Abstract
Objectives
To identify factors that were predictive of improved pain status among older adults with chronic back pain participating in the Adaptive Physical Activity (APA) program and to identify factors that were predictive of adherence to APA.
Methods
An observational cohort study of 392 older adults (ages 50–88) with chronic back pain participating in APA for 12 months. APA was a community-based group exercise program given for 1-hour, twice weekly, in local gyms. Primary outcome measures were improved pain based on a global rating of change evaluation and adherence to the APA program (defined as participation in >75% of exercise sessions). Potential predictor variables were entered into multivariate logistic regression models to determine the most accurate set of variables for predicting improved pain and adherence.
Results
Presence of depressive symptoms, poor self-rated health and adherence to APA were the best predictors of improved pain status, with adherence being the strongest predictor [Odds Ratio:13.88 (95% CI: 8.17, 23.59)] Better physical function, longer pain duration and positive rating of the trainer were all positively associated with adherence to APA; whereas poor self-rated health and further distance from the gym were inversely associated.
Conclusions
Given that adherence to APA is the key predictor of improved back pain, future efforts should focus on strategies to improve adherence. Our data suggest that enhanced training of exercise trainers, development of separate classes for people with different functional levels and use of psychosocial interventions to reduce health pessimism and depression may be potential targets for improving adherence.
Keywords: Back Pain, Exercise, Adherence, Older Adults
INTRODUCTION
Musculoskeletal pain is a well-recognized cause of progressive disability and mobility decline in older adults.(1–2) Estimates suggest that the older population, especially those aged 65 and above, will increase by 75% within the next 20 to 30 years;(3) therefore, there will be an inevitable increase in prevalence of chronic pain and its associated societal costs. Specifically, back pain is one of the most commonly reported symptoms among older adults.(4–5) Nearly 20% of all physician visits for back pain involve older adults.(4, 6–7) In the United States, healthcare charges related to back pain in the geriatric population have increased by almost 400% in recent years.(8) Among older adults, back pain has been associated with a host of negative consequences, including decreased physical function(9–12), increased disability(13) and an increased likelihood of falling(14). It has been hypothesized that a reduction in physical activity secondary to the pain is one of the main reasons for the functional consequences seen among older adults with back pain.(11)
Consistently, the back pain literature has demonstrated that exercise is the one treatment modality that can lead to improved outcomes.(15) Further, regardless of back pain status, regular participation in an exercise or physical activity program is vitally important for the geriatric population to prevent decline in mobility function. However, adherence to an exercise program is problematic in all age groups, but particularly among older adults. For instance, a meta-analysis of 127 exercise interventions for older adults demonstrated that, within the first three to six months, 40–65% of the participants will drop out.(16) Among older adults, there are numerous factors that have been demonstrated as barriers to regular exercise, including perceived poor health, poor self-confidence, low motivation and perceived exercise enjoyment.(17) Experts in group dynamics have suggested that participation in regular group activities can lead to true behavior change through a pathway of social interaction, group bonding and behavior imitation.(18) In other patient populations (i.e. patients with cancer), group exercise has been shown to result in improved quality of life, greater self-confidence, increased motivation and a sense of camaraderie with other participants.(19) Based on social learning(18) and rehabilitation(20) models, we developed an adaptive physical activity (APA) program, designed as a community-based exercise program, to reduce the symptoms of back pain and to improve the function of older adults with chronic back pain. The APA program has become a key component of the chronic disease management initiative for the health authorities in the Tuscany region of Italy.(21–22) As with any exercise intervention, it is important to understand the person-level and environmental factors associated with perceived improvement and with adherence to the exercise program. This type of information allows clinicians and researchers to refine components and potentially identify sub-groups of patients with back pain who are likely to respond positively to the intervention. Thus, the aim of this study was to identify factors that were predictive of improvement in back pain status among older adults with chronic back pain participating in the APA program and to identify factors that were predictive of adherence to the APA program.
MATERIALS AND METHODS
Study Design
This study employed an observational prospective cohort study design. Participants aged 50 or greater with chronic back pain were recruited from local health authorities in Siena, Prato, Pisa and Empoli in the Tuscany region of Italy. Inclusion criteria were presence of back pain (thoracic or lumbar regions) for greater than 4 months, ability to rise from a chair and walk independently (with or without an assistive device), ability to travel to the exercise facility and limited participation in physical activity at the initiation of the exercise program (<90 minutes of structured physical activity per week). Exclusion criteria were as follows: unstable angina, uncontrolled hypertension, orthostatic hypotension, pulmonary disease requiring oxygen therapy, dementia, aphasia, back pain attributable to acute fracture, tumor, cancer or infection, back or leg pain that worsened with spinal extension, and, presence of 2 or more of the following signs of nerve root compression: diminished lower-extremity strength, sensation or reflexes. After referral to the APA program by their family physician, all potential participants were screened for study eligibility by a physician in the coordinating center for each of the four participating local health authorities. Participants provided informed consent according to the guidelines of the Helsinki Declaration. The Local Ethical Committee of the AUSL11 approved this human subject research study.
Baseline Measures
At baseline, participants were evaluated by a physician and a physical therapist at the coordinating center appropriate for their health authority. The evaluators participated in a two-day training course prior to initiation of the study to ensure that performance of study procedures was consistent. The evaluation included collection of basic demographic information, standardized self-report questionnaires, historical questions and physical examination measures.
Demographic/Social Factors
In terms of demographics, information was collected regarding age, sex, education level (attainment of a high school diploma), living situation (alone vs. with others) and current working status.
Health Status Factors
Presence and severity of depressive symptomatology was evaluated using the Geriatric Depression Scale (GDS), with a score of 5 or greater representing a high level of depressive symptoms.(23) The GDS is reliable and valid for identifying depressive symptoms.(24) The Short Physical Performance Battery (SPPB), a reliable and valid measure of functional performance,(25–27) included a three-stance balance test, a 4-meter gait speed test, and a five-repetition chair-stand test.(25) Each test was scored on a 0 to 4 scale, with a summary score ranging from 0 to 12.(27) Higher Scores on the SPPB indicate better functional performance. Based on previous literature, a score of eight or less is considered to represent a moderate to severe level of mobility limitation.(25) Participants were also asked to provide a current rating of their own overall health using a 5-point likert scale ranging from “excellent” to “poor.” Poor self-rated health is indicated by a choice of the “poor” category by the participant. Body mass index (BMI) was also measured in kg/m2.
Back Pain Factors
Pain severity was measured using an 11-point (0–10) numeric pain rating scale, with a score of “0” indicating no pain and “10” indicating the worst pain imaginable. Duration of back pain was categorized as follows: less than one year, between 1 and 2 years, between 2 and 5 years, between 5 and 10 years or greater than 10 years. The Roland Morris Back Pain Disability Questionnaire, a reliable and valid disease-specific measure(28), was used to capture back pain-related functional limitations.(29)
APA Back Pain Program
The APA Back Pain program was designed to improve overall health, physical functioning and back pain symptoms among older adults with back pain. The APA exercise programs were held twice weekly in local gymnasiums. Participants were able to select the gymnasium that was most convenient for them. The number of participants in each exercise group was between 15 and 20 depending on the size of the gymnasium. The exercise trainers were recruited and trained in exercise procedures by physical therapists from the local health authorities. The trainers were most typically recruited from gymnasiums where the classes would be offered. Participants paid € 2.0 (approximately $3) per class and provided their own transportation. The physical therapists periodically did unannounced fidelity checks at each of the exercise facilities within their local health authority to observe the trainer during instruction of the exercise classes. If participants reported any worsening of symptoms or health status, the trainer contacted the local rehabilitation service to report status change. As a result of these calls, a physician visit would then be scheduled for that participant. All participant complaints or incident reports were communicated to the local physical therapist from the health authority. Attendance was taken at each class by the trainer.
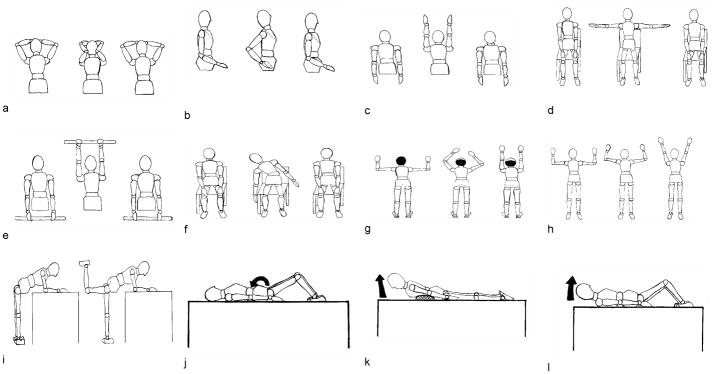
In terms of the actual APA exercise program, each session lasted approximately one hour. Exercises were primarily based on the principle that repeated spinal extension would increase the strength of the trunk extensor muscles, increase mechanical loading to the posterior elements of the spinal column for bone health and improve postural alignment of the spine. Sinaki and Mikkelsen have previously demonstrated that, among post-menopausal women, performance of extension-based trunk exercises imposes a much lower risk of vertebral compression fracture as compared to either flexion-based exercises or a lack of exercise altogether.(20) The exercises used were primarily adapted from the work of Sinaki et al.(14, 30) and augmented by physical therapists involved in the project. The exercise program had a specific focus on thoracolumbar extension, scapular retraction and abdominal strengthening. The abdominal strengthening exercises focused on the rectus abdominus muscles with careful attention paid to maintaining a neutral spine during exercise to avoid excessive lumbar flexion. Each exercise was performed 20–30 times per session. Exercises were primarily done in seated or standing positions based upon the functional tolerance of the individual participant. Some exercises were also done lying on the floor if the participant could tolerate the position. No additional resistance was used for any of the exercises. (See figure 1 for representative exercises for the trunk.) In addition to the trunk focused exercises, each exercise session began with 5–10 minutes of walking where upper extremity movements (i.e. scapular retraction, arm circles, shoulder flexion) were incorporated. Additionally, flexibility exercises (hamstring and calf stretches) and strengthening exercises (mini squats and toe raises) were included for lower extremity musculature.
Figure 1.
Spinal Extension Exercise Program includes the following components: a) scapular retraction with elbow press; b) scapular retraction with cervical extension; c) thoracic extension with shoulder flexion; d) scapular retraction with shoulder joint abduction; e) thoracic extension with wand lift; f) sidebend from erect sitting position; g) wall climb with cervical extension; h) scapular stabilization with arm lift; i) standing hip extension; j) posterior pelvic tilt in supine; k) prone spinal extension to neutral, and; l)abdominal crunch with neutral spine.
Follow-Up Measurements
Twelve months after the baseline examination for the APA program, study staff contacted all participants by telephone to do a follow-up interview. The interview consisted of questions regarding accessibility of the gymnasium, opinions of the facilities and exercise trainers, as well as whether their pain level, health status and mood had improved. To assess whether pain, health status and mood had improved, participants were asked to rate their overall change in each domain since initiating the APA program using a 7-point global rating of change scale described by Jaeschke et al.(31) Scores on the global rating of change scale range from “-3” (a very great deal worse) to “0” (about the same) to “+3” (a very great deal better). Participants with a rating of “-2” or smaller were considered to have worsened, whereas participants with ratings between “-1” and “+1” were considered to be the same and those with scores of “+2” or higher were considered to have improved. The global rating of change scale has been found to be reliable and valid for use as an outcome measure.(32–33)
Accessibility Factors
In terms of accessibility of the gym, participants were asked whether they were able to travel to the gym independently without assistance; possible responses were “yes” or “no.” Further, the distance of the participant’s home to the nearest APA gym facility was determined by using the Yahoo Maps website (http://it.mappe.yahoo.net/tc/home.jsp). The participant’s address and the address of the gym were entered into the web form and walking distance in kilometers was used as the distance to the gym.
APA Program Satisfaction Factors
Participants were also asked about their overall satisfaction with the APA program. Specifically, participants were asked the following questions: (a) “How satisfied are you with your exercise trainer?” (b) “How satisfied are you with the cleanliness of the exercise facility?” and (c) “How satisfied are you with the hours of operation for APA exercise classes?”. All satisfaction questions used a 5-point likert scale for responses ranging from “very satisfied” to “very dissatisfied.” For analytic purposes, satisfaction status was based on selection of the “very satisfied” category for each of the satisfaction questions. For those participants who stopped attending the APA Back Pain program prior to the 12-month interview, they were asked to provide the primary reason for discontinuing participation in the exercise program.
Statistical Analysis
All statistical analyses were performed using PASW Statistics 18 (SPSS Inc., Chicago, IL). Descriptive analyses were performed for baseline characteristics of the entire sample. Further, descriptive analyses were performed to provide basic information regarding proportions of participants who perceived improved pain, overall health and mood following one year of participation in the APA program, as well as to provide information regarding reasons for non-adherence to the APA program.
Our primary outcome measures for this study were improved back pain status based on the global rating of change evaluation (defined as a score of “+2” or greater) and adherence to the APA program (defined as participation in >75% of all exercise sessions for the entire 12 month study period). As a first step in identifying factors that were predictive of improved back pain status, we conducted univariate analyses of all potential predictor variables (i.e., demographic factors, health status factors, back pain factors, accessibility factors and program satisfaction factors) according to improved pain status. The same process was used for the primary outcome of APA program adherence. Independent sample t tests were used to establish group differences for continuous variables and chi-square tests for categorical variables. Then, we performed two separate multivariable logistic regression analyses to determine the combined effects of the appropriate predictor variables on our two primary outcomes—improved pain status and program adherence. Inclusion of appropriate predictor variables in these final multivariate regression models was based on multicollinearity assessment and the strength of their univariate association with the primary outcome measures. For each primary outcome, potential predictor variables with a significant univariate association with that outcome (p<.10) were retained as potential predictor variables for that particular regression model. A more liberal significance level was used because this step was intended to filter variables with no association with the outcome, and we did not wish to exclude any predictor variables that might be potentially useful in a multivariate model. In the final multivariate logistic regression models for improved pain status and adherence, the alpha level was set at .05.
RESULTS
There were 504 patients with chronic back pain who were consecutively referred to the APA program by their family physicians between December 2007 and February 2008; all consented to participate and completed all baseline assessments. Of the 504 participants who consented, 392 initiated participation in the APA exercise program and completed the 12-month follow-up telephone interview. Data from 112 participants were not included in our primary analyses for the following reasons: (a) the participant never attended an exercise session (n=50); (b) study staff was unable to locate the participant for the follow-up telephone interview (n=24); (c) the participant refused the telephone interview (n=37); and (d) the participant was deceased by the 12-month interview (n=1). As seen in table 1, with the exception of education level, there were no differences in participant characteristics between those whose data was included versus not included. For participants whose data was not used in our primary analyses, they were more likely to have had at least a high school education as compared to those whose data was not included (p=.002).
Table 1.
Baseline characteristics of the entire sample
| Included in Analyses N=392 | Not Included in Analyses* N=112 | p-value | |
|---|---|---|---|
| Age (years) | 66.8 (8.0) | 67.9 (8.0) | .168 |
| Sex (N, % female) | 330 (84.2%) | 89 (80.0%) | .198 |
| Live alone? (N, %yes) | 66 (16.8%) | 28 (25.0%) | .079 |
| Education (N, % ≥ high school diploma) | 84 (21.4%) | 38 (33.9%) | .002 |
| Currently working? (N, %yes) | 32 (8.2%) | 11 (9.8%) | .429 |
| Poor Self-Rated Health (N, %yes) | 40 (10.2%) | 18 (16.1%) | .059 |
| Body Mass Index (kg/m2) | 26.4 (3.9) | 26.8 (4.9) | .417 |
| High Depressive Symptoms (N, % GDS>5) | 126 (32.1%) | 27 (24.1%) | .084 |
| Short Physical Performance Battery | 9.3 (2.0) | 9.4 (2.0) | .748 |
| Numeric Pain Rating Scale | 5.1 (3.0) | 4.6 (3.0) | .204 |
| Roland Morris Scale | 8.7 (5.1) | 9.1 (5.0) | .291 |
| Duration of symptoms (N, %>10 years) | 229 (58.3) | 59 (52.7) | .285 |
All values reported are means (standard deviation) unless otherwise noted.
GDS=Geriatric Depression Scale
Participants were not included if they did not participate in the follow-up telephone interview for any of the following reasons: never attended an APA class, refused interview, not found or deceased.
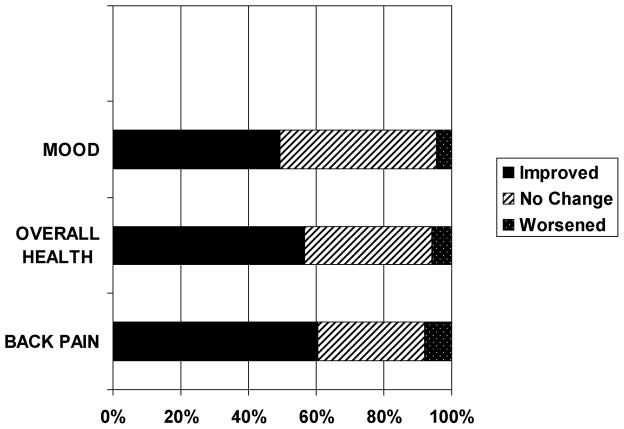
At the end of the 12-month study period, the majority of the participants (60.4%) reported improved back pain, while only 8% reported a worsened pain. (See figure 2.) More than one-half (57%) also reported improved overall health and 49% reported an improvement in their mood. Approximately 60% of the sample were adherent to the exercise program as defined by participation in >75% of all exercise sessions for the entire 12 month study period. When participants were asked to provide the primary reason why they discontinued participation in the APA program, the following were the most commonly given responses: development of a health problem or worsening of an existing health condition (38.4%); family issues (27.4%); minimal interest in exercising (8.5%); worsening of back pain (5.5%); and other (21.2%). No adverse clinical events occurred during any of the APA exercise classes.
Figure 2.
12-month changes since beginning the APA program
Table 2 shows the results of the univariate analyses of demographic, health status, back pain, accessibility and program satisfaction factors as they relate to improved back pain status. Ten variables were significantly related to improved back pain status: living alone, currently working, high depressive symptoms as measured by the GDS, better physical function as measured by an SPPB score >8, poor self-rated health, greater pain severity, greater low back-related functional limitations as measured by the Roland Morris scale, adherence to the APA program, as well as a high level of satisfaction with the trainer and with the available hours for the APA exercise sessions. There were no issues of multicollinearity between these variables. All ten potential predictor variables were entered into the multivariable logistic regression model for improved back pain status and three were statistically significant predictors: high depressive symptoms (GDS>5), poor self-rated health and adherence (table 3). Adherence to the APA exercise program throughout the entire year was the strongest predictor of improvement in back pain [Odds Ratio (OR):13.88 (95% CI: 8.17, 23.59)]; while poor self-rated health [OR: 0.2 (95% CI: 0.08, 0.51)] and high depressive symptoms [OR: 0.47 (95% CI: 0.25, 0.89)] were associated with reduced odds of having improved back pain after 12 months of participation in the APA program.
Table 2.
Univariate analyses of potential predictor variables according to back pain improvement status
| Improved (N=235) | Not improved (N=157) | p-value | |
|---|---|---|---|
| Demographic/Social factors | |||
| Age (years) | 66.4 (7.1) | 67.4 (8.4) | .172 |
| Sex (N, % female) | 198 (84.3%) | 133 (84.7%) | .838 |
| Live alone? (N, %yes) | 33 (14.0%) | 33 (21.0%) | .047 |
| Education (N, % ≥ high school diploma) | 47 (20%) | 37 (23.6%) | .393 |
| Currently working? (N, %yes) | 15 (6.4%) | 17 (10.8%) | .070 |
| Health Status Factors | |||
| High Depressive Symptoms (N, % GDS>5) | 42 (17.9%) | 57 (36.3%) | .000 |
| SPPB score >8 (N, %yes) | 196 (83.4%) | 111 (70.7%) | .002 |
| Poor Self-Rated Health (N, %yes) | 9 (3.9%) | 31 (20%) | .000 |
| Body Mass Index (kg/m2) | 26.4 (4.0) | 26.5 (3.7) | .707 |
| Back Pain Factors | |||
| Numeric Pain Rating Scale | 4.5 (2.5) | 5.2 (2.7) | .006 |
| Roland Morris Scale | 7.9 (4.9) | 9.6 (4.7) | .001 |
| Duration of symptoms (N, %>10 years) | 140 (59.6%) | 88 (56.1%) | .468 |
| Accessibility/Attendance Factors* | |||
| Distance to gym (km) | 2.2 (2.58) | 2.6 (2.5) | .225 |
| Able to go independently? (N, %yes) | 215 (91.4%) | 138 (87.9%) | .275 |
| Adherent to APA program? (N, %yes) | 191 (81.2%) | 35 (22.2%) | .000 |
| APA Satisfaction Factors* | |||
| Trainer (N, %very satisfied) | 135 (57.4%) | 70 (44.5%) | .013 |
| Facilities (N, %very satisfied) | 49 (20.8%) | 28 (17.8%) | .429 |
| Hours of operation (N, %very satisfied) | 67 (28.5%) | 29 (18.5%) | .020 |
All values reported are means (standard deviation) unless otherwise noted.
GDS=Geriatric Depression Scale; SPPB= Short Physical Performance Battery
These factors are from the follow-up telephone interview, but all other factors are from the baseline assessment.
Table 3.
Multivariate logistic regression analysis of factors associated with improved back pain status
| Odds Ratio | 95% CI | p-value | |
|---|---|---|---|
| Demographic/Social factors | |||
| Lives alone | 0.60 | 0.31–1.18 | .140 |
| Currently working | 2.14 | 0.81–5.63 | .125 |
| Health Status Factors | |||
| High Depressive Symptoms (GDS>5) | 0.47 | 0.25–0.89 | .019 |
| SPPB score >8 | 1.71 | 0.88–3.34 | .114 |
| Poor Self-Rated Health | 0.20 | 0.08–0.51 | .001 |
| Back Pain Factors | |||
| Numeric Pain Rating Scale | 0.94 | 0.85–1.05 | .273 |
| Roland Morris Scale | 1.01 | 0.95–1.07 | .786 |
| Accessibility/Attendance Factors* | |||
| Adherent to APA program | 13.88 | 8.17–23.59 | <.001 |
| APA Satisfaction Factors* | |||
| Positive rating of trainer | 1.13 | 0.63–2.02 | .675 |
| Satisfied with hours of operation | 1.36 | 0.67–2.75 | .391 |
GDS=Geriatric Depression Scale; SPPB= Short Physical Performance Battery
These factors are from the follow-up telephone interview, but all other factors are from the baseline assessment.
Table 4 shows the univariate results relating to adherence. Nine variables were significantly associated with adherence to the APA program: education equivalent to at least a high school diploma, high depressive symptoms (GDS>5), better physical function (SPPB score >8), poor self-rated health, longer duration of back pain (>10 years), greater low back pain-related functional limitations, distance from home to the gym, as well as a high level of satisfaction with the trainer and with the available hours for the APA exercise sessions. There were no issues of multicollinearity between these variables. All nine potential predictor variables were entered into the multivariable logistic regression model for program adherence and five were statistically significant predictors: higher levels of physical function (SPPB>8), poor self-rated health, longer duration of back pain (>10 years), greater distance from home to gym and positive rating of the exercise trainer (table 5). Better physical function, longer pain duration and positive rating of the trainer were all significantly associated with a nearly 2-fold greater odds of adherence to the APA program; whereas poor self-rated health [OR: 0.35 (95% CI: 0.17, 0.73)] and further distance from the gym [OR: 0.92 (95% CI: 0.85, 0.99)] were inversely associated with adherence. The odds ratio for distance from the gym is interpreted as follows: for every 1 kilometer increase in distance from the gym, the probability of adherence to the APA program decreases by 8%.
Table 4.
Univariate analysss of potential predictor variables according to adherence status
| Adherent (N=238) | Not Adherent (N=154) | p-value | |
|---|---|---|---|
| Demographic/Social factors | |||
| Age (years) | 66.8 (6.9) | 66.7 (8.5) | .878 |
| Sex (N, % female) | 200 (84.1%) | 132 (85.7%) | .825 |
| Live alone? (N, %yes) | 37 (15.5%) | 32 (20.8%) | .258 |
| Education (N, % ≥ high school diploma) | 40 (16.8%) | 38 (24.6%) | .063 |
| Currently working? (N, %yes) | 15 (6.4%) | 14 (8.9%) | .254 |
| Health Status Factors | |||
| High Depressive Symptoms(N, % GDS>5) | 48 (20.1%) | 47 (30.5%) | .019 |
| SPPB score >8 (N, %yes) | 197 (82.8%) | 113 (73.4%) | .036 |
| Poor Self-Rated Health (N, %yes) | 13 (5.4%) | 25 (16.2%) | .000 |
| Body Mass Index (kg/m2) | 26.5 (4.0) | 26.4 (3.8) | .884 |
| Back Pain Factors | |||
| Numeric Pain Rating Scale | 4.6 (2.5) | 4.9 (2.7) | .246 |
| Roland Morris Scale | 7.9 (4.8) | 9.4 (5.1) | .005 |
| Duration of symptoms (N, %>10 years) | 150 (63.0%) | 78 (50.6%) | .011 |
| Accessibility Factors | |||
| Distance to gym (km) | 2.1 (2.6) | 2.7 (2.5) | .027 |
| Able to go independently (N, %yes) | 216 (90.8%) | 138 (89.6%) | .166 |
| APA Satisfaction Factors* | |||
| Trainer (N, %very satisfied) | 103 (43.2%) | 93 (60.3%) | .002 |
| Facilities (N, %very satisfied) | 47 (19.7%) | 30 (19.4%) | .767 |
| Hours of operation (N, %very satisfied) | 67 (28.1%) | 31 (20.1%) | .036 |
All values reported are means (standard deviation) unless otherwise noted.
GDS=Geriatric Depression Scale; SPPB= Short Physical Performance Battery
These factors are from the follow-up telephone interview, but all other factors are from the baseline assessment.
Table 5.
Multivariate logistic regression analysis of factors associated with adherence to APA program
| Odds Ratio | 95% CI | p-value | |
|---|---|---|---|
| Demographic/Social factors | |||
| ≥ High school level education | 1.58 | 0.96–2.63 | .075 |
| Health Status Factors | |||
| High Depressive Symptoms (GDS>5) | 0.71 | 0.43–1.19 | .196 |
| SPPB score >8 | 1.81 | 1.06–3.10 | .031 |
| Poor Self-Rated Health | 0.35 | 0.17–0.73 | .005 |
| Back Pain Factors | |||
| Roland Morris Scale | 0.98 | 0.94–1.03 | .397 |
| Duration of Back Pain (>10 years) | 1.90 | 1.22–2.97 | .005 |
| Accessibility Factors | |||
| Distance to gym (km) | 0.92 | 0.85–0.99 | .043 |
| APA Satisfaction Factors* | |||
| Positive rating of trainer | 1.71 | 1.08–2.71 | .021 |
| Satisfied with hours of operation | 1.35 | 0.78–2.36 | .286 |
GDS=Geriatric Depression Scale; SPPB= Short Physical Performance Battery
These factors are from the follow-up telephone interview, but all other factors are from the baseline assessment.
DISCUSSION
The primary objectives of this study were to identify factors associated with improved back pain among APA participants and to identify factors associated with adherence to the APA exercise program. As one might expect, participation in the APA program was associated with improved back pain status among those who were most adherent to the exercise program. More than 60% of the sample reported improvement in their back pain status at the 12-month follow-up interview and the strongest predictor of improvement was regular participation in the exercise program. This finding is consistent with the concept that regular exercise in patients with chronic back pain can reduce pain, prevent recurrence and reduce disability.(15, 34)) Several recent systematic reviews of exercise and non-specific chronic low back pain have been performed to disentangle the findings of the many exercise studies that have been done and these reviews report similar findings.(15, 34–35) First, stretching and trunk muscle training are the most effective types of exercise for patients with CLBP. Trunk muscle strengthening consistently results in modest decreases in pain and modest improvements in function. Also, supervised exercise programs were more effective than non-supervised programs, perhaps due to increased compliance.(15, 35) Finally, higher doses of exercise (greater than or equal to 20 hours) throughout the course of the intervention were also found to be more effective in improving outcomes.(15, 35) In the context of the APA program, we have utilized the aforementioned strategies to make our community-based exercise program as effective as possible. Our data also suggests that participation in the APA exercise program was associated with improved overall health for nearly 60% of the sample and with improved mood for 50% of the sample. Regular exercise has consistently been linked with reports of improved self-rated health and improved mood in the geriatric literature.(36–37) Given that adherence to the APA program is the strongest predictor of improvement in back pain status, it becomes even more important to understand the factors (i.e. proximity of exercise facilities, perception of exercise trainer, perceived health and functional status) that were associated with adherence to the exercise program. Understanding factors associated with pain improvement and exercise adherence provides us with vital information to develop new strategies focused on improving exercise adherence and participant outcomes for future iterations of the APA program.
The key variables for predicting back pain status after 12 months of participation in the APA exercise program included: adherence to the exercise program, self-rated health and depressive symptomatology. As previously discussed, adherence to the APA exercise program was the strongest predictor of improved back pain status, by far. For those participants who attended >75% of all exercise sessions for the entire 12-month period, the odds of improved back pain status were increased by nearly 14-fold. This finding strongly advocates for the notion that older adults with chronic pain can see improvements in their pain if they are actively engaged in exercise. Further, we see that the odds of improved back pain status at the 12-month follow-up were reduced by 80% among those with poor self-rated health (SRH) at the beginning of the APA program. SRH has been recognized as an independent predictor of health trajectories, including mortality.(38) It has also been demonstrated that poor SRH was linked with reduced health screenings and increased participation in unhealthy behaviors, i.e. physical inactivity and smoking.(39) Further, Boardman concluded that individuals with poor SRH “may be more likely to ignore a doctor's recommendations, less likely to take prescribed medication regularly, and less likely to pursue a specialist for treatment”.(40) Thus, it is not surprising that poor SRH is an arbiter of poor outcomes for individuals participating in the APA program. The final predictor of back pain improvement for APA participants was depressive sympotmatology with a higher level of depressive symptoms at baseline being associated with a 53% reduction in the odds of improvement 12 months later. Among older adults, there is a bi-directional relationship between low back pain and depressive symptoms as each is a risk factor for the other.(41–43) Karp et al. asserted that the relationship between chronic low back pain and depression “can lead to a cycle of demoralization, physical and psychosocial disability, and exacerbated medical and psychiatric comorbidity.”(44) In the presence of both back pain and depressive symptoms, it may be vitally important to address both issues simultaneously to have good outcomes for either problem.
Community-based exercise programs, such as the APA program, are commonly used interventions to engage specific members of the community in improving their overall physical activity level and physical health. A significant feature of these community-based exercise programs is that they require active engagement and participation from the members of the community. Therefore, it is critical for healthcare professionals who are developing these programs to find the most targeted approaches to engage the intended community in the exercise program. In the context of the APA program, we have identified five factors that are predictive of adherence to the APA exercise program; and they are functional status of the participant, self-rated health, duration of back pain, proximity to the gym and the participant’s perception of the trainer. For participants with an SPPB score >8, they were more likely to be adherent to the APA program. Interestingly, it is the participants who have the least risk of subsequent disability who are most likely to attend the APA classes consistently. There may be several explanations. First, APA participants with lower functional status may have more difficulty getting to the classes due to their functional level. Or, the participants with higher functional levels may have already been more actively engaged in healthy behaviors, such as exercise, therefore it was an easier transition for them to attend the exercise classes consistently. Finally, it is possible that the APA exercise program was too challenging for the participants with low functional status and therefore they were more discouraged in coming to classes. In a preemptive effort to avoid this issue, we developed modifications for all exercises so that individuals of different functional levels could all engage in the exercise program, i.e. performing exercises in seated position rather than standing. But, it may be necessary to develop separate classes that are more tailored to older individuals with lower functional levels.
Similar to the model developed to predict improvement in back pain status, poor SRH is associated with a 65% reduction in the odds of being adherent to the APA program. This is perfectly in line with the assertion of Idler and Benyami that individuals with poor SRH are less likely to engage in positive health behaviors, i.e. attending an exercise program.(39) As SRH is a solid predictor of improvement and adherence, we must consider ways to address poor SRH either before participants begin the APA program or simultaneously. It may be necessary to engage the participants with poor SRH in a psychosocial intervention, i.e. counseling or mindfulness meditation, to address their health pessimism. In terms of back pain duration, it was somewhat surprising that greater duration of pain was associated with greater adherence to the APA program. But, we must keep in mind that 58% of the entire sample had a history of chronic back pain exceeding 10 years. It is possible that participants with longer-standing pain were more willing and motivated to exercise in an attempt to control their symptoms. We also found that living a greater distance from the gym was associated with reduced odds of being adherent to the APA program. This finding is logical and suggests that offering a greater number of APA classes in more geographically dispersed locations may improve adherence for participants. Finally, we found that if participants had a positive perception of the exercise trainer in their APA class they were 86% more likely to be adherent to the APA program. Again, this is a logical finding and speaks strongly to the idea that the exercise trainers need to be knowledgeable, engaging and likeable if we are to improve exercise adherence to the APA program. Enhanced training of the exercise trainers may be a potential way to improve overall adherence to the APA program.
There are some important features of the APA-back pain program that are noteworthy. First, the back pain literature is clear that regular exercise and physical activity is one pathway through which individuals can improve their symptoms and reduce pain-related disability.(15) Based on this evidence, the APA-back pain program was developed to address the call to increased physical activity for older adults with back pain through the implementation of a community-based exercise program. The design of the APA-back pain exercise program was based upon the experimental work of Sinaki et al.(20) Further, we believe that the use of the group exercise paradigm in the APA-back pain program may have contributed to the positive outcomes seen among those who regularly participated in the exercise program by way of increased social support and increase motivation, but we did not measure these factors; future work should focus on the psychosocial benefits of the APA program. Another important feature of the program was its cost-effective design, including the use of low-tech equipment and local gymnasiums, as well as the fact that the participants were actually paying a relatively low fee for the courses. Interestingly, cost of the exercise classes was never given as a reason for dropping out of the APA program.
A major advantage of this study is the use of a large community-dwelling cohort sample of older adults with back pain participating in a community-based exercise program with 12-month follow-up data. The prospective nature of this study allows us to highlight possible approaches to improve the APA-back pain program by identifying factors associated with improvement in back pain symptoms and adherence to the APA program. Nonetheless, several limitations must be considered in interpreting the findings. First, this study utilizes a cohort study design rather than a randomized control design. Therefore, we are not able to empirically establish the effectiveness of the APA-back pain program in the context of this study. Use of the randomized control design was considered initially, but finally deemed to not be feasible given that the APA-back pain exercise program is considered by the local health authorities and residents to be an established component of the healthcare system. Second, although there was missing data in this longitudinal study, the participants who were not included in the analysis were quite similar to the participants who were included in the analysis. Further, although we do have 12-month follow-up data from the telephone interview, we do not have follow-up data on changes in performance based measures of function. Lastly, we did not use any standardized measures of function and disability (i.e. the Late Life Function and Disability Instrument), which would have allowed us to measure the changes in these domains associated with participation in the APA-back pain program. Also, we do not have any data on the psychosocial status of the participants in the APA program. Understanding the participants’ perspectives on fear, self-efficacy, resilience and outcomes expectations would likely provide us with a greater understanding of factors that impact adherence to the APA program.
In conclusion, older adults with back pain were able to safely participate in a community-based exercise program with the majority reporting improved back pain status 12 months later. The key factor that predicted improvement in back pain was continued adherence to the APA-back pain exercise program throughout the entire 12-month time period. If community-based exercise programs are to be successful for this population with chronic pain, it is clear that we must identify strategies to optimize adherence. Our preliminary investigation of adherence to a community-based exercise program suggests that enhanced training of exercise trainers, development of separate classes for people with different functional levels and use of psychosocial interventions to reduce health pessimism and depression may be potential targets for improving adherence. Our findings should be replicated and each of these potential strategies will need to be systematically tested before clinical guidelines can be recommended with confidence.
Acknowledgments
Funding: The study was financially supported by Tuscany Region (DGR 265/07). The work of Dr. Hicks was supported by R21 HD057274 (NICHD).
References
- 1.Leveille SG, Bean J, Bandeen-Roche K, Jones R, Hochberg M, Guralnik JM. Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc. 2002;50:671–8. doi: 10.1046/j.1532-5415.2002.50161.x. [DOI] [PubMed] [Google Scholar]
- 2.Leveille SG, Ling S, Hochberg MC, Resnick HE, Bandeen-Roche KJ, Won A, et al. Widespread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med. 2001;135:1038–46. doi: 10.7326/0003-4819-135-12-200112180-00007. [DOI] [PubMed] [Google Scholar]
- 3.Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1992–2050. Washington, DC: US Government Printing Office; 1992. [Google Scholar]
- 4.Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24:1813–9. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 5.Koch HSM. National Ambulatory Medical Care Survey, 1980 and 1981. Vol. 110. Hyattsville, MD: Advance Data from Vital and Health Statistics, National Center for Health Statistics (NCHS); 1985. Office-based ambulatory care for patients 75 years old and over; pp. 1–14. [Google Scholar]
- 6.Cypress BK. Characteristics of physician visits for back symptoms: a national perspective. Am J Public Health. 1983;73:389–95. doi: 10.2105/ajph.73.4.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hart LG, Deyo RA, Cherkin DC. Physician office visits for low back pain. Frequency, clinical evaluation, and treatment patterns from a U.S. national survey. Spine. 1995;20:11–9. doi: 10.1097/00007632-199501000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Weiner DK, Kim Y, Bonino P, Wang T. Low Back Pain in Older Adults: Are We Utilizing healthcare Resources Wisely? Pain Medicine. 2006;7:143. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]
- 9.Reid MC, Williams CS, Gill TM. Back pain and decline in lower extremity physical function among community-dwelling older persons. J Gerontol A Biol Sci Med Sci. 2005;60:793–7. doi: 10.1093/gerona/60.6.793. [DOI] [PubMed] [Google Scholar]
- 10.Hicks GE, Simonsick EM, Harris TB, Newman AB, Weiner DK, Nevitt MA, et al. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2005;60:882–7. doi: 10.1093/gerona/60.7.882. [DOI] [PubMed] [Google Scholar]
- 11.Hicks GE, Simonsick EM, Harris TB, Newman AB, Weiner DK, Nevitt MA, et al. Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol A Biol Sci Med Sci. 2005;60:1420–4. doi: 10.1093/gerona/60.11.1420. [DOI] [PubMed] [Google Scholar]
- 12.Hicks GEGJ, Shardell M, Simonsick EM. Associations of back and leg pain with health status and functional capacity of older adults: Findings from the Retirement Community Back Pain Study. Arthritis Care Res. 2008 doi: 10.1002/art.24006. In press. [DOI] [PubMed] [Google Scholar]
- 13.Leveille SG, Guralnik JM, Hochberg M, Hirsch R, Ferrucci L, Langlois J, et al. Low back pain and disability in older women: independent association with difficulty but not inability to perform daily activities. J Gerontol A Biol Sci Med Sci. 1999;54:M487–93. doi: 10.1093/gerona/54.10.m487. [DOI] [PubMed] [Google Scholar]
- 14.Sinaki M, Brey RH, Hughes CA, Larson DR, Kaufman KR. Significant reduction in risk of falls and back pain in osteoporotic-kyphotic women through a Spinal Proprioceptive Extension Exercise Dynamic (SPEED) program. Mayo Clin Proc. 2005;80:849–55. doi: 10.4065/80.7.849. [DOI] [PubMed] [Google Scholar]
- 15.Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med. 2005;142:776–85. doi: 10.7326/0003-4819-142-9-200505030-00014. [DOI] [PubMed] [Google Scholar]
- 16.Dishman RK, Buckworth J. Increasing physical activity: a quantitative synthesis. Med Sci Sports Exerc. 1996;28:706–19. doi: 10.1097/00005768-199606000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Lee LL, Arthur A, Avis M. Using self-efficacy theory to develop interventions that help older people overcome psychological barriers to physical activity: a discussion paper. Int J Nurs Stud. 2008;45:1690–9. doi: 10.1016/j.ijnurstu.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 18.Yalom ID. The theory and practice of group psychotherapy. 3. New York: Basic Books; 1985. [Google Scholar]
- 19.Losito J, Murphy S, Thomas M. The effects of group exercise on fatigue and quality of life during cancer treatment. Oncol Nurs Forum. 2006;33:821–5. doi: 10.1188/06.ONF.821-825. [DOI] [PubMed] [Google Scholar]
- 20.Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984;65:593–6. [PubMed] [Google Scholar]
- 21.Stuart M, Benvenuti F, Macko R, Taviani A, Segenni L, Mayer F, et al. Community-based adaptive physical activity program for chronic stroke: feasibility, safety, and efficacy of the Empoli model. Neurorehabil Neural Repair. 2009;23:726–34. doi: 10.1177/1545968309332734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stuart M, Chard S, Benvenuti F, Steinwachs S. Community exercise: a vital component to healthy aging. Healthc Pap. 2009;10:23–8. doi: 10.12927/hcpap.2009.21219. discussion 79–83. [DOI] [PubMed] [Google Scholar]
- 23.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 24.D'Ath P, Katona P, Mullan E, Evans S, Katona C. Screening, detection and management of depression in elderly primary care attenders. I: The acceptability and performance of the 15 item Geriatric Depression Scale (GDS15) and the development of short versions. Fam Pract. 1994;11:260–6. doi: 10.1093/fampra/11.3.260. [DOI] [PubMed] [Google Scholar]
- 25.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 26.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med. 1995;332:556–61. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–31. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 28.Kopec JA, Esdaile JM, Abrahamowicz M, Abenhaim L, Wood-Dauphinee S, Lamping DL, et al. The Quebec Back Pain Disability Scale. Measurement properties. Spine. 1995;20:341–52. doi: 10.1097/00007632-199502000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Roland M, Morris R. A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care. Spine (Phila Pa 1976) 1983;8:145–50. doi: 10.1097/00007632-198303000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002;30:836–41. doi: 10.1016/s8756-3282(02)00739-1. [DOI] [PubMed] [Google Scholar]
- 31.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407–15. doi: 10.1016/0197-2456(89)90005-6. [DOI] [PubMed] [Google Scholar]
- 32.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific Quality of Life Questionnaire. J Clin Epidemiol. 1994;47:81–7. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 33.Goldsmith CH, Boers M, Bombardier C, Tugwell P. Criteria for clinically important changes in outcomes: development, scoring and evaluation of rheumatoid arthritis patient and trial profiles. OMERACT Committee. J Rheumatol. 1993;20:561–5. [PubMed] [Google Scholar]
- 34.van Tulder MW, Malmivaara A, Esmail R, Koes BW. Exercise therapy for low back pain. Cochrane Database Syst Rev. 2000:CD000335. doi: 10.1002/14651858.CD000335. [DOI] [PubMed] [Google Scholar]
- 35.Liddle SD, Baxter GD, Gracey JH. Exercise and chronic low back pain: what works? Pain. 2004;107:176–90. doi: 10.1016/j.pain.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 36.Barbour KA, Blumenthal JA. Exercise training and depression in older adults. Neurobiol Aging. 2005;26 (Suppl 1):119–23. doi: 10.1016/j.neurobiolaging.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 37.Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Arch Intern Med. 1999;159:2349–56. doi: 10.1001/archinte.159.19.2349. [DOI] [PubMed] [Google Scholar]
- 38.Ferraro KF, Farmer MM, Wybraniec JA. Health trajectories: long-term dynamics among black and white adults. J Health Soc Behav. 1997;38:38–54. [PubMed] [Google Scholar]
- 39.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38:21–37. [PubMed] [Google Scholar]
- 40.Boardman JD. Health pessimism among black and white adults: the role of interpersonal and institutional maltreatment. Soc Sci Med. 2004;59:2523–33. doi: 10.1016/j.socscimed.2004.04.014. [DOI] [PubMed] [Google Scholar]
- 41.Herr KA, Mobily PR, Smith C. Depression and the experience of chronic back pain: a study of related variables and age differences. Clin J Pain. 1993;9:104–14. doi: 10.1097/00002508-199306000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Garron DC, Leavitt F. Chronic low back pain and depression. J Clin Psychol. 1983;39:486–93. doi: 10.1002/1097-4679(198307)39:4<486::aid-jclp2270390405>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 43.Reid MC, Williams CS, Concato J, Tinetti ME, Gill TM. Depressive symptoms as a risk factor for disabling back pain in community-dwelling older persons. J Am Geriatr Soc. 2003;51:1710–7. doi: 10.1046/j.1532-5415.2003.51554.x. [DOI] [PubMed] [Google Scholar]
- 44.Karp JF, Weiner DK, Dew MA, Begley A, Miller MD, Reynolds CF., 3rd Duloxetine and care management treatment of older adults with comorbid major depressive disorder and chronic low back pain: results of an open-label pilot study. Int J Geriatr Psychiatry. 2010;25:633–42. doi: 10.1002/gps.2386. [DOI] [PMC free article] [PubMed] [Google Scholar]