Abstract
Experiences of social rejection or loss have been described as some of the most ‘painful’ experiences that we, as humans, face and perhaps for good reason. Because of our prolonged period of immaturity, the social attachment system may have co-opted the pain system, borrowing the pain signal to prevent the detrimental consequences of social separation. This review summarizes a program of research that has explored the idea that experiences of physical and social pain rely on shared neural substrates. First, evidence showing that social pain activates pain-related neural regions is reviewed. Then, studies exploring some of the expected consequences of such a physical-social pain overlap are summarized. These studies demonstrate: 1) that individuals who are more sensitive to one kind of pain are also more sensitive to the other and 2) that factors that increase or decrease one kind of pain alter the other in a similar manner. Finally, what these shared neural substrates mean for our understanding of socially painful experience is discussed.
Keywords: social pain, physical pain, dorsal anterior cingulate cortex, anterior insula, brain, fMRI
Psychologists have long noted the importance of social connection for human survival and have suggested that humans have a fundamental “need to belong” or to be socially connected to others [1–3]. Recent models have attempted to advance this idea further by proposing that, like other basic needs, a lack of social connection may feel “painful.” Specifically, we and others have argued that there may be an overlap in the neural circuitry underlying experiences of physical pain and “social pain”—the painful feelings following social rejection or social loss [4–8].
From an evolutionary perspective, the idea that a lack of social connection feels “painful” makes good sense. As a mammalian species, humans are born relatively immature, without the capacity to feed or fend for themselves and instead rely almost completely on a caregiver to provide care and nourishment. Because of this prolonged period of mammalian immaturity, the social attachment system—which promotes social bonding—may have piggybacked onto the physical pain system, borrowing the pain signal itself to indicate when social relationships are threatened, thus promoting survival [8]. In other words, to the extent that being separated from a caregiver is such a severe threat to survival, being “hurt” by experiences of social separation may be an adaptive way to prevent them.
Indeed, our language provides nice anecdotal evidence for the hypothesis that social and physical pain rely on shared neural circuitry. Specifically, when we describe experiences of social pain—social rejection or social loss—we often do so with physical pain words, complaining of “hurt feelings” or “broken hearts.” In fact, this pattern has been shown to exist across many different languages and is not unique to the English language [8]. Moreover, at least in the English language, we have no other means of expressing these “hurt feelings” other than through the use of physical pain words. Still, linguistic evidence alone does not substantiate the claim that physical and social pain processes overlap. One way to more convincingly demonstrate an overlap in the mechanisms that support physical and social pain processes is to show that they rely on shared neural substrates.
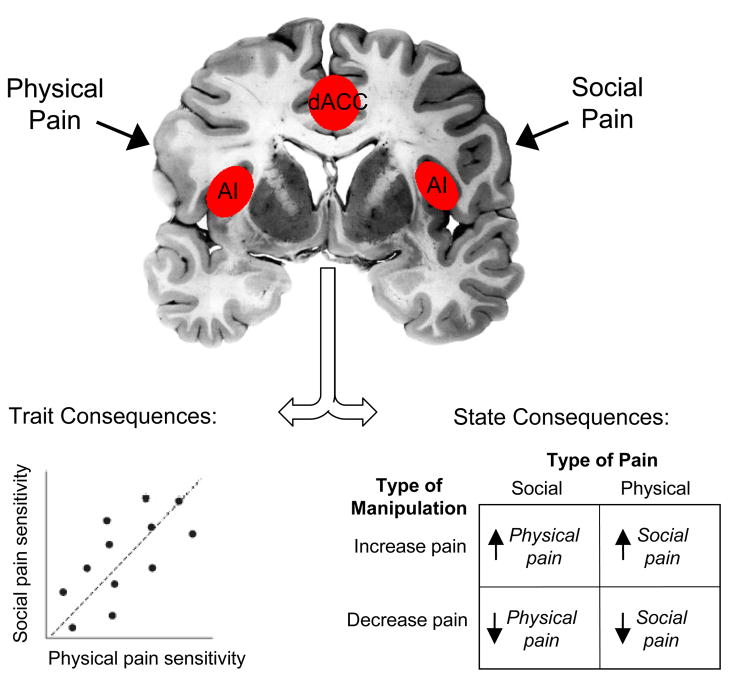
Over the past several years, we have directly investigated the hypothesis that physical and social pain processes overlap using a variety of different methodologies, including behavioral, genetic, and neuroimaging approaches. As a first test of this hypothesis, we have investigated whether experiences of social pain activate neural regions that are typically implicated in physical pain processing. As a second test, we have investigated whether there is evidence for some of the expected consequences of such an overlap. For example, we have explored whether individuals who are more sensitive to one kind of pain are also more sensitive to the other, as individual differences in the functioning of this shared, underlying circuitry should be manifested in both kinds of pain. We have also explored whether altering (increasing or decreasing) one type of painful experience alters the other in a similar manner. Here, I review the evidence accumulated through these investigations (see Figure 1 for a conceptual model). Together, these data support the idea that experiences of social rejection, exclusion, or loss may be described as ‘painful’ because they rely, in part, on pain-related neural circuitry.
Figure 1.
A conceptual model depicting the overlapping neural regions activated by physical and social pain as well as the consequences of this overlap for trait differences in sensitivity to pain (individual differences in physical pain sensitivity should correlate positively with individual differences in social pain sensitivity) and for state differences in sensitivity to pain (factors that increase or decrease one kind of pain should alter the other kind of pain in a congruent manner).
Social Pain Relies on Physical Pain-Related Neural Regions
Physical pain experience can be subdivided into two components, which rely on different neural substrates. These two components include: 1) a sensory component, which codes for the discriminative aspects of pain (e.g., location, intensity, duration) and 2) an affective component, which codes for the unpleasant aspects of pain (e.g., distressing, suffering) [9]. Based on the importance of the affective component of physical pain for signaling a negative state and motivating behaviors aimed at reducing it, we have hypothesized that the affective, rather than the sensory, component of pain would be more critical for understanding feelings of social pain. However, it is possible that the sensory component of pain is involved as well, as somatic complaints can often accompany feelings of social pain [10].
Neural correlates of the affective component of physical pain
Considerable neuropsychological and neuroimaging research has demonstrated that the affective or unpleasant component of physical pain is processed, in part, by the dorsal portion of the anterior cingulate cortex (dACC) and the anterior insula [11–14], whereas the sensory component of pain is processed by the primary and secondary somatosensory cortices (S1, S2) and the posterior insula [11, 15–16]. Thus, chronic pain patients who have undergone cingulotomy—a surgery in which a portion of the dACC is lesioned [17] —report that they can still feel and localize pain sensation (sensory component intact) but that the pain no longer “bothers” them [18–19]. Insular lesions result in similar reductions in emotional responses to painful stimuli [20]. Interestingly, lesions to the somatosensory cortices (S1/S2), associated with the sensory component of pain, disrupt one’s ability to localize painful stimuli but leave the distress of painful experience intact [21].
Neuroimaging studies have largely supported these neuropsychological findings by showing that both the dACC and anterior insula track the affective component of pain. Thus, subjects hypnotized to selectively increase the “unpleasantness” of noxious stimuli (affective component) without altering the intensity (sensory component) showed increased activity in the dACC without altered activity in primary somatosensory cortex (related to the sensory component of pain) [22]. Moreover, self-reports of pain unpleasantness correlate specifically with activity in the dACC [12, 23] and bilateral anterior insular [24]. Alternatively, manipulations that increase the felt intensity of painful stimulation activate S1 and S2/posterior insula [11, 13, 16, 25–28].
Because the dACC and anterior insula are involved in the distress of physical pain, these regions may also play a role in socially painful experience. As further evidence for this possibility, research in non-human mammals has demonstrated that some of these same affective pain-related regions also contribute to certain separation distress behaviors, such as distress vocalizations.
Neural correlates of separation distress behaviors
In many mammalian species, infants produce distress vocalizations upon caregiver separation in order to signal the caregiver to retrieve the infant. These vocalizations are presumed to reflect some degree of distress due to separation and serve the adaptive purpose of reducing prolonged separation from a caregiver. Highlighting a role for the ACC in distress vocalizations, it has been shown that lesions to the ACC (that include both dorsal and ventral regions) eliminate the production of these distress vocalizations [29–30], whereas electrical stimulation of the ACC can lead to the spontaneous production of these vocalizations [31–32]. Similar findings have not been observed for the anterior insula. However, other regions that play a role in pain processing, such as the periaqueductal gray (PAG), have also been shown to be involved in eliciting distress vocalizations [33].
Based on research highlighting a role for the dACC and anterior insula in the distressing experience of physical pain as well as a role for the ACC in separation distress behaviors in non-human mammals, we explored whether these same regions were involved in experiences of social pain in humans.
Neural correlates of social pain in humans
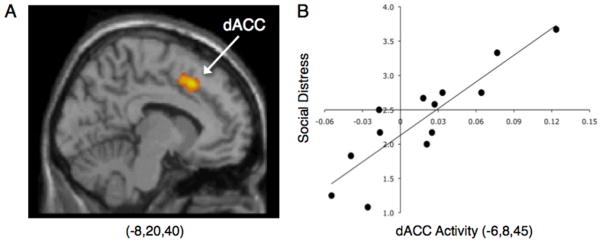
In the first study of social exclusion in humans [34], participants completed a neuroimaging session while playing an interactive virtual ball-tossing game (“Cyberball”; adapted from [35]) over the internet with two other individuals. Unbeknownst to participants, they were actually playing with a preset computer program. Participants completed one round of the ball-tossing game in which they were included in the game and a second round in which they were excluded partway through the game. Upon being excluded from the game, compared to when being included, participants showed increased activity in both the dACC and anterior insula—a pattern very similar to what is typically observed in studies of physical pain. Moreover, individuals who showed greater activity in the dACC reported stronger feelings of social distress (e.g., “I felt rejected,” “I felt meaningless”) in response to the exclusion episode (Figure 2). Thus, for the first time in humans, it was demonstrated that an experience of social exclusion activated neural regions typically associated with physical pain distress.
Figure 2.
(A) Neural activity in the dACC that was greater during social exclusion vs. inclusion. (B) Correlation between dACC activity and self-reported social distress. (Adapted from Eisenberger et al., 2003.)
Subsequent studies, using variations of the ball-tossing game described above, have produced similar findings. Thus, several studies have shown increased activity in the dACC and/or anterior insula in response to social exclusion [36–40] as well as a positive correlation between greater activity in the dACC and/or anterior insula and greater self-reported social distress in response to social exclusion [37, 41–44].
In addition, individual difference factors that typically reduce or enhance responses to social exclusion (e.g., social support, anxious attachment) demonstrate the expected relationships with neural activity. Thus, individuals with more social support or who spend more time with friends—factors that should mitigate the negative effects of exclusion—show reduced activity in the dACC and anterior insula in response to social exclusion [38,42]. Conversely, individuals who score higher in anxious attachment, the tendency to worry about rejection from close others, show increased activity in the dACC and anterior insula in response to social exclusion [41]. Similarly, individuals with lower self-esteem (vs. higher self-esteem) report feeling more hurt in response to social exclusion and show greater activity in the dACC [45]. Finally, greater self-reported social disconnection during real-world social interactions is associated with greater activity in the dACC (as well as the PAG) in response to social exclusion [46].
Building on this, a recent study demonstrated that, within the same subjects, an experience of social rejection and an experience of physical pain activated overlapping neural regions. In this study, subjects who recently experienced an unwanted romantic relationship breakup completed two tasks. In one task, they were asked to view a picture of the person who recently broke up with them and to think back to that experience of rejection. In another task, they received painful heat stimulation. Results from this study showed increased activity in the dACC and anterior insula (as well as increased activity in sensory-related regions: S2 and posterior insula) both in response to reliving the rejection experience as well in response to the painful heat stimulation [47]. As such, this study demonstrates that experiences of rejection and physical pain, when administered within the same individuals, activate common neural regions.
In addition, negative social evaluation, which involves receiving rejecting feedback from others, activates these pain-related regions as well. In one study (modeled after a behavioral paradigm [48]), participants were told that another subject (who was actually a confederate) would serve as an evaluator—providing the participant with some feedback on an interview that he/she completed earlier. During the scanning session, participants believed that the evaluator was listening to their interview and choosing a new descriptive adjective, every 10 seconds, to indicate their impressions of the participant’s interview (the feedback was the same for each participant). Feedback words were pre-selected to be interpreted as rejecting (e.g., “boring”), neutral (e.g., “spontaneous”), or accepting (e.g., “intelligent”). Participants were also asked to rate how they felt in response to each new feedback word. Results demonstrated, not surprisingly, that participants felt significantly worse following the rejecting feedback. Moreover, to the extent that participants reported feeling worse in response to the feedback words, they showed greater activity, once again, in both the dACC and bilateral anterior insula [49].
Interestingly, the dACC and anterior insula may be responsive, not only to experiences of rejection, but to cues that represent or signal social rejection (or the possibility of social rejection) as well. Thus, studies that have simply used rejection-themed images or facial expressions have shown similar effects to those that have attempted to induce a socially painful experience. For example, in response to viewing rejection-themed images (paintings by Edward Hopper) vs. acceptance-themed images (paintings by August Renoir), participants showed increased activity in both the dACC and anterior insula [50]. Moreover, in another study, individuals who scored higher in rejection sensitivity showed greater dACC activity in response to viewing videos of individuals making disapproving facial expressions—a potential cue of social rejection—even when they knew that the videos were not personally directed at them [51].
Finally, research has demonstrated that other types of socially painful experiences, such as experiences of social loss, can activate these pain-related neural regions as well. For example, bereaved participants who viewed pictures of their deceased first-degree relative (vs. pictures of a stranger) showed greater activity in the dACC and anterior insula [52,53]. Moreover, females who lost an unborn child, compared to those who delivered a healthy child, showed greater activity in the dACC in response to viewing pictures of smiling baby faces [54]. Thus, various types of socially painful experiences—including bereavement—may activate these pain-related neural regions as well.
Summary
Together, the evidence reviewed here supports the first test of the physical-social pain overlap, namely that experiences of social pain activate neural regions that are also involved in physical pain processing. Although this work is informative, it will be important for future research to continue to examine whether experiences of social and physical pain lead to overlapping neural activity within the same subjects (as was done previously [47]). It will also be important for future research to further explore the factors that contribute to the observed variability in the precise location of the activations across studies.
Expected Consequences of a Physical-Social Pain Overlap
To the extent that physical and social pain processes rely on shared neural substrates, there should be several expected consequences. First, because both physical and social pain are governed by some of the same underlying neural circuitry, individuals who are more sensitive to one kind of pain should also be more sensitive to the other. Second, because altering one type of pain should alter the underlying neural system that supports both types of pain experience, factors that either increase or decrease one type of pain should alter the other type of pain in a similar manner (see Figure 1). Here, I will review evidence for each of these hypothesized consequences of a physical-social pain overlap. I will then discuss several other possible consequences of this overlap that have remained largely unexplored.
Are individuals who are more sensitive to one kind of pain also more sensitive to the other?
To the extent that physical and social pain rely on overlapping neural regions, individual differences in sensitivity to physical pain should relate to individual differences in sensitivity to social pain. Indeed, we have demonstrated this pattern across two studies. In one study, we examined whether baseline sensitivity to physical pain related to subsequent self-reports of sensitivity to an experience of social exclusion [55]. To assess baseline pain sensitivity, we exposed subjects to painful heat stimuli and measured the temperature at which each subject reported the painful stimuli to be “very unpleasant” (an index of the affective component of pain). Subjects then completed a round of the Cyberball game in which they were socially excluded and asked to report on how much social distress (e.g., “I felt rejected,” “I felt meaningless”) they felt in response. As expected, individuals who displayed greater baseline pain sensitivity also reported feeling higher levels of social distress following exclusion. This effect remained after controlling for neuroticism and trait anxiety, implying that these results were not simply due to subjects being more sensitive to negative affect more generally.
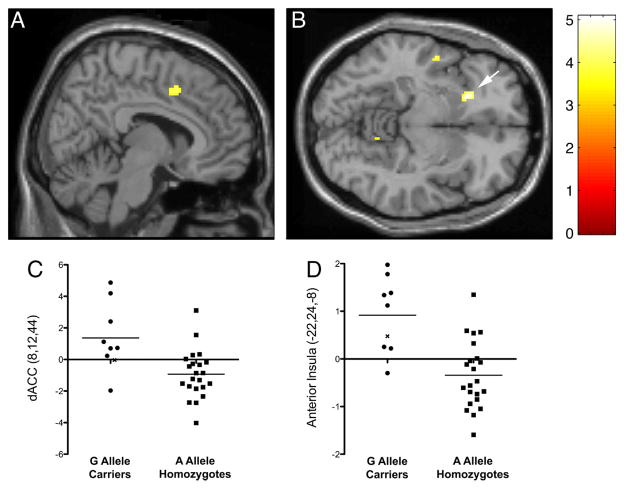
In a subsequent study, we demonstrated that a genetic correlate of physical pain sensitivity, specifically variability in the mu-opioid receptor gene (OPRM1), related to social pain sensitivity [56]. Previous research has identified a polymorphism in the mu-opioid receptor gene (OPRM1; A118G) that is associated with physical pain sensitivity; individuals who carry the rare G allele tend to experience more physical pain and need more morphine to deal with pain [57–59]. Here, we examined whether this polymorphism also related to social pain sensitivity. To do this, participants (n=125) were genotyped for the OPRM1 gene and completed a self-report measure of trait sensitivity to rejection (Mehrabian Sensitivity to Rejection Scale [60]; e.g., “I am very sensitive to any signs that a person might not want to talk to me”). Following this, a subset of these participants (n=30) completed the Cyberball game in the scanner in which they socially included and then excluded. Results demonstrated that G allele carriers—previously shown to be more sensitive to physical pain—also reported significantly higher levels of rejection sensitivity. Moreover, neuroimaging analyses revealed that G allele carriers showed greater activity in the dACC and anterior insula in response to social exclusion (Figure 3). Thus, a genetic correlate of physical pain sensitivity related to both a self-report and a neural measure of social pain sensitivity.
Figure 3.
Neural activity (during exclusion vs. inclusion) that was greater for G allele carriers than A allele homozygotes in the (A) dACC and (B) anterior insula (p<.001, 20 voxels). C) Parameter estimates from the dACC (8,12,44; t(24)= 4.06, p< 0.001); D) Parameter estimates from the left anterior insula (−22,24, −8; t(24)= 5.07, p < 0.001). * denotes G allele homozygote. (Reprinted from Way et al., 2009.)
Does altering one type of pain experience alter the other in a similar manner?
A second consequence of a physical-social pain overlap is that factors that increase or decrease one type of pain experience should have a parallel effect on the other type of pain experience. Here, I review studies related to each of the variants of this hypothesis.
Factors that increase social pain should increase physical pain
To begin to explore the parallel nature of augmenting physical and social pain, we investigated whether an experience of social exclusion increased sensitivity to experimental pain stimuli [55]. In this study, participants were randomly assigned to play a round of the Cyberball game in which they were either included or excluded. Then, toward the end of the game, participants received three painful heat stimuli (customized to each participant’s pain threshold) to their forearm and were asked to rate the unpleasantness of each stimulus (which indexes the affective component of pain). After the game concluded, participants rated how much social distress they felt in response to the Cyberball game. Although there was no main effect of exclusion vs. inclusion on pain ratings (e.g., excluded individuals did not report higher pain ratings in response to the heat stimuli than included individuals), we found that, among excluded subjects, those who felt the most social distress in response to being excluded also reported the highest pain ratings in response to the heat stimuli. In other words, when taking individual differences in susceptibility to social pain into account, those who were more hurt by social exclusion also reported feeling more pain in response to the heat stimuli. Importantly, this effect remained after controlling for neuroticism, suggesting that the positive relationship between social distress and pain distress was not due solely to a greater tendency to report negative affect and could reflect a more specific relationship between physical and social pain processes. Thus, even though this finding is correlational, it suggests that augmented sensitivity to one type of pain is related to augmented sensitivity to the other (c.f., [61]).
Factors that increase physical pain should increase social pain
We have also explored whether factors that increase physical pain, such as inflammatory activity, can increase experiences of social pain as well. Inflammatory activity is the body’s first line of defense against illness and infection. When a foreign agent is detected, the immune system responds by producing chemical messengers, called proinflammatory cytokines, which have several physiological and behavioral consequences. In addition to orchestrating an inflammatory response at the site of infection, proinflammatory cytokines also signal the brain to initiate ‘sickness behavior”—a coordinated set of behaviors including fatigue and increased pain sensitivity, which are hypothesized to promote recovery and recuperation from illness [62]. Because heightened physical pain sensitivity is a commonly induced by inflammation [63] we examined whether inflammatory mechanisms could also increase social pain sensitivity, as indexed by a heightened sense of social disconnection and greater neural sensitivity to social exclusion.
To examine this, participants (n=39) were randomly assigned to either receive placebo or endotoxin—a bacterial agent that induces an inflammatory response. Participants were then asked to report hourly on their feelings of social disconnection (e.g., “I feel disconnected from others,” “I feel overly sensitive around others (e.g., my feelings are easily hurt)”). In addition, participants completed the Cyberball social exclusion task in the fMRI scanner during the time of peak cytokine response (2 hours post-endotoxin infusion). Results revealed that participants exposed to endotoxin vs. placebo showed a greater increase over time in feelings of social disconnection (which resolved by the study’s end) [64]. Moreover, among subjects exposed to endotoxin, those who showed the largest increase in IL-6, one type of proinflammatory cytokine, also showed the greatest neural activity in the dACC and anterior insula in response to social exclusion [65]. It is important to note that subjects exposed to endotoxin did not simply display hypersensitivity to all stimuli, as a separate reward-related task demonstrated the opposite effect; subjects exposed to endotoxin (vs. placebo) displayed reduced reward-related neural activity to the anticipation of monetary rewards [66]. Thus, inflammation, known to increase physical pain sensitivity, also appears to increase feelings of social disconnection and neural sensitivity to social pain.
Factors that decrease social pain should decrease physical pain
In addition to exploring factors that increase physical or social pain, we have also examined factors that decrease these painful experiences. For example, we have examined whether social support, typically assumed to reduce experiences of social pain or loneliness [38,42], can also reduce experiences of physical pain. Although substantial correlational research has demonstrated that those who have more social support tend to experience less physical pain across a number of domains, such as during childbirth and following surgery [67–69], far less research has examined the causal effect of social support on physical pain.
To examine whether social support causally reduces physical pain experience, female participants in long-term romantic relationships received a series of painful heat stimuli as they completed several different experimental conditions, which included holding their partner’s hand (social support) vs. a stranger’s hand or a squeezeball (control conditions) and viewing pictures of their partner (social support) vs. pictures of a stranger or an object (control conditions). Results revealed that participants reported significantly lower pain ratings in the social support conditions—either when they were holding their partner’s hand or when they were viewing a picture of their partner [70]. Indeed, this finding of decreased pain ratings in response to viewing partner pictures has now been replicated across two fMRI studies [71,72]. Moreover, in these studies, participants showed significantly less activity in the dACC and/or anterior insula when viewing pictures of their partners (vs. control images) [71,72]. Thus, simple reminders of one’s social support figure may be capable of directly reducing the experience of physical pain, not just social pain.
Factors that decrease physical pain should decrease social pain
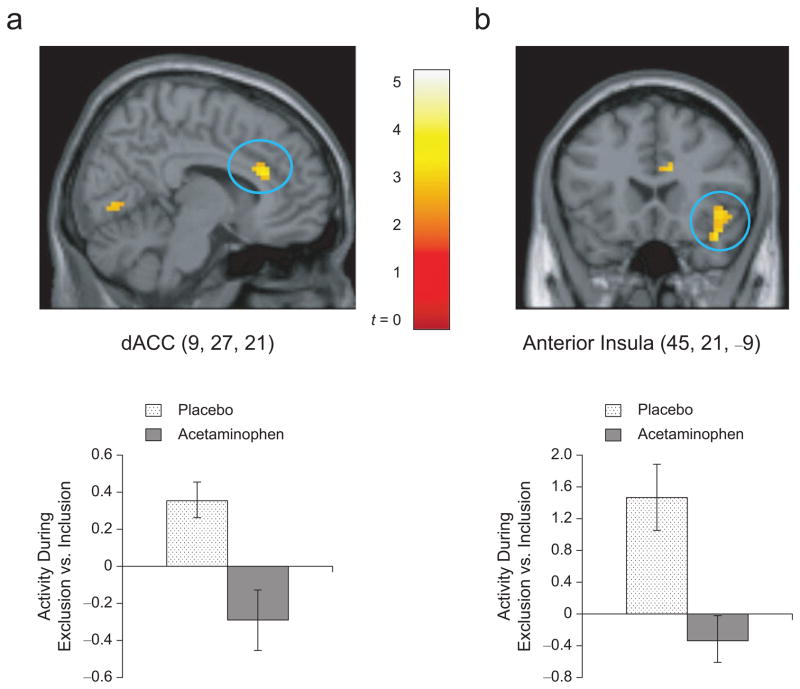
Finally, we have examined whether Tylenol (generic name: acetaminophen), typically thought to reduce physical pain, can also reduce social pain [36]. Here, participants were randomly assigned to take either a normal dose of Tylenol (1000 mg/day) or placebo each day for three weeks. Every night, over this three-week period, participants were asked to rate their daily “hurt feelings” (e.g., “Today, I rarely felt hurt by what other people said or did to me” (reverse-scored)). Results demonstrated that participants in the Tylenol condition showed a significant decrease in self-reported hurt feelings over time, whereas participants in the placebo condition showed no significant change.
To further explore the neural mechanisms that might underlie these changes in self-reported hurt feelings, in a second study, participants were randomly assigned to take either Tylenol (2000 mg/day) or placebo each day for a 3-week period. Then, at the end of the three weeks, participants completed the Cyberball social exclusion task in the fMRI scanner. Consistent with the results from the first study, participants in the Tylenol condition showed significantly less activity in the dACC and anterior insula compared to subjects in the placebo condition, who showed normal increases in these regions (Figure 4). Thus, Tylenol, a physical painkiller, appears to act as a ‘social painkiller’ as well.
Figure 4.
Neural activity (during exclusion vs. inclusion) that was greater for participants who took placebo (vs. those who took acetaminophen) in the dACC and right anterior insula (p < .005, 20 voxels). Bar graphs (with standard error bars) for each region show the activity during exclusion compared to inclusion, averaged across the entire cluster, for the acetaminophen and placebo groups. (Reprinted from DeWall et al., 2010.)
Are there other consequences of a physical-social pain overlap?
There are arguably several other consequences of a physical-social pain overlap that have yet to be explored. Indeed, the psychological literature provides two nice examples of some elusive behavioral findings that might be better understood as a consequence of this overlap.
Social psychologists have long puzzled over the consistent finding that experiences of rejection or exclusion often lead to aggressive behavior [73–75]. From a logical perspective, aggression following rejection seems maladaptive, as aggression is not conducive to re-establishing social ties, and if anything, makes social reconnection more difficult. However, if these results are interpreted in light of a physical-social pain overlap, they begin to make more sense. The threat or experience of physical pain is known to result in aggressive action, and this behavior is typically viewed as adaptive. If one is being physically harmed, one may need to attack to defend oneself [76–77]. When these findings are viewed in the context of a physical-social pain overlap, it highlights the possibility that aggressive responses to rejection may be a bi-product of an adaptive response to physical pain, which was subsequently co-opted by the social pain system. In other words, although aggressive responses to rejection may be maladaptive in recreating social bonds, this response may reflect a conservation of behavioral responses that have been adaptive following physical harm.
A second example comes from research on physiological responses to stress. A growing body of research has demonstrated that experiences of social evaluation, such as giving a public speech, can trigger physiological stress responses, which are typically thought to mobilize energy to deal with threat [78] or to incite the immune system to prepare to deal with wounds following threat [79]. Although it makes sense that these physiological stress responses would be observed following basic physical threats (e.g., physical attacks, life-threatening events) [80], it is more difficult to understand why these same processes would be triggered by situations that involve social evaluation or the possibility of social rejection. Why would individuals need to mobilize significant energy resources or prepare for wounding when faced with delivering a public speech? Again, viewing these findings from the lens of a physical-social pain overlap may shed light on this question. If the brain interprets the threat of social evaluation or social rejection in the same manner as it interprets the threat of physical harm, biological stress responses might be triggered to both for the simple reason that these two systems overlap. Another related possibility is that, given the importance of social inclusion for survival, the body may respond to social threat as it would to physical threat because of the survival disadvantage associated with social isolation.
Summary
To the extent that physical and social pain rely on shared neural circuitry, there should be several functional consequences. Here, we have shown evidence for two of these consequences, namely that individual differences in sensitivity to one kind of pain relate to individual differences in sensitivity to the other and that factors that modulate one type of pain experience affect the other in a similar manner. Future work will benefit from continuing to explore the consequences of a physical-social pain overlap. Moreover, some puzzling findings, such as aggressive responses to social rejection or physiological stress responses to social evaluation, may be better interpreted and understood through this lens.
Caveats and Limitations
Although exploring the similarities between physical and social pain has been an interesting and, at times, fruitful endeavour, it is important to note that there are several caveats and limitations to this approach. The first limitation is that it is difficult to determine whether the overlapping neural activity during physical and social pain is due to pain-related processing or some other kind of process. For example, although the dACC has been implicated in pain processing, it has also been implicated in other processes such as cognitive conflict detection (detecting conflicting response tendencies (e.g., Stroop task) or mismatches between intended and produced responses (e.g., error detection) or between what is expected and what is observed) [81] as well as autonomic activity [82]. Thus, it is not yet clear if the activations observed in the studies reviewed here are indicative of pain per se, or some other underlying process. However, it is important to note that the dACC’s role in cognitive conflict and autonomic activity is not incompatible with its role in pain distress. In fact, we have previously argued that conflict detection and distress may work together as two components of a more general neural alarm system [6]. Thus, in the same way that an alarm system requires: 1) a mechanism that detects discrepancies from a desired setpoint and 2) an alarm bell that recruits attention towards fixing the problem, the dACC may be involved in detecting discrepancies from important goals (e.g., social connection) and triggering distress (and likely autonomic activity) in order to direct attention towards dealing with the problem at hand and correcting behavior. Future research will be needed to more carefully elucidate the precise neurocognitive computations that are instantiated in the dACC and anterior insula in response to social and physical pain.
Another caveat to the findings reviewed here is that while there is substantial evidence that physical and social pain overlap, these experiences and processes certainly do not overlap completely. Intuitively, we know this to be true because we can differentiate between pain due to a relationship snub and pain due to physical injury. Moreover, research has started to identify specific differences between these two types of pain experience. For example, Chen and colleagues have shown that individuals can easily relive the pain of previous relationship breakups or other socially painful events; however, it is much harder, and sometimes impossible to relive the pain of physical injury [83]. This finding implies the operation of separate neural systems underlying these experiences as well. Thus, while it is important to examine the similarities underlying these types of experiences, it will also be important to clearly identify the differences and to establish the boundary conditions of the physical-social pain overlap.
Furthermore, although it can be argued that feeling pain upon social separation is a potent motivator of social connection, it is certainly not the only motivator. One of the other key factors that motivates social connection, currently missing from this line of research, are experiences of social pleasure. Indeed, we are currently turning our attention to exploring the neural correlates underlying the inherently pleasurable social experiences that motivate social connection. For example, we have recently observed that providing social support to a loved one in need activates neural regions that play a role in processing basic rewards, suggesting that it may be ‘rewarding’ or reinforcing to be able to help a close other in need [84]. Future work will be required to more carefully investigate other forms of social experience that reinforce social connection as well.
Conclusions
In sum, the research reviewed here supports the idea that the pain of social rejection, exclusion, or loss may be more than just metaphorical by highlighting a common set of neural regions that underlie both social and physical pain. One of the key implications of these findings is that experiences of social exclusion or relationship loss may be just as emotionally distressing as experiences of physical pain. Although physical pain is typically regarded as more serious or objectively distressing because it has a clear biological basis, the work reviewed here demonstrates that social pain could be argued to be just as distressing because it activates the same underlying neural machinery. These findings encourage us to think more carefully about the consequences of social rejection. For example, while physically hurting another individual is uniformly frowned upon and typically punishable by law, rejecting someone else or inflicting social pain on someone is typically not held to the same standard. The work reviewed here suggests that our intuitions about and rules regarding social pain might be misguided and that these experiences might be just as damaging as experiences of physical pain. In fact, with regards to both mental and physical health, social pain-related experiences may be quite detrimental. For example, those who have experienced the loss of a loved one (vs. those who have not) are twice as likely to develop depression [85] and those who have experienced social rejection are approximately 22 times more likely to develop depression [86] and do so more quickly [87]. Moreover, patients with somatoform pain or fibromyalgia, who experience pain with no medical explanation, report early experiences of social pain (emotional abuse, family conflict, early parental loss) [88–90], highlighting a potential link between these negative social experiences early on and later enhanced sensitivity to physical pain.
Finally, although experiences of social pain are clearly distressing and hurtful in the moment, it is important to remember that these painful feelings following social exclusion or broken social relationships also serve a valuable function, namely to ensure the maintenance of close social ties. To the extent that being rejected hurts, individuals are motivated to avoid situations in which rejection is likely. Over the course of evolutionary history, avoiding social rejection and staying socially connected to others likely increased chances of survival, as being part of a group provided additional resources, protection, and safety. Thus, the experience of social pain, although distressing and hurtful in the short-term, is an evolutionary adaptation that promotes social bonding and ultimately survival.
Acknowledgments
The research reviewed here was supported by a NARSAD Young Investigator Award, a Dana Foundation Grant in Brain and Immunoimaging, a UCLA Faculty Senate Grant, a UCLA Career Development Award, a UCLA Integrative Mood Disorder Study Center Award, and NIMH grants (R21MH66709-01, R21MH071521-01, R01MH56880). This paper was presented as a talk at the 2011 American Psychosomatic Society meeting, where Dr. Eisenberger was presented with the 2011 Herbert Weiner Early Career Award.
References
- 1.Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995;117:497–529. [PubMed] [Google Scholar]
- 2.Bowlby J. Attachment. I. New York: Basic Books; 1969. Attachment & Loss. [Google Scholar]
- 3.James W. The Principles of Psychology. Vol. 1. New York: Dover Publications, Inc; 1890. [Google Scholar]
- 4.Eisenberger NI, Lieberman MD. Broken hearts and broken bones: The neurocognitive overlap between social pain and physical pain. In: Williams KD, Forgas JP, von Hippel, editors. The Social Outcast: Ostracism, Social Exclusion, Rejection, and Bullying. New York: Cambridge University Press; 2005. pp. 109–27. [Google Scholar]
- 5.Eisenberger NI. Why rejection hurts: What social neuroscience has revealed about the brain’s response to social rejection. In: Decety J, Cacioppo J, editors. The Handbook of Social Neuroscience. New York: Oxford University Press; 2011. pp. 109–27. [Google Scholar]
- 6.Eisenberger NI, Lieberman MD. Why rejection hurts: The neurocognitive overlap between physical and social pain. Trends in Cogn Sci. 2004;8:294–300. doi: 10.1016/j.tics.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 7.MacDonald G, Leary MR. Why does social exclusion hurt? The relationship between social and physical pain. Psychol Rev. 2005;131:202–23. doi: 10.1037/0033-2909.131.2.202. [DOI] [PubMed] [Google Scholar]
- 8.Panksepp J. Affective Neuroscience. New York: Oxford University Press; 1998. [Google Scholar]
- 9.Treede RD, Kenshalo DR, Gracely RH, Jones AKP. The cortical representation of pain. Pain. 79:105–111. doi: 10.1016/s0304-3959(98)00184-5. [DOI] [PubMed] [Google Scholar]
- 10.Leary MR, Springer C. Hurt feelings: The neglected emotion. In: Kowalski RM, editor. Behaving Badly: Aversive Behaviors in Interpersonal Relationships. Washington DC: American Psychological Association; 2001. pp. 151–175. [Google Scholar]
- 11.Apkarian AV, Bushnell MC, Treede R-D, Zubieta J-K. Human brain mechanisms of pain perception and regulation in health and disease. J Pain. 2005;9:463–84. doi: 10.1016/j.ejpain.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 12.Peyron R, Laurent B, Garcia-Larrea L. Functional imaging of brain responses to pain. A review and meta-analysis. Neurophysiol Clin. 2000;30:263–88. doi: 10.1016/s0987-7053(00)00227-6. [DOI] [PubMed] [Google Scholar]
- 13.Price DD. Psychological and neural mechanisms of the affective dimension of pain. Science. 2000;288:1769–72. doi: 10.1126/science.288.5472.1769. [DOI] [PubMed] [Google Scholar]
- 14.Rainville P. Brain mechanisms of pain affect and pain modulation. Curr Opin Neurobiol. 2002;12:195–204. doi: 10.1016/s0959-4388(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 15.Bushnell MC, Duncan GH, Hofbauer RK, Ha B, Chen JI, Carrier Pain perception: Is there a role for primary somatosensory cortex? Proceedings of the National Academy of Sciences. 1999;96:7705–7709. doi: 10.1073/pnas.96.14.7705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Craig AD. A new view of pain as a homeostatic emotion. Trends in Neurosci. 2003;26:303–307. doi: 10.1016/s0166-2236(03)00123-1. [DOI] [PubMed] [Google Scholar]
- 17.Richter EO, Davis KD, Hamani C, Hutchison WD, Dostrovsky JO, Lozano AM. Cingulotomy for psychiatric disease: Microelectrode guidance, a callosal reference system for documenting lesion location, and clinical results. Neurosurgery. 2004;54:622–28. doi: 10.1227/01.neu.0000108644.42992.95. [DOI] [PubMed] [Google Scholar]
- 18.Foltz EL, White LE. The role of rostral cingulotomy in “pain” relief. Int J Neurol. 1968;6:353–73. [PubMed] [Google Scholar]
- 19.Hebben N. Toward the assessment of clinical pain. In: Aronoff GM, editor. Evaluation and treatment of chronic pain. Baltimore: Urban & Schwarzenburg; 1985. pp. 451–62. [Google Scholar]
- 20.Berthier M, Starkstein S, Leiguardia R, Carrea R. Asymbolia for pain: A sensory-limbic disconnection system. Ann Neurol. 1988;24:41–9. doi: 10.1002/ana.410240109. [DOI] [PubMed] [Google Scholar]
- 21.Ploner M, Freund HJ, Schnitzler A. Pain affect without pain sensation in a patient with a postcentral lesion. Pain. 1999;81:211–14. doi: 10.1016/s0304-3959(99)00012-3. [DOI] [PubMed] [Google Scholar]
- 22.Rainville P, Duncan GH, Price DD, Carrier B, Bushnell MD. Pain affect encoded in human anterior cingulate but not somatosensory cortex. Science. 1997;277:968–71. doi: 10.1126/science.277.5328.968. [DOI] [PubMed] [Google Scholar]
- 23.Tölle TR, Kaufmann T, Siessmeier T, Lautenbacher S, Berthele A, Munz F, et al. Region-specific encoding of sensory and affective components of pain in the human brain: A positron emission tomography correlation analysis. Ann Neurol. 1999;45:40–7. doi: 10.1002/1531-8249(199901)45:1<40::aid-art8>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 24.Schreckenberger M, Siessmeier T, Viertmann A, Landvogt C, Buchholz H-G, Rolke R, et al. The unpleasantness of tonic pain is encoded by the insular cortex. Neurology. 2005;64:1175–83. doi: 10.1212/01.WNL.0000156353.17305.52. [DOI] [PubMed] [Google Scholar]
- 25.Hofbauer RK, Rainville P, Duncan GH, Bushnell MC. Cortical representations of the sensory dimension of pain. J Neurophys. 2001;86:402–411. doi: 10.1152/jn.2001.86.1.402. [DOI] [PubMed] [Google Scholar]
- 26.Kulkarni B, Bentley DE, Elliot R, Youell P, Watson A, Derbyshire SWG, Frackowiak RSJ, Friston KJ, Jones AKP. Attention to pain localization and unpleasantness discriminates the functions of the medial and lateral pain systems. Eur J Neurosci. 2005;21:3133–3142. doi: 10.1111/j.1460-9568.2005.04098.x. [DOI] [PubMed] [Google Scholar]
- 27.Craig AD, Chen K, Bandy D, Reiman EM. Thermosensory activation of insular cortex. Nat Neurosci. 2000;3:184–190. doi: 10.1038/72131. [DOI] [PubMed] [Google Scholar]
- 28.Craig AD. How do you feel? Interoception: the sense of the physiological condition of the body. Nat Rev Neuro. 2002;3:655–666. doi: 10.1038/nrn894. [DOI] [PubMed] [Google Scholar]
- 29.Hadland KA, Rushworth MFS, Gaffan D, Passingham RE. The effect of cingulate lesions on social behaviour and emotion. Neuropsychologia. 2003;41:919–31. doi: 10.1016/s0028-3932(02)00325-1. [DOI] [PubMed] [Google Scholar]
- 30.MacLean PD, Newman JD. Role of midline frontolimbic cortex in production of the isolation call of squirrel monkeys. Brain Res. 1988;45:111–123. doi: 10.1016/0006-8993(88)91550-8. [DOI] [PubMed] [Google Scholar]
- 31.Robinson BW. Neurological aspects of evoked vocalizations. In: Altmann SA, editor. Social Communication Among Primates. Chicago, IL: The University Press; 1967. pp. 135–47. [Google Scholar]
- 32.Smith W. The functional significance of the rostral cingular cortex as revealed by its responses to electrical excitation. J Neurophysiol. 1945;8:241–255. [Google Scholar]
- 33.Bandler R, Shipley MT. Columnar organization in the midbrain periaqueductal gray: Modules for emotional expression? Trends in Neurosci. 1994;17:379–89. doi: 10.1016/0166-2236(94)90047-7. [DOI] [PubMed] [Google Scholar]
- 34.Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt: An fMRI study of social exclusion. Science. 2003;302:290–2. doi: 10.1126/science.1089134. [DOI] [PubMed] [Google Scholar]
- 35.Williams KD, Cheung CKT, Choi W. Cyberostracism: Effects of being ignored over the internet. J Pers Soc Psychol. 2000;79:748–62. doi: 10.1037//0022-3514.79.5.748. [DOI] [PubMed] [Google Scholar]
- 36.DeWall CN, MacDonald G, Webster GD, Masten CL, Baumeister RF, Powell C, Combs D, Schurtz DR, Stillman TF, Tice DM, Eisenberger NI. Acetaminophen reduces social pain: Behavioral and neural evidence. Psychol Sci. 2010;21:931–7. doi: 10.1177/0956797610374741. [DOI] [PubMed] [Google Scholar]
- 37.Masten CL, Eisenberger NI, Borofsky L, Pfeifer JH, McNealy K, Dapretto M. Neural correlates of social exclusion during adolescence: Understanding the distress of peer rejection. Social Cognitive and Affective Neuroscience. 2009;4:143–57. doi: 10.1093/scan/nsp007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Masten CL, Telzer EH, Fuligni A, Lieberman MD, Eisenberger NI. Time spent with friends in adolescence relates to less neural sensitivity to later peer rejection. Soc Cogn Affective Neuro. doi: 10.1093/scan/nsq098. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bolling DZ, Pitskel NB, Deen B, Crowley MJ, McPartland JC, Mayes LC, Pelphrey KA. Dissociable brain mechanisms for processing social exclusion and rule violation. Neuroimage. 2011;54:2462–2471. doi: 10.1016/j.neuroimage.2010.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gunther Moor B, Guroglu B, Op de Macks ZA, Rombouts SARB, Van der Molen MW, Crone EA. Social exclusion and punishment of excluders: Neural correlates and developmental trajectories. Neuroimage. doi: 10.1016/j.neuroimage.2011.07.028. in press. [DOI] [PubMed] [Google Scholar]
- 41.DeWall CN, Masten CL, Powell C, Combs D, Schurtz DR, Eisenberger NI. Does the pain of rejection depend on attachment style? An fMRI study. Soc Cogn Aff Neuro. doi: 10.1093/scan/nsq107. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eisenberger NI, Taylor SE, Gable SL, Hilmert CJ, Lieberman MD. Neural pathways link social support to attenuated neuroendocrine stress responses. Neuroimage. 2007;35:1601–12. doi: 10.1016/j.neuroimage.2007.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Onoda K, Okamoto Y, Nakashima K, Nittono H, Ura M, Yamawaki S. Decreased ventral anterior cingulate cortex activity is associated with reduced social pain during emotional support. Soc Neuro. 2009;4:443–54. doi: 10.1080/17470910902955884. [DOI] [PubMed] [Google Scholar]
- 44.Krill A, Platek SM. In-group and out-group membership mediates anterior cingulate activation to social exclusion. Front Evol Neurosci. 2009;1:1–7. doi: 10.3389/neuro.18.001.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Onoda K, Okamoto Y, Nakashima K, Nittoni H, Yoshimura S, Yamawaki S, Yamaguchi S, Ura M. Does low self-esteem enhance social pain? The relationships between trait self-esteem and anterior cingulate cortex activation induced by ostracism. Soc Cogn Aff Neuro. 2010;5:383–91. doi: 10.1093/scan/nsq002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eisenberger NI, Gable SL, Lieberman MD. fMRI responses relate to differences in real-world social experience. Emotion. 2007;7:745–54. doi: 10.1037/1528-3542.7.4.745. [DOI] [PubMed] [Google Scholar]
- 47.Kross E, Berman MG, Mischel W, Smith EE, Wager TD. Social rejection shares somatosensory representations with physical pain. P Natl A Sci. 2011;108:6270–5. doi: 10.1073/pnas.1102693108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Leary MR, Haupt AL, Strausser KS, Chokel JT. Calibrating the sociometer: The relationship between interpersonal appraisals and state self-esteem. J Pers Soc Psychol. 74:1290–9. doi: 10.1037//0022-3514.74.5.1290. [DOI] [PubMed] [Google Scholar]
- 49.Eisenberger NI, Inagaki TK, Muscatell KA, Haltom KEB, Leary MR. The neural sociometer: A mechanism for translating interpersonal appraisals into state self-esteem. J Cognitive Neurosci. doi: 10.1162/jocn_a_00027. In Press. [DOI] [PubMed] [Google Scholar]
- 50.Kross E, Egner T, Ochsner K, Hirsch J, Downey G. Neural dynamics of rejection sensitivity. J Cognitive Neurosci. 2007;19:945–56. doi: 10.1162/jocn.2007.19.6.945. [DOI] [PubMed] [Google Scholar]
- 51.Burklund LJ, Eisenberger NI, Lieberman MD. Rejection sensitivity moderates dorsal anterior cingulate activity to disapproving facial expressions. Soc Neurosci. 50(2):238–53. doi: 10.1080/17470910701391711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gündel H, O’Connor M-F, Littrell L, Fort C, Richard L. Functional Neuroanatomy of grief: An fMRI study. J Psychiat. 2003;160:1946–53. doi: 10.1176/appi.ajp.160.11.1946. [DOI] [PubMed] [Google Scholar]
- 53.O’Connor MF, Wellisch DK, Stanton A, Eisenberger NI, Irwin MR, Lieberman MD. Craving love? Enduing grief activates brain’s reward center. Neruo Image. 2008;42:969–72. doi: 10.1016/j.neuroimage.2008.04.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kersting A, Ohrmann P, Pedersen A, Kroker K, Samberg D, Bauer J, et al. Neural activation underlying acute grief in women after ther loss of an unborn child. Am J Psychiat. 2009;166:1402–10. doi: 10.1176/appi.ajp.2009.08121875. [DOI] [PubMed] [Google Scholar]
- 55.Eisenberger NI, Jarcho JM, Lieberman MD, Naliboff BD. An experimental study of shared sensitivity to physical pain and social rejection. Pain. 2006;126:132–8. doi: 10.1016/j.pain.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 56.Way BM, Taylor SE, Eisenberger NI. Variation in the mu-opioid receptor gene (OPRM1) is associated with dispositional and neural sensitivity to social rejection. P Natl Acad Sci. 2009;106:15079–84. doi: 10.1073/pnas.0812612106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chou W-Y, Yang L-C, Lu HF, Ko JY, Wang CH, Lin SH, et al. Association of mu-opiod receptor gene polymorphism (A118G) with variations in morphine consumption for analgesia after total knee arthroplasty. Acta Anaesth Scand. 2006;50:787–92. doi: 10.1111/j.1399-6576.2006.01058.x. [DOI] [PubMed] [Google Scholar]
- 58.Chou WY, Wang C-H, Liu P-H, Liu C-C, Tseng C-C, Jawan B. Human opioid receptor A118G polymorphism, affects Intravenous patient-controlled analgesia morphine consumption after total abdominal hysterectomy. Anesthesiology. 2006;105:334–7. doi: 10.1097/00000542-200608000-00016. [DOI] [PubMed] [Google Scholar]
- 59.Coulbalt L, Beaussier M, Verstuyft C, Weikmans H, Dubert L, Trégouet D, et al. Environmental and genetic factors associated with morphine response in the postoperative period. Pharmacogenet Gen. 2006;79:316–24. doi: 10.1016/j.clpt.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 60.Mehrabian A. Questionnaire measures of affiliative tendency and sensitivity to rejection. Psychol Rep. 176(38):199–209. [Google Scholar]
- 61.DeWall CN, Baumeister RF. Alone but feeling no pain: Effects of social exclusion on physical pain tolerance and pain threshold, affective forecasting, and interpersonal empathy. J Pers Soc Psychol. 2006;91:1–15. doi: 10.1037/0022-3514.91.1.1. [DOI] [PubMed] [Google Scholar]
- 62.Maier SF, Watkins LR. Cytokines for psychologists: Implications of bidirectional immune-to-brain communication for understanding behavior, mood, and cognition. Psychol Rev. 1998;105:83–107. doi: 10.1037/0033-295x.105.1.83. [DOI] [PubMed] [Google Scholar]
- 63.Watkins LR, Maier SF. The pain of being sick: Implications of immune-to-brain communication for understanding pain. Annu Rev Psychol. 2000;51:29–57. doi: 10.1146/annurev.psych.51.1.29. [DOI] [PubMed] [Google Scholar]
- 64.Eisenberger NI, Inagaki TK, Mashal NM, Irwin MR. Inflammation and social experience: An inflammatory challenge induces feelings of social disconnection in addition to depressed mood. Brain Beh Immun. 2010;24:558–563. doi: 10.1016/j.bbi.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eisenberger NI, Inagaki TK, Rameson L, Mashal NM, Irwin MR. An fMRI study of cytokine-induced depressed mood and social pain: The role of sex differences. Neuroimage. 2009;47:881–90. doi: 10.1016/j.neuroimage.2009.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Eisenberger NI, Berkman ET, Inagaki TK, Rameson L, Mashal N, Irwin MR. Inflammation-induced anhedonia: Endotoxin reduces ventral striatum responses to reward. Biol Psychiatry. 2010;68:748–754. doi: 10.1016/j.biopsych.2010.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kennell J, Klaus M, McGrath S, Robertson S, Hinkley C. Continuous emotional support during labor in US hospital: A randomized control trial. J Am Med Assoc. 1991;265:2197–201. [PubMed] [Google Scholar]
- 68.King KB, Reis HT, Porter LA, Norsen LH. Social support and long-term recovery from coronary artery surgery: Effects on patients and spouses. Health Psychol. 1993;12:56–63. doi: 10.1037//0278-6133.12.1.56. [DOI] [PubMed] [Google Scholar]
- 69.Kulik JA, Mahler HI. Social support and recovery from surgery. Health Psychology. 1989;8:221–38. doi: 10.1037//0278-6133.8.2.221. [DOI] [PubMed] [Google Scholar]
- 70.Master SL, Eisenberger NI, Taylor SE, Naliboff BD, Shirinyan D, Lieberman MD. A picture’s worth: Partner photographs reduce experimentally induced pain. Psychol Sci. 2009;20:1316–8. doi: 10.1111/j.1467-9280.2009.02444.x. [DOI] [PubMed] [Google Scholar]
- 71.Eisenberger NI, Master SL, Inagaki TK, Taylor SE, Shirinyan D, Lieberman MD, Naliboff B. Attachment figures activate a safety signal-related neural region and reduce pain experience. P Natl Acad Sci. 2011;108:11721–11726. doi: 10.1073/pnas.1108239108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Younger J, Aron A, Parke S, Chatterjee N, Mackey S. Viewing pictures of a romantic partner reduces experimental pain: Involvement of neural reward systems. PLOS One. 2010;5:1–7. doi: 10.1371/journal.pone.0013309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Leary MR, Twenge JM, Quinlivan E. Interpersonal rejection as a determinant of anger and aggression. Pers Soc Psychol Rev. 2006;10:111–32. doi: 10.1207/s15327957pspr1002_2. [DOI] [PubMed] [Google Scholar]
- 74.Twenge JM, Baumeister RF, Tice DM, Stucke TS. If you can’t join them, beat them: Effects of social exclusion on aggressive behavior. J Pers Soc Psychol. 2001;81:1058–69. doi: 10.1037//0022-3514.81.6.1058. [DOI] [PubMed] [Google Scholar]
- 75.Warburton WA, Williams KD, Cairns DR. When ostracism leads to aggression: The moderating effects of control deprivation. J Exp Soc Psychol. 2006;42:213–20. [Google Scholar]
- 76.Berkowitz L. Aversively stimulated aggression: Some parallels and differences in research with animals and humans. Am Psychol. 1983;38:1135–44. doi: 10.1037//0003-066x.38.11.1135. [DOI] [PubMed] [Google Scholar]
- 77.Berkowitz L. Aggression: Its Causes, Consequences and Control. Philadelphia, PA: Temple University Press; 1993. [Google Scholar]
- 78.Dickerson S, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol Bull. 2004;103:355–91. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- 79.Dickerson SS, Gable SL, Irwin MR, Aziz N, Kemeny ME. Social-evaluative threat and proinflammatory cytokine regulation: An experimental laboratory investigation. Psychol Sci. 2009;20:1237–44. doi: 10.1111/j.1467-9280.2009.02437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Taylor SE. Health Psychology. 5. New York: McGraw Hill Publishers; 2003. [Google Scholar]
- 81.Botvinick MM, Cohen JD, Carter CS. Conflict monitoring and anterior cingulate cortex: An update. Trends Cogn Sci. 2004;8:539–46. doi: 10.1016/j.tics.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 82.Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol. 2005;493:154–66. doi: 10.1002/cne.20749. [DOI] [PubMed] [Google Scholar]
- 83.Chen Z, Williams KD, Fitness J, Newton N. When hurt won’t heal: Exploring the capacity to relive social and physical pain. Psychol Sci. 2008;46:612–8. doi: 10.1111/j.1467-9280.2008.02158.x. [DOI] [PubMed] [Google Scholar]
- 84.Inagaki TK, Eisenberger NI. Neural correlates of giving support to a loved one. Psychosom Med. doi: 10.1097/PSY.0b013e3182359335. In Press. [DOI] [PubMed] [Google Scholar]
- 85.Monroe SM, Rohde P, Seeley JR, Lewinsohn PM. Life events and depression in adolescence: Relationship loss as a prospective risk factor for first onset of major depressive disorder. J Abnorm Psychol. 1999;108:606–14. doi: 10.1037//0021-843x.108.4.606. [DOI] [PubMed] [Google Scholar]
- 86.Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiat. 2003;60:789–96. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- 87.Slavich GM, Thornton T, Torres LD, Monroe SM, Gotlib IH. Targeted rejection predicts hastened onset of major depression. J Soc Clin Psychol. 2009;28:223–43. doi: 10.1521/jscp.2009.28.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Brown RJ, Schrag A, Trimble MR. Dissociation, childhood interpersonal trauma, and family functioning in patients with somatization disorder. Am J Psychiat. 2005;162:899–905. doi: 10.1176/appi.ajp.162.5.899. [DOI] [PubMed] [Google Scholar]
- 89.Mallouh SK, Abbey SE, Gillies LA. The role of loss in treatment outcomes of persistent somatization. Gen Hosp Psychiat. 1995;17:187–91. doi: 10.1016/0163-8343(95)00026-n. [DOI] [PubMed] [Google Scholar]
- 90.Imbierowicz K, Egle UT. Childhood adversities in patients with fibromyalgia and somatoform pain disorder. Eur J Pain. 2003;7:113–119. doi: 10.1016/S1090-3801(02)00072-1. [DOI] [PubMed] [Google Scholar]