Abstract
Objective To shed light on the difficulties faced by relatives, friends, and colleagues in interpreting signs of suicidality and deciding whether and how to intervene.
Design Qualitative study of completed suicides, based on in-depth interviews with multiple informants.
Setting London, southwest England, and south Wales.
Participants 31 lay informants (one to five for each case), including parents, partners, siblings, friends, and colleagues of 14 cases of suicide in which the deceased was aged 18-34 and was not in contact with secondary mental health services.
Results Informants described both intellectual and emotional barriers to awareness and intervention within the family and social network. They reported that signs and communications of distress were often oblique and difficult to interpret, that they may have disregarded warning signals and focused instead on positive signs, and that, even when they were aware that something was seriously wrong, taking any action at all involved considerable personal risks.
Conclusions As the suicidal process unfolds, significant others are faced with a highly complex task. Their proximity to the suicidal person and their emotional investment in the relationship make it difficult for them to see what is happening, to say anything to the person or to other members of the network, or to seek help outside the network. Efforts to strengthen the capacity of lay people to play a role in preventing suicide are urgently needed and should be informed by a thorough understanding of these difficulties. They should highlight the ambiguous nature of warning signs and should focus on helping people to acknowledge and overcome their fears about intervening.
Introduction
Prevention of suicide is a major public health concern in both developed and developing nations. The World Health Organization estimates that almost one million people die as a result of suicide every year—a global mortality rate of 16 per 100 000 or one death every 40 seconds—and calls for concerted effort by national authorities, health and non-health agencies, and the public to overcome the challenges of suicide prevention.1 Many nations and states have developed suicide prevention strategies, and these are increasingly recognising the need for involvement of the whole community.2 3 4 5 For example, New Zealand’s strategy begins with an explicit acknowledgment that “everyone has a role in suicide prevention.”4 Western Australia’s strategy is subtitled “everybody’s business” and highlights “the important role of family, friends, colleagues and peers in suicide prevention.”5 International campaigns, including World Suicide Prevention Day in 2005 and International Suicide Awareness Week in 2006, have also used the slogan “Suicide prevention is everybody’s business.” However, limited evidence exists on which to build action plans.
What role family members, friends, colleagues, and peers can play in suicide prevention, what challenges it might pose for them, and what resources they need in order to contribute effectively are unclear. Research has largely focused on the role of health professionals in identifying and managing risk to self. However, 75% of people who take their own lives are not under the care of a mental health team and many have not had recent contact with their general practitioner,6 7 so little or no opportunity exists for clinical intervention. Relatives, friends, and colleagues may be the only people to know that a person is distressed, and the burden of care lies entirely with them, until such time as the person decides, or is persuaded, to consult a doctor.
We know very little about what the suicidal process looks like from the lay point of view, or about how significant others interpret signs of escalating distress and decide what action, if any, they should take. Our study aimed to shed light on this neglected area. Such knowledge is essential to inform the development of interventions to promote the involvement of the whole community in suicide prevention.
Methods
Design
In this retrospective study of completed suicides, we used a qualitative case study approach. In each case, we sought to interview as many members of the deceased’s family and social network as possible, to gain a range of perspectives on events leading up to the death.8 The design is a modification of the psychological autopsy method.9
Recruitment and sampling
We identified deaths through HM Coroners in London, southwest England, and south Wales. We included those that were given a verdict of suicide, died aged 18-34, and were not in contact with secondary mental health services in the year before death. Cases in which family members were working with mental health practitioners to manage risk of suicide as part of a care plan are likely to present an entirely different set of characteristics and warrant separate investigation. This study builds on a body of previous work on suicides outside the care of mental health services.10 11 12 13
For eligible cases, the coroner who had conducted the inquest wrote to the next of kin inviting them to participate. If the next of kin agreed, we did an interview, during which we identified and sought consent to contact further members of the deceased’s social network who might be able to offer additional insights or an alternative perspective. Although this potentially limited access to additional informants, embarking on further enquiries without the consent of the next of kin would have been unethical. We also invited subsequent informants to nominate others, resulting in peer referrals. Each informant gave signed consent immediately before the interview. We stopped recruitment when we reached 30-35 interviews, owing to the depth and duration of interviews, richness of data, and complexity of the analytical task.8 14
Interviews
GO did in-depth interviews, using a single opening question designed to elicit an extended and uninterrupted narrative. The opening question was: “Please tell me, in your own time, about [the deceased], about your relationship with him/her, and about what happened in the period leading up to his/her death.” This approach leaves informants free to decide what information to include and how to organise it, ensuring that the narrative is not influenced by the preconceptions of the researcher.15 16 17 It also allows participants to feel in control and to disclose painful details at a pace that feels comfortable.18 19 The interviewer then asked pertinent follow-up questions, clarifying and elaborating on aspects of the narrative and focusing the conversation on areas of particular relevance to the study.20 We were keen to know what signs of distress members of the lay network had noticed, how they interpreted these, and what influenced decisions about whether and how to intervene. We were also interested more broadly in the social processes operating in the lay network and the ways in which personal relationships may have affected people’s ability to recognise and respond to the possibility of suicide.
Analysis
We tape recorded and transcribed interviews. Analysis took place alongside data collection, to allow for progressive focusing of interviews and testing of tentative hypotheses and theoretical constructs.21 Three members of the research team (CO, GO, and HL) independently read a set of three transcripts, identified prominent themes (some of which emerged spontaneously from the data, whereas others related to our own research questions), and agreed on a list of preliminary codes, which we added to and refined as coding progressed. We did coding and data management manually, using a set of proformas and analytical charts designed for the purpose. Working through each transcript, we copied textual material relating to each theme, together with line references, interpretive comments, and memos, on to a single proforma (one for each transcript). This allowed us to retain the integrity of each narrative and prevent the fragmentation and decontextualisation that can occur with software assisted coding.22 Two investigators (CO and GO) did the process independently for three whole cases (eight interviews), meeting regularly to examine discrepancies in coding and differences in interpretation of individual passages and revising definitions of codes where necessary, thus ensuring consistency and inter-coder reliability. We discussed these analyses at length at team meetings before applying the method to the remainder of the dataset. We then used a set of thematic charts (one for each theme) to look across narratives and compare diverse accounts within cases and between cases, “unpacking” and breaking down each theme into constituent elements as we went.22
We offered participants the opportunity to review their interview transcript, to contribute any further thoughts prompted by it, and to participate in an ongoing dialogue to validate our analysis and interpretation of their story. The published protocol gives a more detailed account of the methods.23
Results
We recruited next of kin for 14 cases (two female and 12 male), out of 53 eligible deaths. Six cases yielded only one interview, either because the next of kin asked us not to approach other members of the network (two cases) or because other members did not respond to the invitation. The remaining eight cases yielded 25 interviews, making a total of 31 interviews, some involving more than one informant. Parents, siblings, employers, peers, and colleagues contributed to the study. In addition, we interviewed 10 general practitioners, counsellors, and therapists but their data are not reported here, as this paper focuses on lay perspectives. The table shows characteristics of the sample. The cases are representative of suicides in this age group in respect of sex and method of suicide.24 25 To reduce the risk of cases and co-informants being identifiable, we have transposed some details between cases, while leaving the number of informants per case unaffected. We have also changed minor details within verbatim quotations, and we present quotations without their case numbers; these are available from the authors.
Table 1.
Characteristics of cases and lay informants
| Case | Age at death (years) | Sex | Method of suicide | No and relationship of informants |
|---|---|---|---|---|
| 01 | 18-24 | Male | Cutting or stabbing | 01.1 Mother |
| 01.2 Sibling (female) | ||||
| 02 | 25-34 | Female | Hanging | 02.1 Father |
| 03 | 25-34 | Male | Hanging | 03.1 Mother and father |
| 03.2 Sibling (male) | ||||
| 03.3 Colleague (male) | ||||
| 04 | 25-34 | Male | Poisoning by gases or vapours | 04.1 Mother and father |
| 04.2 Colleague (female) | ||||
| 04.3 Close friend (male) | ||||
| 04.4 Close friend (male) | ||||
| 04.5 Close friend (female) | ||||
| 05 | 25-34 | Male | Hanging | 05.1 Mother |
| 06 | 25-34 | Male | Hanging | 06.1 Mother |
| 07 | 18-24 | Male | Poisoning (overdose) | 07.1 Father |
| 08 | 25-34 | Male | Hanging | 08.1 Partner (female) |
| 08.2 Father-in-law | ||||
| 09 | 18-24 | Male | Hanging | 09.1 Mother |
| 10 | 25-34 | Female | Hanging | 10.1 Mother |
| 10.2 Partner (male) | ||||
| 11 | 25-34 | Male | Hanging | 11.1 Mother |
| 12 | 25-34 | Male | Poisoning (overdose) | 12.1 Mother |
| 12.2 Father | ||||
| 13 | 25-34 | Male | Jumping/lying before moving object | 13.1 Father |
| 13.2 Mother | ||||
| 13.3 Close friend (male) | ||||
| 13.4 Close friend (male) | ||||
| 13.5 Close friend (male) | ||||
| 14 | 18-24 | Male | Hanging | 14.1 Mother |
| 14.2 Close friends (male and female) | ||||
| 14.3 Employer (female) | ||||
| 14.4 Ex-partner (female) |
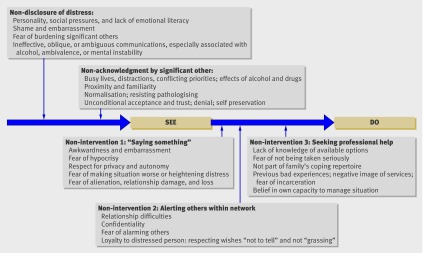
From the accounts given, we identified several factors that may have prevented members of the family and social network from recognising and responding to the suicidal crisis. These fell into three broad categories: difficulties faced by the suicidal person in effectively communicating distress, difficulties experienced by significant others in interpreting and heeding distress signals, and difficulties experienced by significant others in taking action.
Difficulties in communicating distress
Many informants suggested that the deceased did not give out clear distress signals. Some attributed this to personality, reporting that the deceased was introverted or “private” by nature and habitually concealed their emotions from those around them:
Father: “He was a very private person . . . You never knew what he was thinking or feeling . . . He’d present a façade to suggest that things were normal when in fact they weren’t, and try and tell you it was black when in fact it was white.”
Informants also mentioned the strong social pressures, especially among young men, to hide distress and keep up a pretence of coping. The social contexts in which young men meet, such as pubs and clubs, may not be conducive to “troubles telling,”26 and lack of emotional literacy may mean that they do not have the vocabulary or skills to do so:
Friend: “He’s a bloke, isn’t he? We don’t do emotion.”
Sibling: “I’d try and get things out of him about how he felt, especially when he’d had a few drinks, but he never ever opened up . . . He was a typical bloke in that respect . . . So I never really pushed it. I didn’t want to make him feel uncomfortable.”
These quotations betray a tacit acceptance of this situation on the part of significant others, and even an expectation that boys will not talk about emotions, which may have served to reinforce inhibitions and close down opportunities to confide.
Shame and embarrassment were given as further reasons why the deceased may not have felt able to reveal the depths of their distress to those around them, especially when the underlying problem was of a sexual or criminal nature. Fear of losing face, provoking an adverse reaction, or alienating significant others may have played a part in non-disclosure. Several informants believed that the deceased had kept their distress to themselves for fear of burdening those close to them, especially when those significant others were known to have mental health problems of their own:
Mother: “I think he didn’t want to worry me . . . Maybe he thought I couldn’t cope with it because of everything else that was going on in our lives at the time.”
Several accounts suggest that the deceased may have tried to communicate distress but failed to do so effectively or gave oblique and ambiguous signals. The role of alcohol in both facilitating and hindering communication emerged distinctly. Alcohol is often used as a way of coping with distress and can serve to break down inhibitions, but it can also sabotage attempts to communicate distress by rendering them unintelligible:
Mother: “A few times he rang me in the early hours of the morning absolutely piddled out of his head, and he’d be gabbling on but I couldn’t understand a word he was saying because he was so drunk.”
Over time, significant others may come to disregard talk induced by drink, so that further attempts to communicate distress and even suicidal ideation are ignored:
Father: “She said, if you don’t get him out Dad, I’ll top myself. But she was very drunk and I thought, this is the drink talking.”
Playing the part of the clown and joking about problems seems to have been another strategy for coping with distress, particularly used by young men within the context of “pub talk,” that masked inner turmoil and gave out an opposite message, suggesting to others that the person was untroubled by his difficulties. One informant reported how his friend had talked of suicide several times but without exhibiting the appropriate emotion, thus rendering the verbal message unconvincing:
Friend: “Towards the end he was saying that he was going to kill himself. But he’d say it with a smile . . . There was no real emotion behind it, no sort of tears or breakdown. He said it just as you’d say hello to someone.”
Other informants commented that the person’s behaviour or demeanour before suicide did not conform to their picture of the typically depressed or suicidal person, and several highlighted the difficulty of discerning the depth of another’s distress in the absence of any explicit outward display:
Friend: “When somebody’s giving off no signals whatsoever, apart from just being quiet and withdrawn, how can you tell how low they are? It’s really difficult if they’re not going round stabbing themselves or . . . constantly talking about killing themselves.”
Signs and countersigns
With hindsight, nearly all the informants were able to identify some “signs” or cues that might have alerted them to the depth of the other’s distress or warned them of an impending crisis. These included excessive quietness; emotional detachment from significant others; resisting physical contact, including eye contact; social withdrawal; fatigue; irritability; uncharacteristic outbursts and rages; talking about death and specifically suicide; and bizarre acts or gestures that were subsequently interpreted as “rehearsals” for the suicidal act or as attempts to say goodbye. However, their accounts also contained a wealth of evidence of “countersigns.” We defined these as verbal or non-verbal behaviours that counteracted unusual and potentially troubling signs and suggested to observers that no real cause for alarm existed. They included the deceased going about his or her normal business, going to work, going out with mates, laughing and joking as usual, making plans for the future, and giving explicit reassurances, typically “I’m OK, mum.”
Some of these seemingly normal behaviours may have been deliberately calculated to deceive or distract significant others and thus prevent intervention. Some may have represented brave attempts to battle on and keep up appearances so as to spare others distress, and others may have reflected vacillation. The ambivalence of people contemplating suicide is well recognised in the clinical literature,27 and it is confirmed by many of these accounts. Torn by conflicting impulses and unable to decide whether to live or to die, the suicidal person may be living two parallel lives, planning for the future while simultaneously planning and procuring the means for death, thereby giving out inconsistent or conflicting messages to those around them. Mental instability and mood swings may have the same result:
Partner: “I was married to two different men in those last few weeks. One was calm, very calm; the other was not.”
Whatever the reason, significant others found themselves faced with the task of weighing one set of signals against another and deciding whether to be concerned or reassured by what they saw.
Difficulties in interpreting and heeding distress signals
Several informants admitted to having allowed themselves to believe that nothing was seriously amiss. Several factors seem to have contributed to their decisions, not always conscious, to heed the positive signs and disregard the more ominous ones.
Alcohol and drugs may not only have interfered with the ability of the deceased to communicate distress effectively. One group of friends confessed that their capacity to recognise the gravity of the situation was also compromised:
Friend: “None of us could see clearly . . . We were all in a drug-fuelled haze.”
Family members blamed busy lives and competing claims on their attention. Several reported that they were preoccupied at the time by other events or circumstances, including health problems elsewhere in the family:
Father: “My son’s got very serious asthma and that gets him down . . . I was more concerned about him doing something like this than her . . . I knew she was depressed but she seemed to be so resilient . . . She could always bounce back.”
This quotation also illustrates popular notions of candidacy,28 which are evident throughout our data and may have predisposed relatives and friends to dismiss warning signs. Several informants insisted, even after the event, that the deceased was not “the suicidal type.”
Paradoxically, proximity of relationship may have acted as a barrier to awareness. Several accounts suggest that subtle changes in mental state or behaviour were overlooked because significant others were too close to the distressed person to see what was happening:
Mother: “For me it was quite a gradual thing . . . I suppose you just get used to the tiny little changes.”
Intimate knowledge of a person’s habits may also make it easy to explain away odd or disturbing behaviours and find plausible excuses for abnormal conduct. One parent told how, on being unable to contact her son, she had dismissed her concerns by telling herself, “He’s probably just gone off to Lanzarote again.” Another mother admitted to having interpreted her daughter’s withdrawal and irritability as the behaviour of an “overgrown moody teenager.” Distress may also be seen as a perfectly normal response to adverse personal circumstances, as in the case of one young man, whose evident desolation after the traumatic death of his wife rang no alarm bells whatsoever with family and friends.
All the accounts contain examples of behaviours that, with hindsight, were recognised by significant others as odd but that, at the time, were accepted as normal. This suggests a tendency in personal networks to stretch the boundaries of normality and to avoid pathologising distress or labelling behaviours as deviant, because to do so may be seen to imply rejection. This is clear from one mother’s account of an occasion on which her son tried to convey his confusion about his sexual identity. Her unconditional love and acceptance of him, together with her own liberal views, rendered her unable to recognise the extent to which he needed help:
Mother: “I said, well that’s OK, you’re still my son and I love you whatever you are . . . I didn’t want to show disapproval of him . . . I just wanted him to feel accepted.”
Several informants highlighted the necessity of trust within intimate relationships and attributed their inability to acknowledge what was happening to their implicit faith in the deceased. One told how his partner had repeatedly talked of suicide but had also given him assurances that she would not do it, and his love for her compelled him to believe her:
Partner: “I trusted her . . . You’ve got to trust the person. I mean, you have to have some faith in what that person’s telling you.”
Another participant told how, despite knowledge of her husband’s distress and a nagging awareness of the possibility of suicide, she could not bring herself to believe that he would do such a thing. The prospect was too awful to contemplate, and she confessed afterwards to having suppressed her fears because of her need to preserve her own mental health and to stay positive for the sake of the children. The concept of self preservation emerges strongly throughout the data. Several informants acknowledged that fear of being drawn into the other’s distress may have led them to withdraw support at a critical time:
Friend: “At the time I’d got a job and I needed to keep my head down . . . I thought, something’s going to happen to this person and I don’t really want to be there when it does . . . And at the end of the day I think I probably cut [him] off for reasons of self-preservation . . . In terms of responsibility, the ultimate responsibility you have is to yourself.”
Difficulties in taking action
Informants reported that, even when they were aware that something was seriously wrong, deciding to intervene, working out what action to take, and then summoning the courage to take it posed further challenges. The tendency to “watch and wait,” putting off decision making, was strong.
From the accounts, we identified three types of missed opportunity for intervention or actions that, with hindsight, informants thought might have helped to prevent the suicide: “saying something” to the distressed person, alerting others in the personal network, and seeking help outside the network.
“Saying something”
Several informants had recognised that the deceased was in trouble and had tried to talk to him or her. Others deeply regretted not saying anything. Some attributed their silence to awkwardness or embarrassment. Again, this was particularly associated with cases involving problems of sexual identity or illegal activity and with young male informants, who admitted that they lacked the confidence and skills to encourage peers to confide:
Sibling: “I don’t find it easy to talk about feelings myself . . . I guess we none of us are that brilliant at talking about our feelings, us lads, and when something like that happens it’s just like, oh bloody hell, what can you say?”
Some peer informants spoke of not feeling qualified to offer advice or not wishing to be accused of hypocrisy. In one case, the deceased’s friends were aware that he was consuming dangerous quantities of illegal drugs but did not feel able to say anything to him because they were heavy drug users themselves:
Friend: “We couldn’t really say too much because we were on that road with him . . . I was an addict myself . . . How can you tell someone they’re doing too many drugs when you’re sitting there getting absolutely mashed with them? . . . They’d think you’re a hypocrite.”
Respect for the person’s privacy and autonomy prevented some from confronting problems directly. Trust in the person’s capacity to resolve his or her own problems may have played a part in this; equally, withdrawal on the part of the distressed person may have reinforced significant others’ belief that they should not intrude:
Colleague: “Actually I thought I should give him a bit of privacy . . . I thought he wanted to be on his own . . . All the signs he was sending me suggested he didn’t want to be with anyone . . . and I respected that.”
Parents spoke of not wanting to be seen to be fussing or interfering in their children’s lives:
Father: “As his father, I’d always struggled with getting the balance right between being supportive enough but not being so supportive that I got in the way of his own independent development . . . There was always that tension in my relationship with him . . . And I felt that he too was trying to be an adult and not wanting to divulge everything to his father.”
In other cases, the fear of “saying the wrong thing” and thereby alienating the distressed person or making the situation worse was overwhelming. One informant, aware that his partner’s mental state was highly unstable, was terrified that he might “tip her over the edge” if he chose the wrong words or the wrong moment. Underlying this was a fear of inflicting irreparable damage on the relationship. Others reported similar struggles:
Sibling: “I guess I was scared that he’d just say, stay out of my life . . . I think me and mum both had the fear of not wanting to alienate him really.”
Alerting others in the network
Several accounts highlighted the importance of sharing concerns with other members of the family or social network at the earliest opportunity. This may enable significant others to check hunches, gather corroborating evidence, and summon the confidence to act and also increase the chances of weaving an effective safety net around the distressed person. However, informants identified a series of barriers to information sharing. Some blamed their own relationship difficulties for breakdowns in communication:
Mother: “I find it very hard to speak to his father . . . It was a very bitter divorce . . . very, very bitter.”
In another case, the deceased’s employers held crucial information but were prevented by confidentiality from sharing it with his parents, despite their urgent enquiries:
Father: “It’s this Secret Service thing . . . I told them, he’s not answering his phone, he’s not answering his e-mails, and they still wouldn’t tell me he was off work sick . . . I mean this was in July, and they wouldn’t tell us that he hadn’t been in work since February.”
Several accounts suggested that the distressed person may have tried to limit the spread of information around the social network by confiding in a single, trusted friend and extracting promises that the information would not be shared with others. One informant described how his partner had presented him with an agonising moral dilemma, to tell or not to tell:
Partner: “I was having a wrestling match with myself . . . between respecting the privacy and trust of a person I cared about, and at the same time knowing that breaching that trust might be the best thing to do . . . I’d given her my word that I wouldn’t talk to her mother and I didn’t breach that trust. And I wish I had . . . But I thought, she’ll go bloody doolally if she finds out and that’ll really set things off . . . I had an awful lot to lose and I ended up losing it anyway.”
Although a confiding relationship is generally held to be the best protection against suicide, this eloquent account highlights the unbearable strain placed on sole confidants when they are entrusted with vital information but sworn to secrecy. Peer informants told how a desire to protect their friend had prevented them from sharing information with parents or employers:
Friend: “There were occasions on which he told me things and said, please don’t tell anyone else . . . In an ideal world I would have spoken to somebody where he worked . . . but that’s crossing such a big boundary. It’s like grassing . . . because he might have lost his job.”
Seeking help outside the network
Finally, informants talked about the difficulty of knowing when, where, and how to seek help outside the social network. Even informants who worked in the health sector or had experience of using mental health services themselves complained of lack of knowledge of available avenues. In some cases, lack of confidence and a fear of not being taken seriously may have deterred both the deceased and significant others from approaching professional agencies:
Mother: “Probably he thought, oh, they won’t believe me anyway, ’cos that was drummed into his head when he was being abused . . . If you’re not very good at explaining, which I feel sometimes I’m not, I’m not very good with big words and whatever, you just can’t get over how you feel.”
Others made it clear that their family’s coping style did not include seeking professional help:
Mother: “We’re basically copers, my family . . . Stiff upper lip, don’t make a big deal of it, don’t let’s have a drama . . . I haven’t been near my GP since all this happened.”
Previous bad experiences of mental healthcare, the negative public image of local services, and the desire to protect the loved one from involuntary incarceration were all cited as disincentives to seeking medical advice:
Mother: “He was very, very scared of being sectioned . . . because some of the people he knew had been sectioned . . . That’s why [friend] didn’t call the police . . . because she knew he was frightened.”
Another informant spoke poignantly of her confidence in her own ability to manage the situation and her belief in the healing power of love:
Partner: “I know I’m naive and ridiculous, but I believed . . . that my love and the children’s unconditional love . . . would be enough. Ultimately I thought we would heal him.”
Some informants admitted that, misjudging the urgency of the situation and unsure of the best approach to take, they had simply put off taking any action at all.
Discussion
As the suicidal process unfolds, significant others are required to make a series of complex decisions about what is happening and what, if anything, they should do about it. They must collect and weigh evidence from a range of sources, correctly decipher and assess the significance of both signs and countersigns, identify the appropriate actions to take, and then summon the courage to take them. Risks are involved at every stage; cherished relationships are at stake. Significant others must weigh the danger of doing nothing against the perceived dangers of saying or doing “the wrong thing.”
Experts agree that a clear and unambiguous warning message is a prerequisite for effective disaster planning and crisis management.29 Our data suggest that, in a suicidal crisis, members of the family and social network may not always receive a clear and unambiguous warning message. This may be because the person fails to give out a clear enough distress signal or because distress signals are given but significant others cannot decode them correctly at the time. Equally, they may not be able to bring themselves to accept that anything is seriously wrong or that suicide is a possibility. Writing in another context, about clinical identification of child abuse, one author comments: “[It] is a difficult intellectual and emotional exercise. . . The biggest barrier to diagnosis is the existence of emotional blocks in the minds of professionals.”30 The emotional blocks that can operate in clinical practice are magnified many times in close personal relationships, where every word or action may be emotionally charged and gauging the right response is critical. Our findings suggest that those very relationships, generally believed to be a protective factor for suicide,31 32 may sometimes heighten risk by acting as barriers to both awareness and intervention.
Research into the prevention and management of civil disasters suggests that critical errors in judgment often result from the so-called “normalcy bias,” defined as the tendency of people who have never experienced a catastrophe to disregard ominous signs and behave as if nothing is wrong. The strong desire for everything to be normal inclines people to believe that it is, even in the face of evidence to the contrary.33 Our findings suggest that this same principle may operate at the private level, particularly in the context of family life. The cycles of avoidance model, proposed by Biddle et al to account for non-help seeking for mental distress, provides an alternative framework that also fits our data well.34 Although Biddle and colleagues generated the model in relation to self referral, it also works for lay referral. Our data show that lay people may go to considerable lengths to avoid pathologising the distress of those close to them; their thresholds are repeatedly pushed back by powerful emotions, especially fear of the consequences (for themselves, as well as for the distressed person) of acknowledgment and intervention.
Limitations and strengths of study
Our data come from retrospective accounts of completed suicides. We had no corresponding data on prevented suicides with which to compare them and no way of testing hypotheses prospectively. Knowledge of the outcome of historical events powerfully shapes the construction of a narrative. In reconstructing events that have had a shattering effect on their own lives, informants will be driven by the “quest after meaning,” avidly searching for clues that they may have missed at the time and reading significance into verbal and non-verbal behaviours in the light of subsequent events. The research interview may intensify this process. Moreover, informants may have felt under pressure to justify and excuse their own perceived failure to avert the tragedy, thus producing narratives that are primarily defensive in orientation.13 This may have resulted in an overemphasis on barriers and blocks and on the role of countersigns in “throwing them off the scent.” The interviewer was highly conscious throughout the interview process of its potential to induce guilt and self blame and drew on a background in social work to help participants to acknowledge and harness painful emotions. These considerations do not diminish the authenticity of the narratives or the plausibility of the analysis and interpretation. A major strength of our study lies in the level of validation by respondents that we achieved through ongoing engagement with participants,35 three of whom provided “participant reviews” before we submitted this manuscript.
Our numbers are small because negotiating access to social networks was slow and labour intensive, but our methods generated exceptionally rich data. Kendall et al argue that the time consuming nature of data generation and concerns about small sample size should not deter researchers from using multiperspective qualitative interviews.8
We had to exclude socially isolated cases, but this is true for all psychological autopsy-type studies that rely on interviews with members of the deceased’s family and social network. Our research was designed specifically to learn from cases in which, despite the presence of a social support network, a fatal outcome could not be averted.23 The strength of our qualitative approach lies in its potential to generate deep insight into the way in which the suicidal process unfolds in particular micro-social contexts and the way in which events are construed, both at the time and in retrospect, by significant others.
Implications
Any decision to seek medical help during a possible suicidal crisis is the result of a long, perilous, and emotional journey, and family members’ concerns should always be taken seriously. The difficulties described by these lay people can only be tackled through public education, but our findings challenge the models on which many public health campaigns rely—namely “see-do” or “see-say-do.” Guidance typically takes the form of either “If you see this, you should do that” (see-do) or “If you see this, you should encourage the afflicted person to do that” (see-say-do). These models are based on two assumptions: that people can be taught what signs to look for and that, when they spot them, they will act rationally and in accordance with received guidance. Our data suggest that in practice it is not always so straightforward. Their proximity to the distressed person and their emotional investment in the relationship, together with a range of other factors, may prevent significant others from seeing, saying, and doing anything at all. The figure represents these obstacles, which should be explicitly tackled in training programmes that aim to improve suicide awareness and intervention skills.36 37 38 In particular, people may need to be reassured that to act on their concerns may save life and that this may mean having to disregard customary codes of respect that usually limit intrusion into another person’s emotional life. Our findings may be also useful in suicide bereavement work, to help assuage the guilt of relatives and friends.
Potential barriers to awareness and intervention in family and social networks
Much has been written on the nature of clinical judgment and on the ability of clinicians to recognise and respond to risk of suicide.39 40 41 Further research may be needed to understand the nature of lay judgment; the role of emotions, as opposed to rational thinking, as drivers of healthcare decision making; and the way those decisions are situated in social networks.42
What is already known on this topic
Prevention of suicide is “everybody’s business,” requiring concerted effort by health and non-health agencies, community groups, and members of the public
Very little is known about the role that lay people can play in suicide prevention, what challenges it poses for them, and what resources they need to contribute effectively
What this study adds
During a suicidal crisis, significant others are required to make a series of highly complex decisions about what is happening and what, if anything, they should do about it
Their proximity to the suicidal person, their emotional investment in the relationship, and a range of other factors make it difficult for them to decipher and heed warning signs and take appropriate action
Interventions to promote public involvement in suicide prevention should highlight the ambiguous nature of warning signs and explicitly tackle the emotional blocks to awareness and intervention
We thank all the participants who contributed their personal stories, and especially those who helped with ongoing interpretation of findings. We also thank Susan Lumb, who transcribed the interviews, and Tony Jorm and Betty Kitchener for their helpful comments on an earlier draft of the manuscript.
Contributors: CO had the idea for the study and was principal investigator, analysed the data, and wrote drafts of the manuscript. GO helped to develop the methods, collected and analysed the data, and helped with interpretation. JB, KL, JD, and HL were involved in designing the study and interpreting the findings. HL also read transcripts and helped to develop the analytical framework. JB advised on ethical matters. FR helped to develop the methods. GO, JB, FR, and HL commented on an earlier draft of the manuscript. All authors have seen and approved the final version of the manuscript. CO is the guarantor.
Funding: The study was funded by the UK Medical Research Council, grant number G0600296. CO was partly supported during the writing of this paper by NIHR CLAHRC for the Southwest Peninsula. The views expressed are those of the authors and not necessarily those of the MRC, NHS, NIHR, or Department of Health. The sponsor for the study was Devon Partnership NHS Trust. The role of the sponsor was to ensure that the study was carried out in accordance with the Research Governance Framework issued by the Department of Health. Neither the funder nor the sponsor played any role in the study design; in the collection, analysis, and interpretation of data; or in the drafting of this paper.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf and declare no financial relationships with any organisations that might have an interest in the submitted work in the previous three years, and no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study was approved by London NHS Multicentre Research Ethics Committee, reference number 07/MRE02/36. Each informant gave signed consent immediately before interview.
Data sharing: No additional data available.
Cite this as: BMJ 2011;343:d5801
References
- 1.World Health Organization. Suicide prevention (SUPRE). 2010. www.who.int/mental_health/prevention/suicide/suicideprevent/en/.
- 2.Department of Health. National suicide prevention strategy for England. Department of Health, 2002.
- 3.Scottish Executive. Choose life: a national strategy and action plan to prevent suicide in Scotland. Stationery Office, 2002.
- 4.Associate Minister of Health. New Zealand suicide prevention strategy 2006-2016. Ministry of Health, 2006.
- 5.Government of Western Australia Department of Health. Western Australian suicide prevention strategy 2009-2013: everybody’s business. Department of Health, 2009.
- 6.Appleby L, Shaw J, Amos T, McDonnell R, Harris C, McCann K, et al. Suicide within 12 months of contact with mental health services: national clinical survey. BMJ 1999;318:1235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry 2002;159:909-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kendall M, Murray S, Carduff E, Worth A, Harris F, Lloyd A, et al. Use of multiperspective qualitative interviews to understand patients’ and carers’ beliefs, experiences, and needs. BMJ 2009;339:196-9. [DOI] [PubMed] [Google Scholar]
- 9.Hawton K, Appleby L, Platt S, Foster T, Cooper J, Malmberg A, et al. The psychological autopsy approach to studying suicide: a review of methodological issues. J Affect Disord 1998;50:269-76. [DOI] [PubMed] [Google Scholar]
- 10.Owens C, Booth N, Briscoe M, Lawrence C, Lloyd K. Suicide outside the care of mental health services: a case-controlled psychological autopsy study. Crisis 2003;24:113-21. [DOI] [PubMed] [Google Scholar]
- 11.Owens C, Lloyd K, Campbell J. Access to health care prior to suicide: findings from a psychological autopsy study. Br J Gen Pract 2004;54:279-81. [PMC free article] [PubMed] [Google Scholar]
- 12.Owens C, Lambert H, Donovan J, Lloyd K. A qualitative study of help seeking and primary care consultation prior to suicide. Br J Gen Pract 2005;55:503-9. [PMC free article] [PubMed] [Google Scholar]
- 13.Owens C, Lambert H, Lloyd K, Donovan J. Tales of biographical disintegration: how parents make sense of their sons’ suicides. Sociol Health Illn 2008;30:237-54. [DOI] [PubMed] [Google Scholar]
- 14.Britten N. Qualitative interviews in health care research. In: Pope C, Mays N, eds. Qualitative research in health care. 2nd ed. BMJ Books, 2000.
- 15.Holloway W, Jefferson T. Doing qualitative research differently: free association, narrative and the interview method. Sage, 2000.
- 16.Wengraf T. Qualitative research interviewing: biographic narrative and semi-structured methods. Sage, 2001.
- 17.McCance T, McKenna H, Boore J. Exploring caring using narrative methodology: an analysis of the approach. J Adv Nurs 2001;33:350-6. [DOI] [PubMed] [Google Scholar]
- 18.Cannon S. Social research in stressful settings: difficulties for the sociologist studying the treatment of breast cancer. Sociol Health Illn 1989;11:62-77. [Google Scholar]
- 19.Lee RM. Doing research on sensitive topics. Sage, 1993.
- 20.Holstein K, Gubrium J. Active interviewing. In: Silverman D, ed. Qualitative research: theory, method and practice. Sage, 1997.
- 21.Britten N, Jones R, Murphy E, Stacy R. Qualitative research methods in general practice. Oxford University Press, 1995. [DOI] [PubMed]
- 22.Ritchie J, Spencer L, O’Connell W. Carrying out data analysis. In: Ritchie J, Lewis J, eds. Qualitative research practice: a guide for social science students and researchers. Sage, 2003.
- 23.Owens C, Owen G, Lambert H, Donovan J, Belam J, Rapport F, et al. Public involvement in suicide prevention: understanding and strengthening lay responses to distress. BMC Public Health 2009;9:308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Biddle L, Brock A, Brookes S, Gunnell D. Suicide rates in young men in England and Wales in the 21st century: time trend study. BMJ 2008;336:539-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gunnell D, Bennewith O, Hawton K, Simkin S, Kapur N. The epidemiology and prevention of suicide by hanging: a systematic review. Int J Epidemiol 2005;34:433-42. [DOI] [PubMed] [Google Scholar]
- 26.Jefferson G. The rejection of advice: managing the problematic convergence of a “troubles-telling” and a “service encounter.” J Pragmat 1981;5:399-422. [Google Scholar]
- 27.Hale R. Psychoanalysis and suicide: process and typology. In: Briggs S, Lemma A, Crouch W, eds. Relating to self-harm and suicide: psychoanalytic perspectives on practice, theory and prevention. Routledge, 2008.
- 28.Davison C, Smith GD, Frankel S. Lay epidemiology and the prevention paradox: the implications of coronary candidacy for health education. Sociol Health Illn 1991;13:1-19. [Google Scholar]
- 29.Nigg J. Risk communication and warning systems. In: Amendola A, Horlick-Jones T, Casale R, eds. Natural risk and civil protection. E & FN Spon, 1995.
- 30.Speight N. ABC of child abuse: non-accidental injury. BMJ 1989;298:879-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maris R. Social forces in urban suicide. Dorsey Press, 1969.
- 32.Maris R. Pathways to suicide: a survey of self-destructive behaviors. Johns Hopkins University Press, 1981.
- 33.Omer H, Alon N. The continuity principle: a unified approach to disaster and trauma. Am J Community Psychol 1994;22:273-87. [DOI] [PubMed] [Google Scholar]
- 34.Biddle L, Donovan J, Sharp D, Gunnell D. Explaining non-help-seeking amongst young adults with mental distress: a dynamic interpretive model of illness behaviour. Sociol Health Illn 2007;29:983-1002. [DOI] [PubMed] [Google Scholar]
- 35.Mays N, Pope C. Quality in qualitative health research. In: Pope C, Mays N, eds. Qualitative research in health care. 2nd ed. BMJ Publishing, 2000.
- 36.Kitchener B, Jorm A. Mental health first aid training for the public: evaluation of effects on knowledge, attitudes and helping behavior. BMC Psychiatry 2002;2:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kelly C, Jorm A, Kitchener B, Langlands R. Development of mental health first aid guidelines for suicidal ideation and behaviour: a Delphi study. BMC Psychiatry 2008;18:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mellanby R, Hudson N, Allister R, Bell C, Else R, Gunn-Moore D, et al. Evaluation of suicide awareness programmes delivered to veterinary undergraduates and academic staff. Vet Rec 2010;167:730-4. [DOI] [PubMed] [Google Scholar]
- 39.MacNaughton J. Clinical judgement. In: Jones R, Britten N, Culpepper L, Gass D, Grol R, Mant D, et al, eds. Oxford textbook of primary medical care. Vol 1: principles and concepts. Oxford University Press, 2004.
- 40.Rutz W, Knorring L, Walinder J. Frequency of suicide on Gotland after systematic postgraduate education of general practitioners. Acta Psychiatr Scand 1989;80:151-4. [DOI] [PubMed] [Google Scholar]
- 41.Hendin H, Maltsberger J, Lipschitz A, Haas A, Kyle J. Recognizing and responding to a suicide crisis. Suicide Life Threat Behav 2001;31:115-28. [DOI] [PubMed] [Google Scholar]
- 42.Pescosolido BA. Beyond rational choice: the social dynamics of how people seek help Am J Sociology 1992;97:1096-138. [Google Scholar]