Abstract
Reverse genetics viruses for influenza vaccine production usually utilize the internal genes of the egg-adapted A/Puerto Rico/8/34 (PR8) strain. This egg-adapted strain provides high production yield in embryonated eggs but does not necessarily give the best yield in mammalian cell culture. In order to generate a reverse genetics viral backbone that is well-adapted to high growth in mammalian cell culture, a swine influenza isolate (A/swine/Iowa/15/30 (H1N1) (rg1930) that was shown to give high yield in Madin-Darby Canine Kidney (MDCK) cells was used as the internal gene donor for reverse genetics plasmids. In this report, the internal genes from rg1930 were used for construction of reverse genetics viruses carrying a cleavage site-modified hemagglutinin (HA) gene and neuraminidase (NA) gene from a highly pathogenic H5N1 virus. The resulting virus (rg1930H5N1) was low pathogenic in vivo. Inactivated rg1930H5N1 vaccine completely protected chickens from morbidity and mortality after challenge with highly pathogenic H5N1. Protective immunity was obtained when chickens were immunized with an inactivated vaccine consisting of at least 29 HA units of the rg1930H5N1 virus. In comparison to the PR8-based reverse genetics viruses carrying the same HA and NA genes from an H5N1 virus, rg1930 based viruses yielded higher viral titers in MDCK and Vero cells. In addition, the reverse genetics derived H3N2 and H5N2 viruses with the rg1930 backbone replicated in MDCK cells better than the cognate viruses with the rgPR8 backbone. It is concluded that this newly established reverse genetics backbone system could serve as a candidate for a master donor strain for development of inactivated influenza vaccines in cell-based systems.
Keywords: Influenza A virus, avian influenza virus subtype H5N1, reverse genetics vaccine, cell-based vaccine, vaccine efficacy
Introduction
Influenza A virus is classified in genus Influenzavirus A, family Orthomyxoviridae. It infects various animal species such as humans, birds, dogs, seals, horses, and swine [1]. Emergence of new subtypes in human and animals may result in pandemic or panzootic diseases. Highly pathogenic avian influenza (HPAI) virus subtype H5N1 is the most recognized panzootic influenza thus far. The virus was initially reported in poultry and humans in Hong Kong in 1997 [2]. Re-emerging of the HPAI virus (H5N1) in late 2003 caused several severe outbreaks in East and South-East Asia. Genetic analysis revealed that HA gene of the HPAI viruses which emerged in 1997 and 2003 had a common ancestor which is closely related to an avian influenza virus from Southern China, the A/Goose/ Guangdong/1/1996 H5N1 virus. In May 2005, a new strain of the H5N1 HPAI virus emerged and caused an outbreak in migratory waterfowl at Qinghai Lake in China [3]; this new strain rapidly spread to several countries in Central Asia, Middle East, Europe and Africa [4, 5]. Although the HPAI H5N1 virus is presently only endemic in Asia and the Middle East, it still poses a significant zoonotic and pandemic threat as many human cases are reported to the WHO each year [6]. In addition, the HPAI H5N1 virus outbreak in 2011 in countries where the virus was previously eradicated, such as Japan and Korea [5], indicates re-emerging and panzootic capabilities of this virus. Therefore, it is essential for countries which are topographically close to countries endemic for H5N1 to monitor the occurrence of the HPAI H5N1 virus and have an effective control and eradication strategy in place.
An effective control strategy for the HPAI consists through a combination of various measurements including culling of infected and exposed animals, strengthening of biosecurity and prohibiting animal movement. In addition, in regions with high density of poultry, vaccination is an important measure which increases the effectiveness of the outbreak control [7, 8]. Hong Kong SAR implemented massive vaccination in combination with strengthening biosecurity and culling of infected birds which lead to a successful control of the disease [9, 10]. In an emergency control strategy, vaccination may be used to immunize poultry in the periphery of an outbreak region in combination with stamping out of the affected poultry. In addition, in an endemic area, appropriate vaccination could decrease the viral load in the environment which in turn would decrease transmission of the H5N1 viruses to other animals and humans [11]. In such circumstances, an efficacious vaccine is indispensable.
Various vaccines against HPAI H5N1viruses have been developed including heterologous killed vaccine [12], Fowl pox-based vector vaccine [13] and reverse genetics-based inactivated vaccines [12, 14-17]. The reverse genetics-based inactivated vaccines were very effective in preventing chickens from clinical signs and death because the reverse genetics derived seed viruses contained the homologous protective HA and NA antigens and possessed the ability to grow to high titer in embryonated chicken eggs. Reverse genetics-based viruses developed thus far contained the six internal genes derived from A/PR/8/34 [12, 14, 16-17], A/WSN/33 [15] and the HPAI H5N1 virus [18]. Most of them could replicate very well in embryonated chicken eggs. However, the supply of specific pathogen free (SPF) embryonated eggs for vaccine production may be limited, especially during an influenza pandemic period [19]. In addition, it takes at least six months for additional SPF eggs to be produced [20] if you have to start a new brood of layer hens. Thus, a reverse genetics-based virus that can be grown to high titers in cell cultures would be an alternative approach for vaccine production during a shortage of SPF eggs.
The first ever cultivated influenza A virus was isolated in 1930 from pigs with respiratory signs, and called A/swine /Iowa/15/1930 [21]. A serological study showed that the swine virus was closely related to the concurrent human influenza virus [22]. The 1930 swine virus might have been introduced into the swine population after the 1918 pandemic outbreak in the Midwest of the United States [23]. Recent phylogenetic analysis revealed that A/swine /Iowa/15/1930 and the first reported human influenza virus (A/PR/8/1934) originated from the pandemic 1918 influenza virus [24]. This information suggested a genetic and antigenic relatedness between A/swine /Iowa/15/1930 and A/PR/8/1934, the latter one being the donor strain for most reverse genetics-based influenza virus vaccines. Importantly, a study on growth characteristics of both viruses in MDCK cells demonstrated that the swine virus grew to significantly higher titers than the human virus (by at least 1 log10; unpublished data). Thus, it appears that the A/swine /Iowa/15/1930 virus may be an alternative backbone to generate reverse genetics based viruses for cell-culture grown vaccines.
This study aimed to generate a reverse genetics derived virus based on the rg1930 internal genes and the envelope proteins of an H5N1 virus (rg1930H5N1) that replicates efficiently in cell lines and can be used for vaccine production. The pathogenic characteristics of the rg1930H5N1 virus were determined in vitro and in vivo. In addition, growth characteristic of the rg1930H5N1 virus in MDCK and Vero cells was compared to that of viruses with A/PR/8/1934 internal genes. Finally, safety, efficacy and potency tests of the rg1930H5N1 vaccine in the chickens were evaluated.
Materials and Methods
1. Viruses
The influenza viruses used in this study are briefly described here. A/swine/Iowa/15/1930 (H1N1) RNA was amplified and cloned into a bidirectional transcription vector, pDZ (kindly provided by Prof. Dr. Adolfo Gracia Sastre at Mount Sinai School of Medicine, New York, USA), to produce eight reverse genetics plasmids, called rg1930. Six internal genes of the rg1930 were used as the reverse genetics backbone for the generation of a virus containing HA and NA genes of avian influenza virus (H5N1), designated rg1930H5N1. All eight genes of A/PR/8/1934 (H1N1) cloned into pHW2000, kindly provided by Drs. Hoffmann and Webster at St. Jude’s Children Hospital, Memphis, TN, USA, were included in this study for comparison as the reference reverse genetics backbone (rgPR8); six of the genes were used in various studies as the internal genes for reverse genetics-based avian influenza vaccines. A/chicken/Thailand/KU14/2004 (H5N1) was the donor for the HA and NA genes (accession numbers JN634875 and JN634876) to generate a reverse genetics derived virus with the six 1930 internal backbone, rg1930H5N1, for the production of the vaccine against avian influenza viruses (rg1930H5N1 vaccine). A/chicken/Thailand (Bangkok)/vsmu-3/2004 (H5N1) was a highly pathogenic avian influenza virus used to challenge the chickens in the virulence and efficacy tests. A/Thailand/Kan1/2004 (H5N1) was isolated from a patient infected with the avian influenza virus during the first outbreak in Thailand. It was the donor for the HA and NA genes for the reverse genetics virus with PR8 backbone, rgPR8H5N1. Both H5N1 viruses are genetically similar to A/chicken/Thailand/KU14/2004 (H5N1). A/swine/Thailand/KU5.1/2005 (H3N2) is a swine virus isolated from a pig with respiratory signs and was the HA and NA donors to generate the reverse genetics viruses subtype H3 and N2 in this study.
2. Cloning of viral genes
Total RNA was isolated from allantoic fluid containing highly pathogenic avian influenza (HPAI) virus subtype H5N1, A/chicken/Thailand/KU14/2004 (KU14), swine influenza virus (SIV) subtype H1N1, A/swine/IA/15/1930 (1930), or SIV subtype H3N2, A/swine/Thailand/KU5.1/2004 (5.1), using Trizol reagent (Invitrogen) and cDNA was synthesized using universal primers [25] and superscript III (Invitrogen) following the manufacturer’s protocol. The PCR was performed using primers specific to each gene of influenza A virus [25, 26] with SapI recognition site at both 3’ and 5’ ends of the primers. SIV 1930, SIV KU 5.1 and HPAIV KU14 cDNAs were used as the templates for amplification of HA and NA genes for the production of the reverse genetics viruses as shown in Supplemental Table 1. The nucleotides, AGAAAAAAGAGA, encoded for polybasic amino acids at the cleavage site were removed from the HA gene of HPAIV KU14 during PCR amplification using the fusion PCR technique with the two pairs of primers [12]. The PCR cloning of HA and NA genes of Kan 1 virus was performed similar to those of KU14 and the polybasic amino acids were deleted from the HA gene. PB2, PB1, PA, NP, M and NS genes were amplified from SIV 1930 cDNA in which the restriction enzyme markers were introduced into each gene using fusion PCR as published previously [27]. BspEI was introduced into PB2 and NP genes while XmaI, BamHI, SacI and XhoI were introduced into PB1, PA, M and NS genes, respectively.
3. Transfection and virus rescue
Transfection of eight plasmids was performed as previously described [28]. Briefly, 1 μg of each of eight plasmids (Supplemental Table 1) was mixed with TransIT (Mirus) and OptiMEM (Invitrogen) prior to gently dripping onto the monolayer of the MDCK-293T cells (kindly provided by Dr. Richard Webby at St. Jude Children’s Research Hospital, TN, USA) and incubating at 37°C with 5% CO2. The collected supernatant from the transfected cells was inoculated into the allantoic cavity of two 10-day-old embryonated chicken eggs and a monolayer of overnight seeded MDCK cells. Both inoculated embryonated chicken eggs and MDCK cells were incubated at 37°C for 72 hours before the rescued viruses were harvested. Each gene of the rescued viruses was verified by partial sequencing.
4. Growth curve determination
MDCK or Vero cells (kindly provided by Dr. Suthee Yoksan at Mahidol University, Thailand) were seeded in each well of the 6-well plates and incubated overnight at 37°C with 5% CO2. Each reverse genetics-derived virus was inoculated onto the monolayer of cells in five wells, five replicates, at MOI of 0.01. The supernatant from the infected cells was collected every 8-12 hour interval and kept at -80°C until needed. The supernatant was collected for 12 time points or until more than 90% of infected cells were dead. The titer of each sample was determined by inoculation of the ten-fold serially-diluted supernatant onto a monolayer of MDCK or Vero cells in the 96 well plates. The infectivity of the virus in each well was confirmed by immunoperoxidase monolayer assay (IPMA) [26, 29]. The titers were calculated as described by Reed and Muench [30]. The mean titers of the viruses at each time point were compared using the procedure of Generalized Linear Model (SAS version 9.2).
5. Plaque assay
The rg1930H5N1 virus was ten-fold serially diluted in MEM. A monolayer of MDCK cells in 6-well plates was inoculated with 0.5 ml of each dilution of rg1930H5N1 virus in the maintenance medium with or without trypsin. The viruses were allowed to attach to the cells for one hour. The viruses were removed and the media was replaced with 2.5 ml of the maintenance medium containing 0.9% agarose (Cambrex) with or without trypsin. The plates were incubated at 37°C with 5% CO2 for 72 hours. The plaques were stained by overlaying the first layer with MEM containing 0.9% agarose and 0.006% neutral red.
6. Vaccine preparation
The rg1930H5N1 virus was inoculated into the allantoic cavity of 10-day-old embryonated chicken eggs at 105 EID50. Eggs were incubated at 37°C for 48 hours before the allantoic fluid was collected. The virus was inactivated in formalin buffer at the final concentration of 0.2% at 4°C. The rg1930H5N1 virus was clarified by centrifugation at 5,000 rpm for 15 minutes. The titer of the virus was determined by hemagglutination (HA) assay [31]. The formalin treated rg1930H5N1 virus was tested for complete loss of the infectivity by inoculation into 10-day-old embryonated eggs for three passages. The virus was adjusted to have the final concentration of 210 HA units per dose before mixed with equal volume of Montanide-based oil emulsion.
7. Virulence test
The virulence test was performed by following the protocol provided in the OIE Terrestrial Manual [32]. Briefly, twenty 5-week-old specific pathogen free (SPF) chickens were assigned into two groups of 10 animals (Supplemental Table 2). The chickens in the first group were inoculated with 5×105 TCID50 of live rg1930H5N1 virus intravenously. The chickens in groups 2 were inoculated with similar amount of live wild type (wt) HPAIV, A/chicken/Thailand (Bangkok)/vsmu-3/2004 (H5N1), intravenously. The chickens were kept in the separated isolators within an animal biosafety level 3 (ABSL3) facilities at Mahidol University for 10 days. Lung, liver, spleen and intestine were collected from each animal at necropsy. The organs were minced and the tissue suspension was inoculated onto overnight grown MDCK cells in the maintenance media with trypsin. The supernatant from inoculated cells was passed in MDCK cells for three times. The pathogenic index was ranged from 0.00 to 3.00 as described in the OIE Terrestrial Manual [32]. A virus is considered as highly pathogenic when at least 7 out of 10 birds die from intravenous inoculation and the pathogenic index is equal or more than 1.2.
8. Efficacy test
Thirty-six White Leghorn SPF chickens were divided into three groups, 12 animals each; 1) mock and no challenge, 2) mock and challenge and 3) vaccine and challenge (Supplemental Table 2). The chickens in each group were housed separately. At 3-week-old, 24 chickens in groups 1 and 2 were mock injected intramuscularly with 0.5 ml normal saline and served as negative and challenge controls, respectively. Twelve chickens were vaccinated once with one dose of the rg1930H5N1 vaccine. At three week post vaccination, 12 chickens with mock injection and 12 chickens in vaccinated groups were moved to the ABSL3 facility and challenged intratracheally with 10 EID50 of the HPAI, A/chicken/Thailand (Bangkok)/vsmu-3/2004 (H5N1). Chickens were euthanized for necropsy at 14 days post inoculation (pi.) or when determined moribund. Oropharyngeal and cloacal swabs of the chickens were collected at 3, 7 and 14 days pi for virus isolation. Trachea, lung lobe, liver, spleen and intestine were collected for viral isolation at necropsy.
9. Potency test
The potency test was performed in two chicken flocks, 50 chickens in each flock. These chickens were hatched from non-vaccinated hens and they were negative for antibodies to HPAIV H5N1 prior to vaccination as examined by hemagglutination inhibition (HI) assay. At three week old, 50 chickens in each flock were assigned into five groups, 10 chickens in each group (Supplemental Table 3). The chickens were vaccinated with full (group 1), half (group 2), 1/4 (group 3) or 1/10 (group 4) dose of the rg1930H5N1 vaccine. The chickens in group 5 were left unvaccinated but injected with PBS and adjuvant as a negative control. The chickens in all groups were bled on the vaccination day and every week after vaccination for 5 weeks and at 20 weeks post vaccination. The blood was centrifuged at 2,000 rpm for 30 minutes and the sera were tested for the antibodies specific to the rg1930H5N1 virus by the mean of HI [31]. The HI titers to the H5N1 virus were observed weekly for 5 weeks and at 20 weeks post vaccination. The data from each flock was collected and combined for analysis. The geometric means of HI titers were determined and plotted. The HI titer of equal or more than 24 is considered as protective titer [16]. In addition, the differences of overall mean HI titers between each group were analyzed using the repeated measurement method from Generalized Linear Model procedure (SAS version 9.2).
Results
1. Establishment and characteristics of rg1930H5N1 virus
The 6 internal genes of A/swine/IA/15/1930 (rg1930) and the HA and NA genes of A/chicken/Thailand KU14/2004, all cloned in the pDZ vector, were transfected into a 293T/MDCK cell culture mix. Viable virus was obtained and the biological properties of the rg1930H5N1 virus were further characterized by inoculation onto a monolayer of overnight grown MDCK cells and 10-day-old embryonated chicken eggs. The virus produced cytopathic effect (CPE) within 24 hours in MDCK cells and yielded the titer of 1×109 TCID50/ml in 48 hours pi. The virus did not kill the embryo and the allantoic fluid collected from the inoculated eggs at 72 hours pi had a titer of 1×109 TCID50/ml and an HA titer of 211HA units. In addition, MDCK cells inoculated with the rescued rg1930H5N1 virus reacted strongly to monoclonal antibodies to NP as detected by IPMA confirming that the rg1930H5N1 virus replicated well in cell culture. Subsequently, total RNA was extracted from the allantoic fluid containing the rg1930H5N1 virus and used for cDNA synthesis and PCR amplification of all eight genes. The purified full length HA and NA DNAs were sequenced while the PCR products of other genes were digested with appropriated restriction enzymes. The sequencing results showed that HA and NA genes of the rg1930H5N1 are 100% identical to the original cDNA clones derived from A/chicken/Thailand/KU14/2004 (H5N1). Importantly, the nucleotides coding for the polybasic amino acids at the HA cleavage site were deleted as expected (Supplemental Fig. 1). Restriction analysis demonstrated that PB2, PB1, PA, NA, M and NS genes of rg1930H5N1 contained the introduced restriction enzyme markers (Data not shown).
To determine trypsin dependent characteristics of rg1930H5N1 virus, the rescued virus was inoculated onto a monolayer of MDCK cells covered with agar containing 1 μg/ml trypsin or without trypsin. After 48 hours pi, plaques were observed in wells containing agar with trypsin but not in wells without trypsin. The results indicated that the rg1930H5N1 virus required trypsin for its infectivity (Supplemental Fig. 2). Thus, in vitro results demonstrated that the rg1930H5N1 virus possesses non-virulent characteristics.
2. Virulence test of rg1930H5N1virus
To examine the pathogenic index of rg1930H5N1 virus, 10 five-week-old chickens were inoculated intravenously with live rg1930H5N1 or live wt HPAIV H5N1 in the ABSL3 facility. All chickens inoculated with the wt virus were very sick and died within 48 hours. The chickens in the rg1930H5N1 group were normal until 5 days pi. At 6 days pi, three chickens in this group were sick and one died on day 7. The remaining chickens were normal and were necropsied at 10 days pi. When the sick and dead animals were included, the pathogenic index for the rg1930H5N1 virus was 0.26 which was considered as low-pathogenic virus. If the sick/dead animals were not included, the pathogenic index for the rg1930H5N1 was 0.00.
To reveal the causative agent, tissue suspension from lung, liver, spleen, and intestine from sick and dead chickens was inoculated onto MDCK cells for three passages. The virus isolation of every sample in all three passages showed negative results indicating that the rg1930H5N1 was not the direct cause of the sickness. The frozen tissues of the dead chicken as well as oropharyngeal and cloacal swabs of the sick chickens were submitted to Veterinary Diagnostic Laboratory for the detection of New Castle disease virus, infectious bronchitis virus and infectious bursal disease virus by RT-PCR and pathogenic bacteria by bacterial culture. RT-PCR results of the three viruses were negative. In addition, pathogenic bacteria were not detected in all swab samples. However, E.coli was observed in the mixed organ culture. Therefore, colibacillosis might be the cause of the illness. However, E.coli is the normal flora in the chicken intestine and intestine was also included in the mix organs used for bacterial culture.
3. Efficacy test of rg1930H5N1 vaccine
The protective efficacy of the rg1930H5N1 vaccine was determined in 3-week-old chickens. Thirty-six chickens were divided in to three groups of twelve, vaccination control, challenge control and vaccination-challenge. As positive controls, twelve non-vaccinated chickens were challenged with wt HPAIV H5N1 and died within 48 hours. Inoculation of 10% tissue homogenates from lung, liver, intestine and spleen from each chicken in this group revealed positive results on first passage on MDCK cells. As negative controls, twelve chickens were mock vaccinated and not challenged and remained normal throughout the observation period. Also, the oropharyngeal and cloacal swabs as well as tissue homogenates from lung, liver, intestine and spleen were negative when inoculated onto MDCK cells for three passages. Similarly to the negative control group, all chickens in the vaccinated and challenged group survived and no clinical signs were detected during 14 days of observation (Table 1). The oropharyngeal and cloacal swabs as well as organs were inoculated onto MDCK cells for three passages. All samples were found to be negative in the first passage. The oropharyngeal swabs collected at 3 days pi from seven chickens (n=12), a cloacal swab from one chicken (n=12) and lung suspension from two chickens (n=12) in this group were positive in the second passage on MDCK cells. The remaining swabs and tissue suspensions were negative for viral isolation after three passages in MDCK cells.
Table 1.
Results of efficacy test with numbers of sick and dead chickens and numbers of chickens positive in viral isolation performed in MDCK cells for three passages
| Groups | No. sick | No. dead | Oropharyngeal swab | Cloacal swab | Lung | Liver | Intestine | Spleen |
|---|---|---|---|---|---|---|---|---|
| Control | 0/12 | 0/12 | 0 | 0 | 0 | 0 | 0 | 0 |
| Challenge | 12/12 | 12/12 | N/D | N/D | 12/12; P1 | 12/12; P1 | 12/12; P1 | 12/12; P1 |
| Vaccination + challenge | 0/12 | 0/12 | 7/12; D3; P2 | 1/12; D3;P2 | 2/12; P2 | 0/12 | 0/12 | 0/12 |
Note: Nominator is the number of affected samples. Denominator is the number of tested samples. D represents days pi and P is passage of viruses in MDCK cells. N/D = not done.
4. Potency test of rg1930H5N1 vaccine
The ability of the rg1930H5N1 to induce virus-specific immune responses was determined via immunization of 100 chickens with various doses of the rg1930H5N1 vaccine (Supplemental Table 3); antibody responses to the virus were observed weekly for the duration of 5 weeks. The results of the geometric mean HI titers are demonstrated in figure 1. Antibodies to the virus were first detected in some of the vaccinated chickens in the first week after vaccination. After two weeks post vaccination, the HI titers of chickens in all vaccinated groups were significant higher than those in the non-vaccinated control group (P<0.001). Antibodies directed against the H5N1 virus increased dramatically in the third week post vaccination. At week 4 and 5 post vaccination, HI titers of the chickens vaccinated with full and half doses were significantly higher than those of the other 2 groups (P<0.001). Additionally, HI titers of the chickens in the full and half-dose groups were above a generally considered protective HI level of 24 [16] at three weeks post vaccination and remained at the protective level (25) until 20 weeks post vaccination, the last week of the study period. However, the chickens vaccinated with ¼ and 1/10 doses of the vaccine produced antibodies to the H5N1 virus but the average antibody titers were around or lower than the protective level.
Figure 1.
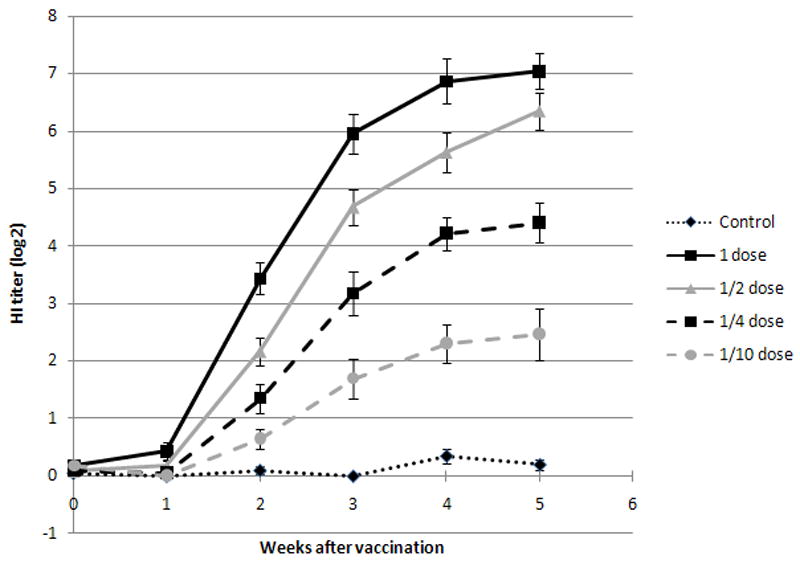
Plot of geometric means demonstrating HI titers of chickens vaccinated with different doses of rg1930H5N1 vaccine.
5. Genetic stability of rg1930H5N1
To examine genetic stability of rg1930H5N1 virus, the virus was passed in 10-day old embryonic chicken eggs for 10 passages. The total RNA was isolated from the allantoic fluid at passage 10th and used as the template for cDNA synthesis. Each gene was amplified using gene specific primers as described previously. The PCR products were sequenced and the DNA sequences of eight gene segments were compared with the original plasmids used for transfection. The results showed that the rg1930H5N1virus is stable since no nucleic acid mutation was found within the HA and NA genes and the novel restriction sites were maintained within the internal genes. In addition, at passage 10th, there is no insertion of codons in the putative cleavage site within HA gene indicating that its non-virulent characteristics were maintained.
6. Potential use of rg1930 as the backbone for seed virus vaccine
To determine the potential use of rg1930 for vaccine production, the six internal genes of rg1930 were combined with the HA and NA genes of different influenza subtypes (Supplemental Table 1). The results showed that PB2, PB1, PA, NP, M and NS genes of rg1930 were compatible to HA and NA genes of SIV H3N2 and avian H5 plus SIV N2 subtypes. Thus, rg1930H3N2 and rg1930H5N2 were successfully rescued from the transfected 293T-MDCK cells mixture and they all were infectious. Similarly, reverse genetics viruses consisting of six internal genes of PR8 and different HA and NA subtypes (Supplemental Table 1) were successfully generated. Subsequently, growth curves of the viruses containing either rg1930 or rgPR8 backbone were compared in MDCK cells or Vero cells. The results demonstrated that the reverse genetics H5N1 and H5N2 viruses containing rg1930 backbone (rg1930H5N1 and rg1930H5N2) replicated in MDCK cells at higher titer than the corresponding subtypes with PR8 backbone (rgPR8H5N1 and rgPR8H5N2) (P<0.001; Fig. 2). The rg1930H3N2 and rgPR8H3N2 replicated in MDCK cells at similar rate. In addition, when a one step growth curve was performed in Vero cells, rg1930H5N1 replicated much more efficiently than the reverse genetics virus containing six internal genes of PR8 (P<0.001) (Fig. 3).
Figure 2.
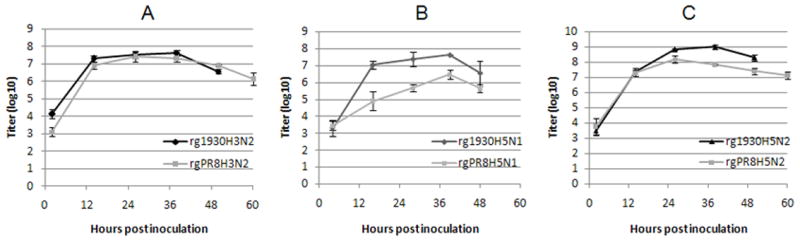
Growth curves of rg1930H3N2 versus rgPR8H3N2 (A), rg1930H5N1 versus rgPR8H5N1 (B) and rg1930H5N2 versus rgPR8H5N2 (C) in MDCK cells.
Figure 3.
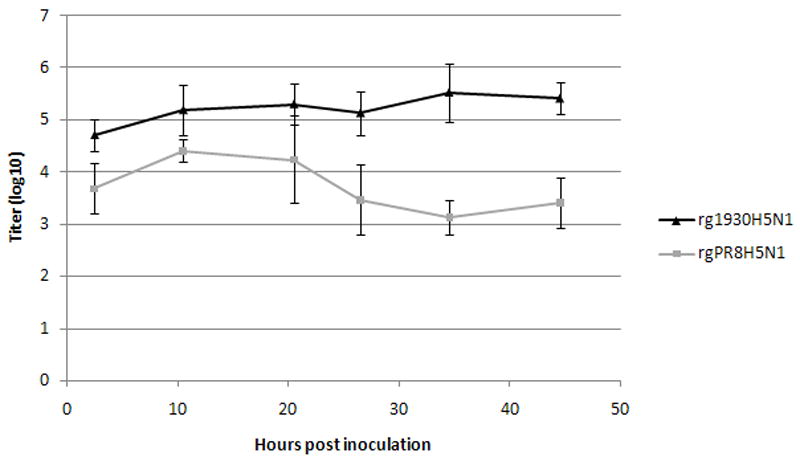
Growth curves of rg1930H5N1 and rgPR8H5N1 viruses in Vero cells. rg1930H5N1 virus replicated in Vero cells at higher titer than rgPR8H5N1 (P<0.001).
Discussions
Since emerging in 1997, the HPAI H5N1 viruses have continually evolved into 10 clades and multiple subclades [33]. The different genotypes of the H5N1 viruses are generated by reassortment with other avian influenza viruses in Southern China [34-36] while antigenic diversity among each clade results from accumulation of point mutations within the HA gene, so called genetic drift [37]. The ancestor virus, A/Goose/ Guangdong /1/1996, and closely related viruses are assigned as clade 0. The viruses that spread to Vietnam, Thailand and Malaysia during 2003-2004 panzootic wave are in clade 1; viruses that caused the outbreak in Indonesia are in clade 2, subclade 2.1; the 2005 Qinghai panzootic viruses are in clade 2, subclade 2.2 and 2.2.1 [3, 38]. The Fujian-like viruses that caused the outbreaks in domestic poultry in South China, Vietnam, Loa PDR and Thailand in 2005 are clustered in clade 2, subclade 2.3.4 [35, 38-39]. The viruses that have been endemic in Hong Kong and Vietnam since 2005 are in subclade 2.3.2 [33, 38]. Other additional clades are found only in Southern China [33, 36]. Thus, Southern China is considered as the primary epicenter for continual generation of new strains of H5N1 viruses that are ready to be spread to other regions of the world. Recent evidence also indicates that Indonesia, Egypt and Nigeria might be secondary H5N1 epicenters [37].
As avian influenza virus H5N1 is endemic and/or re-emerged in some countries, development or improvement of novel seed virus for vaccine production is needed. Most if not all reverse genetics-based avian influenza virus vaccines utilize 6 internal genes from A/PR8/1934 [12, 14-17]. These vaccines are safe and provide excellent protective immunity in animals. The reverse genetics-based HPAI (H5N1) vaccine developed in this study, rg1930H5N1, was also non-virulent in chicken and induced protective immunity similar to the previously reported reverse genetics H5N1 vaccines. Additionally, it contains a novel internal genetic backbone. Each gene of the rg1930 also contains restriction enzyme markers for easily monitoring during vaccine development process. Generally, to confirm the fidelity of the six internal genes, cDNA of the rescued virus would be sequenced. However, in this study, we can monitor internal genes of the rg1930 conveniently by treatment of each gene with the appropriated restriction enzyme instead of DNA sequencing.
It was clearly shown earlier that the vaccine with the most similarity of HA gene to the challenged avian influenza virus possessed the highest protection efficiency [40]. In addition, a challenge experiment with wild type HPAI H5N1 virus subclades 2.2 or 2.3 presently endemic in Egypt confirmed that only vaccines containing the homologous antigen completely protect chickens from virus shedding [41]. On the other hand, the vaccines with non-homologous antigens could not protect the vaccinated chickens efficiently [42]. Most reverse genetics derived, inactivated vaccines including the rg1930H5N1 vaccine in this study contained homologous HA to the HPAI H5N1 viruses. Thus, they protected chickens from morbidity and mortality [12, 14-16]. However, most of them did not provide a sterile immunity since some vaccinated chickens still shed virus after challenge with the wild type H5N1 viruses for 3-5 days. A meta-analysis found that homologous inactivated vaccines decreased the virus shedding in the challenge animals more efficiently than vector-based vaccines [43]. Particularly, the reverse genetics H5N3 vaccine containing the antigen equivalent to 1.2 μg HA completely protected chickens, geese and ducks from shedding [17].
In addition to antigenic similarity, concentration of antigen in the vaccine also determines the efficacy and potency of the vaccine [44] since each dose of vaccine requires high amount of the virus or antigen in limited volume such as 0.5 ml. Therefore, a virus with high growth characteristic which translates into high yield of antigen is essential for vaccine production. The rg1930H5N1 virus grew at high titer in both embryonated chicken eggs and MDCK cells. This study showed that each dose of the vaccine against HPAI H5N1 should contain at least 29 HA units of the virus to elicit the protective immune responses within three weeks and the protection lasts as long as 20 weeks, the last week of the experiment. When the vaccine was decreased to ¼ dose (virus titer was 28 HA units), HI titers of the vaccinated chickens were around the protective level, 24, and began to drop when reconfirmed at 20 week post vaccination. It would be possible that boosting with a similar dose of the vaccine may increase the HI titer to be above the protective level. This study therefore demonstrated that determination of the antigen content in a vaccine using HA units is feasible and most likely easier than other methods.
Apart from the amount of antigen, another essential composition for influenza vaccine production is the availability of SPF eggs. Most of influenza virus vaccines are produced in embryonated chicken eggs. However, resources of high quality, specific pathogen free (SPF), embryonated chicken egg may not be sufficient for vaccine production, especially when a huge number of vaccines are needed such as during a pandemic period [19]. Furthermore, it takes at least six months for clean egg preparation beginning from hatching the SPF chickens till laying eggs [20]. Thus, cell-based technology is considered for influenza vaccine production since cell lines can be of unlimited supply. MDCK and Vero cell lines appear to be suitable for vaccine production [45-46]. However, some of influenza A viruses including avian influenza viruses cannot grow well in mammalian cells. In this study, novel reverse genetics derived vaccine viruses with rg1930 internal genes were established in order to have vaccine viruses which can replicate very well not only in embryonated chicken eggs but also in MDCK and Vero cells. The subtype H5N1 and H5N2 viruses with six internal genes of the rg1930 replicated in MDCK cells better than those with rgPR8 backbone by at least 10 times.
The six internal genes of the rg1930 developed here are an efficient backbone for the production of both egg- and cell-based reverse genetics derived vaccines for the control of HPAI in animals. Each gene contains a novel restriction enzyme marker for easy monitoring. The six internal genes can accommodate various subtypes of HA and NA genes. The viruses containing the six internal genes of rg1930 replicate at similar or higher titers than those of PR8 in MDCK and Vero cells. The titer of the rg1930-based reverse genetics virus may be increased by exploring the conditions for viral growth such as optimal amount of cells and virus as well as incubation times. It is also possible to enhance the replication rate of this reverse genetics system in different cells used for vaccine production such as the novel MDCK cell lines (MDCK-SFS) [47]. This cell line retained high expression level of α-2, 6 and α-2, 3 sialic acid receptors and grew efficiently in suspension useful for large scale influenza virus vaccine production. Therefore, the six internal genes of rg1930 have a potential application for reverse genetics vaccine production using either egg- or cell-based vaccine technology.
Supplementary Material
Supplemental Figure 1 Nucleotide sequences encoding polybasic amino acids within the HA gene of rg1930H5N1 virus compared to the original plasmid used for transfection (pDZ_1930H5N1_HA) and the wild type A/chicken/Thailand/KU14/04 (H5N1).
Supplemental Figure 2 Trypsin dependent characteristics of rg1930H5N1. rg1930H5N1 could not produce plaque in the maintenance media without trypsin (A) while plaque formation occurred when the media was supplemented with TPCK treated trypsin (B).
Highlight.
>The novel 8 plasmid reverse genetics of influenza A virus, rg1930, was generated.
>Each gene contains the introduced genetic marker for easy monitoring.
>The 6 internal genes (backbone) of rg1930 accommodated various HA and NA subtypes.
>The rg1930 derived viruses grew better than those with widely used backbone (rgPR8).
>Efficacy and safety of rg1930- and rgPR8-based vaccines are similar.
Acknowledgments
This study was supported by Charoen Pokpan Foundation, National Center for Genetic Engineering and Biotechnology, BIOTEC THAILAND (grant number F-BT-RDE-08) and Kasetsart University Research and Development Institute, KURDI (grant number 5210471000/2552) through PL. This project was partially funded by the National Institute Allergy and Infectious Disease, National Institutes of Health, Department of Health and Human Services, under contract number HHSN266200700005C.
The authors appreciate Prof. Dr. Adolfo Garcia Sastre at Mount Sinai School of Medicine, NY, USA, for kindly providing pDZ; Prof. Dr. Robert Webster, Dr. Erich Hoffmann and Dr. Richard A Webby at St. Jude’s Children Hospital, TN, USA, for kindly providing the PR8 reverse genetics system, MDCK and 293T cells and Dr. Suthee Yoksan at Mahidol University, Thailand, for kindly providing Vero cells.
We thank Drs. Narin Romlumduan and Nittaya Suriyathongthum for their assistant in animal experiments as well as Ms Jutharat Lidjun and Mr. Natharat Thungthumniyom for technical assistant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Webster RG, Bean WJ, Gorman OT, Chamber TM, Kawaoka Y. Evolution and ecology of influenza A viruses. Microbiol Rev. 1992;56:152–79. doi: 10.1128/mr.56.1.152-179.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Jong JC, Claas EC, Osterhaus AD, Webster RG, Lim WL. A pandemic warning? Nature. 1997;389(6651):554. doi: 10.1038/39218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen H, Smith GJ, Zhang SY, Qin K, Wang J, Li KS, Webster RG, Peiris JS, Guan Y. Avian flu: H5N1 virus outbreak in migratory waterfowl. Nature. 2005;436(7048):191–2. doi: 10.1038/nature03974. [DOI] [PubMed] [Google Scholar]
- 4.Salzberg SL, Kingsford C, Cattoli G, Spiro DJ, Janies DA, Aly MM, Brown IH, Couacy-Hymann E, De Mia GM, Dung do H, Guercio A, Joannis T, Maken Ali AS, Osmani A, Padalino I, Saad MD, Savić V, Sengamalay NA, Yingst S, Zaborsky J, Zorman-Rojs O, Ghedin E, Capua I. Genome analysis linking recent European and African influenza (H5N1) viruses. Emerg Infect Dis. 2007;13(5):713–8. doi: 10.3201/eid1305.070013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Organization for Animal Health. Update on Highly Pathogenic Avian Influenza in Animals (Type H5 an H7) [2011 June 8]; Available from http://www.oie.int/en/animal-health-in-the-world/update-on-avian-influenza/2011/
- 6.WHO. Cumulative number of confirmed human cases of avian influenza A (H5N1) reported to WHO. [2011 May 5]; Available from http://www.who.int/crs/disease/avian_influenza/country/cases_table_2011_04_21/en/
- 7.Marangon S, Cristalli A, Busani L. Planning and executing a vaccination campaign against avian influenza. Dev Biol (Basel) 2007;130:99–108. [PubMed] [Google Scholar]
- 8.Pfeiffer DU, Otte MJ, Roland-Holst D, Inui K, Tung N, Zilberman D. Implications of global and regional patterns of highly pathogenic avian influenza virus H5N1 clades for risk management. Vet J. 2011 doi: 10.1016/j.tvjl.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 9.Sims LD, Guan Y, Ellis TM, Liu KK, Dyrting K, Wong H, Kung NY, Shortridge KF, Peiris M. An update on avian influenza in Hong Kong 2002. Avian Dis. 2003;47(3 Suppl):1083–6. doi: 10.1637/0005-2086-47.s3.1083. [DOI] [PubMed] [Google Scholar]
- 10.Ellis TM, Leung CY, Chow MK, Bissett LA, Wong W, Guan Y, Malik Peiris JS. Vaccination of chickens against H5N1 avian influenza in the face of an outbreak interrupts virus transmission. Avian Pathol. 2004;33(4):405–12. doi: 10.1080/03079450410001724012. [DOI] [PubMed] [Google Scholar]
- 11.Food and Agriculture Organization and World Organization for Animal Health in collaboration with World Health Organization. A global strategy for the progressive control of highly pathogenic avian influenza (HPAI) 2005 May; [Google Scholar]
- 12.Liu M, Wood JM, Ellis T, Krauss S, Seiler P, Johnson C, Hoffmann E, Humberd J, Hulse D, Zhang Y, Webster RG, Perez DR. Preparation of a standardized, efficacious agricultural H5N3 vaccine by reverse genetics. Virology. 2003;314(2):580–90. doi: 10.1016/s0042-6822(03)00458-6. [DOI] [PubMed] [Google Scholar]
- 13.Qiao CL, Yu KZ, Jiang YP, Jia YQ, Tian GB, Liu M, Deng GH, Wang XR, Meng QW, Tang XY. Protection of chickens against highly lethal H5N1 and H7N1 avian influenza viruses with a recombinant fowlpox virus co-expressing H5 haemagglutinin and N1 neuraminidase genes. Avian Pathol. 2003;32(1):25–32. doi: 10.1080/0307945021000070688. [DOI] [PubMed] [Google Scholar]
- 14.Subbarao K, Chen H, Swayne D, Mingay L, Fodor E, Brownlee G, Xu X, Lu X, Katz J, Cox N, Matsuoka Y. Evaluation of a genetically modified reassortant H5N1 influenza A virus vaccine candidate generated by plasmid-based reverse genetics. Virology. 2003;305(1):192–200. doi: 10.1006/viro.2002.1742. [DOI] [PubMed] [Google Scholar]
- 15.Lee CW, Senne DA, Suarez DL. Generation of reassortant influenza vaccines by reverse genetics that allows utilization of a DIVA (Differentiating Infected from Vaccinated Animals) strategy for the control of avian influenza. Vaccine. 2004;22(23-24):3175–81. doi: 10.1016/j.vaccine.2004.01.055. [DOI] [PubMed] [Google Scholar]
- 16.Tian G, Zhang S, Li Y, Bu Z, Liu P, Zhou J, Li C, Shi J, Yu K, Chen H. Protective efficacy in chickens, geese and ducks of an H5N1-inactivated vaccine developed by reverse genetics. Virology. 2005;341(1):153–62. doi: 10.1016/j.virol.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 17.Webster RG, Webby RJ, Hoffmann E, Rodenberg J, Kumar M, Chu HJ, Seiler P, Krauss S, Songserm T. The immunogenicity and efficacy against H5N1 challenge of reverse genetics-derived H5N3 influenza vaccine in ducks and chickens. Virology. 2006;351(2):303–11. doi: 10.1016/j.virol.2006.01.044. [DOI] [PubMed] [Google Scholar]
- 18.Horimoto T, Takada A, Fujii K, Goto H, Hatta M, Watanabe S, Iwatsuki-Horimoto K, Ito M, Tagawa-Sakai Y, Yamada S, Ito H, Ito T, Imai M, Itamura S, Odagiri T, Tashiro M, Lim W, Guan Y, Peiris M, Kawaoka Y. The development and characterization of H5 influenza virus vaccines derived from a 2003 human isolate. Vaccine. 2006;24(17):3669–76. doi: 10.1016/j.vaccine.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 19.Monto AS, Maassab HF, Bryan ER. Relative efficacy of embryonated eggs and cell culture for isolation of contemporary influenza viruses. J Clin Microbiol. 1981;13(1):233–5. doi: 10.1128/jcm.13.1.233-235.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gerdil C. The annual production cycle for influenza vaccine. Vaccine. 2003;21(16):1776–9. doi: 10.1016/s0264-410x(03)00071-9. [DOI] [PubMed] [Google Scholar]
- 21.Shope RE. Swine influenza. I. Experimental transmission and pathology. J Exp Med. 1931;54:349–59. doi: 10.1084/jem.54.3.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Francis T, Shope RE. Neutralization tests with sera of convalescent or immunized animals and the viruses of swine and human influenza. J Exp Med. 1936;63(5):645–53. doi: 10.1084/jem.63.5.645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shope RE. The incidence of neutralizing antibodies for swine influenza virus in the sera of human beings of different ages. J Exp Med. 1936;63(5):669–84. doi: 10.1084/jem.63.5.669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tumpey TM, Basler CF, Aguilar PV, Zeng H, Solórzano A, Swayne DE, Cox NJ, Katz JM, Taubenberger JK, Palese P, García-Sastre A. Characterization of the reconstructed 1918 Spanish influenza pandemic virus. Science. 2005;10(5745):77–80. doi: 10.1126/science.1119392. [DOI] [PubMed] [Google Scholar]
- 25.Hoffmann E, Stech J, Guan Y, Webster RG, Perez DR. Universal primer set for the full-length amplification of all influenza A viruses. Arch Virol. 2001;146(12):2275–89. doi: 10.1007/s007050170002. [DOI] [PubMed] [Google Scholar]
- 26.Lekcharoensuk P, Nanakorn J, Wajjwalku W, Webby R, Chumsing W. First whole genome characterization of swine influenza virus subtype H3N2 in Thailand. Vet Microbiol. 2010;145(3-4):230–44. doi: 10.1016/j.vetmic.2010.04.008. [DOI] [PubMed] [Google Scholar]
- 27.Ma W, Lager KM, Lekcharoensuk P, Ulery ES, Janke BH, Solórzano A, Webby RJ, García-Sastre A, Richt JA. Viral reassortment and transmission after co-infection of pigs with classical H1N1 and triple-reassortant H3N2 swine influenza viruses. J Gen Virol. 2010;91(Pt 9):2314–21. doi: 10.1099/vir.0.021402-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoffmann E, Krauss S, Perez D, Webby R, Webster RG. Eight-plasmid system for rapid generation of influenza virus vaccines. Vaccine. 2002;20(25-26):3165–70. doi: 10.1016/s0264-410x(02)00268-2. [DOI] [PubMed] [Google Scholar]
- 29.Nakharuthai C, Boonsoongnern A, Poolperm P, Wajjwalku W, Urairong K, Chumsing W, Lertwitcharasarakul P, Lekcharoensuk P. Occurrence of swine influenza virus in swine with respiratory disease complex. Southeast Asian J Trop Med Public Health. 2008;39(6):1045–53. [PubMed] [Google Scholar]
- 30.Reed LJ, Muench H. A simple method of estimating fifty percent endpoints. Am J Hyg. 1938;27:493–97. [Google Scholar]
- 31.Lekcharoensuk P, Lager KM, Vemulapalli R, Woodruff M, Vincent AL, Richt JA. Novel swine influenza virus subtype H3N1, United States. Emerging Infect Dis. 2006;12(5):787–94. doi: 10.3201/eid1205.051060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. [2011 June 8];OIE Terrestrial Manual 2009. Chapter 2.3.4. Avian Influenza. Available from http://oie.int/fileadmin/Home/eng/Animal-Health-in-the-world/docs/pdf/2.03.04_AI.pdf.
- 33.WHO. Antigenic and genetic characteristics of influenza A (H5N1) and influenza A (H9N2) viruses and candidate vaccine viruses developed for potential use in human vaccines. February 2011. [2011 June 8]; Available from http://www.who.int/csr/disease/avian_influenza/guidelines/h5n1virus/en/index.html. [PubMed]
- 34.Chen H, Smith GJ, Li KS, Wang J, Fan XH, Rayner JM, Vijaykrishna D, Zhang JX, Zhang LJ, Guo CT, Cheung CL, Xu KM, Duan L, Huang K, Qin K, Leung YH, Wu WL, Lu HR, Chen Y, Xia NS, Naipospos TS, Yuen KY, Hassan SS, Bahri S, Nguyen TD, Webster RG, Peiris JS, Guan Y. Establishment of multiple sublineages of H5N1 influenza virus in Asia: implications for pandemic control. Proc Natl Acad Sci USA. 2006;103(8):2845–50. doi: 10.1073/pnas.0511120103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith GJ, Fan XH, Wang J, Li KS, Qin K, Zhang JX, Vijaykrishna D, Cheung CL, Huang K, Rayner JM, Peiris JS, Chen H, Webster RG, Guan Y. Emergence and predominance of an H5N1 influenza variant in China. Proc Natl Acad Sci USA. 2006;103(45):16936–41. doi: 10.1073/pnas.0608157103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li KS, Guan Y, Wang J, Smith GJ, Xu KM, Duan L, Rahardjo AP, Puthavathana P, Buranathai C, Nguyen TD, Estoepangestie AT, Chaisingh A, Auewarakul P, Long HT, Hanh NT, Webby RJ, Poon LL, Chen H, Shortridge KF, Yuen KY, Webster RG, Peiris JS. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430(6996):209–13. doi: 10.1038/nature02746. [DOI] [PubMed] [Google Scholar]
- 37.Guan Y, Smith GJ, Webby R, Webster RG. Molecular epidemiology of H5N1 avian influenza. Rev Sci Tech. 2009;28(1):39–47. doi: 10.20506/rst.28.1.1868. [DOI] [PubMed] [Google Scholar]
- 38.WHO. Antigenic and genetic characteristics of influenza A (H5N1) and influenza A (H9N2) viruses and candidate vaccine viruses developed for potential use in human vaccines. February 2010. [2011 June 8]; Available from http://www.who.int/csr/disease/avian_influenza/guidelines/h5n1virus/en/index.html. [PubMed]
- 39.Suwannakarn K, Amonsin A, Sasipreeyajan J, Kitikoon P, Tantilertcharoen R, Parchariyanon S, Chaisingh A, Nuansrichay B, Songserm T, Theamboonlers A, Poovorawan Y. Molecular evolution of H5N1 in Thailand between 2004 and 2008. Infect Genet Evol. 2009;9(5):896–902. doi: 10.1016/j.meegid.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 40.Swayne DE, Perdue ML, Beck JR, Garcia M, Suarez DL. Vaccines protect chickens against H5 highly pathogenic avian influenza in the face of genetic changes in field viruses over multiple years. Vet Microbiol. 2000;74(1-2):165–72. doi: 10.1016/s0378-1135(00)00176-0. [DOI] [PubMed] [Google Scholar]
- 41.Grund C, Abdelwhab ES, Arafa AS, Ziller M, Hassan MK, Aly MM, Hafez HM, Harder TC, Beer M. Highly pathogenic avian influenza virus H5N1 from Egypt escapes vaccine-induced immunity but confers clinical protection against a heterologous clade 2.2.1 Egyptian isolate. Vaccine. 2011;29(33):5567–73. doi: 10.1016/j.vaccine.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 42.Kilany WH, Abdelwhab EM, Arafa AS, Selim A, Safwat M, Nawar AA, Erfan AM, Hassan MK, Aly MM, Hafez HM. Protective efficacy of H5 inactivated vaccines in meat turkey poults after challenge with Egyptian variant highly pathogenic avian influenza H5N1 virus. Vet Microbiol. 2011;150(1-2):28–34. doi: 10.1016/j.vetmic.2010.12.016. [DOI] [PubMed] [Google Scholar]
- 43.Hsu SM, Chen TH, Wang CH. Efficacy of avian influenza vaccine in poultry: a meta-analysis. Avian Dis. 2010;54(4):1197–209. doi: 10.1637/9305-031710-Reg.1. [DOI] [PubMed] [Google Scholar]
- 44.Webster RG, Peiris M, Chen H, Guan Y. H5N1 outbreaks and enzootic influenza. Emerg Infect Dis. 2006;12:3–8. doi: 10.3201/eid1201.051024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kistner O, Barrett PN, Mundt W, Reiter M, Schober-Bendixen S, Dorner F. Development of a mammalian cell (Vero) derived candidate influenza virus vaccine. Vaccine. 1998;16(9-10):960–8. doi: 10.1016/s0264-410x(97)00301-0. [DOI] [PubMed] [Google Scholar]
- 46.Ozaki H, Govorkova EA, Li C, Xiong X, Webster RG, Webby RJ. Generation of high-yielding influenza A viruses in African green monkey kidney (Vero) cells by reverse genetics. J Virol. 2004;78(4):1851–7. doi: 10.1128/JVI.78.4.1851-1857.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.vanWielink R, Kant-Eenbergen HC, Harmsen MM, Martens DE, Wijffels RH, Coco-Martin JM. Adaptation of a Madin-Darby canine kidney cell line to suspension growth in serum-free media and comparison of its ability to produce avian influenza virus to Vero and BHK21 cell lines. J Virol Methods. 2011;171(1):53–60. doi: 10.1016/j.jviromet.2010.09.029. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1 Nucleotide sequences encoding polybasic amino acids within the HA gene of rg1930H5N1 virus compared to the original plasmid used for transfection (pDZ_1930H5N1_HA) and the wild type A/chicken/Thailand/KU14/04 (H5N1).
Supplemental Figure 2 Trypsin dependent characteristics of rg1930H5N1. rg1930H5N1 could not produce plaque in the maintenance media without trypsin (A) while plaque formation occurred when the media was supplemented with TPCK treated trypsin (B).


