Abstract
Background:
Alterations in scapular and glenohumeral kinematics in patients with shoulder dysfunction have been recognized by this studies authors' and described in multiple other studies available in the literature. A reliability study was developed to assess a new technique for measuring scapulohumeral kinematics. Previous scapular position measuring techniques may require expensive equipment which decreases clinical utility. Other techniques require identification of multiple anatomic landmarks that may decrease accuracy, precision, and reliability.
Methods:
A sample of asymptomatic controls and symptomatic study subjects were recruited. Each subject had markers placed on each acromion and stood at a standardized distance in front of a light. The shadow projected from the acromial marker onto a standardized, data collection board was measured during the resting, flexion, and scaption positions for bilateral shoulders. The horizontal and vertical translations of the shadows were measured compared to the resting point for both flexion and scaption.
Results:
The scapula translated superiorly and medially during both flexion and scaption movements in all subjects and controls. There was good inter-rater reliability for measuring scapular translation with scaption (ICC= 0.81) and moderate reliability for measuring scapular translation with flexion (ICC = 0.62). There was increased superior and medial scapular translation in the subjects with flexion (p= 0.004 and p=0.002) and scaption (p= 0.01 and p=0.007) in the symptomatic shoulder compared to the asymptomatic shoulder. Superior scapular translation with flexion (p=0.0003) and scaption (p=0.006) and medial scapular translation with flexion (p<0.0001) and scaption (p<0.0001) was greater in the symptomatic subjects compared to controls.
Conclusions:
The scapula translates both superiorly and medially with flexion and scaption in asymptomatic and symptomatic subjects. After shoulder surgery, patients have increased superior and medial translation of the scapula compared to 1) their asymptomatic shoulder and 2) an asymptomatic control group. The current technique has good inter-rater reliability (ICC=0.81) when measuring scaption and moderate reliability when measuring flexion (ICC=0.62).
Level of Evidence:
III Diagnostic Case-Control Study
Keywords: Measurement of scapular position scapular kinematics, scapular dyskinesis
BACKGROUND
It has been noted anecdotally by the authors of this manuscript that when patients with shoulder pain and dysfunction attempt glenohumeral flexion or scaption, there is increased trapezius activation and subsequent scapulohumeral elevation.1 We have noted that with this scapulohumeral substitution, the acromial aspect of the scapula appears to translate both superiorly and medially. We have recognized these alterations in scapulohumeral kinematics in both nonoperatively treated patients with shoulder dysfunction and also in patients in the early postoperative period after shoulder surgery. Other authors have also identified increased superior translation of the scapula2–4, increased lateral rotation of the scapula5–6, and a more upwardly rotated scapula7 in patients with symptomatic shoulders due to a variety of pathologies. It is difficult to determine if this scapulohumeral substitution is a negative consequence of shoulder dysfunction, or an adaptive process that benefits the patient with shoulder dysfunction. Unfortunately, previously described methods of measuring scapular movements require expensive equipment2,5,7–15 or require identification of multiple anatomic landmarks that could cause a decrease in precision, accuracy, and reliability of measurements.2,16–19 In an attempt to further investigate whether scapulohumeral substitution in patients with shoulder dysfunction is an adaptive process or a negative consequence, the authors developed a new technique for measuring scapulohumeral position. This technique can be readily performed in the physical therapist's or orthopaedist's clinic and does not require expensive equipment.
The purpose of this study was to investigate the reliability of a novel technique for measuring scapulohumeral translation. The initial hypotheses of this study was that this novel technique for measuring scapulohumeral translation will: 1) demonstrate at least moderate inter-rater reliability20 in measuring scapular translation during shoulder flexion and scaption. Additionally, the authors hypothesized that the acromial aspect of the scapula will translate superiorly and medially during shoulder flexion and elevation in the scapular plane (scaption). Lastly, the authors hypothesized that: 1) there would be no difference in scapular translation between the dominant and non-dominant shoulders in asymptomatic control patients, 2) there would be a difference in scapular translation between the symptomatic shoulder and the asymptomatic shoulder in subjects with unilateral shoulder dysfunction, and 3) there would be a difference in scapular translation between subjects with postoperative shoulder dysfunction and asymptomatic controls.
METHODS
After institutional review board approval was obtained, the inter-rater reliability of this novel technique was examined by recruiting 10 asymptomatic individuals (ages 25-50) from the staff of the rehabilitation department of the authors' institution. Inclusion for subjects in the reliability pilot study required that these individuals had no prior history of shoulder pain or dysfunction, and all had symmetric range of motion of bilateral shoulders in both the scaption and flexion motions. Three physical therapists (RO, DS, JE), each with at least 13 years of experience treating musculoskeletal conditions about the shoulder complex, independently assessed each study participant using this novel technique for measuring scapular translation. Each investigator was blinded to the other investigators' ratings. Inter-rater reliability was determined for scapulohumeral movement in the sagittal plane (superior/inferior) and the coronal plane (medial/lateral) for both glenohumeral flexion and scaption.
To determine the amount of scapular translation that occurs in asymptomatic individuals during glenohumeral flexion and scaption, a second cohort of 18 asymptomatic individuals (mean age 37; range 26-50) were recruited from the staff of the rehabilitation department of the authors' institution. Inclusion in this control group required that these individuals had no prior history of shoulder pain and dysfunction, and all had symmetric range of motion of bilateral shoulders in both the scaption and flexion motions. This cohort is hereafter referred to as the control group.
A third cohort of subjects was recruited to examine patients with shoulder dysfunction. This cohort included 13 patients in postoperative recovery from shoulder surgery (mean age 56; range 44-75) that were recruited from the physical therapy clinics of the authors' institution [Table 1]. These patients had symptoms of pain and weakness that are typical of postoperative patients in the various phases of rehabilitation after shoulder surgery. Exclusion criteria included patients with bilateral shoulder symptoms or cervical spine pathology.
Table 1.
Demographics of subjects.
| Patient # | Gender | Age | Procedure | Timepoint of Measurement (months after surgery) |
|---|---|---|---|---|
| 1 | Female | 56 | Arthroscopic Rotator Cuff Repair / Labral Repair | 3 months |
| 2 | Male | 56 | Arthroscopic Rotator Cuff Repair | 3 months |
| 3 | Male | 63 | Arthroscopic Rotator Cuff Repair | 3 months |
| 4 | Male | 75 | Arthroscopic Rotator Cuff Repair | 3 months |
| 5 | Male | 57 | Arthroscopic Rotator Cuff Repair | 1.5 months |
| 6 | Male | 44 | Arthroscopic Labral Repair | 5 months |
| 7 | Female | 46 | Arthroscopic Rotator Cuff Repair / Labral Repair | 5 months |
| 8 | Male | 54 | Arthroscopic Rotator Cuff Repair | 6 months |
| 9 | Male | 47 | Arthroscopic Rotator Cuff Repair | 4 months |
| 10 | Male | 62 | Arthroscopic Rotator Cuff Repair | 5 months |
| 11 | Male | 53 | Arthroscopic Rotator Cuff Repair | 2 months |
| 12 | Female | 56 | Arthroscopic Rotator Cuff Repair | 2 months |
| 13 | Male | 55 | Total Shoulder Arthroplasty | 2 months |
All subjects provided their informed consent for participation within this study. The participants in both the control and investigational cohorts were examined using this novel technique to examine scapulohumeral translation by a single physical therapist (RO) with 32 years' experience treating conditions of the shoulder complex. Side-to-side differences among the cohorts and differences between the cohorts were examined to determine if symptoms of shoulder pain and dysfunction affected the degree of scapulohumeral translation that occurs with glenohumeral flexion and scaption.
Measurement Technique
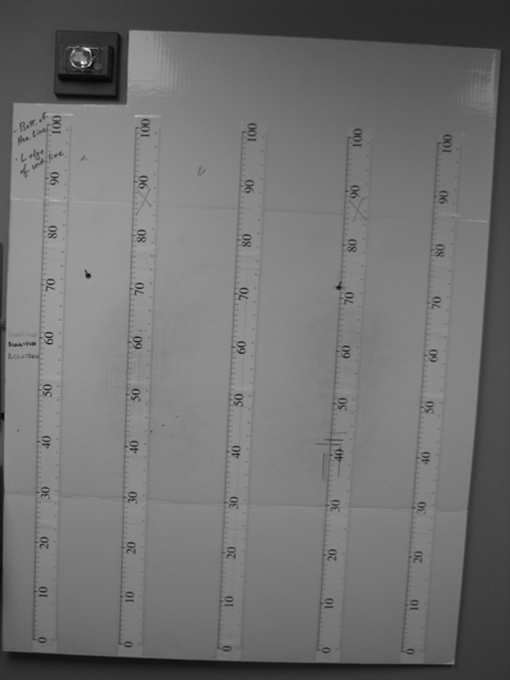
Each subject stood on a 55 cm long adhesive tape marker located on the floor parallel to and centered at 15 cm from a wall containing a specially formulated board upon which all data points were placed [Figure 1] This board was 91 cm wide by 121 cm tall and was mounted to the wall in a semi-permanent mount. The board contained five 100 cm long scales oriented vertically. A four foot level was utilized to ensure all scales were parallel to the floor surface and aligned with each other [Figure 2]. Each subject was instructed to stand in front of the board (on the adhesive tape) facing away from the board with retroreflective markers in place on each shoulder [Figure 3]. One retroreflective marker was placed on each shoulder between the acromioclavicular joint and the lateral acromion. The retroreflective markers were held in place with adhesive discs. A high intensity light (Lowel Pro-Light, Hauppauge, NY) was utilized to cast a shadow of the retroreflective markers on the board. The light was always positioned so it was centered on the board and was also always positioned at the same height (140 cm from floor surface) and the same distance from the board (200 cm) for all patients [Figure 4].
Figure 1.
Each subject stood on an adhesive tape marker located on the floor parallel to and centered 15 cm from a wall containing a specially formulated board.
Figure 2.
The specially formulated board positioned behind the subjects upon which all data points were placed.
Figure 3.
Each subject was instructed to stand in front of the board facing away from the board with retroreflective markers in place on each shoulder. Each retroreflective marker was placed on the shoulder between the acromioclavicular joint and the lateral acromion.
Figure 4.
A high intensity light was utilized to cast a shadow of the retroreflective markers on the board. The light was centered on the board and was always positioned at the same height and the same distance from the board for all subjects.
Each subject was properly disrobed to permit unrestricted motion of both upper extremities (women were asked to remove their bra if bra straps crossed the shoulder - a gown was utilized to provide adequate coverage for privacy) and permit visibility of the markers during movement of the shoulders. Each subject was instructed to center themselves directly above the center point of the tape with the feet spaced comfortably apart placing equal weight on each foot and facing away from the board toward the high intensity light. Subjects were instructed to remain still during the remainder of the session as the researchers placed marks on the board.
Prior to measurement, each subject was instructed to shrug their shoulders three to four times and then relax. Once the subject was relaxed and standing upright, the light was turned on and a colored pencil was used to place a single point mark at the highest point of the shadow cast by each retroreflective marker onto the board while the subject was at rest. The light was left on for the remainder of the session. Patients were then instructed to perform forward flexion to 90° with thumbs pointing toward the ceiling. The subject performed this motion three times and on the last movement the subject was advised to hold the position while marks were placed on the board with a different colored marker using the same procedure noted above. The position of 90° was visually estimated when the upper arm was parallel to the floor surface.21 Subjects were then instructed to perform elevation in the plane of the scapula to 90° with the thumbs pointing toward the ceiling. The subject again performed this motion three times and on the last movement the subject was advised to hold the position while marks were placed on the board with a different colored marker using the same procedure noted above.
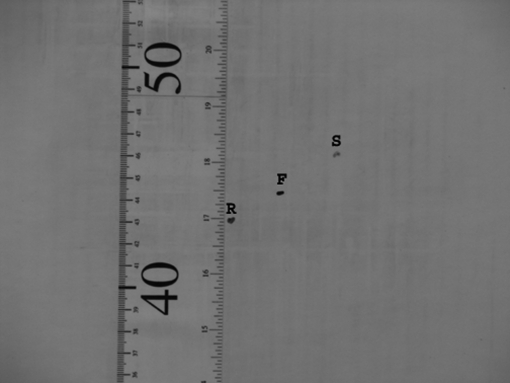
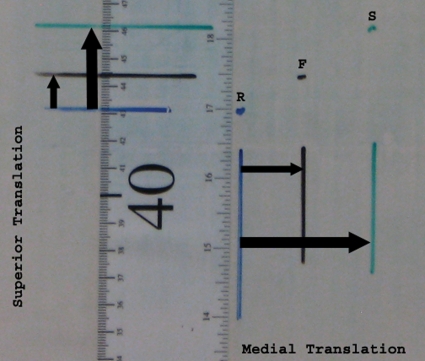
At the completion of the measuring phase there were three colored marks (dots) for each shoulder on the recording surface [Figure 5]. In order to measure the amount and direction of scapular translation in the superior/inferior plane, a bullet level was used to draw a horizontal line through the location of each “dot” that was recorded for each side (three colored dots on each side). The level line was extended so it intersected with one of the vertical measurement scales. The vertical numerical values for the resting, flexion and scaption positions were recorded. This number was recorded to the nearest millimeter. In order to measure the amount and direction of scapular translation in the medial/lateral plane, a bullet level was used to draw a plumb (vertical) line through the location of each colored mark (dot). The distance between the vertical (plumb) lines drawn from each colored mark was then measured with a standard non-elastic fiber tape graduated in millimeters and the result was recorded on a data collection sheet. The distance from the resting vertical line to the flexion vertical line and from the resting vertical line to the scaption vertical line was measured and the result recorded on the data collection sheet [Figure 6].
Figure 5.
The shadow projected by the light was marked at its apex for the resting position (R), the flexion position (F), and the scaption position (S).
Figure 6.
In order to measure the amount and direction of scapular translation that occurred with flexion and scaption, plumb lines were drawn in both the horizontal and vertical directions from the resting (R), flexion (F), and scaption (S) positions. The amount of superior and medial translation for flexion and scaption compared to the resting measurements were measured.
STATISTICAL ANALYSIS
Interrater reliability coefficients were calculated as random effects (i.e., conservatively assuming that the raters are a random subset of all possible raters) intraclass correlations using SAS® software and the method described by Shrout and Fleiss22 and Hamer.23 Fischer's test was used to determine whether statistically significant differences existed between reliability for the scaption and flexion measurements.24 Tests for normality were performed using the Shapiro-Wilk test. Differences between groups was determined by two-tailed t-tests using Excel 2003 (Microsoft, Redmond, WA). Alpha level for significance was preselected at p<.05.
RESULTS
Inter-rater Reliability for Determining Scapular Translation
The inter-rater reliability using this technique for measuring the amount of superior and medial translation of the scapula was determined to have moderate to good (ICC's ranging from 0.753-0.807) agreement20 [Table 2] as determined in the reliability study. When all measurements were examined collectively, scaption measurements (ICC = 0.807) were significantly more reliable than flexion measurements (ICC = 0.616) (z = 11.82, p < .0001).
Table 2.
Inter-rater reliability of scapular translation measurements.
| Test Measurement Position | ICC |
|---|---|
| Resting Position | 0.996 |
| Vertical Flexion Translation | 0.608 |
| Vertical S caption Translation | 0.704 |
| Horizontal Flexion Translation | 0.697 |
| Horizontal Scaption Translation | 0.723 |
| All Horizontal Measurements | 0.712 |
| All Vertical Measurements | 0.753 |
| All Flexion Measurements | 0.616 |
| All Scaption Measurements | 0.807 |
Direction of Scapular Translation
All controls demonstrated: 1) superior scapular translation (elevation) with scaption (2.6+1.3 cm) and 2) medial scapular translation with both flexion (2.4+0.9 cm) and scaption (2.8+1.1 cm). For shoulder flexion, 16 of 18 controls demonstrated superior scapular translation for both dominant and non-dominant shoulders (1.6+1.2 cm). In the superior/inferior direction, one patient demonstrated no scapular translation with dominant shoulder flexion and one patient showed no scapular translation with non-dominant shoulder flexion. None of the controls demonstrated lateral or inferior scapular translation. The scaption measurements within the control population were determined to be normally distributed (p=.80).
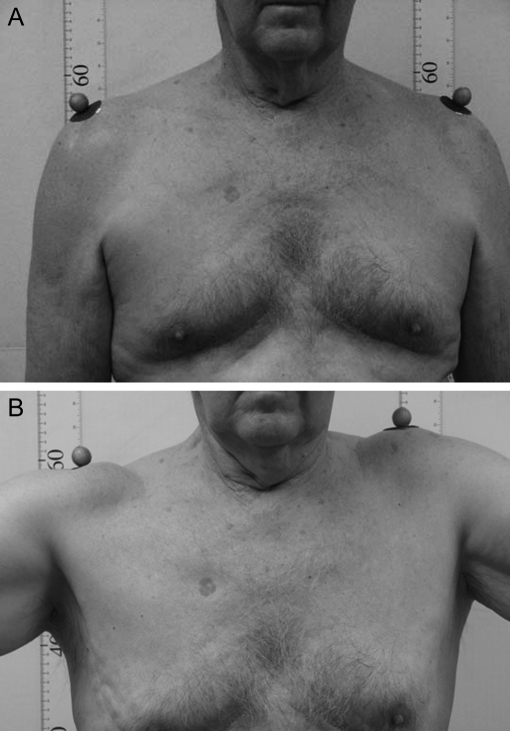
In the post-operative subjects, all symptomatic shoulders demonstrated both superior scapular translation with both flexion (4.1+1.9 cm) and scaption (4.7+2.2 cm) and medial scapular translation with both flexion (5.4+1.6 cm)and scaption (6.2+2.0 cm) [Figure 7a and 7b]. Of these subjects' asymptomatic shoulders, 11 of 13 demonstrated both superior and medial scapular translation with both flexion and scaption. One subject's asymptomatic shoulder showed no scapular translation with shoulder flexion (in the superior/inferior plane) and one subject's asymptomatic shoulder showed no scapular translation (in the medial/lateral plane) with shoulder flexion. No post-operative subjects demonstrated lateral or inferior scapular translation.
Figure 7.
(A) A subject with unilateral left shoulder symptoms is photographed in the resting position. (B) The same subject with unilateral left shoulder pain demonstrates superior and medial scapular translation occurring during shoulder scaption.
Difference in scapular translation between dominant and non-dominant shoulders in the control group
The control group was used to determine if a difference existed in the degree of scapulohumeral movement between dominant and non-dominant shoulders. There were no statistically significant differences found in relation to shoulder dominance for the degree of superior scapular translation with flexion (p=0.84) and scaption (p=0.89) or medial scapular translation with flexion (p=.68) and scaption (p=0.07) [Table 3].
Table 3.
Scapular translation between dominant and non-dominant shoulders in the control group.
| Dominant | Non-Dominant | P-value | |
|---|---|---|---|
| Flexion Superior Translation | 1.6±1.2 cm | 1.5±1.3 cm | 0.84 |
| Scaption Superior Translation | 2.7±1.3 cm | 2.6±1.2 cm | 0.89 |
| Flexion Medial Translation | 2.4±1.0 cm | 2.3±0.8 cm | 0.68 |
| Scaption Medial Translation | 3.1±1.3 cm | 2.4±0.9 cm | 0.07 |
Comparison of Scapular Translation between the Symptomatic Shoulder and the Asymptomatic Shoulder in the Post-Operative Subjects
In the post-operative subjects, there was a statistically significant difference between the symptomatic shoulder and the asymptomatic shoulder regarding superior scapular translation with flexion (p= 0.004) and scaption (p= 0.01) and the degree of medial scapular translation with flexion (p=0.002) and scaption (p= 0.007). However, there was no significant difference in the static resting position of the symptomatic and asymptomatic shoulder [Table 4].
Table 4.
Scapular translation between the symptomatic shoulder and the asymptomatic shoulder in the post-operative subjects.
| Symptomatic Shoulder | Asymptomatic Shoulder | P-value | |
|---|---|---|---|
| Resting Value | 52.3±7.9 cm | 52.1±7.2 cm | 0.953 |
| Flexion Superior Translation | 4.14±1.87 cm | 2.40±1.29 cm | 0.004 |
| Scaption Superior Translation | 4.72±2.24 cm | 2.69±1.44 cm | 0.01 |
| Flexion Medial Translation | 5.36±1.62 cm | 2.58±1.53 cm | 0.002 |
| Scaption Medial Translation | 6.24±1.98 cm | 3.48±1.76 cm | 0.007 |
Comparison of Scapular Translation between the Control Group and the Post-Operative Subjects
Since there was no statistical difference between dominant and non-dominant shoulders in the control group, the two were combined to compare the scapular translation of the control group to that of the symptomatic shoulder subjects. A statistically significant difference was found between the control group and the subjects for the degree of superior scapular translation with flexion (p=0.0003) and scaption (p=0.006) and the degree of medial scapular translation with flexion (p<0.0001) and scaption (p<0.0001) [Table 5].
Table 5.
Scapular translation between the controls and the post-operative subjects
| Controls | Post- Op Subjects | P-value | |
|---|---|---|---|
| Flexion Superior Translation | 1.6+ 1.2 cm | 4.14+1.87 cm | 0.0003 |
| Scaption Superior Translation | 2.6±1.3 cm | 4.72±2.24 cm | 0.006 |
| Flexion Medial Translation | 2.4±0.9 cm | 5.36+ 1.62 cm | 0.00001 |
| Scaption Medial Translation | 2.8+1.1 cm | 6.24+1.98 cm | 0.00003 |
Comparison of Side-to-side Differences between the Control and Post-Operative Subjects
For flexion measurements, the side-to-side differences were greater in the post-operative subjects for both superior translation (1.88+1.60 vs. 0.68+0.47 cm; p=0.02) and medial translation (2.79+2.50 vs. 1.27+0.83 cm; p= 0.05) compared to the control group. For scaption measurements, the side-to-side differences were also greater in the post-operative subjects for both superior translation (2.28+2.16 vs. 0.71+0.72 cm; p=0.02) and medial translation (3.22+2.54 vs. 1.34+1.07; p=0.07) compared to the control group.
Using this data, a side-to-side difference of 2 centimeters was shown to have a sensitivity of 0.55 and a specificity of 0.97 in demonstrating abnormal or pathologic scapular elevation with scaption.
DISCUSSION
The initial purpose of this study was to develop and investigate the reliability of a novel technique for measuring scapulohumeral translation. The hypotheses of this study were supported by the data and statistical interpretation.
This study demonstrates that the current technique has moderate to good inter-rater reliability in measuring both the superior and medial translation of the acromial aspect of the scapula that occurs with glenohumeral flexion and scaption in asymptomatic patients. Since scaption measurements were normally distributed in the control population and appear to be more reliable compared to flexion measurements, the authors of the current study recommend the use of scaption measurements over flexion measurements for assessment of scapulohumeral translation.
Patients assessed during their post-operative recovery after shoulder surgery demonstrated significantly increased scapular superior and medial translation compared to: 1) their asymptomatic shoulder and 2) an asymptomatic control group. In order to determine a reference measurement that may be used in future studies or clinical scenarios to demonstrate an abnormal amount of vertical translation that occurs with scaption in symptomatic subjects, the side-to-side difference was examined. The side-to-side difference in the control group was 0.71+0.72 cm and the difference in the postoperative subjects was 2.27+2.16 cm. Using a side-to-side difference of 2 centimeters as the reference measurement for pathological translation, the authors propose the use of a value that is close to two standard deviations greater than the mean side-to-side difference of the control group. This value also approximates the mean side-to-side difference of the postoperative subjects. Therefore, using a side-to-side difference of 2 centimeters as the reference value to demonstrate abnormal or pathologic scapular elevation with scaption reveals a sensitivity of 0.55 and a specificity of 0.97. These values support the use of a side-to-side difference of 2 centimeters as an appropriate clinical screening tool to examine for pathologic vertical scapular translation with scaption, when using this technique.
Although this manuscript describes a novel technique that demonstrates that the scapula translates medially and superiorly with glenohumeral flexion and scaption, it is not the first technique that documents scapular elevation. There have been several different techniques described for measuring scapular kinematics. Several of these techniques are able to analyze scapular kinematics in three dimensions2,5,7–9,14,25–28, whereas the currently described technique is only able to assess scapular kinematics in two dimensions. However, the advantages of the current technique is that it does not require expensive equipment such as the electromagnetic movement sensors2,5,7–10, digital inclinometers11–12, electromyography10,13, projectors and microcomputers14, or radiography.15 In addition, this new technique does not require identification of multiple anatomic landmarks that could cause a decrease in precision, accuracy, and reliability of measurements.2,16–19 Therefore, this method has been shown to be both reliable and easily reproducible in the physical therapist's or orthopaedist's clinic.
In addition to the inability of this technique to determine three dimensional scapular position, other potential limitations of this study include 1) small number of patients included in the study groups and 2) the heterogeneity of the patients included in the subject group. Additional studies should be expanded to include larger numbers of subjects as well as a more diverse subject pool by diagnosis (including those without operative diagnoses), age, and chronicity of shoulder dysfunction.
The findings of this current study are similar to several previously published findings. Lukasiewicz et al. also demonstrated that the scapula moved superiorly and medially with increasing arm elevation in the scapular plane.2 In addition, they showed that the patients with impingement demonstrated significantly greater superior translation of the scapula during arm elevation when compared to controls.2 However, unlike the current study, differences between the asymptomatic and symptomatic sides of patients with impingement were not significantly different.2 Babyar also found increased scapular elevation in symptomatic individuals although they suggested that scapular elevation could be influenced by verbal instruction and practice.3 Using Moiré topographical techniques, Warner et al. suggested that in patients with impingement the symptomatic shoulder is higher than the contralateral, asymptomatic side.4 Lastly, similar to the current findings, no side to side differences were demonstrated in scapular elevation during glenohumeral abduction in asymptomatic patients.29
Other studies have examined the concept of scapular substitution in patients with shoulder dysfunction.7,13 Utilizing a three dimensions electromagnetic motion-tracking system, Rundquist demonstrated that subjects with symptomatic shoulders exhibited more upwardly rotated scapulae when compared to the asymptomatic side.7 Fayad et al. also utilized an electromagnetic motion-tracking system to demonstrate increased scapular lateral rotation in patients with glenohumeral osteoarthritis and adhesive capsulitis.5 In the review of the literature for the current study, only one other study was identified that assessed postoperative scapular kinematics. Using an electromagnetic tracking device, increased lateral scapular rotation was identified in patients undergoing reverse shoulder arthroplasty when compared to those with healthy shoulders.6
Evidence of increased upper trapezius activation, combined with increased superior translation of the scapula, has been demonstrated in persons with shoulder pathology.9–10,30 Electromyographic studies have demonstrated an increased activation in the upper trapezius during shoulder elevation tasks in patients with symptomatic shoulders compared to asymptomatic patients.13,30 Patients with impingement had more upper and lower trapezius muscle activation compared with asymptomatic subjects.9 Ludeweg et al. suggested that excessive upper trapezius activation and imbalances of force production between the serratus anterior and the upper trapezius can result in a shoulder-shrugging motion with arm elevation causing increased superior translation of the scapula and less efficient upward rotation and reduced posterior tipping of the acromion.10
Rundquist suggested that scapular substitution may be a compensatory mechanism that allows a patient to continue to function in the presence of shoulder symptoms.7 Fayad et al. suggested that these alterations in scapular kinematics may help patients by providing a more effective scapular position for arm elevation.5 Negative consequences of scapular substitution and altered flexion and scaption patterns may include subacromial impingement, rotator cuff or biceps tendon irritation and subsequent tendinopathy, and altered acromioclavicular joint forces which may predispose to degenerative changes.9–10,30 In addition, the authors of the current study believe that altered scapular kinematics may be associated with a higher incidence of neck pain related to the trapezius.
As shoulder rehabilitation programs evolve, comparative testing of different rehabilitation approaches is needed. To improve our understanding of the mechanisms by which shoulder function is enhanced through rehabilitation, outcome assessments should address kinematic and muscle activity alterations as well as symptoms and functional status.9 Further research into the association between scapular substitution and the presence of pain and weakness is warranted in both operatively and nonoperatively treated patients. Further studies are needed to determine: 1) if postoperative scapulohumeral kinematic alterations can be modified and 2) what rehabilitative techniques are optimal for normalizing these alterations.
CONCLUSION
The novel technique for measuring scapulohumeral translation described herein demonstrated moderate to good reliability with scaption and flexion, respectively. It is easily reproducible in the clinic and does not require expensive equipment. With both scaption and flexion, the acromial aspect of the scapula tends to translate medially and superiorly and is representative of the alterations of the scapulohumeral region that occur with these movements. In asymptomatic individuals, there are no statistically significant differences in scapular translation between the dominant and non-dominant arms. Patients in their postoperative recovery after shoulder surgery have significantly increased superior and medial translation of the scapula compared to 1) their asymptomatic shoulder and 2) an asymptomatic control group. A side-to-side difference of two centimeters may signify an abnormal or pathologic amount of vertical scapular translation with scaption.
REFERENCES
- 1.Osborn R, Baumgarten KM. Unpublished data. 2011 [Google Scholar]
- 2.Lukasiewicz AC, McClure P, Michener L, et al. Comparison of 3-dimensional scapular position and orientation between subjects with and without shoulder impingement. J Orthop Sports Phys Ther 1999;29-10:574–83; discussion 84–6 [DOI] [PubMed] [Google Scholar]
- 3.Babyar SR. Excessive scapular motion in individuals recovering from painful and stiff shoulders: causes and treatment strategies. Phys Ther 1996;76-3:226–38; discussion 39–47 [DOI] [PubMed] [Google Scholar]
- 4.Warner JJ, Micheli LJ, Arslanian LE, et al. Scapulothoracic motion in normal shoulders and shoulders with glenohumeral instability and impingement syndrome. A study using Moire topographic analysis. Clin Orthop Relat Res 1992-285:191–9 [PubMed] [Google Scholar]
- 5.Fayad F, Roby-Brami A, Yazbeck C, et al. Three-dimensional scapular kinematics and scapulohumeral rhythm in patients with glenohumeral osteoarthritis or frozen shoulder. J Biomech 2008;41-2:326–32 [DOI] [PubMed] [Google Scholar]
- 6.Kontaxis A, Johnson GR. Adaptation of scapula lateral rotation after reverse anatomy shoulder replacement. Comput Methods Biomech Biomed Engin 2008;11-1:73–80 [DOI] [PubMed] [Google Scholar]
- 7.Rundquist PJ. Alterations in scapular kinematics in subjects with idiopathic loss of shoulder range of motion. J Orthop Sports Phys Ther 2007;37-1:19–25 [DOI] [PubMed] [Google Scholar]
- 8.Barnett ND, Duncan RD, Johnson GR. The measurement of three dimensional scapulohumeral kinematics–a study of reliability. Clin Biomech (Bristol, Avon) 1999;14-4:287–90 [DOI] [PubMed] [Google Scholar]
- 9.Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther 2000;80-3:276–91 [PubMed] [Google Scholar]
- 10.Ludewig PM, Hoff MS, Osowski EE, et al. Relative balance of serratus anterior and upper trapezius muscle activity during push-up exercises. Am J Sports Med 2004;32-2:484–93 [DOI] [PubMed] [Google Scholar]
- 11.Borsa PA, Timmons MK, Sauers EL. Scapular-Positioning Patterns During Humeral Elevation in Unimpaired Shoulders. J Athl Train 2003;38-1:12–7 [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson MP, McClure PW, Karduna AR. New method to assess scapular upward rotation in subjects with shoulder pathology. J Orthop Sports Phys Ther 2001;31-2:81–9 [DOI] [PubMed] [Google Scholar]
- 13.Kelly BT, Williams RJ, Cordasco FA, et al. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J Shoulder Elbow Surg 2005;14-2:165–71 [DOI] [PubMed] [Google Scholar]
- 14.Gomes PF, Sesselmann M, Faria CD, et al. Measurement of scapular kinematics with the moire fringe projection technique. J Biomech 2010;43-6:1215–9 [DOI] [PubMed] [Google Scholar]
- 15.Inman VT, Saunders JB, Abbott LC. Observations of the function of the shoulder joint. 1944. Clin Orthop Relat Res 1996-330:3–12 [DOI] [PubMed] [Google Scholar]
- 16.Lewis JS, Valentine RE. Intraobserver reliability of angular and linear measurements of scapular position in subjects with and without symptoms. Arch Phys Med Rehabil 2008;89-9:1795–802 [DOI] [PubMed] [Google Scholar]
- 17.DeVita J, Walker ML, Skibinski B. Relationship between performance of selected scapular muscles and scapular abduction in standing subjects. Phys Ther 1990;70:470–6 [DOI] [PubMed] [Google Scholar]
- 18.Kibler WB. Role of the scapula in the overhead throwing motion. Contemp Orthop 1991;22-525–532 [Google Scholar]
- 19.Gibson MH, Goebel GV, Jordan TM, et al. A reliability study of measurement techniques to determine static scapular position. J Orthop Sports Phys Ther 1995;21-2:100–6 [DOI] [PubMed] [Google Scholar]
- 20.Portney L, Watkins M. Foundations of Clinical research: Applications to Practice. Upper Saddle River, NJ: Prentice Hall, 2000 [Google Scholar]
- 21.Hayes K, Walton JR, Szomor ZR, et al. Reliability of five methods for assessing shoulder range of motion. Aust J Physiother 2001;47-4:289–94 [DOI] [PubMed] [Google Scholar]
- 22.Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psych. Bull. 1979;86:428–9 [DOI] [PubMed] [Google Scholar]
- 23.Hamer RM. A SAS macro for computing intraclass correlation coeffients. Virginia Commonwealth University, 1990 [Google Scholar]
- 24.Fisher RA. Statistical Methods for Research Workers. 1925
- 25.Johnson GR, Stuart PR, Mitchell S. A method for measurement of three-dimensional scapular movement. Clin Biomech (Bristol, Avon) 1993;8:269–73 [DOI] [PubMed] [Google Scholar]
- 26.An KN, Browne AO, Korinek S, et al. Three-dimensional kinematics of glenohumeral elevation. J Orthop Res 1991;9-1:143–9 [DOI] [PubMed] [Google Scholar]
- 27.Veeger HE, van der Helm FC, Chadwick EK, et al. Toward standardized procedures for recording and describing 3-D shoulder movements. Behav Res Methods Instrum Comput 2003;35-3:440–6 [DOI] [PubMed] [Google Scholar]
- 28.van der Helm FC, Pronk GM. Three-dimensional recording and description of motions of the shoulder mechanism. J Biomech Eng 1995;117-1:27–40 [DOI] [PubMed] [Google Scholar]
- 29.Hallaceli H, Manisali M, Gunal I. Does scapular elevation accompany glenohumeral abduction in healthy subjects? Arch Orthop Trauma Surg 2004;124-6:378–81 [DOI] [PubMed] [Google Scholar]
- 30.Lin JJ, Wu YT, Wang SF, et al. Trapezius muscle imbalance in individuals suffering from frozen shoulder syndrome. Clin Rheumatol 2005;24-6:569–75 [DOI] [PubMed] [Google Scholar]