Abstract
Background
Numerous videokeratographic methods are used in the diagnosis of keratoconus. The purpose of this study was to compare the sensitivity and specificity of the KISA% index with the keratometry (K) value, inferior-superior (I-S) value, relative skewing of the steepest radial axes (SRAX), and keratometric astigmatism (AST) indices in 25 patients presenting with bilateral keratoconus.
Methods
Twenty-five patients presenting with bilateral keratoconus were enrolled. Fifty eyes from 25 healthy individuals without corneal abnormalities were used as controls. The clinical diagnosis of keratoconus was made by observation of scissors reflex at retinoscopy and characteristic slit lamp findings. Corneal topographic analysis was performed in each eye to calculate the K value, I-S value, AST, and SRAX indices.
Results
The keratoconus percentage index (KISA%) was significantly more sensitive and specific than the other indices examined. Furthermore, it was significantly better at predicting positive and negative results than the other indices included in the study.
Conclusion
The current research suggests that KISA% could be used to detect/diagnose keratoconus but further studies are required to confirm the specificity and sensitivity of KISA% for the detection of early-stage disease and keratoconus suspects.
Keywords: cornea, keratoconus, KISA% index
Introduction
Keratoconus, a degenerative disorder characterized by thinning of the cornea, can result in substantial distortion of vision. Clinical diagnosis should involve researching a patient’s medical history, refraction, keratometry, and slit-lamp examination to evaluate the status of the cornea.1 Corneal topography, also known as photokeratoscopy or videokeratography, is a noninvasive imaging technique used to map the surface curvature of the cornea.2 It has been argued that topography should be used in conjunction with manual keratometry and not as an alternative.1 However, it has been demonstrated that corneal topography provides a more definitive diagnosis, detecting the disorder during the early stages despite normal results after slit-lamp examination and keratometry,3 that it can be used to detect keratoconus suspects,4 and it is considered obligatory for pre-operative evaluation before refractive surgery is carried out.5
Mathematical indices are used to determine the disorder with high specificity and sensitivity.5 Solis-Vivanco et al compared corneal topography with clinical diagnosis, which serves as the gold standard, reporting that topography indices had a sensitivity of 87% and a specificity of 92% in terms of diagnosing keratoconus.6 Using a combination of four topography indices, namely the central keratometry (K) value, the inferior-superior (I-S) value, relative skewing of the steepest radial axes (SRAX), and keratometric astigmatism (AST), Rabinowitz demonstrated that corneal topography yielded a false-positive rate of 0.5% and false-negative rate of 2.5% in the diagnosis of keratoconus.7
It has been reported that no single videokeratoscopic index is capable of discriminating between groups of individuals with clinical signs of disease and first-degree relatives of patients with keratoconus.8 However, a study carried out by Rabinowitz and Rasheed compared a new index, keratoconus percentage index (KISA%), derived from the aforementioned topographic parameters (K value, I-S value, SRAX, and AST) with modified Rabinowitz/McDonnell (K value and I-S value) and Maeda/Klyce (keratoconus prediction index [KCI] and KCI%) indices, and demonstrated that with a cut-off value of 100%, KISA% yielded an improvement in the rate of correct diagnosis (99.6%).9 In order to further elucidate the diagnostic accuracy of the KISA% index, the present study compared the K value, I-S value, SRAX, and AST corneal topographic indices in 25 individuals suffering from bilateral keratoconus.
Materials and methods
Twenty-five patients presenting with bilateral keratoconus between April and December 2007 were enrolled in the study. Informed consent was obtained, and the subjects’ age, gender, family history, past medical history, and details of ophthalmologic surgery were recorded. The inclusion criterion was clinical detection of keratoconus, and exclusion criteria were recent history of contact lens use, past history of eye surgery, and the presence of a corneal ulcer or other corneal diseases.10,11 Fifty eyes from 25 healthy individuals without corneal abnormalities were used as controls. All subjects were subjected to examination by slit-lamp, and direct ophthalmoscopic and retinoscopic examinations. The clinical diagnosis of keratoconus was made by observation of scissors reflex at retinoscopy and characteristic slit lamp findings, eg, Fleischer ring and Vogt’s striae.12–14 Using an EyeSys videokeratoscope (VK EyeSys Laboratories, Houston, TX), corneal topographic analysis was performed in each eye to calculate the K value, I-S value, AST, and SRAX indices. KISA% was calculated using the following formula:
Absolute values were used in the calculation and values less than one were replaced with a value of one. K values less than 47.2 D were replaced with a value of one and those greater than 47.2 D were replaced with (K −47.2) as detailed in Rabinowitz and Rasheed.9
Data were expressed as the mean ± standard deviation. Statistical analyses were performed using SPSS for Windows (v 11.0; SPSS Inc, Chicago, IL) using the independent samples t-test and Pearson’s Chi-square test. Statistical significance was accepted at P < 0.05. Cut-off values of variables (K value >47.2 D, I-S value >1.4 D, AST > 1.5 D, SRAX index >21°, KISA% > 100%) reported by Rabinowitz7 and Rabinowitz and Rasheed9 for the determination of keratoconus were used to calculate the sensitivity, specificity, and positive and negative predictive values for each variable in the diagnosis of keratoconus. According to the aforementioned cut-off values of the variables, a positive predictive value was defined as the proportion of patients with positive test results who were correctly diagnosed based on the clinical diagnosis of keratoconus. Moreover, a negative predictive value was defined as the proportion of patients with negative test results that were correctly diagnosed.9,15
Results
The mean age of the patients was 25.84 ± 7.04 years and the mean age of the control group was 24.84 ± 6.08 years (P = 0.449). Male:female ratios were 11:14 in the keratoconus group and 13:12 in the control group; both groups were sex-matched (Chi-square test, P = 0.571). The K value, I-S value, SRAX index, and KISA% were higher in the experimental group than the control group, but the I-S value and SRAX index demonstrated greater variation among keratoconus patients (Table 1). There were no statistically significant differences between the K value, I-S value, AST, SRAX indices, and KISA% among patients with respect to gender (P > 0.1).
Table 1.
Topographic index values
| Patients | Control | P value | |
|---|---|---|---|
| K value | 54.68 ± 8.78 | 46.48 ± 1.78 | <0.01 |
| I-S value | 5.62 ± 7.04 | 1.91 ± 1.12 | <0.001 |
| AST | 4.92 ± 2.81 | 4.26 ± 2.41 | 0.209 |
| SRAX | 13.88 ± 18.68 | 5.32 ± 6.41 | 0.003 |
| KISA% | 10126.67 ± 13662.47 | 21.35 ± 16.63 | <0.01 |
Abbreviations: K, keratometry; I-S, inferior-superior; AST, keratometric astigmatism; SRAX, relative skewing of the steepest radial axes; KISA%, keratoconus percentage index.
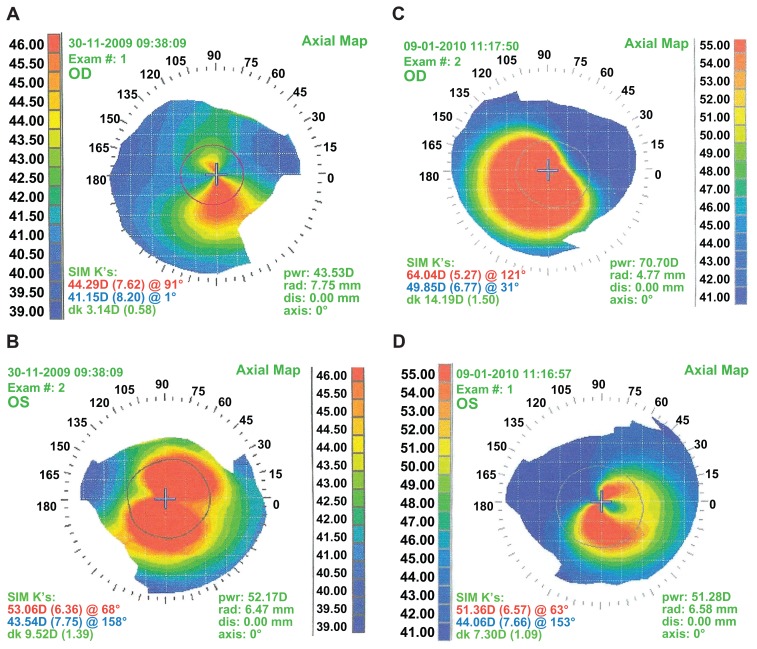
Several topographic indices have been developed for the determination of keratoconus. Comparing the sensitivity and specificity of each of the studied topographic indices revealed that while the K value and AST demonstrated >80% sensitivity and the SRAX demonstrated >90% specificity, SRAX and AST indices had the lowest sensitivity and specificity, respectively. KISA% was the only index with specificity and sensitivity >90% (Table 2). Furthermore, KISA% was the only index demonstrating positive and negative predictive values >95%. Corneal topography images of two patients with keratoconus are shown in Figure 1A–D.
Table 2.
Measured parameters of topographic indices
| Variable | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|
| K value | 82 | 68 | 71.93 | 79.09 |
| I-S value | 74 | 38 | 54.41 | 59.38 |
| AST | 88 | 10 | 49.44 | 45.45 |
| SRAX | 24 | 96 | 85.71 | 55.81 |
| KISA% | 96 | 100 | 100 | 96.15 |
Abbreviations: K, keratometry; I-S, inferior-superior; AST, keratometric astigmatism; SRAX, relative skewing of the steepest radial axes; KISA%, keratoconus percentage index.
Figure 1.
Corneal topography images of patient 1 (A) right eye and (B) left eye and patient 2 (C) right eye and (D) left eye.
Discussion
Corneal topography is effective in the early diagnosis of keratoconus, irrespective of clinical symptoms,3 and when compared to clinical examination has been reported to have a sensitivity of 87% and a specificity of 92% in terms of diagnosing the disorder.6 However, this study demonstrates that there is great variation among different indices in terms of the sensitivity, specificity, and the ability to predict positive and negative values. Therefore, studies concerning the determination of keratoconus or keratoconus suspects usually use combined topographical indices to confirm the presence of the disorder.4,7
In the present study, the SRAX index demonstrated the lowest sensitivity, the AST index had the lowest specificity, and the K and I-S values were also associated with low specificity. These results suggest that using a single topographic index for the determination of keratoconus would result in variation of diagnosis, ie, higher rates of false positive and/or false negative diagnosis than using multiple indices for assessment of patients. However, the KISA% index demonstrated sensitivity and specificity of 96% and 100%, respectively, in terms of keratoconus diagnosis. These results are comparable to those reported in the study carried out by Rabinowitz and Rasheed,9 who demonstrated that with a cut-off value of 100%, KISA% determined the correct diagnosis in 99.6% of cases.
It is tempting to suggest that the KISA% index should be used in place of other topographical indices such as the K value, I-S value, SRAX, and AST, used alone or in combination. However, data from a study carried out by Li et al16 in which the K value, I-S value, and KISA% indices were used to detect keratoconus in a group of normal individuals, keratoconus suspects, and a group of patients with early keratoconus, reported a total classification rate of 68.9%. Therefore, although the present study demonstrates that the KISA% index is significantly more sensitive and specific than other topographical indices, further research is required to confirm this conclusion in early-stage disease and suspected cases of keratoconus with no clinical symptoms. Until that time, KISA% should be used in combination with other indices for the diagnosis and detection of keratoconus.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nordan LT. Keratoconus: diagnosis and treatment. Int Ophthalmol Clin. 1997;37(1):51–63. doi: 10.1097/00004397-199703710-00005. [DOI] [PubMed] [Google Scholar]
- 2.Missotten L. Corneal topography. Curr Opin Ophthalmol. 1994;5(4):68–74. doi: 10.1097/00055735-199408000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Maguire LJ, Bourne WM. Corneal topography of early keratoconus. Am J Ophthalmol. 1989;108(2):107–112. doi: 10.1016/0002-9394(89)90001-9. [DOI] [PubMed] [Google Scholar]
- 4.Claude S, Verdier R, Arnaud B, Schmitt-Bernard CF. Accuracy of videokeratographic quantitative criteria for detection of keratoconus suspects in families with keratoconus. J Fr Ophtalmol. 2004;27(7):773–778. doi: 10.1016/s0181-5512(04)96212-2. [DOI] [PubMed] [Google Scholar]
- 5.Dumitrica DM, Colin J. Indices for the detection of keratoconus. Oftalmologia. 2010;54(2):19–29. [PubMed] [Google Scholar]
- 6.Solis-Vivanco A, Hernandez-Quintela E, Fromow-Guerra JJ, Cruz-Sanchez A, Ponce-de-Leon S, Naranjo-Tackman R. Corneal topography as a screening method for keratoconus suspects. Invest Ophthalmol Vis Sci. 2002;43:e-Abst 172. [Google Scholar]
- 7.Rabinowitz YS. Videokeratographic indices to aid in screening for keratoconus. J Refract Surg. 1995;11(5):371–379. doi: 10.3928/1081-597X-19950901-14. [DOI] [PubMed] [Google Scholar]
- 8.Mato JL, Lema I, Díez-Feijoo E. Videokeratoscopic indices in relation to epidemiological exposure to keratoconus. Graefes Arch Clin Exp Ophthalmol. 2010;248(7):991–998. doi: 10.1007/s00417-010-1332-y. [DOI] [PubMed] [Google Scholar]
- 9.Rabinowitz YS, Rasheed K. KISA% index: a quantitative videokeratography algorithm embodying minimal topographic criteria for diagnosing keratoconus. J Cataract Refract Surg. 1999;25(10):1327–1335. doi: 10.1016/s0886-3350(99)00195-9. [DOI] [PubMed] [Google Scholar]
- 10.Sedghipour MR, Mostafaei A, Taghavi Y. Low-dose subconjunctival bevacizumab to augment trabeculectomy for glaucoma. Clin Ophthalmol. 2011;5:797–800. doi: 10.2147/OPTH.S17896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sedghipour MR, Sorkhabi R, Shenasi A, Dehghan H. Outcome of penetrating keratoplasty in corneal ulcer: a single-center experience. Clin Ophthalmol. 2011;5:1265–1268. doi: 10.2147/OPTH.S22959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krachmer JH, Feder RS, Belin MW. Keratoconus and related noninflammatory corneal thinning disorders. Surv Ophthalmol. 1984;28(4):293–322. doi: 10.1016/0039-6257(84)90094-8. [DOI] [PubMed] [Google Scholar]
- 13.Lee LR, Hirst LW, Readshaw G. Clinical detection of unilateral keratoconus. Aust N Z J Ophthalmol. 1995;23(2):129–133. doi: 10.1111/j.1442-9071.1995.tb00141.x. [DOI] [PubMed] [Google Scholar]
- 14.Leibowitz HM, Waring GO. Corneal Disorders: Clinical Diagnosis and Management. 2nd ed. Philadelphia, PA: WB Saunders; 1998. [Google Scholar]
- 15.Altman DG, Bland JM. Diagnostic tests 2: Predictive values. BMJ. 1994;309(6947):102. doi: 10.1136/bmj.309.6947.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li X, Yang H, Rabinowitz YS. Keratoconus: classification scheme based on videokeratography and clinical signs. J Cataract Refract Surg. 2009;35(9):1597–1603. doi: 10.1016/j.jcrs.2009.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]