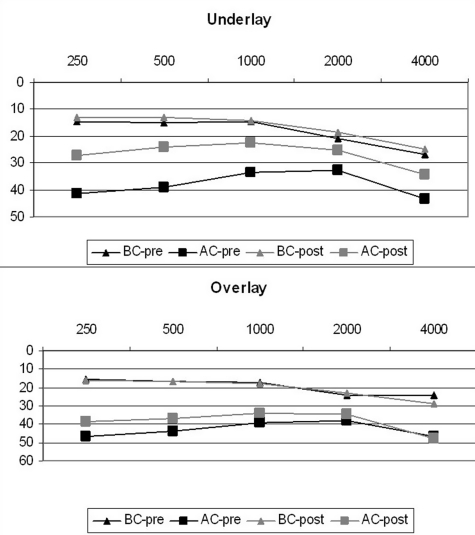
Figure 4 shows the median variation of AC and BC for each frequency in both the underlay and overlay groups. The pre-operative air conduction PTA (ACPTA) did not differ significantly between the underlay (mean PTA = 37.96 ± 12.39 dB) and overlay groups (mean PTA = 42.8 ± 18 dB HL; p = 0.12), similar to the Bone Conduction PTA (mean BCPTA in underlay group = 18.31 ± 7.3 dB; mean BCPTA in overlay group = 19.83 ± 7.3 dB; p = 0.456). No significant postoperative BCPTA variations were noticed in the two groups (p> 0.05). The underlay technique was associated with a significantly higher likelihood of achieving ABG closure compared to the overlay technique (chi square p < 0.001, OR = 4.1, 95%CI = 1.7-2.3). Logistic regression analysis adjusted for age and gender demonstrates a higher likelihood of achieving a ≥ 10 dB gain with the underlay technique (OR = 2.512; 95%CI = 1.07- 5.9; p = 0.035). No significant relationship was found between outcome and hearing function and the perforation site or cause.
Fig. 4.
Median variation of AC and BC for each frequency in both the underlay and overlay groups.
Discussion
The ideal reconstructive technique should obtain a thin, conically shaped, vibrating membrane replacing the original ear drum in order to prevent infection and restore or improve hearing. There is still no consensus about the optimal technique, which is often employed on the basis of the surgeon's preference and skills, and not on the type of the tympanic membrane perforation. The main concept that should be pointed out is that the middle ear is part of the upper airway, and that some unsuccessful surgeries, excluding post-traumatic lesions, are due to unsolved underlying pathology of the rhino-tubaric area.
In 1972, Doyle et al. 6 reported on 131 myringoplasty surgeries using both the overlay and underlay techniques. In the overlay technique (52 ears), there was recurrence of perforation in 23% of patients at 1 year and 43% over 2 years. With the underlay technique (79 ears), there was recurrence of perforation in 17% of patients at 1 year and 12% after 3 years. Glasscock 7 reported a 91% success rate using the overlay technique and a 96% success rate with the underlay technique in a total of 273 ears. Sheehy and Anderson 8 reported a 97% take rate in 472 overlay myringoplasty surgeries. Rizer 9 reported a success rate of 95.6% in 554 overlay grafts and 88.8% in 158 underlay grafts. Gibb and Chang 10 and Packer et al. 11 have reported a high success rate of revision myringoplasty as being high, and similar to that of primary surgery. Others have shown a success rate of 59% in revision myringoplasty 12. Recently, Wang and Lin 13 published a retrospective study in which they achieved a 82.1% and a 85% take rate with the overlay and the underlay techniques, respectively. Our outcomes are similar to those reported by Doyle 6 and Glasscock 7, but inconsistent with those of Sheehy 8 and Rizer 9.
In our series, we achieved a high grade of success with both techniques (overall healing rate was 92.7%), although the underlay technique was slightly better than the overlay technique in terms of tympanic membrane closure (94.2% vs. 91.5%). The incidence of unexpected residual perforation was similar in both groups, but the three cases in the underlay group, which involved always the anterior portion, would suggest that an overlay should be performed
in such perforations. The onset of complications was not significantly different between the two techniques: we observed a longer healing time in the overlay group due to the surgical manipulation which led to the development of a larger amount of granulation tissue. In contrast with other series 6 7, concerning the overlay technique, we did not observe more cases of anterior blunting, graft lateralization, thickening of the drum, iatrogenic cholesteatoma or post-inflammatory ear canal stenosis. We attribute the good results with the overlay technique to the use of a postauricular approach and to the adequate drilling of the bone of the external auditory canal, especially the anterior bulge, thus improving the exposure of the anterior remnant and preventing the anterior blunting. We always completely remove the tympanic membrane remnant and the skin of the ear canal that could cause epithelial pearls or develop iatrogenic cholesteatoma. The fascia is placed exactly onto the bony annulus after having obtained a good haemostasis and with just a little overriding onto the canal wall it is anchored to the malleus to avoid lateralization and blunting of the graft. Finally, we use packing in the ear canal from the anterior part with narrow strips of Gelfoam ® to reinforce the anterior aspect of the ear drum.
The high success achieved with the underlay technique is probably due to the reduced surgical manipulation of middle ear structures and to faster healing which minimizes the bias related to occasional otologic surgeons. Patient selection may also have had a role in the high success rate of our series: we excluded patients with severe disease presenting with mastoid or ossicular signs of pathology.
Concerning functional results, it is still debated if myringoplasty should be offered to patients to improve hearing 14. Singh et al. 15 reported a 93.3% success rate for each technique and a better hearing gain (92.8% vs. 57.1%) for patients treated with the underlay technique. Similar results have been reported by other authors who achieved a better success rate and hearing function improvement with the underlay technique 11. In underlay patients, however, ABG closure was not always achieved and one of the reasons for residual conductive deafness after a successful graft using the underlay technique may be that the neo-tympanic membrane is not as mobile as the normal one, thereby increasing the impedance of the middle ear. A prospective study revealed a mean value for hearing improvement in only 52% of all patients, and significant postoperative hearing improvement in 67% of patients in whom the procedure was performed to improve hearing 16. Bhat and De 17, in a smaller study, found an overall hearing improvement of 59%. Black et al. 18 and Perkins et al. 19 reported, respectively, 77.9 and 97% postoperative hearing improvement. Karela 20 reported on a series of 211 patients operated on an underlay myringoplasty for any size and site of perforation, achieving a 91.5% success rate and a mean improvement in hearing function by 14.67 dB in 91.5% of patients. These authors stated that myringoplasty can improve hearing independent of the site and size of perforation, and support that the hearing improvement can be used as an indication for myringoplasty.
In our series, both techniques were associated with significant improvement in ABGPTA. However, the underlay technique appears to achieve a higher gain than the overlay technique (higher degree of significance), as confirmed by logistic regression analysis which showed a significant correlation between underlay technique and a ≥ 10 dB gain likelihood. Poorer hearing results after the overlay technique could be due to a subclinical lateralization of the graft, fixation of incudomalleolar joint in attic due to surgical manipulation, acoustic trauma due to the larger amount of manipulation to remove the remnant and to more extensive drill use.
The optimal results achieved with the underlay technique (better hearing gain, no complications) suggest that this technique should be more widely used, although it is possible that in cases of larger and anterior perforations the overlay technique, even with poorer functional results, ensures a higher degree of uptake. In fact, there were three cases of unexpected residual perforation in the underlay group, and the anterior part of the tympanic membrane was always involved.
Conclusions
Myringoplasty is a safe and effective technique to improve the quality of life of patients, avoiding continuous infections and allowing them contact with water. It is our belief that to achieve the best results a well-trained ear surgeon must be familiar with both underlay and overlay techniques, which should be employed based on the site of perforation, and the surgeon's preference.
References
- 1.Galdstone HB, Jackler RK, Varav K. Tympanic membrane wound healing. An overview. Otolaryngol Clin North Am. 1995;28:913–932. [PubMed] [Google Scholar]
- 2.Berthold E. Ueber myringoplastik. Wier Med Bull. 1878;1:627–627. [Google Scholar]
- 3.Wullstein H. Theory and practice of myringoplasty. Laryngoscope. 1956;66:1076–93. doi: 10.1288/00005537-195608000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Zollner F. The principles of plastic surgery of the sound-conducting apparatus. J Laryngol Otol. 1955;69:637–652. [PubMed] [Google Scholar]
- 5.Aggarwal R, Saeed SR, Green KJ. Myringoplasty. J Laryngol Otol. 2006;120:429–432. doi: 10.1017/S0022215106000697. [DOI] [PubMed] [Google Scholar]
- 6.Doyle JP, Schleuning AJ, Echevarria J. Myringoplasty: should grafts be placed medial or lateral to the tympanic membrane? Laryngoscope. 1972;82:1425–1430. doi: 10.1288/00005537-197208000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Glasscock ME III. Tympanic membrane grafting with fascia: overlay vs undersurface technique. Laryngoscope. 1973;83:754–770. doi: 10.1288/00005537-197305000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Sheehy JL, Anderson RG. Myringoplasty: a review of 472 cases. Ann Otol Rhinol Laryngol. 1980;89:331–334. doi: 10.1177/000348948008900407. [DOI] [PubMed] [Google Scholar]
- 9.Rizer FM. Overlay versus underlay myringoplasty. Part II: the study. Laryngoscope. 1997;107:26–36. doi: 10.1097/00005537-199712001-00002. [DOI] [PubMed] [Google Scholar]
- 10.Gibb AG, Chang S-K. Myringoplasty (a review of 365 operations) J Laryngol Otol. 1982;96:915–930. doi: 10.1017/s0022215100093270. [DOI] [PubMed] [Google Scholar]
- 11.Packer P, Mackendrick A, Solar M. What's best in myringoplasty: underlay or overlay, dura or fascia. J Laryngol Otol. 1982;96:25–41. doi: 10.1017/s0022215100092203. [DOI] [PubMed] [Google Scholar]
- 12.Halik JJ, Smyth GDL. Long-term results of tympanic membrane repair. Otolaryngol Head Neck Surg. 1988;98:162–169. doi: 10.1177/019459988809800211. [DOI] [PubMed] [Google Scholar]
- 13.Wang WH, Lin YC. Minimally invasive inlay and underlay myringoplasty. Am J Otolaryngol. 2008;29:363–366. doi: 10.1016/j.amjoto.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Lee P, Kelly G, Mills RP. Myringoplasty: does the size of the perforation matter? Clin Otolaryngol Allied Sci. 2002;27:331–334. doi: 10.1046/j.1365-2273.2002.00590.x. [DOI] [PubMed] [Google Scholar]
- 15.Singh M, Rai A, Bandyopadhyay S, et al. Comparative study of the underlay and overlay techniques of myringoplasty in large and subtotal perforations of the tympanic membrane. J Laryngol Otol. 2003;117:444–448. doi: 10.1258/002221503321892262. [DOI] [PubMed] [Google Scholar]
- 16.Kotecha B, Fowler S, Topham J. Myringoplasty: a prospective audit study. Clin Otolaryngol Allied Sci. 1999;24:126–129. doi: 10.1046/j.1365-2273.1999.00227.x. [DOI] [PubMed] [Google Scholar]
- 17.Bhat NA, De R. Retrospective analysis of surgical outcome, symptom changes, and hearing improvement following myringoplasty. J Otolaryngol. 2000;29:229–232. [PubMed] [Google Scholar]
- 18.Black JH, Wormald PJ. Myringoplasty-effects on hearing and contributing factors. S Afr Med J. 1995;85:41–43. [PubMed] [Google Scholar]
- 19.Perkins R, Bui HT. Tympanic membrane reconstruction using formaldehyde-formed autogenous temporalis fascia: twenty years' experience. Otolaryngol Head Neck Surg. 1996;114:366–379. doi: 10.1016/s0194-5998(96)70205-x. [DOI] [PubMed] [Google Scholar]
- 20.Karela M, Sandeep B, Watkins A, et al. Myringoplasty: surgical outcomes and hearing improvement: is it worth performing to improve hearing? Eur Arch Otorhinolaryngol. 2008;265:1039–1042. doi: 10.1007/s00405-007-0570-z. [DOI] [PubMed] [Google Scholar]