Abstract
Study Objectives:
To investigate changes over 15 years in the prevalence of insomnia and its association with demographic characteristics and hypnotic medication use.
Design:
Analysis of 3 cross-sectional national mental health surveys carried out in 1993, 2000, and 2007, which used comparable sampling methods and identical insomnia assessments.
Setting:
Adults living in private households in England.
Patients or Participants:
20,503 people aged 16-64 years.
Measurements and Results:
Insomnia was defined according to 4 different criteria, using relevant questions from the revised Clinical Interview Schedule. Modest increases in insomnia prevalence were found over the survey periods (any symptoms increasing from 35.0% in 1993 to 38.6% in 2007; insomnia diagnosis from 3.1% to 5.8%, respectively). In all 3 surveys, similar strengths of association in relation to all criteria were found, with female gender, increased age, lower educational attainment, depression, unemployment, economic inactivity, and widowed, divorced, or separated status. Prevalence of hypnotic use was double in 2000 (0.8%) compared to 1993 (0.4%); from limited information on selected medications, there was no such increase between 2000 and 2007. The reasons reported for any sleep disturbance over the last month were generally similar across surveys, the most marked change being illness/discomfort increasing as an explanation from 14.3% to 17.4% to 19.0%.
Conclusions:
In the English general population, insomnia (by any definition) showed a modest but steady increase in prevalence over a 15-year period. Strengths of associations with demographic factors and self-reported reasons for sleep disturbance remained reasonably stable over this period.
Citation:
Calem M; Bisla J; Begum A; Dewey M; Bebbington PE; Brugha T; Cooper C; Jenkins R; Lindesay J; McManus S; Meltzer H; Spiers N; Weich S; Stewart R. Increased prevalence of insomnia and changes in hypnotics use in England over 15 years: analysis of the 1993, 2000, and 2007 national psychiatric morbidity surveys. SLEEP 2012;35(3):377-384.
Keywords: Insomnia, sleep, hypnotic use, national survey, trends
INTRODUCTION
Insomnia is a very common symptom with high economic and personal costs associated with decreased quality of life and functioning.1 In a recent UK study by Morphy and colleagues, 37% of respondents reported insomnia at baseline; a year later 69% of these still had problems sleeping, while 15% of those without insomnia at baseline had developed it.2 Insomnia is also a persistent condition. In a recent longitudinal study of people with insomnia at baseline, 74% still reported insomnia after a year, and 46% still reported insomnia after 3 years.3 More severe insomnia at baseline was more likely to persist.
Despite concerns in the media that the duration and quality of sleep have decreased over recent years, we know little about how the prevalence of insomnia has changed over time. A recent re-analysis of data from multiple different surveys of Finnish populations found evidence of an increase in the reporting of insomnia symptoms over a 10-year period.4 The authors also found evidence of increased self-reported consumption of hypnotic medication, but not in the prevalence of hypnotic use, implying increased use in people already receiving these agents. An analysis of medication use based on data from the National Psychiatric Morbidity Surveys of 1993 and 2000 found an increase in the prevalence of use of hypnotic medication.5 There have been concerns that sleep medication use has increased in spite of limited benefits and considerable drawbacks to its use.6
Comparing insomnia prevalence between places and populations is made difficult by differences in the definition of insomnia,7 which vary from self-reported symptoms of sleeplessness to the stricter DSM-IV criteria. Changes in insomnia over time can only genuinely be inferred from repeated surveys of single populations which have used comparable sampling methods and measurements. The aim of this paper was to investigate changes in prevalence in insomnia over a 15-year period, as well as the stability of its associations with demographic characteristics, use of hypnotic medication and subjective reasons given for sleep disturbance by participants. To achieve this we used data from 3 national surveys8 carried out in the UK in 1993, 2000, and 2007, all employing the same measurements and definitions of insomnia, allowing for comparisons based on identical data across time.
METHODS
Study Samples
The data for this paper were drawn from 3 separate national surveys of psychiatric morbidity among adults living in private households: the British National Surveys of Psychiatric Morbidity of 1993, 2000, and 2007. The first 2 surveys were carried out by the Office for National Statistics, while the 2007 survey was undertaken by the National Centre for Social Research (NatCen) in collaboration with the University of Leicester.
The first 2 surveys were carried out in England, Wales, and Scotland, whereas the 2007 survey was based only in England; therefore, for all 3 surveys, only residents from England were included in the analyses presented here. The lower age limit for participation was 16 years for all 3 surveys, but the upper age limit varied: 64 years for the 1993 survey, 74 years for the 2000 survey, and no upper age limit for the 2007 survey. For this reason, all analyses in this paper were limited to those under 65. The 1993 and 2000 surveys were carried out from January to April in their respective years, whereas data in the 2007 survey were collected throughout the year. Another notable difference was that the 1993 survey was paper based, whereas the 2000 and 2007 surveys used computer-assisted interviewing. In other respects, the last 2 surveys used the same methods as the first survey, in so far as this was possible, to maximize the comparability of results.8
All 3 surveys employed independent random sampling across the geographic areas in question and none sought to recruit previous participants or to sample from identical areas. The sampling methodology was comparable across all 3 surveys. In each, primary sampling units (postal sectors) were selected from the Small Users Postcode Address File stratified for region and social class composition to generate a nationally representative sample. Households were randomly selected from within each sampling unit and in households containing at least one member in the age range for that survey, one person was randomly selected and invited to participate. Response rates fell over time. In 1993, a total of 10,108 participants were interviewed (79.4% of those approached); in 2000, 8580 (67.1%) participants were interviewed; and in 2007, 7461 (56.6%) participants were interviewed.
Definitions of Sleep Disturbance
The revised Clinical Interview Schedule9 (CIS-R), a validated and widely used structured clinical interview for assessing psychiatric morbidity, was administered to all participants in all 3 surveys. It includes questions on 14 areas of functioning, including a section on sleep problems containing a series of stem and contingent questions. These 14 CIS-R subscales generate individual scores ranging from 0-4 or 0-5; a cut-off point ≥ 2 is conventionally applied to categorize symptoms at a significant level. Subscale scores are also conventionally summed to generate a total score signifying overall symptom burden.
Sleep disturbance was defined in the following 4 ways for this analysis according to Ohayon's recommendations,7 and as previously reported for the 2000 survey10:
Insomnia symptoms: Any complaint of difficulty initiating or maintaining sleep in the previous month.
Insomnia of (at least) moderate severity: spending ≥ 1 hour trying to get to sleep or trying to get back to sleep on ≥ 4 occasions in the previous week.
Insomnia and fatigue: any complaint of difficulty initiating or maintaining sleep in the previous month and significant reported daytime fatigue in the past week (CIS-R fatigue subscale (B) score ≥ 2).
Insomnia diagnosis (a category approximating DSM-IV criteria for primary or secondary insomnia): moderate insomnia (see definition 2) with both daytime fatigue and duration of ≥ 6 months.
No data were available on subjective sleep quality, and this was not a criterion for any of the definitions of sleep disturbance in this study. Participants who reported any sleep problems (over- or under-sleeping) over the previous month were also asked to select a single principal reason for these problems from a list (see Table 4). The frequency of responses to this question were compared between the 3 survey samples.
Table 4.
Reported reasons for insomnia in the three surveys
| Reason for insomnia | Number (%) in people with sleep problems* |
||
|---|---|---|---|
| 1993 (n = 2066) | 2000 (n = 1799) | 2007 (n = 1570) | |
| Worry/thinking | 981 (42.6%) | 777 (43.2%) | 644 (41.0%) |
| Illness/discomfort | 346 (15.0%) | 313 (17.4%) | 299 (19.0%) |
| Noise | 138 (6.0%) | 75 (4.2%) | 54 (3.4%) |
| Shift work/too busy to sleep | 120 (5.2%) | 128 (7.1%) | 72 (4.6%) |
| Needing to go to the toilet | 79 (3.4%) | 58 (3.2%) | 45 (2.9%) |
| Having to do something (e.g., look after baby) | 128 (5.6%) | 90 (5.0%) | 87 (5.5%) |
| Tired | 104 (4.5%) | 66 (3.7%) | 50 (3.2%) |
| Medication | 22 (1.0%) | 25 (1.4%) | 34 (2.2%) |
| Other | 386 (16.8%) | 267 (14.8%) | 285 (18.2%) |
Reporting sleep problems in the last month.
Covariates
We included data on age, gender, education, employment, marital status, and depression. Age was kept as a continuous variable, but was entered in decades rather than years in logistic regression analyses for ease of interpretation of the odds ratios. The highest level of education achieved was recoded into 3 groups: high (“A-level” or higher, implying education until ≥ 18 years of age), medium (“O-level” or “GCSE,” indicating having left school at the UK statutory school leaving age of 16), and low (implying having left school before the age of 16 and/or with no educational qualifications). Employment was coded into 3 groups: currently in employment, currently unemployed, and economically inactive (i.e. retired, in full-time education or a homemaker). Marital status was originally coded into 6 groups; in logistic regression it was simplified into 2 categories: married/cohabiting/single vs. widowed/divorced/separated. An ICD-10 diagnosis of depression was calculated from the CIS-R data using a standard algorithm.
Medication Use
Ascertainment of current medication use varied across the 3 surveys. In the 1993 and 2000 surveys, participants were asked to list current prescribed medications, which were then coded by standard British National Formulary (BNF)11 code. In addition, in 2000 the name of the individual medication was also recorded (but individual medications were not recorded in 1993). In 2007 a different approach was used: participants were shown a card with a list of medications and were asked whether they were receiving any of them. This list included 2 hypnotic medications, nitrazepam and temazepam, and one anxiolytic, diazepam. Due to these differences, there was no comparable information across all 3 surveys. For the purposes of comparing data from 1993 and 2000, use of medication in the hypnotic category of the BNF was examined as a separate binary outcome. To compare data from 2000 and 2007, prevalence of use of either temazepam or nitrazepam was coded as a binary variable, as was prevalence of use of temazepam, nitrazepam, or diazepam.
Statistical Analysis
All analyses were undertaken using Stata version 10. Initial descriptive analyses of the characteristics of each survey sample were carried out using standard weighting procedures specific to the survey in question, in order to account for the stratified clustered sampling and non-response. Initial descriptive analyses were carried out to compare changes in the prevalence of insomnia categories across the 3 surveys with those of other CIS-R symptoms (defined using subscale cut-offs as described above). Next, samples from the 3 surveys were combined, and separate logistic regression analyses were carried out for each of the binary outcomes (4 insomnia definitions). This was not done for hypnotic use, as there was no comparable information across the 3 surveys. The effect of survey period on insomnia prevalence was investigated in fully adjusted models (i.e., all listed covariates were entered into each model). Between-survey differences in the strengths of association between exposures and outcomes were tested by entering interaction terms with survey year; interaction terms were entered separately for each variable. Wald tests were carried out to test the improvement of fit of the model for each main effect or interaction. Residuals were examined to check on model assumption and possible nonlinear effects of age. The logistic regression results presented were not adjusted for the complex survey design. The effect of such adjustment was checked and found not to lead to substantive differences.
RESULTS
Of the 26,091 participants in the combined 3 surveys, 23,553 (90%) were from England; 20,503 (87%) of these were under the age of 65. The remainder of the results relates to this sample. Of these participants, 8,903 were from the 1993 survey, 6,175 from the 2000 survey, and 5,425 from the 2007 survey. Table 1 describes, for each survey, sociodemographic characteristics of the participants and the prevalences of the 5 outcomes of interest. There were no marked differences in average sample age or gender distribution across the 3 surveys. The proportion of unemployed participants was higher in 1993 than in 2000 or 2007. Education levels increased across the surveys. The proportion of participants who were single or cohabitating increased across the 3 surveys, whereas the proportion who were married or widowed decreased, and the proportion divorced or separated showed no steady pattern. The proportion of participants meeting ICD-10 criteria for a diagnosis of depression remained reasonably stable across the 3 surveys, with a slight increase from the 1993 to the 2000 survey.
Table 1.
Characteristics of the samples
| Year of survey sample |
|||
|---|---|---|---|
| 1993 (n = 8903) | 2000 (n = 6175) | 2007 (n = 5425) | |
| Gender Female n (%) | 4,728 (49.5%) | 3,392 (50.0%) | 3,059 (50.4%) |
| Age mean (standard error) | 38.2 (0.16) | 39.2 (0.22) | 39.7 (0.23) |
| Employment status n (%) | |||
| In employment | 5,918 (69.0%) | 4,405 (75.0%) | 3,825 (72.6%) |
| Unemployed | 746 (8.5%) | 210 (3.2%) | 163 (3.5%) |
| Economically inactive | 2,220 (22.5%) | 1,525 (21.8%) | 1,428 (23.8%) |
| Level of education n (%) | |||
| High | 2,930 (34.3%) | 2,360 (41.0%) | 2,484 (49.3%) |
| Medium | 3,177 (37.5%) | 2,012 (35.4%) | 1,631 (32.4%) |
| Low | 2,632 (28.2%) | 1,462 (23.6%) | 1,060 (18.3%) |
| Depressed n (%) | 226 (2.2%) | 197 (2.8%) | 178 (2.6%) |
| Marital status n (%) | |||
| Married | 4,920 (59.5%) | 3,083 (54.1%) | 2,688 (51.4%) |
| Cohabitating | 569 (7.2%) | 615 (11.3%) | 591 (12.6%) |
| Single | 2,051 (24.2%) | 1,424 (24.7%) | 1,310 (27.0%) |
| Widowed | 307 (2.1%) | 181 (1.7%) | 168 (1.6%) |
| Divorced | 761 (5.3%) | 615 (5.8%) | 500 (5.3%) |
| Separated | 251 (1.7%) | 257 (2.6%) | 188 (2.1%) |
| Total reporting taking hypnotic medication n (%) | 54 (0.4%) | 62 (0.8%) | |
| Reported taking hypnotic medication (within those reporting insomnia symptoms) n (%) | 47 (1.1%) | 48 (1.7%) | |
| Reported talking temazepam or nitrazepam n (%) | 20 (0.3%) | 14 (0.2%) | |
| Reported taking temazepam, nitrazepam or diazepam n (%) | 55 (0.7%) | 50 (0.8%) | |
| Insomnia symptoms n (%) | 3,178 (35.0%) | 2,466 (38.0%) | 2.239 (38.6%) |
| Insomnia of at least moderate severity n (%) | 900 (9.3%) | 788 (11.5%) | 799 (13.2%) |
| Insomnia and fatigue n (%) | 1,034 (12.6%) | 909 (13.3%) | 862 (13.9%) |
| Insomnia diagnosis n (%) | 311 (3.1%) | 355 (5.0%) | 365 (5.8%) |
All percentages and means weighted.
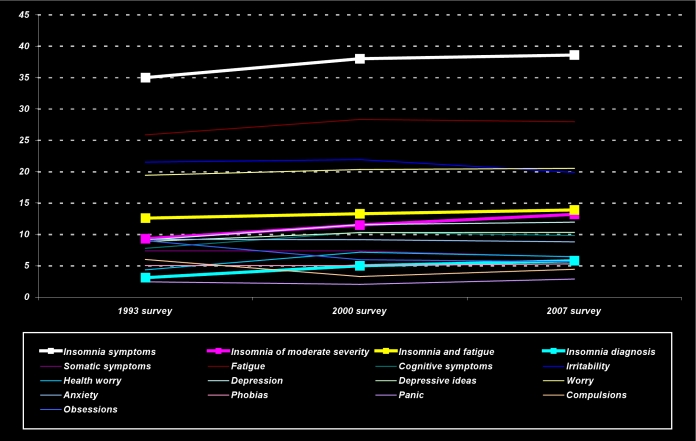
For each of the 4 definitions of insomnia, the prevalence increased from 1993 to 2007. This increase was most noticeable for the most restrictive category of insomnia diagnosis, with the prevalence almost doubling from 1993 to 2007. Unweighted increases in proportions from 1993 to 2007 were 6% (95% CI 4%-7%) for insomnia symptoms, 5% (3%-6%) for insomnia of at least moderate severity, 4% (3%-6%) for insomnia with fatigue, and 3% (2%-4%) for insomnia diagnosis. The prevalences for 2007 were recalculated, this time restricting data to those interviews collected between January and April (the months in which the 1993 and 2000 interviews were carried out); they did not noticeably change for the 4 insomnia definitions (40.3%, 13.6%, 13.5%, and 5.8%, respectively). These changes in prevalence are compared to those of other CIS-R derived mental health symptoms in Figure 1. The median summary scores for the CIS-R scale in the analyzed samples were 8.9 in 1993, 9.7 in 2000, and 9.3 in 2007.
Figure 1.
Prevalence (%) of insomnia categories relative to other mental health concerns (CIS-R subscale scores ≥ 2) in the three surveys.
The proportion of respondents reporting current hypnotic medication use was double in 2000 compared to 1993 (unweighted odds ratio 1.7, 95% CI 1.2-2.4). There was information on 2 hypnotic medications for comparison between the 2000 and 2007 surveys: nitrazepam and temazepam; 32% of those who reported using hypnotic medication in 2000 reported taking one of these 2 medications. The reported prevalence of the use of either nitrazepam or temazepam did not noticeably increase between the 2000 and 2007 surveys. The prevalence of the use of nitrazepam, temazepam, or diazepam was also similar across these 2 surveys. Of those participants reporting insomnia symptoms, 51 (1.1%) reported taking hypnotic medication in 1993 and 95 (1.7%) in 2000.
Table 2 presents associations between the 4 insomnia definitions and sociodemographic factors and survey year; all variables were entered at the same time for each model, so that all coefficients were mutually adjusted for all other variables. All insomnia syndromes were associated with female gender, unemployment and economic inactivity, lower levels of education, depression, and widowed, divorced, or separated marital status. Greater age was associated with 2 of the insomnia syndromes: insomnia symptoms and insomnia diagnosis. Later survey year was significantly associated with each of the 4 definitions of insomnia, reflecting a steady increase in prevalence; this association was strongest for insomnia diagnosis.
Table 2.
Associations between demographic variables and insomnia in the combined three surveys
| Association with four outcomes; mutually adjusted coefficients (odds ratio, 95% confidence intervals) |
||||
|---|---|---|---|---|
| Insomnia symptoms | Moderate insomnia | Insomnia and fatigue | Insomnia diagnosis | |
| Gender | ||||
| Male | ref | ref | ref | ref |
| Female | 1.5 (1.4-1.6) | 1.4 (1.3-1.6) | 1.6 (1.5-1.8) | 1.3 (1.1-1.5) |
| Age (in ten years) | 1.07 (1.05-1.10) | 1.02 (0.99-1.06) | 1.02 (0.98-1.05) | 1.12 (1.06-1.19) |
| Employment status | ||||
| In employment | ref | ref | ref | ref |
| Unemployed | 1.5 (1.3-1.7) | 1.7 (1.5-2.1) | 1.4 (1.1-1.7) | 1.4 (1.0-1.9) |
| Economically inactive | 1.4 (1.3-1.5) | 1.9 (1.7-2.1) | 1.5 (1.4-1.7) | 2.3 (2.0-2.7) |
| Level of education | ||||
| High | ref | ref | ref | ref |
| Medium | 1.0 (0.9-1.1) | 1.1 (1.0-1.2) | 1.0 (0.9-1.2) | 1.2 (1.0-1.4) |
| Low | 1.1 (1.0-1.2) | 1.4 (1.3-1.6) | 1.2 (1.1-1.3) | 1.4 (1.2-1.7) |
| Survey year | ||||
| 1993 | ref | ref | ref | ref |
| 2000 | 1.1 (1.1-1.2) | 1.3 (1.1-1.4) | 1.1 (1.0-1.2) | 1.5 (1.3-1.8) |
| 2007 | 1.2 (1.1-1.3) | 1.6 (1.4-1.8) | 1.2 (1.1-1.3) | 2.0 (1.7-2.3) |
| Depression | ||||
| Not depressed | ref | ref | ref | ref |
| Depressed | 7.2 (5.7-9.0) | 7.7 (6.5-9.2) | 15.7 (12.9-19.2) | 10.9 (8.9-13.3) |
| Marital status | ||||
| Married/cohabiting/single | ref | ref | ref | ref |
| Widowed/divorced/separated | 1.3 (1.2-1.4) | 1.6 (1.4-1.8) | 1.4 (1.3-1.6) | 1.7 (1.4-2.0) |
Table 3 shows the results from a series of separate analyses in each of which one interaction was added to the model shown in Table 2. Interaction terms were fitted to investigate the extent to which demographic associations were modified by survey year. In summary, although some individual terms were statistically significant, there were no consistent interactions across the different outcomes. Wald tests were carried out to test improvement of fit for each interaction, and for the most part were not significant, except in the case of insomnia symptoms, the most prevalent outcome (see Table 3).
Table 3.
Interactions between survey year and demographic variables
| Insomnia symptoms | Moderate insomnia | Insomnia and fatigue | Insomnia diagnosis | |
|---|---|---|---|---|
| Survey and age interaction | ||||
| 1993*age (10 years) | ref | ref | ref | ref |
| 2000*age (10 years) | 1.00 (0.95-1.06) | 0.92 (0.85-1.00) | 1.00 (0.92-1.08) | 0.92 (0.81-1.05) |
| 2007*age (10 years) | 1.02 (0.97-1.08) | 0.94 (0.87-1.02) | 1.00 (0.92-1.07) | 0.90 (0.79-1.02) |
| Wald test | χ2 = 0.63, P = 0.73 | χ2 = 4.54, P = 0.10 | χ2 = 0.04, P = 0.98 | χ2 = 3.06, P = 0.22 |
| Survey and gender interaction | ||||
| 1993*gender | ref | ref | ref | ref |
| 2000*gender | 1.13 (0.98-1.30) | 0.88 (0.70-1.10) | 0.97 (0.78-1.21) | 0.82 (0.58-1.17) |
| 2007*gender | 1.35 (1.16-1.57) | 1.06 (0.84-1.33) | 1.06 (0.85-1.32) | 0.86 (0.60-1.21) |
| Wald test | χ2 = 15.77, P < 0.001 | χ2 = 2.46, P = 0.29 | χ2 = 0.54, P = 0.76 | χ2 = 1.31, P = 0.52 |
| Survey and employment interaction | ||||
| 1993 or employed | ref | ref | ref | ref |
| 2000*unemployed | 0.87 (0.62-1.22) | 1.16 (0.74-1.83) | 0.97 (0.60-1.59) | 0.88 (0.39-1.98) |
| 2007*unemployed | 1.10 (0.93-1.30) | 0.91 (0.72-1.14) | 1.21 (0.97-1.52) | 1.09 (0.77-1.53) |
| 2000*econ. inactive | 1.03 (0.70-1.50) | 0.89 (0.53-1.48) | 1.53 (0.93-2.50) | 1.44 (0.67-3.07) |
| 2007*econ. Inactive | 1.26 (1.07-1.50) | 0.89 (0.71-1.11) | 1.20 (0.96-1.51) | 1.16 (0.83-1.64) |
| Wald test | χ2 = 8.61, P = 0.07 | χ2 = 2.18, P = 0.70 | χ2 = 6.33, P = 0.18 | χ2 = 1.78, P = 0.78 |
| Survey and education interaction | ||||
| 1993 or high | ref | ref | ref | ref |
| 2000*medium | 1.02 (0.87-1.21) | 1.02 (0.77-1.34) | 1.03 (0.80-1.33) | 1.08 (0.69-1.67) |
| 2007*medium | 1.21 (1.02-1.45) | 0.96 (0.73-1.25) | 1.15 (0.89-1.48) | 1.17 (0.77-1.78) |
| 2000*low | 1.20 (1.01-1.42) | 1.24 (0.95-1.62) | 1.33 (1.03-1.71) | 1.14 (0.75-1.74) |
| 2007*low | 1.26 (1.05-1.52) | 0.75 (0.57-0.99) | 1.24 (0.95-1.62) | 1.02 (0.68-1.55) |
| Wald test | χ2 = 10.88, P < 0.01 | χ2 = 14.29, P < 0.01 | χ2 = 6.75, P = 0.15 | χ2 = 1.28, P = 0.87 |
| Survey and depression interaction | ||||
| 1993/depression | ref | ref | ref | ref |
| 2000*depression | 1.1 (0.7-1.9) | 1.0 (0.7-1.5) | 1.6 (1.0-2.5) | 1.1 (0.7-1.8) |
| 2007*depression | 1.2 (0.7-2.0) | 1.3 (0.8-2.0) | 1.4 (0.8-2.2) | 1.2 (0.8-2.0) |
| Wald test | χ2 = 0.32, P = 0.85 | χ2 = 1.64, P = 0.43 | χ2 = 3.75, P = 0.15 | χ2 = 0.67, P = 0.71 |
| Survey and marital status interaction | ||||
| 1993/marital status | ref | ref | ref | ref |
| 2000*marital status | 1.1 (0.9-1.4) | 1.0 (0.8-1.3) | 1.2 (0.9-1.5) | 0.9 (0.6-1.3) |
| 2007*marital status | 0.9 (0.7-1.1) | 0.8 (0.6-1.0) | 1.0 (0.8-1.3) | 0.9 (0.6-1.3) |
| Wald test | χ2 = 5.15, P = 0.08 | χ2 = 3.12, P = 0.21 | χ2 = 2.10, P = 0.35 | χ2 = 0.38, P = 0.82 |
Table 4 displays the proportion of participants with any sleep problems (under or over sleeping) in the past month who cited each of the potential reasons, by survey year. The main reason given was worry, and the proportion of respondents reporting this did not vary noticeably across surveys. However, the proportion reporting illness or discomfort as the main reason increased across the 3 surveys, as did the proportion reporting medication as the main reason for their sleep problems. On the other hand, the proportion reporting noise as the main reason decreased. The remaining reasons remained relatively stable. The overall distribution of reasons varied significantly across the 3 surveys: χ2 (n = 5673,df = 16) = 57.12, P < 0.001.
DISCUSSION
Insomnia prevalence was found to have increased across three national surveys carried out with similar methodology over a 15-year period. This increase was observed for each of four definitions applied for insomnia, although it was strongest for the most restrictive definition of insomnia diagnosis. These results are comparable to a 2008 analysis of Finnish surveys 4 which found some evidence for an increase in the prevalence of chronic and occasional insomnia-related symptoms over the previous ten years in working-age populations. In line with previous research, insomnia was found to be associated with female gender, increased age, lower educational attainment, not being in employment, depression, and widowed, divorced, or separated status. These associations were consistent across the three surveys, and most self-reported reasons for insomnia symptoms also had not changed substantially.
The main strength of this analysis is that it was based on three surveys that were near-identical in design, both in terms of sampling procedure and questions asked, each recruiting large nationally representative samples. This provided a rare opportunity to investigate changing trends in both the prevalence of insomnia, and in its associations with key demographic factors. Four different definitions of insomnia were used, and the prevalences reported here are consistent with previous research2,4,12 and the reference ranges summarized in Ohayon's overview7 of epidemiological research in this field.
One limitation is that these three surveys span 15 years, which could be argued to be a relatively short period over which to expect substantial demographic trends. The observed changes in prevalence are therefore more remarkable and likely to have meaningful population-level impact, in addition to clinical relevance (in terms of the absolute numbers of people fulfilling diagnostic criteria for the syndrome). In considering changes across the surveys, differences between the samples and measurements should be considered. As described above, a major advantage was the consistency in both sampling and insomnia ascertainment and definition. An important potential limitation, however, is that participation rates decreased over the three surveys (in line with the decline in participation in epidemiological research in general over the last 30 years13), which raises the possibility of selection bias. The weighting procedures applied for initial within-survey analyses took non-response into account, although could only apply weights based on area level socioeconomic properties. The observed increase in prevalence would be exaggerated if people with insomnia became proportionately more likely to agree to participate over time. However, most research tends to indicate lower participation rates in people with psychological symptoms or disorders13 and we feel the underlying differences are more likely to have been obscured than exaggerated through non-participation, although we clearly cannot infer this conclusively. The surveys were carried out to measure general mental health in the community and insomnia was not highlighted in recruitment materials. Furthermore, as discussed below, associations between insomnia syndromes and demographic factors remained very stable across examinations, which reduces the likelihood of substantial bias. Finally, trajectories (displayed in Figure 1) and the median CIS-R scores for the three surveys did not suggest a consistent trend for increases in symptom prevalence, so that bias, if present, would have to be specifically influencing insomnia outcomes, which again seems unlikely.
The definition of insomnia diagnosis used in this analysis was slightly tighter than the DSM-IV definition, as the CIS-R asks whether insomnia symptoms have lasted at least 6 months, compared to the DSM-IV criterion of at least 3 months. However, we feel that this is unlikely to have had a substantial effect on prevalence estimates, given the known chronicity of the syndrome.14 No data were available on subjective sleep quality or of sleep duration, and the information on sleep problems was based on self-report. No information was gathered on how long participants had been experiencing these problems, so incidence could not be examined. Furthermore, as the surveys were cross-sectional, directions of cause and effect cannot be concluded (for example between insomnia and economic activity). Analyses were limited to a small number of demographic factors, but ones that have repeatedly been shown to be associated with insomnia in other studies.7,12,15 Apart from depression, common mental disorders such as anxiety were not controlled for in these analyses, and it is possible that the increased insomnia prevalence may be linked to an increase in the prevalence of these disorders. However, no consistent changes were noted in other CIS-R symptoms, as displayed in Figure 1. Furthermore, across the three surveys, the proportion of working-age participants meeting criteria for at least one common mental disorder has remained reasonably stable, with a slight increase between the first two surveys (15.5% in 1993, 17.5% in 2000, and 17.6% in 2007).8
As well as insomnia syndromes, we had planned to investigate changes in hypnotic use. However, directly comparable data were not available for the three surveys. The prevalence of hypnotic use doubled between 1993 and 2000 (in line with previous analysis); the prevalence of the use of those hypnotic medications we had information on (nitrazepam and temazepam) did not show an increase between 2000 and 2007. The proportion of participants reporting insomnia who were currently taking hypnotic medication in 1993 and 2000 was extremely low. Although it is possible that the increase from 1993 to 2000 reflects random fluctuation identified as significant because of the large sample sizes, one possible explanation for the increased use is the introduction in prescribing of “z” non-benzodiazepine hypnotics (zaleplon, zolpidem, zopiclone, and eszopiclone). It is possible that this prevalence may have declined in 2007, as these medications were since claimed to not be safe and effective as initially hoped.6 Unfortunately, as a breakdown of drug names was not available in all surveys, we were unable to address this question directly. The Finnish analysis mentioned above4 found no evidence of increased prevalence in use of sleeping medication over time despite national data pointing to increased consumption (National Agency for Medicines and Social Insurance Institution, 2006). The authors pointed to two possible explanations: either the questions asked in the different surveys analyzed were subtly different, or consumption may have increased per consumer but not in prevalence.
Although there were some differences across surveys in the relationship of employment and education with one of the insomnia definitions (insomnia symptoms), as implied by significant interaction terms, the associations between insomnia and the demographic factors studied were generally stable across the surveys. As discussed above, this is reassuring in the light of concern about selection bias, and suggests that the prevalence changes are more likely to be genuine. The reasons reported for sleep problems were broadly similar across surveys, with worry and discomfort being the most commonly cited. Reasons for secular changes in insomnia prevalence require further research. Given the age range focused on in this analysis, one possibility lies in changes in working conditions and patterns. Current definitions of insomnia assume that the person has adequate opportunity for sleep. However, moves towards shift work and multiple occupations may compromise this. Although there were no consistent changes in work-related attributions of sleep disturbance across the three surveys (Table 4), further investigation of this issue is indicated.
Given the signs of the gradually increasing prevalence of insomnia, further research is needed to examine the effects of this increase on the health, well-being, and functioning of modern society; to develop effective interventions; and to enhance their availability to those affected: for example, a recent UK study found that 63% of participants with baseline insomnia and psychological distress had not made relevant health care use (defined as a GP consultation for anxiety, depression, or insomnia or prescription for antidepressant, hypnotic, or anxiolytic medication) after one year.16 The increasing prevalence of insomnia, however defined, suggests that service delivery needs to be considered at multiple levels—in primary care for milder forms with higher prevalence, and in secondary care for the lower prevalence but more severe syndromes. A key element in this will be to establish more precisely the impact of insomnia to provide clearer modeling of cost-effectiveness, and for quantification of this impact to encompass societal outcomes as well as the more traditionally included health effects. In a recent review of the societal costs of insomnia, Leger points out the need to include not only direct, indirect, and related economic costs of insomnia, but also to consider the impact of insomnia of quality of life17; however, very few studies have specifically addressed this.
DISCLOSURE STATEMENT
This was not an industry supported study. Drs. Stewart and Dewey have received research support from Pfizer, Johnson & Johnson and Lundbeck Pharmaceuticals. Dr. Stewart also received financial assistance for travel from Pfizer. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
Work for this study was performed at King's College London (Institute of Psychiatry), London, United Kingdom. The National Psychiatric Morbidity Surveys were supported by the Department of Health, the Scottish Health Executive (formerly the Scottish Office), the Welsh Assembly Government (formerly the Welsh Office), and the NHS Information Centre for health and social care. Dr. Stewart is funded by the NIHR Specialist Biomedical Research Centre for Mental Health at the South London and Maudsley NHS Foundation Trust and Institute of Psychiatry, King's College London. Drs. Calem, Bisla, and Begum are funded by the Guys and St Thomas Trustees and the South London and Maudsley NHS Foundation Trust Special Trustees.
Footnotes
A commentary on this article appears in this issue on page 313.
REFERENCES
- 1.Morin C. The nature of insomnia and the need to refine our diagnostic criteria. Psychosom Med. 2000;62:483–5. doi: 10.1097/00006842-200007000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Morphy H, Dunn KM, Lewis M, et al. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30:274–80. [PubMed] [Google Scholar]
- 3.Morin CM, Belanger L, LeBlanc M, et al. The natural history of insomnia: a population-based 3-Year longitudinal study. Arch Intern Med. 2009;169:447–53. doi: 10.1001/archinternmed.2008.610. [DOI] [PubMed] [Google Scholar]
- 4.Kronholm E, Partonen T, Laatikainen T, et al. Trends in self-reported sleep duration and insomnia-related symptoms in Finland from 1972 to 2005. J Sleep Res. 2008;17:54–62. doi: 10.1111/j.1365-2869.2008.00627.x. [DOI] [PubMed] [Google Scholar]
- 5.Brugha TS, Bebbington PE, Singleton N, et al. Trends in service use and treatment for mental disorders in adults throughout Great Britain. Brit J Psychiatry. 2004;185:378–84. doi: 10.1192/bjp.185.5.378. [DOI] [PubMed] [Google Scholar]
- 6.Holbrook AM. Treating insomnia: use of drugs is rising despite evidence of harm and little meaningful benefit. BMJ. 2004;329:1198–9. doi: 10.1136/bmj.329.7476.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 8.Jenkins R, Meltzer H, Bebbington P, et al. The British Mental Health Survey Programme: achievements and latest findings. Soc Psychiatry Psychiatr Epidemiol. 2009;44:899–904. doi: 10.1007/s00127-009-0112-7. [DOI] [PubMed] [Google Scholar]
- 9.Lewis G, Pelosi A, Araya RC, Dunn G. Measuring psychiatric disorder in the community: a standardised assessment for use by lay interviewers. Psychol Med. 1992;22:465–86. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- 10.Stewart R, Besset A, Bebbington P, et al. Insomnia comorbidity and impact and hypnotic use by age group in a national survey population aged 16 to 74 years. Sleep. 2006;29:1391–7. doi: 10.1093/sleep/29.11.1391. [DOI] [PubMed] [Google Scholar]
- 11.Royal Pharmaceutical Company of Great Britain. London: British Medical Association,; 2004. British National Formulary. [Google Scholar]
- 12.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med. 2007;3:S7–S10. [PMC free article] [PubMed] [Google Scholar]
- 13.Galea S, Tracy M. Participation rates in epidemiological studies. Ann Epidemiol. 2007;17:643–53. doi: 10.1016/j.annepidem.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 14.Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 2000;23:243–308. [PubMed] [Google Scholar]
- 15.Bixler E. Sleep and society: an epidemiological perspective. Sleep Med. 2009;10:S3–6. doi: 10.1016/j.sleep.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Hayward R, Jordan KP, Croft P. Healthcare use in adults with insomnia: a longitudinal study. Brit J Gen Pract. 2010;60:334–40. doi: 10.3399/bjgp10X501822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leger D, Bayon V. Societal costs of insomnia. Sleep Med Rev. 2010;14:379–89. doi: 10.1016/j.smrv.2010.01.003. [DOI] [PubMed] [Google Scholar]