Abstract
Drug-related law enforcement activities may undermine the protective effects of syringe exchange programs (SEPs) on local injectors’ risk of injection-related infections. We explored the spatial overlap of drug-related arrest rates and access to SEPs over time (1995-2006) in New York City health districts, and used multilevel models to investigate the relationship of these two district-level exposures to the odds of injecting with an unsterile syringe. Districts with better SEP access had higher arrest rates, and arrest rates undermined SEPs’ protective relationship with unsterile injecting. Drug-related enforcement strategies targeting drug users should be de-emphasized in areas surrounding SEPs.
Keywords: syringe exchange programs, harm reduction, injection drug use, HIV, drug-related law enforcement, geospatial analyses
The presence of syringe exchange programs (SEPs) in US communities has gradually increased since the early 1990s. Between 1994 and 2009, surveys indicate that the number of SEPs operating in US communities almost tripled, while the volume of syringes these programs distributed rose 414%, from 8 million to 33.1 million.(Des Jarlais et al., 2010) SEPs’ legal status has also advanced: to permit SEPs to operate legally, many US states and cities have modified laws that require a prescription to acquire or possess a syringe.(Burris et al., 2010) In 2010, the 21-year ban on spending federal funds to support SEPs was repealed.(US Congress, 2009) The US “war on drugs”, however, persists: between 1982 and 2007 arrests for drug possession almost tripled, from 538,100 to 1,519,000.(US Federal Bureau of Investigation, 2010) A large body of research indicates that drug-related law enforcement activities that target drug users increase vulnerability to HIV and other harms among drug injectors.(Bluthenthal et al., 1999b; Cooper et al., 2005a; Kerr et al., 2005; Maher and Dixon, 1999; Miller et al., 2008) Given that they share a target population (i.e., injectors of illicit drugs), SEPs and drug-related enforcement activities may often operate in the same localities. While many researchers and practitioners have noted this possibility,(e.g., Bluthenthal et al., 1997; Davis et al., 2005; Wood et al., 2003) the spatial overlap of SEPs and drug-related enforcement efforts in injectors’ microenvironments has rarely been quantified, and the effects of this overlap on local injectors’ HIV risk behaviors have received little empirical attention.
The present multilevel longitudinal analyses thus seek to (1) document the spatial overlap of SEPs and drug-related enforcement activities in small geographic areas in one US city (New York City) over time (1995-2006); (2) investigate whether exposure to this overlap varies across racial/ethnic groups of injectors; and (3) examine the combined effects of spatial access to SEPs and exposure to drug-related enforcement activities on injectors’ risk of HIV and other injection-related infections over time. The following sections discuss the theoretical framework guiding these analyses, our conceptualizations of SEPs and drug-related enforcement activities, and the rationale for considering the interplay of these two interventions, both overall and across racial/ethnic groups.
Conceptual Framework: The Risk Environment
This analysis is guided by the Risk Environment Model, a framework designed to structure conceptualizations of the determinants of HIV among drug users. The “risk environment” is defined as “the space...in which a variety of factors exogenous to the individual interact to increase the chances of HIV transmission”.(Rhodes et al., 2005, p. 1027) Conversely, features of “protective” environments reduce vulnerability to HIV transmission. This model proposes that four main types of influences – physical, social, economic, and policy – operate at micro and macro levels to shape vulnerability to HIV among users.(Rhodes, 2002; Rhodes et al., 2005) This model has been widely used in research on the determinants of HIV and other injection-related infections among drug users.(e.g.,Maas et al., 2007; Ramos et al., 2009; Strathdee et al., 2008)
Two constructs are particularly salient to our analyses: the “interplay” of features of the risk environment and “racialized risk environments”. The former is indigenous to the original formulation of the Risk Environment Model; we have previously discussed the latter as a possible extension of this model.(Cooper et al., 2009) The Risk Environment Model posits that features of the risk environment interact with one another, both within and across levels of influence, and that this interplay shapes the geographic distribution of HIV and other injection-related harms among injectors.(Rhodes, 2002; Rhodes et al., 2005) The influence of one feature on HIV risk, for example, may depend on the presence of a second feature. The concept of “racialized risk environments” has its roots, in part, in Critical Race Theory.(Bonilla-Silva, 2001) According to this theory, racialized social systems are “societies that allocate differential economic, political, social, and even psychological rewards to groups along racial lines”.(Bonilla-Silva, 2001, p. 44) We have previously proposed that risk environments are racialized when the presence of a particular protective or harmful feature varies across geographic areas according to the racial/ethnic composition of the underlying local population, or of the underlying local injecting population.(Cooper et al., 2009) As discussed below, these two constructs guided the development of our research questions.
Conceptualizing SEPs and Drug-Related Law Enforcement Activities as Placed-Based Structural Interventions
Drug-user-focused enforcement strategies and SEPs are among the most well-documented features of the risk and protective environments, respectively. Multiple studies have found that drug-related enforcement strategies that target drug users and street level dealers increase rates of receptive syringe sharing (RSS) and a range of other risk behaviors among injectors. (Bluthenthal et al., 1999a; Cooper et al., 2005a; Kerr et al., 2005; Maher and Dixon, 1999; Miller et al., 2008; Pollini et al., 2007; Rhodes et al., 2003) Ecologic research has found that HIV prevalence is greater among injectors living in geographic areas with higher drug-related arrest rates.(Friedman et al., 2006) In contrast, a large body of research has found that consistent SEP participation substantially reduces RSS and HIV incidence. (Des Jarlais et al., 1996a; Des Jarlais et al., 1996b; Gibson et al., 2002; Gibson et al., 2001; Ksobiech, 2003; World Health Organization, 2004) In the Risk Environment Model, drug user-focused enforcement strategies have been conceptualized as a micro-level social influence, and, in areas where SEPs are legal, spatial access to these programs has been conceptualized as a micro-level policy influence.(Rhodes, 2009)
Both SEPs and drug-user-focused enforcement strategies can be conceptualized as structural interventions that exert their strongest effects locally. Structural interventions are interventions that alter the “context within which health is produced and reproduced” (Blankenship et al., 2006, p. 59). While SEPs’ effects may be greatest for individuals who personally attend these programs, they extend beyond program participants to shape the contexts in which people use drugs.(Bastos and Strathdee, 2000; Des Jarlais, 2000; Sumartojo, 2000) SEPs increase the flow of sterile syringes into geographic areas, and remove used syringes from circulation.(Kaplan and Heimer, 1994) SEPs reach non-participants in at least two ways: through secondary syringe exchange, in which SEP participants transfer sterile syringes to their network members, and through satellite syringe exchange, in which SEP participants travel to an underserved area to distribute or sell syringes to individuals who are outside their network.(Valente et al., 1998) Moreover, by reducing HIV incidence, and thus (over time) HIV prevalence among local injectors, SEPs also reduce the likelihood that a single instance of RSS will result in HIV transmission.(Bastos and Strathdee, 2000; Des Jarlais, 2000; Sumartojo, 2000) As with many healthcare services, proximity to SEPs shapes utilization patterns: individuals who live near SEPs are more likely to attend them, and less likely to engage in RSS.(Cooper et al., 2011; Rockwell et al., 1999; Williams and Metzger, 2010) Given that injectors may be more likely to form relationships with injectors living near them,(Friedman et al., 1999b) non-participants who live near SEPs may also be likely to reap the benefits of secondary syringe exchange.
Likewise, police departments design and implement drug-user-focused enforcement activities as place-based structural interventions. Social geographers have conceptualized policing (regardless of the target offense) as inherently concerned with controlling public space.(Fyfe, 1992; Herbert, 1996, 1997) Consonant with this conceptualization, drug-user-focused interventions are often place-based: their scope is usually geographically bounded (e.g., limited to a particular precinct or cluster of adjacent precincts), and officers may be assigned to monitor specific terrain within these boundaries.(Cooper et al., 2004; Zimmer, 1990) These strategies also seek to alter the contexts in which drug-related activity occurs. For example, deterrence is a cornerstone of drug-related enforcement, and rests on the assumption that punishing one individual or group for violating drug-related laws will discourage others from violating these laws in the future.(Sherman, 1990) Likewise, drug-user-focused enforcement activities’ effects on HIV risk extend beyond individuals who are arrested. Injectors living, using drugs, or buying drugs in heavily-policed areas often implement a range of strategies to minimize their risk of arrest. Some of these strategies – including not carrying sterile syringes and injecting rapidly – increase their risk of injection-related harms. (Bluthenthal et al., 1999a; Cooper et al., 2005a; Kerr et al., 2005; Maher and Dixon, 1999; Miller et al., 2008; Pollini et al., 2007; Rhodes et al., 2003
The Interplay of Drug-Related Enforcement Activities and SEPs
The concept of “interplay” in the Risk Environment model might be particularly salient when considering SEPs and drug-related enforcement activities targeting drug users: as noted by several researchers and practitioners, (e.g., Bluthenthal et al., 1997; Davis et al., 2005; Wood et al., 2003) these two structural interventions may often operate in the same microenvironments. To facilitate the identification of users and street-level dealers and to deter drug-related activity, police departments locate user-focused enforcement strategies in places where people buy and use drugs.(Cooper et al., 2005a; Fyfe, 1992; Moore, 1990) Likewise, SEPs are most effective at preventing HIV epidemics, and at reversing the course of existing epidemics, when they are located in or near such places.(UNAIDS, 2006; WHO, 2007) The extent of the spatial overlap of SEPs and drug-user-focused enforcement activities, however, has rarely been quantified. A recent Vancouver-based study is an exception: Shannon and colleagues concluded that the street corners and blocks where sex-working women accessed SEPs and other health services were substantially more likely to be located within the heavily policed and violent “core” of Vancouver's Downtown East Side than in its periphery.(Shannon et al., 2008)
Most research on the effects of SEPs and drug-related enforcement activities on HIV risk behavior among injectors has studied one intervention in isolation from the other. The few studies that have explored the co-location of these interventions have primarily focused on the ways that enforcement strategies affect SEP operations and utilization. These studies have uniformly found that SEP visits decline during police drug crackdowns. (Aitken et al., 2002; Bluthenthal et al., 1997; Davis et al., 2005; Rhodes et al., 2003; Small et al., 2006; Wood et al., 2003) Legal SEPs may not buffer the effects of such interventions in some circumstances: a California-based study found that participants of legal SEPs were more likely to be arrested on paraphernalia charges than participants of illegal SEPs.(Martinez et al., 2007) Notably, while some have found that the number of syringes distributed by SEPs also declines during crackdowns,(Davis et al., 2005; Hammett et al., 2005; Wood et al., 2003) others have found that this number remains constant or even increases.(Aitken et al., 2002; Wood et al., 2004) Research on enforcement and SEP utilization has thus not yet determined whether impaired SEP operations affect a key outcome: local injectors’ ability to inject with sterile syringes.
Additionally, the effects of the spatial overlap between SEPs and drug-related enforcement activities may extend beyond impaired SEP operations and possible reductions in syringe flow from SEPs. For example, to avert detection as a drug user during a police stop and search, injectors may hesitate to carry syringes when they travel to their injection site;(Cooper et al., 2005a; Grund et al., 1995) in heavily-policed contexts, even individuals who have acquired syringes through SEPs may thus not have a syringe with them when they inject.
Racialized Risk Environments
The geographic distributions of both user-focused drug enforcement activities and SEPs may be racialized. In the USA, user-focused drug enforcement activities are likely to be located in microenvironments that are predominately Black or Latino and impoverished.(Beckett et al., 2006; Cooper et al., 2005b; Tonry, 1994) Likewise, given the high prevalence of HIV among these racial/ethnic groups of injectors,(Des Jarlais et al., 2009; Friedman et al., 1999a) SEPs may try to locate sites in places that Black and Latino injectors can access easily. Black and Latino injectors may thus be particularly likely to contend with the interplay of SEPs and drug-user-focused enforcement activities. Potentially testifying to the racialization of this spatial overlap, SEPs serving higher proportions of injectors of color are more likely to report frequent client arrest.(Beletsky et al., 2011)
Research Questions
New York City (NYC) was selected as the site for the present study in part because it has experienced considerable variations in SEP presence and user-focused drug-related enforcement. In 1992, New York State began permitting select SEPs to operate legally, and spatial access to SEP sites increased thereafter.(Cooper et al., 2011; The New York State AIDS Advisory Council, 2005) The NYC mayor implemented an increasingly intensive “zero tolerance” policy on illicit drugs between 1995-2001,(Cooper et al., 2005b; Greene, 1999) a policy that the subsequent mayor de-emphasized.
The present longitudinal multilevel analyses investigate the possibility of the interplay and racialization of two features of the risk and protective environment, namely user-focused drug enforcement activities and SEP access, and explore their combined impact on local injectors’ risk of HIV and other injection-related infections. Specifically, we:
document variations in the spatial overlap of drug-related enforcement activities and SEP access in NYC health districts over time (1995-2006);
investigate whether exposure to this overlap varies across racial/ethnic groups of injectors; and
examine the combined effects of drug-related enforcement activities and SEP access on injectors’ risk behaviors over time.
Methods
Overview and Units of Analysis
The geospatial units of analysis in this study were NYC's 42 health districts. Each health district contains 3-9 adjacent ZIP code areas with similar sociodemographic characteristics.(United Hospital Fund, 2005) The median district population size in 1995 was 179,189 (range: 28,739 to 428,867). Administrative data were used to operationalize district-level constructs (e.g., spatial access to SEPs) for each year of the study period.
While Research Question 1 pertains only to district-level constructs, Research Questions 2 and 3 pertain to district-level and individual-level constructs. To explore these two questions, we combined district-level data with individual-level data drawn from the “Risk Factors for AIDS among Intravenous Drug Users” study (DA003574, Principal Investigator: Des Jarlais). As discussed in detail elsewhere,(Des Jarlais et al., 2007) the Risk Factors study is a series of cross-sectional surveys of injectors and non-injection drug users entering a large detoxification program in NYC. Approximately 96% of the people approached annually participate.(Des Jarlais et al., 2004) Risk Factors participants were included in the present sample if they were surveyed between 1995-2006, had injected in the prior 6 months, and reported a NYC ZIP code; homeless people were assigned the ZIP code where they slept most. 4,067 people met these criteria. We combined annual cross-sectional Risk Factors data for 1995-2006, thereby creating a three-level database in which each Risk Factors participant was nested within time, and time was nested in districts.
Variables
District-Level Constructs
Spatial access to SEPs
Our measure of SEP access captured the percent of each district's surface area within one mile of an SEP site. This measure has been described in detail elsewhere,(Cooper et al., 2011) and so we review it briefly here. For each year of the study period, we created a digital point map of SEP sites by geocoding the addresses of all legal SEPs operating in NYC and within one mile of NYC's borders; all SEP modalities were included (e.g., van stops, walkabout stops, storefronts). Eighty legal sites operated in this area between 1995-2006; all sites were geocoded to their street address or nearest intersection. Next, we overlaid a street network map onto each year's SEP site map, and created a walking distance buffer around each site that extended one mile from the site along local streets (excluding major highways). A one-mile buffer was selected because past research indicates that injectors will travel ≤1 mile to reach an SEP, (Hutchinson et al., 2000); additionally past research suggests that injectors in districts with a higher proportion of their surface area with one mile of an SEP are less likely to inject with unsterile syringes.(Cooper et al., 2011) Finally, for each year of the study period we calculated the percentage of each district's surface area that was covered by at least one SEP's buffer.
Drug-related arrest rates
Arrest rates per 1000 adult residents were calculated by dividing the number of drug-related arrests occurring in each district and year by the number of adults living in that district that year; the result was multiplied by 1000. Data on drug-related arrests were obtained from the NYS Division of Criminal Justice Statistics, and included all arrests in which at least one charge concerned the possession of illegal drugs for personal use or drug paraphernalia. Arrests were reported for police precincts, and not health districts. We allocated arrests from precincts to districts according to the percent of each precinct's surface areas that lay within each district. Data on adult population size (aged 15-64) were drawn from the US decennial 1990 and 2000 censuses. Data were reported for census tracts rather than districts. We allocated tract-level population counts for 1990 and 2000 to health districts using the methods described for arrests. Annual district-level population counts were calculated for 1995-1999 and 2001-2006 assuming linear change over time.
Spatial access to pharmacies selling syringes over the counter (OTC)
In 2001, New York State (NYS) initiated a demonstration project that allowed pharmacies to sell ≤10 syringes without a prescription, provided that they registered with the NYS Department of Health.(New York State Department of Health AIDS Institute, 2008) Registration in ESAP was voluntary for pharmacies. (New York State Department of Health AIDS Institute, 2008) Past research suggests that injectors who live in districts with better spatial access to OTC pharmacies are less likely to inject with unsterile syringes.(Cooper et al., 2011) To measure spatial access to OTC pharmacies, we followed the same steps that were applied to calculate SEP access. For each year between 2001-2006, we obtained the census of registered pharmacies (N=1316 over the study period) from the NYS Department of Health, and used these data to create annual measures of OTC access; 97% of the pharmacies were geocoded to their nearest street address or intersection.”
Local poverty rates may confound the relationship of our focal features of the risk environment to our outcomes. We assessed whether each district would qualify as a federal poverty area using decennial census data. This dichotomous variable captured whether or not >20% of households were at or below the federal poverty line.(U.S. Census Bureau, 1995)
Temporal Constructs
Time was operationalized in two ways. Study year was expressed as a continuous variable that ranged from 0 in 1995 to 11 in 2006. “OTC Time” was a continuous variable that captured the number of years that had elapsed since 2001.
Individual-Level Constructs
Individual-Level Covariates
To explore Research Question 2, which concerns racialized risk environments, we drew individual-level data on injector race/ethnicity from the Risk Factors database. For Research Question 3, which concerns the relationships of SEP access and drug-related arrest rates to unsterile injecting and distributive syringe sharing (DSS), we used Risk Factors data to measure potential confounders and effect modifiers. We identified potential individual-level confounders in two ways: (a) a literature review that identified factors that were associated with the exposure and the outcome, but unlikely to be mediators, and (b) analyses of temporal changes in the Risk Factors cohort; we sought to control for compositional changes that might be associated with the outcome. Possible confounders included injection frequency, years since first injection, sexual orientation, and age. Race/ethnicity, gender, self-reported HIV serostatus, and homelessness were treated as possible effect modifiers. All covariates were binary except years since first injection, which was continuous.
Individual-Level Outcomes
To explore Research Question 3, we used Risk Factors data to assess individual-level outcomes. We operationalized “injecting with an unsterile syringe” (a construct that includes both RSS and personal re-use of a syringe) as an ordinal outcome with three levels: injecting with a sterile syringe in ≤25% of injection events during the past six months; in 26%-74% of injection events; and in ≥75% of injection events. This measure reflects public health guidelines to use a new sterile syringe for each injection.(Centers for Disease Control and Prevention et al., 1997) RSS has well-established links to HIV and HCV transmission(Normand et al., 1995; Villano et al., 1997); personal syringe re-use may increase the risk of endocarditis, abscesses, and cellulitis.(Murphy et al., 2001; Vlahov et al., 1992) The outcome variable thus captures the extent to which injectors are able to follow public health guidelines designed to prevent these and other infections. DSS was a binary variable that captured whether the participant had given or lent someone a used syringe during the past six months.
Analyses
We used exploratory data analysis and hierarchical linear models (HLM) to investigate Research Question 1, which concerns the spatial overlap of district-level drug-related arrest rates and SEP access. We first charted temporal trajectories of drug-related arrest rates by three categories of SEP access (i.e., some SEP access during each year of the study period; no SEP access at baseline, but some access during at least one year of the study period; and no SEP access during any year of the study period). We then used two-level HLM methods in which study year was nested in districts to model the relationship of SEP access to drug-related arrest rates.
To explore Research Question 2, which pertains to racialized risk environments, we first identified districts in the highest quartile of drug-related arrest rates, of SEP access, and of both these exposures for each year of the study period. We then conducted chi-square tests for each year of the study period that compared the odds that Black and Latino injectors vs. White injectors lived in districts that had elevated drug-related arrest rates, high SEP access, and the combination of high arrest rates and high SEP access.
To investigate Research Question 3, which concerns the relationship of SEP access and arrest rates to injecting with an unsterile syringe and DSS, we first explored temporal trends in the cumulative log odds of injecting with an unsterile syringe (and the log odds of DSS) using growth curve models that controlled for compositional changes in the Risk Factors sample over time. We then applied three-level hierarchical generalized linear models (HGLM) to investigate the relationships of district-level drug-related arrest rates and SEP access to each individual-level outcome.(Raudenbush and Bryk, 2002) We investigated random effects, lagged and non-linear relationships between these two exposures and each outcome, and intra-level and cross-level interactions. Because Type II errors are likely when testing interaction effects in non-experimental designs, interactions were deemed significant when p<0.10.(Busemeyer and Jones, 1983; McClelland and Judd, 1993) This cut-point has been increasingly used in research on the social determinants of health.(e.g., Chae et al., 2010; Chae et al., 2008; Cooper, 2010; Shields et al., 2008; Wei et al., 2008) SEP access and OTC pharmacy access were logged to linearize their relationships to each outcome. We selected optimal models using likelihood ratio tests, visual displays of data, and relevant literature.(Raudenbush and Bryk, 2002; Singer and Willett, 2003) Individual-level continuous variables were mean-centered. Time-varying continuous variables were centered at their initial value.(Raudenbush and Bryk, 2002; Singer and Willett, 2003) Since no districts had arrest rates of zero in 1995, we constructed the baseline drug-related arrest rate variable so that it equaled zero when arrest rates were at their lowest. Study year and district were treated as random variables. The optimal covariance structure for time-varying observations was autoregressive; the optimal covariance structure was unstructured for district-level observations. Analyses were conducted in SAS 9.2 and ArcInfo 9.3.(ESRI, 2006; SAS Institute, 2008)
Results
Approximately 80% of the Risk Factors participants included in these analyses were men (Table 1). Half the participants were Latino, 21% were African-American/Black, and 28% were White or of another race. In the six months preceding the interview, slightly less than half of the participants reported that they had injected with a sterile syringe ≤25% of the time and one quarter reported engaging in DSS.
Table 1.
Select sociodemographic characteristics and injection practices of individual injectors in the sample (N=4,067)
| Characteristics of Individual Injectors | No. (%) or Median (Range) |
|---|---|
| Gender | |
| Woman | 846 (20.80%) |
| Man | 3,221 (79.20%) |
| Race/ethnicity | |
| Latino/a (regardless of race) | 2,005 (50.31%) |
| Non-Hispanic Black/African-American | 848 (20.85%) |
| Non-Hispanic White and Other3 | 1,132 (27.83%) |
| Age | 38 (18, 75) |
| Heterosexual | 3,628 (89.21%) |
| Homeless | 1,374 (33.78%) |
| HIV positive (self-report) | 463 (11.38%) |
| Years since started injecting | 14 (0, 52) |
| Injected ≥4 times a day in the last 6 mo | 1,736 (42.69%) |
| Injected with a sterile syringe in the last 6 mo | |
| ≤ 25% of injection events | 1939 (47.68%) |
| 26% - 74% of injection events | 768 (18.88%) |
| ≥ 75% of injection events | 1,360 (33.44%) |
| Gave a used syringe to someone in the last 6 mo | 1,044 (25.67%) |
Only 87 people reported that they were not Latino/Hispanic, White or African-American/Black during the study period. These individuals were grouped with non-Hispanic White individuals in analyses because their risk profile most closely matched those of this racial/ethnic group.
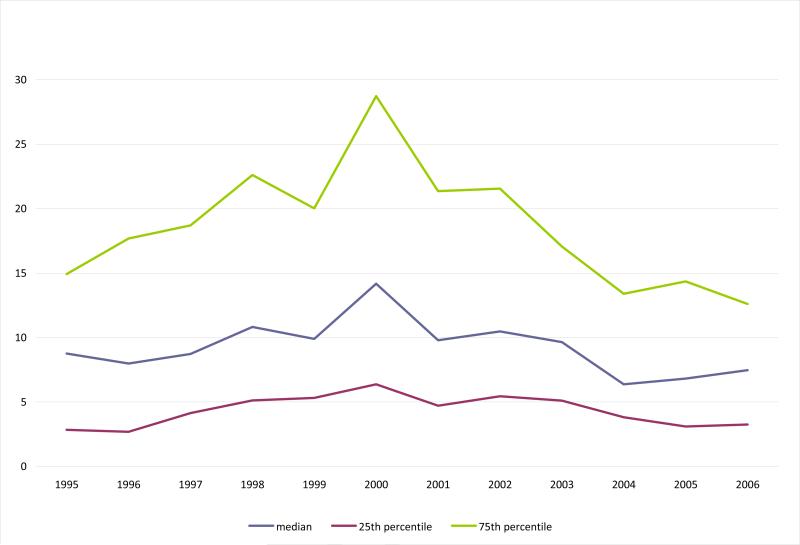
District-level drug-related arrest rates first rose and then fell between 1995-2006. The median drug-related arrest rate in 1995 was 8.75 arrests/1000 residents. This rate increased by 62% to 14.18/1000 in 2000, and then declined by 47% to 7.46 in 2006 (Figure 1a). The 25th and 75th percentiles followed roughly similar trajectories, although at different scales.
Figure 1a.
Median and Interquartile Range of Drug-Related Arrest Rates Per 1000 Adults in New York City Health Districts Over Time (1995-2006)
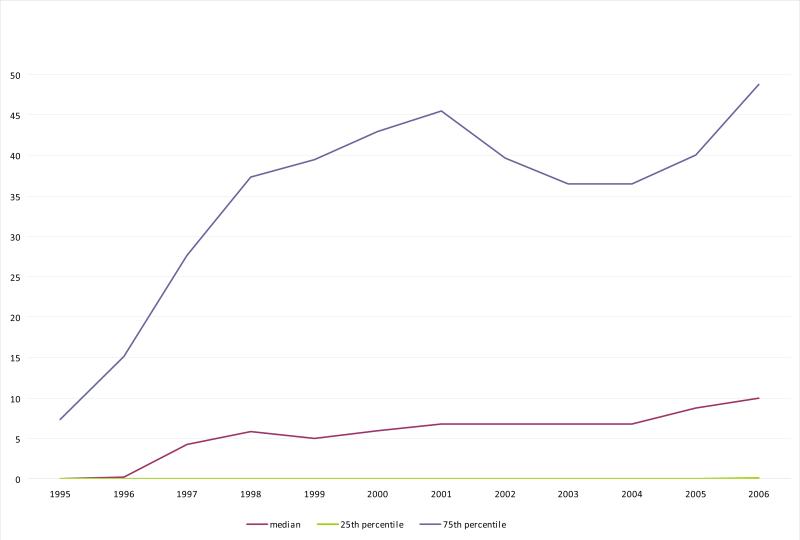
Twenty-three districts had no SEP within 1.00 mile in 1995, and nine had no SEP access throughout the study period. Across the 42 health districts, the median percent of district surface area within a mile of an SEP increased from 0% in 1995 to 6.75% in 2001, remained static between 2001-2004, and then increased by 43% to 10.00% in 2005 (Figure 1b). The 75th percentile increased more than sixfold between 1995 and 2001, from 7.34% to 45.53%; after declining between 2002 and 2005, the 75th percentile returned to its 2001 value in 2006 (48.81%).
Figure 1b.
Median and Interquartile Range of Spatial Access to Syringe Exchange Programs (SEPs) in New York City Health Districts Over Time (1995-2006)
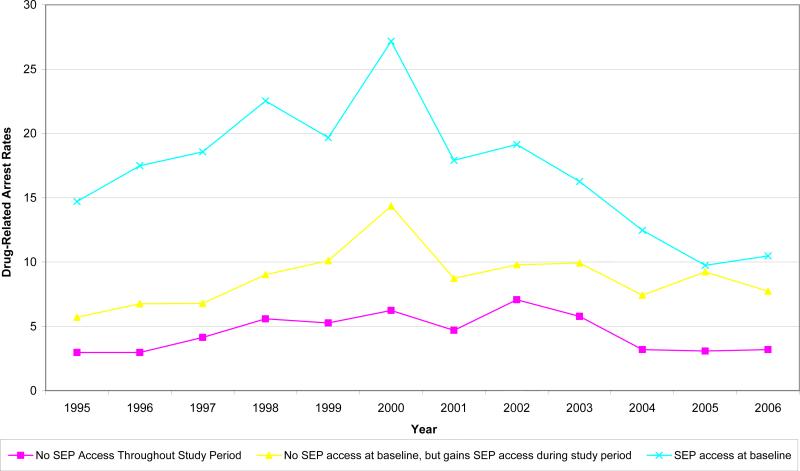
Research Question 1: Spatial Overlap of SEPs and User-Focused Drug Enforcement
Analyses indicate that drug-related arrest rates were higher in districts that had better SEP access. In the nine districts that had no SEP access throughout the study period, median drug-related arrest rates were low and relatively stable over time, ranging from 2.96-7.07 arrests/1000 residents (Figure 1c). In the 14 districts that had no SEP access in 1995 but later gained access to such programs, median arrest rates were slightly higher and fluctuated between 5.70-14.36/1000 residents over time. Median arrest rates were substantially higher in the remaining districts, and ranged from 9.74-27.16/1000
Figure 1c.
Drug-Related Arrest Rates per 10,000 Adults in New York City Health Districts (1995-2006), Classed by District-Level SEP Access
The statistical model designed to explore the relationship of drug-related arrests to SEP access indicates that the average drug-related arrest rate in 1995 was 8.35 arrests/1000 adult residents in districts that had no spatial access to an SEP (p<0.0001; Table 2). On average at baseline, a one-unit difference in logged SEP access across districts was positively associated with a difference of 5.38 drug-related arrests/1000 residents (p<0.0001), though this variable's interaction with study year indicates that this relationship declined over time. Turning to time-dependent findings, on average a one-unit increase in logged SEP access over time was associated with an increase of 11.18 arrests/1000 residents (p<0.0001); the magnitude of this relationship declined over time.
Table 2.
Regression of Spatial Access to Syringe Exchange Programs (SEPs) on Drug-Related Arrest Rates per 1000 Residents in New York City's 42 Health Districts Over Time (1995-2006)
| Variable | Estimate | p-value |
|---|---|---|
| Intercept | 8.35 | <0.0001 |
| Time4 | 2.76 | <0.0001 |
| Time-Squared | -0.10 | 0.008 |
| Log of SEP Access in 1995 | 5.38 | <0.0001 |
| Log SEP Access in 1995 * Time | -0.24 | 0.0007 |
| Log of the Change in SEP Access Since 1995 | 11.18 | <0.0001 |
| Log of the Change in SEP Access Since 1995 * Time | -0.73 | 0.0007 |
Number of years since study period began.
Research Question 2: Racialized Risk Environments
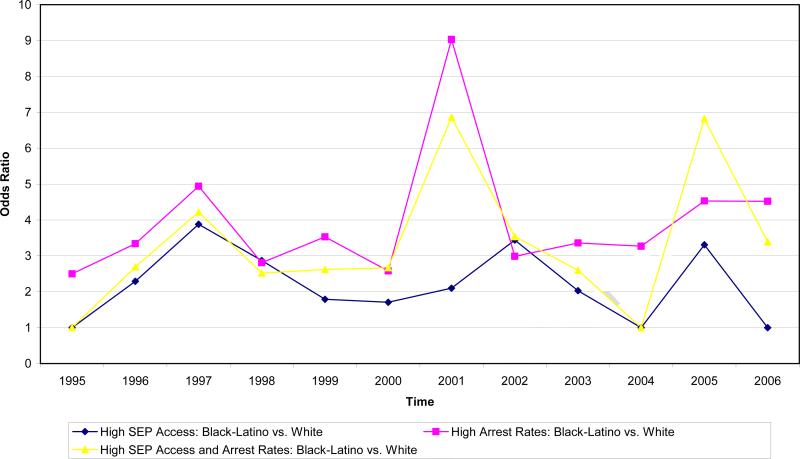
Figure 2 depicts the odds that Black and Latino injectors vs. White injectors lived in a health district that was in the highest quartile for SEP access, drug-related arrest rates, or both (Black and Latino injectors were collapsed into one group because they were similarly distributed across districts). Over the course of the study period, Black and Latino injectors were between 2.50 and 9.03 times more likely to live in a health district that had a high arrest rate (median OR across time: 3.35). Annual odds ratios peaked in 2001 at 9.03, when arrest rates were at their highest in the city, and seem to rise toward the end of the study period. Racial/ethnic differences in the odds of living in a health district with high SEP access were less striking: odds ratios ranged from 1.00 to 3.88 (median OR across time: 2.06), and did not attain statistical significance in three years of the study period. Black and Latino injectors were between 1.00 and 6.86 times more likely than White injectors to live in a health district that had both high arrest rates and high SEP access (median OR across time: 2.68). Odds ratios peaked in 2001 and in 2005 at 6.86 and 6.82, respectively.
Figure 2.
Odds of Living in an NYC Health District with High SEP Access, Drug-Related Arrest Rates, or Both for Black/Latino Injectors vs. White Injectors (Odds Ratios that are not statistically significant were set to equal 1.00)
Research Question 3: Relationship of SEPs and User-Focused Drug Enforcement to Local Injectors’ Risk Behavior
Growth curve models (GCMs) indicate that at baseline 50% of participants reported injecting with a sterile syringe during ≤25% of injection events in the past six months (Table 3); 21% of participants injected with a sterile syringe between 26% and 74% of injection events during that period.1 (Note: The magnitude and direction of relationships between our primary predictors and the ordinal values for this outcome are identical; hereafter we therefore discuss results in terms of injecting with a sterile syringe ≤25% of the time). The optimal GCM contained coefficients for the interaction of year and time since OTC pharmacy sales were legalized. Specifically, the odds of injecting with a sterile syringe ≤25% of the time increased 10% annually on average until 2001 (AOR=1.10, p=0.0003). With the onset of OTC syringe sales in 2001, this trend reversed course (AOR=0.96, p=0.003).
Table 3.
Regression of Spatial Access to Syringe Exchange Programs (SEPs) and of Drug-Related Arrest Rates per 1000 Residents on Select Risk Behaviors Among Injection Drug Users (N=4067) in New York City's 42 Health Districts Over Time (1995-2006)
| Injecting with an Unsterile Syringe | Distributive Syringe Sharing | |||||||
|---|---|---|---|---|---|---|---|---|
| GCM AOR | p-value | Full explanatory model | p-value | GCM AOR | p-value | Full explanatory model | p-value | |
| Intercept5 | 1.08 | 0.74 | 1.37 | 0.36 | N/A | N/A | N/A | N/A |
| Intercept6 | 2.49 | 0.003 | 3.17 | 0.002 | 2.30 | 0.02 | 2.53 | 0.02 |
| Age (ref: >40) | 0.92 | |||||||
| <30 years | 1.18 | 0.17 | 1.20 | 0.12 | 1.47 | 0.009 | 1.49 | 0.007 |
| 31-40 years | 1.10 | 0.30 | 1.10 | 0.28 | 1.16 | 0.18 | 1.16 | 0.18 |
| Gender (ref: men) | 0.79 | 0.005 | 0.79 | 0.006 | 1.23 | 0.04 | 1.25 | 0.02 |
| Race/ethnicity (ref: Latino) | ||||||||
| Black | 0.96 | 0.66 | 0.96 | 0.68 | 0.88 | 0.25 | 0.88 | 0.26 |
| White | 1.32 | 0.002 | 1.29 | 0.004 | 1.45 | 0.0002 | 1.36 | 0.002 |
| Homeless | 1.26 | 0.002 | 1.25 | 0.002 | 1.49 | <0.0001 | 1.48 | <0.0001 |
| Lesbian/Gay/Bisexual | 1.14 | 0.23 | 1.16 | 0.18 | 1.41 | 0.008 | 1.37 | 0.01 |
| HIV-positive (self-report) | 0.96 | 0.67 | 0.96 | 0.69 | 0.68 | 0.008 | 0.67 | 0.005 |
| Inject ≥4 times daily | 1.76 | <0.0001 | 1.76 | <0.0001 | 1.63 | <0.0001 | 1.64 | <0.0001 |
| Married | 0.79 | 0.005 | 0.79 | 0.005 | 1.12 | 0.27 | 1.09 | 0.38 |
| Education (ref: <high-school grad) | ||||||||
| High-school graduate | 0.91 | 0.22 | 0.91 | 0.24 | 0.91 | 0.32 | 0.90 | 0.25 |
| More than high-school graduate | 0.74 | 0.0005 | 0.73 | 0.0004 | 0.92 | 0.41 | 0.92 | 0.42 |
| Deviation from mean years of injecting for district and year | 1.00 | 0.85 | 1.00 | 0.79 | 1.00 | 0.37 | 1.00 | 0.34 |
| Mean years since first injection for that district and year | 0.99 | 0.18 | 0.99 | 0.17 | 0.98 | 0.08 | 0.98 | 0.13 |
| Time | 1.10 | 0.0003 | 1.13 | <0.0001 | 0.92 | <0.0001 | 0.93 | 0.003 |
| Years since OTC pharmacy sales permitted | 1.16 | 0.29 | 2.71 | <0.0001 | N/A | N/A | ||
| Time * Years since OTC pharmacy sales permitted | 0.96 | 0.003 | 0.90 | <0.0001 | N/A | N/A | ||
| Difference of 10 drug-related arrests per 1000 residents in 1995 | 1.13 | 0.09 | 1.02 | 0.59 | ||||
| Spatial access to SEPs in 1995 (natural log) | 0.93 | 0.05 | 0.95 | 0.09 | ||||
| Interaction of a ten-unit change in drug-related arrests per 1000 in 1995 with the log of spatial access to SEPs in 1995 | 0.96 | 0.07 | N/A | N/A | ||||
| 10-unit change in drug-related arrests per 1000 since 1995 | 0.99 | 0.88 | 1.04 | 0.52 | ||||
| Changes in the log of spatial access to SEPs since 1995 | 0.94 | 0.29 | 0.93 | 0.15 | ||||
| Poverty area | 0.95 | 0.59 | 0.82 | 0.05 | ||||
| Spatial access to an OTC pharmacy (logged) | 0.82 | <0.0001 | 0.98 | 0.51 | ||||
When receptive syringe sharing is the outcome, this is the intercept when the outcome is injecting with a sterile syringe in ≤25% of the time.
When receptive syringe sharing is the outcome, this is the intercept when the outcome is injecting with a sterile syringe 26%-74% of the time.
In the full explanatory model, the interaction between drug-related arrest rates in 1995 and SEP access in 1995 was statistically significant, indicating that the relationship of one district-level exposure to the odds of injecting with an unsterile syringe depended on the other district-level exposure. Specifically, within the 23 districts that had no SEP access in 1995, a difference across districts of 10 arrests per 1000 residents at baseline was positively associated with a 13% difference in the odds of rarely injecting with a sterile syringe on average (AOR=1.13; p=0.092). In districts that had low drug-related arrest rates in 1995, we find that a one-unit difference in the log of SEP access across districts at baseline was negatively related to a 7% difference in this outcome on average (AOR=0.93, p=0.05). In districts that had both SEP access and higher drug-related arrest rates in 1995, higher drug-related arrest rates appear to erode local SEPs’ protective effects on sterile syringe use, and vice versa (AOR=0.96; p=0.07). The relationship between subsequent increases in SEP access over time and the odds of rarely injecting with a sterile syringe was not statistically significant, nor was the relationship between changes in drug-related arrest rates over time to this outcome.
As we have found in previous analyses(Cooper et al., 2011), injectors living in districts with better spatial access to OTC pharmacies were less likely to inject with unsterile syringes. Specifically, a one-unit increase in the log of OTC pharmacy access was associated with an 18% decline in the odds of rarely injecting with a sterile syringe (AOR=0.82; p<0.0001).
GCM analyses indicate that at baseline 72% of participants on average reported DSS at least once in the past 6 months. On average across districts the odds of reporting DSS decreased linearly over time by 8% annually (AOR= 0.92; p<0.0001). The full model contained no interaction between arrest rates and SEP access. The relationship between baseline SEP access and DSS attained borderline significance (p=0.09), and suggests a trend in which a one-unit difference in logged SEP access across districts at baseline is negatively associated with a 5% difference in the odds of engaging in DSS. Subsequent increases in SEP access over time were unrelated to DSS, and drug-related arrest rates were not associated with DSS.
Discussion
Our analyses found considerable spatial overlap between SEP access and drug-related arrest rates in NYC health districts, and indicate that this spatial overlap – an overlap that Black and Latino injectors are considerably more likely than White injectors to experience in the districts where they live – has consequences for local injectors’ injection practices. Districts with better SEP access at baseline had higher drug-related arrests, and districts that experienced increases in SEP access over time also experienced increases in arrest rates over time, though the magnitude of this relationship decayed as time passed. The spatial overlap of these two features of the risk and protective environment likely reflects their shared target population and target behaviors. SEPs may have been established in high-need locations, and police drug crackdowns (a user-focused drug strategy implemented by the NYC Police Department from 1994-2001) targeted geographic areas with high drug activity. The temporal decay that we found in the strength of the relationship between district-level SEP access and arrest rates likely reflects diverging trajectories of these two structural interventions in the city over the study period: spatial access to legal SEPs rose throughout the study period, an increase that may have been driven by grassroots advocacy, growing local acceptance of SEPs, and improved funding in the wake of the 1992 state policy change that permitted select SEPs to operate. (Tempalski, 2007; Tempalski et al., 2008; Tempalski et al., 2007) In contrast, drug-related arrest rates began to fall in 2002 when Mayor Giuliani, the architect of NYC's user-focused enforcement strategies, stepped down. (N.B., violent crime rates continued to fall, even after the de-escalation of drug-related enforcement.(FBI Uniform Crime Reports, 2011))
Our analyses suggest that this spatial overlap eroded the relationship between SEP access and safer injection practices. In districts with low drug-related arrest rates in 1995, SEPs were associated with lower rates of unsterile injecting among local residents. Where SEP access was accompanied by higher drug-related arrest rates, however, SEPs’ protective effects were attenuated. As discussed above, several mechanisms may have weakened this relationship. User-focused enforcement activities can reduce SEP utilization, and possibly also the number of syringes that SEPs distribute.(Aitken et al., 2002; Bluthenthal et al., 1997; Davis et al., 2005; Hammett et al., 2005; Rhodes et al., 2003; Small et al., 2006; Wood et al., 2003) Intensive user-focused enforcement activities can also profoundly affect local injecting communities and injectors’ drug use patterns. Injectors living in areas with high drug-related arrest rates may experience substantial turnover in their injecting networks, as network members cycle through jail and prison. This turnover may disrupt secondary syringe exchange activities. Additionally, injectors operating in heavily-policed circumstances develop strategies that may increase HIV risk. These include not carrying syringes to avoid detection as a user, (Bourgois et al., 1997; Cooper et al., 2005a; Maher and Dixon, 1999) and trying to minimize contact with one another in public spaces.(Cooper et al., 2005a) Minimizing contact with other injectors may reduce their risk of arrest, but may also curtail injectors’ ability to circulate sterile syringes. We note that it is also possible that the resulting reduced contact among injectors may have diminished opportunities for group injecting, and thus have reduced HIV transmission.
Our analyses suggest that SEP access and drug-related arrest rates are deeply racialized features of risk and protective environments. While Black and Latino injectors had better odds of living in districts with high SEP access than White injectors, they also had greater odds of living in districts with high drug-related arrest rates, and of living in districts where both of these features were particularly prominent. We note that the magnitudes of the odds ratios suggest that spatial access to SEPs, a protective feature, was more evenly distributed across racial/ethnic groups of injectors than arrest rates, a harmful feature. When integrated with our findings about the combined effects of SEPs and drug-related arrest rates on injection practices, our results collectively suggest that this particular racialization of the risk and protective environment may undermine SEPs’ ability to reduce longstanding racial/ethnic disparities in injection-related harms.(Des Jarlais et al., 2009; Friedman et al., 1999a)
We found no statistically significant relationship between changes in SEP access or drug-related arrest rates over time and injecting with an unsterile syringe. This absence of a relationship may be a function of limited statistical power: it is often difficult to detect relationships between changes in time-varying predictors and outcomes.(Basagañaa and Spiegelman, 2009) While we analyzed data from >4000 injectors, participants were distributed across 12 years and 42 districts in this serial cross-sectional study.
In this sample, DSS was unrelated to drug-related arrest rates and had a marginally significant relationship to SEP access. Possibly – and consonant with studies of other samples of injectors (Cooper et al., 2005a; Maher and Dixon, 1999; Small et al., 2006)– Risk Factors participants living in high-arrest districts rapidly discarded their syringes in public spaces after using them; while others may have retrieved (and used) these discarded syringes, these participants would not have reported this inadvertent syringe transfer as “DSS” (though recipients would report injecting with a used syringe). SEPs reduce DSS among their participants.(Golub et al., 2007; Ouellet et al., 2004; Vlahov et al., 1997) While our analysis found a trend toward a protective relationship between SEP access and DSS, it was not statistically significant. Unlike our unsterile injecting variable (which was ordinal), DSS was operationalized as a dichotomous variable, and thus might have been insufficiently sensitive to capture variations in this behavior across time and space.
These findings must be considered in light of four possible limitations. First, spatial access to SEP sites does not necessarily parallel access to sterile syringes acquired from an SEP. A portion of sterile syringes acquired from SEPs are redistributed to other districts via satellite and secondary exchanges, and by injectors who travel (perhaps via public transportation) across district boundaries to acquire syringes from SEPs for personal use. Given that the overall direction of this redistribution is most likely from districts with SEP access to districts with poor or no SEP access, this redistribution likely biases relationships between SEP access and unsterile injecting (and DSS) to the null. Possibly further driving these relationships to the null, illegal SEPs may tend to be located in districts with poor spatial access to legal SEPs. Additionally, SEP sites vary in the number of syringes they distribute annually. Though we are developing a measure that includes the volume of syringes distributed by each site, the present measure simply assessed spatial access to an SEP site.
Second, we might not have controlled for all relevant compositional changes in the Risk Factors sample. Residual confounding might conflate changes in the sample's composition over time with temporal changes in the outcomes, or in focal predictors’ relationships to the outcomes.
Third, the Risk Factors sample is not randomly drawn from the underlying population of NYC injectors. The extent to which our findings can be generalized to this underlying population is unknown, though our results are consonant with a large body of research on SEPs, drug-related enforcement activities, and injectors’ risk behaviors.
Finally, we may have misclassified exposure to district-level constructs for some injectors. Health districts do not necessarily reflect injectors’ subjective neighborhoods. Additionally, injectors may use drugs, and access drugs and injection paraphernalia, outside of the district where they live. We did not gather data on the locations of these activities.
In summary, our analyses identified a high level of geospatial overlap between SEP access and drug-related arrests in NYC health districts, an overlap that Black and Latino injectors are more likely to experience than White injectors. The co-location of SEPs and drug-related arrests appears to undermine SEPs’ effectiveness at reducing unsterile injecting. These findings have implications for both research and policy. The Risk Environment Model calls attention to the possibility that dimensions of the risk and protective environment may interact with one another to shape injectors’ vulnerability to HIV.(Rhodes et al., 2005) Empirical research, however, rarely explores this interplay, despite the likely co-location of several place-based features of the risk and protective environment. Our results testify to the importance of exploring this interplay, both in research on SEPs and arrests and more broadly. They also testify generally to the utility of conceptualizing harm reduction efforts (and drug-related enforcement efforts) as structural, place-based phenomena.(Cooper et al., 2008; Tempalski and McQuie, 2009)
Additionally, our findings contribute to the large body of research that suggests that user-focused law enforcement activities should be de-emphasized in the microenvironments surrounding SEPs. As others have found (Aitken et al., 2002; Bluthenthal et al., 1997; Davis et al., 2005; Rhodes et al., 2003; Small et al., 2006; Wood et al., 2003), these efforts impair SEP operations. They also appear to undermine these programs’ capacity to support injectors’ harm reduction practices.
Highlights.
Areas with more spatial access to syringe exchange programs have more drug arrests
Drug-related arrests damage SEPs’ protective effects on injectors’ HIV risk
Enforcement efforts targeting drug users should be scaled back in areas around SEPs
Acknowledgements
This research was supported by three NIDA grants: Spatial Variations in IDU HIV Risk: Relationship to Structural Interventions (5R21DA023391; PI: Hannah Cooper); Community Vulnerability and Responses to Drug-User-Related HIV/AIDS (5R01DA013336 ; PI: Samuel R. Friedman); and Risk Factors for HIV/AIDS in Drug Users (5R01DA003574 ; PI: Don Des Jarlais). We would also like to thank the New York State Department of Health for kindly sharing data on SEP location and on pharmacies that were registered to sell syringes over the counter, and staff at St. Ann's Corner of Harm Reduction for their help finding “missing” years of SEP location data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The probability of RSS at baseline was calculated as follows: 1/(1+ exponent(-intercept)). When intercepts were not statistically significant, they were entered into this formula as 0.00.
As discussed in the methods section, we have used p<0.10 as our cutpoint for statistical significance when considering interactions of two geospatial exposures.
Contributor Information
Hannah LF Cooper, Department of Behavioral Sciences and Health Education Rollins School of Public Health at Emory University 1518 Clifton Road NE, Room 526 Atlanta, GA 30322 USA Phone: 404 727 – 0261 Fax: 404 727 -1369 hcoope3@emory.edu.
Don C Des Jarlais, Baron Edmund de Rothschild Chemical Dependency Institute at Beth Israel Hospital dcdesjarla@aol.com.
Barbara Tempalski, National Development and Research Institutes, Inc Tempalski@ndri.org.
Brian H Bossak, Jiann-Ping Hsu College of Public Health at Georgia Southern University bbossak@georgiasouthern.edu.
Zev Ross, ZevRoss Spatial Analysis zev@zevross.com.
Samuel R Friedman, National Development and Research Institutes, Inc Friedman@ndri.org.
References
- Aitken C, Moore D, Higgs P, Kelsall J, Kerger M. The impact of a police crackdown on a street drug scene: evidence from the street. International Journal of Drug Policy. 2002;13:193–202. [Google Scholar]
- Basagañaa X, Spiegelman D. Power and sample size calculations for longitudinal studies comparing rates of change with a time-varying exposure. Statistics in Medicine. 2009;29:181–192. doi: 10.1002/sim.3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastos FI, Strathdee SA. Evaluating the Effectiveness of Syringe Exchange Programmes: Current Issues and Future Prospects. Social Science & Medicine. 2000;51:1771–1782. doi: 10.1016/s0277-9536(00)00109-x. [DOI] [PubMed] [Google Scholar]
- Beckett K, Nyrop K, Pfingst L. Race, drugs, and policing: understanding disparities in drug delivery arrests. Criminology. 2006;44:105–137. [Google Scholar]
- Beletsky L, Grau L, White E, Bowman S, Heimer R. The roles of law, client race and program visibility in shaping police interference with the operation of US syrigne exchange programs. Addiction. 2011;106:357–365. doi: 10.1111/j.1360-0443.2010.03149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blankenship KM, Friedman SR, Dworkin S, Mantell J. Structural Interventions: Concepts, Challenges, and Opportunities for Research. Journal of Urban Health. 2006;83:59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Kral A, Erringer E, Edlin BR. Drug paraphernalia laws and injection-related infectious disease risk among drug injectors. Journal of Drug Issues. 1999a;29:1–16. [Google Scholar]
- Bluthenthal RN, Kral AH, Lorvick J, Watters JK. Impact of law enforcement on syringe exchange programs: a look at Oakland and San Francisco. Medical Anthropology. 1997;18:61–83. doi: 10.1080/01459740.1997.9966150. [DOI] [PubMed] [Google Scholar]
- Bluthenthal RN, Lorvick J, Kral AH, Erringer EA, Kahn JG. Collateral damage in the war on drugs: injection drug use. International Journal of Drug Policy. 1999b;10:25–38. [Google Scholar]
- Bonilla-Silva E. White Supremacy and Racism in the Post-Civil Rights Era. Rienner; Boulder, Colorado: 2001. [Google Scholar]
- Bourgois P, Lettiere M, Quesada J. Social Misery and the Sanctions of Substance Abuse: Confronting HIV risk among homeless heroin addictis in San Francisco. Social Problems. 1997;44:155–173. [Google Scholar]
- Burris S, Anderson ED, Craigg A, Davis C, Case P. Racial disparities in injection-related HIV: A case study of toxic law. Temple Law Review Spring/Summer. 2010:1–51. [Google Scholar]
- Busemeyer JR, Jones LE. Analysis of multiplicative combination rules when the causal variables are measured with error. Psychological Bulletin. 1983;93:549–562. [Google Scholar]
- Centers for Disease Control and Prevention. Health Resources & Services Administration. National Institute on Drug Abuse of the National Institutes of Health, Administration. t.C.f.S.A.T.o.t.S.A.a.M.H.S. HIV prevention bulletin: Medical advice for persons who inject illicit drugs. 1997.
- Chae DH, Lincoln KD, Adler N, Syme SL. Do experiences of racial discrimination predict cardiovascular disease among African American men? The moderating role of internalized negative racial group attitudes. Social Science & Medicine. 2010;71:1182–1188. doi: 10.1016/j.socscimed.2010.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chae DH, Takeuchi D, Barbeau EM, Bennett G, Lindsay J, Stoddard A, Krieger N. Alcohol disorders among Asian Americans: associations with unfair treatment, racial/ethnic discrimination, and ethnic identification (the national Latino and Asian Americans study, 2002–2003). Journal of Epidemiology and Community Health. 2008;62:973–979. doi: 10.1136/jech.2007.066811. [DOI] [PubMed] [Google Scholar]
- Cooper H, Bossak BH, Tempalski B, Friedman SR, Des Jarlais DC. Temporal trends in spatial access to pharmacies that sell over-the-counter syringes in New York City health districts: Relationship to local racial/ethnic composition and need. Journal of Urban Health. 2009;86:929–945. doi: 10.1007/s11524-009-9399-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Moore L, Gruskin S, Krieger N. Characterizing Perceived Police Violence: Implications for Public Health. American Journal of Public Health. 2004;94:1109–1118. doi: 10.2105/ajph.94.7.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Moore L, Gruskin S, Krieger N. The Impact of a Police Drug Crackdown on Drug Injectors’ Ability to Practice Harm Reduction: A Qualitative Study. Social Science & Medicine. 2005a;61:673–684. doi: 10.1016/j.socscimed.2004.12.030. [DOI] [PubMed] [Google Scholar]
- Cooper HL, Bossak BH, Tempalski B, Des Jarlais DC, Friedman SR. Geographic approaches to quantifying the risk environment: Drug-related law enforcement and access to syringe exchange programmes. International Journal of Drug Policy. 2008;20:217–226. doi: 10.1016/j.drugpo.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Des Jarlais C, Ross Z, Tempalski B, Bossak B, Friedman S. Spatial access to syringe exchange programs and pharmacies selling over-the-counter syringes predicts drug injectors’ use of sterile syringes. American Journal of Public Health. 2011;101:1118–1125. doi: 10.2105/AJPH.2009.184580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Wypij D, Krieger N. Police Drug Crackdowns and Hospitalization Rates For Illicit-Injection-Related Infections in New York City. International Journal of Drug Policy. 2005b;16:150–160. [Google Scholar]
- Cooper ML. Toward a Person ⍰ Situation Model of Sexual Risk-Taking Behaviors: Illuminating the Conditional Effects of Traits Across Sexual Situations and Relationship Contexts. Journal of Personality and Social Psychology. 2010;98:319–341. doi: 10.1037/a0017785. [DOI] [PubMed] [Google Scholar]
- Davis CS, Burris S, Kraut-Becher J, Lynch KG, Metzger D. Effects of an intensive street-level police intervention on syringe exchange program use in Philadelphia, PA. American Journal of Public Health. 2005;95:2333–2236. doi: 10.2105/AJPH.2003.033563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais D, Arasteh K, Hagan H, McKnight C, Perlman D, Friedman S. Persistence and change in disparities in HIV infection among injection drug users in New York City after large-scale syringe exchange programs. American Journal of Public Health. 2009;99:S445–451. doi: 10.2105/AJPH.2008.159327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais D, Perlis T, Arasteh K, Torian L, Beatrice S, Milliken J, Mildvan D, Yancovitz S, Friedman S. HIV incidence among injection drug users in New York City, 1990 to 2002: use of serologic test algorithm to assess expansion of HIV prevention services. American Journal of Public Health. 1996a;95:1439–1444. doi: 10.2105/AJPH.2003.036517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Des Jarlais DC. Structural interventions to reduce HIV transmission among injecting drug users. AIDS. 2000;14:S41–S46. doi: 10.1097/00002030-200006001-00006. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Arasteh K, Perlis T, Hagan H, Abdul-Quader A, Heckathorn DD, McKnight C, Bramson H, Nemeth C, Torian L, Friedman SR. Convergence of HIV seroprevalence among injecting and non-injecting drug users in New York City. AIDS. 2007;21:231–235. doi: 10.1097/QAD.0b013e3280114a15. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Guardino V, Arasteh K, McKnight C, Milliken J, Purchase D. Current state of syringe exchange in the known universe, NASEC 2010. Austin; Texas: 2010. [Google Scholar]
- Des Jarlais DC, Marmor M, Paone D, Titus S, Shi Q, Perlis T, Jose B, Friedman SR. HIV incidence among injecting drug users in New York City syringe-exchange programmes. Lancet. 1996b;348:987–991. doi: 10.1016/s0140-6736(96)02536-6. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Perlis T, Arasteh K, Hagan H, Milliken J, Braine N, Yancovitz S, Mildvan D, Perlman D, Maslow C, Friedman SR. “Informed altruism” and “Partner restriction” in the reduction of HIV infection in injecting drug users entering detoxification treatment in New York City, 1990-2001. JAIDS. 2004;35:158–166. doi: 10.1097/00126334-200402010-00010. [DOI] [PubMed] [Google Scholar]
- ESRI . ArcInfo. 9.2 ed. ESRI; Redlands, CA: 2006. [Google Scholar]
- FBI Uniform Crime Reports . Crime reported by New York City Police Dept, New York from 1985 - 2009. FBI; 2011. [Google Scholar]
- Friedman SR, Chapman TF, Perlis TE, Rockwell R, Paone D, Sotheran JL, Des Jarlais DC. Similarities and differences by race/ethnicity in changes of HIV seroprevalence and related behaviors among drug injectors in New York City, 1991-1996. Journal of Acquired Immune Deficiency Syndromes: JAIDS. 1999a;22:83–91. doi: 10.1097/00042560-199909010-00011. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Cooper HL, Tempalski B, Keem M, Friedman R, Flom PL, Des Jarlais DC. Relationships of deterrence and law enforcement to drug-related harms among drug injectors in US metropolitan areas. AIDS. 2006;20:93–99. doi: 10.1097/01.aids.0000196176.65551.a3. [DOI] [PubMed] [Google Scholar]
- Friedman SR, Curtis R, Neaigus A, Jose B, Des Jarlais DC. Social Networks, Drug Injectors’ Lives, and HIV/AIDS. Kluwer/Plenum; New York: 1999b. [Google Scholar]
- Fyfe N. Space, time, and policing: toward a contexual understanding of police work. Environment and planning D: society and space. 1992;10:469–481. [Google Scholar]
- Gibson DR, Brand R, Anderson K, Kahn JG, Perales D, Guydish J. Two- to Sixfold Decreased Odds of HIV Risk Behavior Associated with Use of Syringe Exchange. JAIDS. 2002;31:237–242. doi: 10.1097/00126334-200210010-00015. [DOI] [PubMed] [Google Scholar]
- Gibson DR, Flynn NM, Perales D. Effectiveness of syringe exchange programs in reducing HIV risk behavior and HIV seroconversion among injecting drug users. AIDS. 2001;15:1329–1341. doi: 10.1097/00002030-200107270-00002. [DOI] [PubMed] [Google Scholar]
- Golub E, Strathdee SA, Bailey S, Hagan H, Latka MH, Hudson SM, Garfein RS. Distributive syringe sharing among young adult injection drug users in five U.S. cities⍰. Drug and Alcohol Dependence. 2007;91S:S30–S38. doi: 10.1016/j.drugalcdep.2007.02.013. [DOI] [PubMed] [Google Scholar]
- Greene J. Zero-tolerance: A case study of police policies and practices in New York City. Crime and Delinquency. 1999;45:171–187. [Google Scholar]
- Grund JP, Heckathorn D, Anthony D. In Eastern Connecticut, IDUs purchase syringes from pharmacies but don't carry syringes. JAIDS. 1995;10:105. doi: 10.1097/00042560-199509000-00016. [DOI] [PubMed] [Google Scholar]
- Hammett TM, Bartlett NA, Chen Y, Ngu D, Cuong DD, Phoung NM, Tho NH, Van LK, Liu W, Donghua M, Shamoi X, Chen H, Quyen HN, Broadhead RS, Des Jarlais DC. Law enforcement influences on HIV prevention for injection drug users: Observations from a cross-border project in China and Viet Nam. International Journal of Drug Policy. 2005;16:235–245. [Google Scholar]
- Herbert S. The normative ordering of police territoriality: Making and marking space with the Los Angeles police department. Annals of the American Association of Geographers. 1996;86:567–582. [Google Scholar]
- Herbert S. Territoriality and the police. Professional Geographer. 1997;49:86–94. [Google Scholar]
- Hutchinson S, Taylor A, Goldberg D, Gruer L. Factors Associated with injecting risk behavior among serial community-wide samples of injecting drug users in Glasgow 1990-1994: implications for control and prevention of blood-borne viruses. Addiction. 2000;95:931–940. doi: 10.1046/j.1360-0443.2000.9569319.x. [DOI] [PubMed] [Google Scholar]
- Kaplan E, Heimer R. A circulation theory of needle exchange. AIDS. 1994;8:567–574. doi: 10.1097/00002030-199405000-00001. [DOI] [PubMed] [Google Scholar]
- Kerr T, Small W, Wood E. The public health and social impacts of drug market enforcement: A review of the evidence. International Journal of Drug Policy. 2005;16:210–220. [Google Scholar]
- Ksobiech K. A Meta-Analysis of Needle Sharing, Lending, and Borrowing Behaviors of Needle Exchange Program Attenders. AIDS Education & Prevention. 2003;15:257–268. doi: 10.1521/aeap.15.4.257.23828. [DOI] [PubMed] [Google Scholar]
- Maas B, Fairbairn N, Kerr T, Li K, Montaner JSG, Wood E. Neighborhood and HIV infection among IDU: Place of residence independently predicts HIV infection among a cohort of injection drug users. Health and Place. 2007;13:432–439. doi: 10.1016/j.healthplace.2006.05.005. [DOI] [PubMed] [Google Scholar]
- Maher L, Dixon D. Policing and public health: law enforcement and harm reduction in a street-level drug market. British Journal of Criminology. 1999;39:488–512. [Google Scholar]
- Martinez AN, Bluthenthal RN, Lorvick J, Anderson R, Flynn NM, Kral AH. The impact of legalizing syringe exchange programs on arrests among injection drug users in California. Journal of Urban Health. 2007;84:423–435. doi: 10.1007/s11524-006-9139-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Miller C, Firestone M, Ramos R, Burris S, Ramos ME, Case P, Brouwer K, Fraga MA, Strathdee SA. Injecting drug users’ experiences of policing practices in two Mexican-US border cities: public health perspectives. International Journal of Drug Policy. 2008;19:324–331. doi: 10.1016/j.drugpo.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore M. An analytic view of drug control policies. Harvard University; Cambridge, MA: 1990. [Google Scholar]
- Murphy EL, DeVita D, Liu H, Vittinghoff E, Leung P, Ciccarone D, Edlin BR. Risk factors for skin and soft tissue abscess among injection drug users: A case–control study. Clinical Infectious Disease. 2001;33:35–40. doi: 10.1086/320879. [DOI] [PubMed] [Google Scholar]
- New York State Department of Health AIDS Institute . Expanded Syringe Access Program: Overview of the Law and Regulations. NYSDOH; New York City: 2008. [Google Scholar]
- Normand J, Vlahov D, Moses L. Preventing HIV transmission: the role of sterile needles and bleach. National Academy Press; Washington, DC: 1995. [PubMed] [Google Scholar]
- Ouellet L, Huo D, Bailey S. HIV Risk Practices among needle exchange users and non-users in Chicago. JAIDS. 2004;37:1187–1196. doi: 10.1097/01.qai.0000120802.43677.ea. [DOI] [PubMed] [Google Scholar]
- Pollini R, Brouwer KC, Lozada R, Ramos R, Cruz M, Magis-Rodriguez C, Case P, Burris S, Pu M, Frost SD, Palinkas LA, Miller C, Strathdee SA. Syringe possession arrests are associated with receptive syringe sharing in two Mexico-US border cities. Addiction. 2007;103:101–108. doi: 10.1111/j.1360-0443.2007.02051.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos R, Ferreira-Pinto J, Brouwer KC, Ramos ME, Lozada R, Firestone-Cruz M, Strathdee SA. A tale of two cities: Social and environmental influences shaping risk factors and protective behaviors in two Mexico-US border cities. Health and Place. 2009;15:999–1005. doi: 10.1016/j.healthplace.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush S, Bryk A. Hierarchical Linear Models: Applications and Data Analysis Methods. Sage; London, UK: 2002. [Google Scholar]
- Rhodes T. The ‘risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13:85–94. [Google Scholar]
- Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20:193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Mikhailova L, Sarang A, Lowndes C, Rylkov A, Khutorskoy M, Renton A. Situational factors influencing drug injecting, risk reduction and syringe exchange in Togliatti City, Russian Federation: a qualitative study of micro risk environment. Social Science & Medicine. 2003;57:39–54. doi: 10.1016/s0277-9536(02)00521-x. [DOI] [PubMed] [Google Scholar]
- Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Social Science & Medicine. 2005;61:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- Rockwell R, Des Jarlais DC, Friedman SR, Perlis TE, Paone D. Geographic proximity, policy and utilization of syringe exchange programmes. AIDS Care. 1999;11:437–442. doi: 10.1080/09540129947811. [DOI] [PubMed] [Google Scholar]
- SAS Institute . SAS/STAT 9.2. SAS Institute; Cary, NC: 2008. [Google Scholar]
- Shannon K, Rusch M, Shoveller J, Alexson D, Gibson K, Tyndall M, The Maka Project Partnership Mapping violence and policing as an environmental–structural barrier to health service and syringe availability among substance-using women in street-level sex work. International Journal of Drug Policy. 2008;19:140–147. doi: 10.1016/j.drugpo.2007.11.024. [DOI] [PubMed] [Google Scholar]
- Sherman LW. Police crackdowns: Initial and residual deterrence. Crime and justice: A review of research. 1990;12:1–48. [Google Scholar]
- Shields N, Nadasen K, Pierce L. The effects of community violence on children in Cape Town, South Africa. Child Abuse and Neglect. 2008;32:589–601. doi: 10.1016/j.chiabu.2007.07.010. [DOI] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. Oxford University Press; New York City: 2003. [Google Scholar]
- Small W, Kerr T, Charette J, Schechter M, Spittal P. Impacts of intensified police activity on injection drug users: evidence from an ethnographic investigation. International Journal of Drug Policy. 2006;17:85–95. [Google Scholar]
- Strathdee SA, Lozada R, Pollini R, Brouwer KC, Mantsios A, Abramovitz DA, Rhodes T, Latkin C, Loza O, Alvelias J, Magis-Rodriguez C, Patterson TL. Individual, social, and environmental influences associated with HIV infection among injection drug users in Tijuana, Mexico. JAIDS. 2008;47:369–376. doi: 10.1097/QAI.0b013e318160d5ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sumartojo E. Structural factors in HIV prevention: concepts, examples, and implications for research. AIDS. 2000;14:S2–S10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- Tempalski B. Placing the Dynamics of Syringe Exchange Programs in the United States. Health and Place. 2007;13:417–431. doi: 10.1016/j.healthplace.2006.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Cooper HL, Friedman SR, Des Jarlais DC, Brady JE, Gostnell K. Correlates of syringe coverage for heroin injection in 35 large metropolitan areas in the US in which heroin is the dominant injected drug. International Journal of Drug Policy. 2008;19:S47–S58. doi: 10.1016/j.drugpo.2007.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, Friedman R, Keem M, Cooper H, Friedman SR. NIMBY localism and national inequitable exclusion alliances: The case of syringe exchange programs in the United States. Geoforum. 2007;38:1250–1263. doi: 10.1016/j.geoforum.2007.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tempalski B, McQuie H. Drugscapes and the role of place and space in injection drug use-related HIV risk environments. International Journal of Drug Policy. 2009;20:4–13. doi: 10.1016/j.drugpo.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The New York State AIDS Advisory Council . Report on Syringe Access in New York State. The New York State AIDS Advisory Council; New York City: 2005. [Google Scholar]
- Tonry M. Race and the War on Drugs. Vol. 25. University of Chicago Legal Forum; 1994. pp. 25–81. [Google Scholar]
- U.S. Census Bureau . Statistical brief: Poverty areas. Washington, DC: 1995. [Google Scholar]
- UNAIDS High Coverage Sites: HIV Prevention among Injecting Drug Users in Transitional and Developing Countries: Case Studies, UNAIDS Best Practice Collection. 2006.
- UNAIDS, Geneva. United Hospital Fund . UHF Health Atlas. United Hospital Fund; New York City: 2005. [Google Scholar]
- US Congress . Consolidated Appropriations Act of 2010, PL111–117. In: US Congress, editor. US Federal Bureau of Investigation, 2010. Drug and Crime Facts: Drug Law Enforcement. FBI; Washington, DC: 2009. [Google Scholar]
- Valente T, Foreman R, Junge B, Vlahov D. Satellite Exchange in the Baltimore Needle Exchange Program. Public Health Reports. 1998;113:90–96. [PMC free article] [PubMed] [Google Scholar]
- Villano SA, Vlahov D, Nelson K, Lyles CM, Cohn S, Thomas DL. Incidence and Risk Factors for Hepatitis C among Injection Drug Users in Baltimore, Maryland. Journal of Clinical Microbiology. 1997;35:3274–3277. doi: 10.1128/jcm.35.12.3274-3277.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Junge B, Brookmeyer RS, Cohn S, Riley E, Armenian H, Beilenson P. Reductions in high-risk drug use behaviors among participants in the Baltimore Needle Exchange Program. JAIDS. 1997;16:400–406. doi: 10.1097/00042560-199712150-00014. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Sullivan M, Astemborski J, Nelson K. Bacterial infections and skin cleaning prior to injecting among intravenous drug users. Public Health Reports. 1992;5:595–598. [PMC free article] [PubMed] [Google Scholar]
- Wei M, Ku T-Y, Russell D, Liao KY-H, Mallinckrodt B. Moderating Effects of Three Coping Strategies and Self-Esteem on Perceived Discrimination and Depressive Symptoms: A Minority Stress Model for Asian International Students. Journal of Counseling Psychology. 2008;55:451–462. doi: 10.1037/a0012511. [DOI] [PubMed] [Google Scholar]
- WHO . Guide to starting and managing needle and syringe programmes. WHO; Geneva: 2007. [Google Scholar]
- Williams C, Metzger D. Race and Distance Effects on Regular Syringe Exchange Program Use and Injection Risks: A Geobehavioral Analysis. American Journal of Public Health. 2010;100:1068–1074. doi: 10.2105/AJPH.2008.158337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood E, Kerr T, Small W, Jones J, Schechter M, Tyndall M. The impact of police presence on access to needle exchange programs. JAIDS. 2003;34:116–118. doi: 10.1097/00126334-200309010-00019. [DOI] [PubMed] [Google Scholar]
- Wood E, Spittal P, Small W, Kerr T, Li K, Hogg R, Tyndall M, Montaner J, Schechter M. Displacement of Canada's largest public illicit drug market in response to a police crackdown. CMAJ Canadian Medical Association Journal. 2004;170:1551–1556. doi: 10.1503/cmaj.1031928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Effectiveness of sterile needle and syringe programming in reducing HIV/AIDS among injecting drug users. In: Organizatio WH, editor. Evidence for Action Technical Papers. World Health Organization; Geneva: 2004. p. 54. [Google Scholar]
- Zimmer L. Proactive Policing Against Street-Level Drug Trafficking. American Journal of Police. 1990;9:43–74. [Google Scholar]