Abstract
Introduction
Patients must have transportation to the treatment site before they can access appropriate cancer care. This paper describes factors associated with patients experiencing transportation-related barriers to accessing cancer care.
Patients and Methods
The Cancer Care Assessment & Responsive Evaluation Studies (C-CARES) questionnaire was mailed to VA colorectal cancer (CRC) patients during fall 2009. Eligible patients were diagnosed at any VA facility in 2008, male, and alive at time of mailing. A total of 1,409 surveys were returned (approximately 67% response rate). To assess transportation barriers, patients were asked how often it was difficult to get transportation to or from treatment. Symptoms were assessed using validated PROMIS scales for fatigue, pain, and depression. Multivariate logistic regression was used to examine determinants of transportation barriers.
Results
A minority (19%) of respondents reported transportation barriers. Patients experiencing pain (OR 1.04, 95% CI 1.02, 1.06) had greater odds of transportation barriers than patients without this symptom. Patients who reported no primary social support (OR 6.13, 95% CI 3.10, 12.14) or non-spousal support (OR 2.00, 95% CI 1.40, 2.87) were more likely to experience transportation barriers than patients whose spouse provided social support.
Discussion
Patients with uncontrolled pain or less social support have greater odds of transportation barriers. The directional association between social support, symptoms, and transportation cannot be determined in this data.
Conclusion
Inquiring about accessible transportation should become a routine part of cancer care, particularly for patients with known risk factors.
Keywords: transportation, access to health care, colorectal neoplasms, health services research, veterans affairs
INTRODUCTION
Transportation to and from treatment is an important and often overlooked aspect of cancer care quality continuum.1,2 Extensive research has been conducted examining lack of transportation as a barrier for cancer screening.3,4 In contrast to the literature regarding cancer screening, transportation barriers among patients undergoing active treatment have received considerably less research attention and continue to be a problem. Difficulty with transportation is a problem for many cancer patients – limiting access to healthcare services and hindering a patient’s likelihood of obtaining appropriate cancer care. Longer transportation time to health services has been associated with increased burdens on time, cost to the patient, and patient discomfort.5 Travel distances are also important because patients may not have local services or may bypass local services due to lack of confidence in their quality.5 This may result in an increased burden on both cancer patients and their caregivers.7
It has been previously reported that an estimated 13-14% of cancer patients experience transportation problems related to obtaining care.6 Problems with transportation and other access to healthcare have been shown to predominately affect the elderly8,9, those who live in rural areas1,5,8,10-12, racial and ethnic minorities9, patients with lower annual household income 6,9,10,13, and patients with less social support.1,9,10,13 Therefore, it may be particularly important to examine transportation issues in colorectal cancer patients who are older, non-white, and who present with later stage disease at diagnosis.
Little is known about the transportation difficulties of veterans with cancer who receive their care at a VA facility. Eligible Veterans have access to the largest integrated healthcare service network in the county, including 143 VA medical centers offering cancer treatment services. However, Veterans are more likely to live in rural areas and have lower incomes than the general public, two factors previously linked with transportation barriers.14 In addition, within the VA healthcare system there is further regionalization of certain procedures such as bone marrow transplantation.15 As a result, there may be persistent access issues for VA patients.
The aims of the present study are to determine the level of healthcare-related transportation difficulty reported by VA colorectal cancer patients and identify patient-level determinants of experiencing transportation as a barrier to cancer care. We hypothesized that, after controlling for patient and disease characteristics, patients with limited access to informal caregiving, lower annual income, and higher symptoms will have greater odds of reporting that transportation difficulties are a barrier affecting their ability to access cancer care.
PATIENTS AND METHODS
The present study utilizes survey data from VA patients with colorectal cancer diagnosed in 2008. The protocol for survey administration and use of data for analysis were approved by the Institutional Review Board (IRB) of the Minneapolis VA Medical Center and University of Minnesota School of Medicine. The Durham VA Medical Center IRB also approved using survey data for analysis.
The C-CARES Survey
The Cancer Care Assessment and Responsive Evaluation (C-CARES) survey was developed though a consortium of researches representing VA Health Services Research & Development, Department of Defense, National Cancer Institute, and the University of Minnesota. The goal of C-CARES was to obtain patient-reported symptoms, symptom management, and the patient-reported experience with the VA healthcare system among newly diagnosed colorectal cancer patients. A consensus panel of VA and non-VA researchers, psychometricians, and clinicians identified items for inclusion in the survey.
Patient Identification and Survey Mailing
Patients were identified through the VA Central Cancer Registry (VACCR). The VACCR uses custom software (OncoTraX) that integrates with the VA electronic health record system to identify all cancer cases diagnosed and treated within VA, making it a comprehensive resource for patient identification. It has been estimated that VACCR captures approximately 90% of cancer cases treated in VA.21
Our study aimed to survey 100% of eligible patients newly diagnosed with colorectal cancer in 2008. To be included in the survey cohort, patients had to meet the following eligibility criteria: 1) newly diagnosed with colorectal cancer during calendar year 2008, 2) received over half of their cancer care at any medical center in the VA healthcare system, and 3) be living at the time of the mailing. After attaining the initial list from the VACCR (n=2,555), a research assistant at the Minneapolis VA manually reviewed patients’ electronic medical record to confirm eligibility criteria, including vital status, and to identify the patient’s mailing address to which the survey would be sent. Surveys were mailed to 2,090 patients between August and November 2009.
The C-CARES survey was administered in paper-pencil format, mailed directly to the patients’ homes. The C-CARES survey was developed for an eighth grade reading level. A ten-dollar incentive was included in the survey packet.
A total of 1,409 surveys were returned, resulting in an overall response rate of approximately 67%. Individuals who indicated that they received most of their cancer care outside of the VA were excluded from analysis. After this secondary eligibility screening process, there were a total of 1,147 surveys remaining for analysis. Additional exclusion criteria were applied post-hoc. There were few female respondents (n=30). The small number of women rendered gender comparisons infeasible and there is reason to suspect that women may perceive barriers to care differently than their male counterparts.22 Therefore, women’s surveys were excluded from this analysis. Some surveys were returned with incomplete information regarding presence of symptoms or other key factors (n=116). Surveys missing this information were excluded. This resulted in a final number of 954 surveys for inclusion in analysis (Figure 1).
Figure 1.
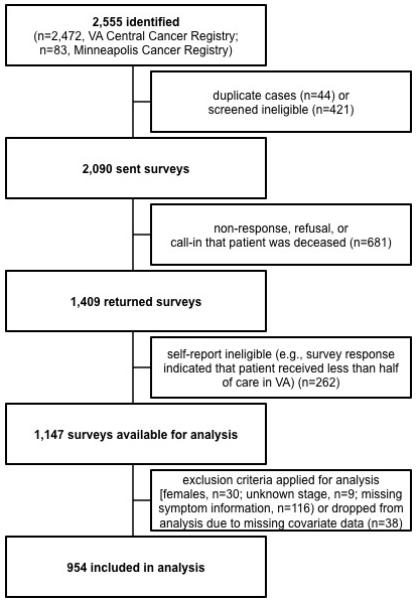
Survey Flow.
Outcome
The outcome variable, transportation difficulties, was derived from the following question in the C-CARES survey: “How often was it difficult to get transportation to or from your treatment or follow-up appointment?” Response options were: ‘does not apply’, ‘never’, ‘sometimes’, ‘often’ and ‘always’. Patients who responded in the latter two categories were coded as having a transportation barrier. Symptoms were assessed using dichotomized survey items from validated scales for fatigue, pain, and depression.
Explanatory Variables
Measures of patient characteristics, disease characteristics, and symptoms were included as explanatory and control variables. Attributes of the patient included age (continuous), race (categorical), employment status (binary), educational level (binary), and income (categorical). Age was measured as a continuous variable describing the age at diagnosis of CRC. Race information was aggregated into four mutually exclusive categories: white, black, Hispanic, or other race. There were two hierarchical sources of racial information. We first used the race category indicated by the respondent on the returned survey. However, race from the VA Central Cancer Registry was utilized if the patient failed to report a race on the C-CARES survey. The C-CARES survey served as the sole data source for employment status, educational level, and annual income. Respondents were coded as employed if they reported any, part-or full-time, employment. A binary variable was created to categorize educational level. Respondents who reported completing high school or higher-level education were coded as one; respondents who reported partial completion of high school or less education were coded as zero. Annual income was characterized in four distinct categories: less than $10,000, between $10,000 and $20,000, between $20,001 and $40,000, or greater than $40,000.
Low social support is a known predictor of transportation problems. 1,9,10,13 Many cancer patients rely on their social support network to transport them to necessary treatment and follow-up appointments. In order to assess the effect of social support on transportation, patients were asked, “If you had to choose, which person is most likely to help or take care of you, if you needed it?” Possible responses included: ‘my spouse’, ‘my daughter’, ‘my son’, ‘my boyfriend/girlfriend or partner’, ‘another family member’, ‘a friend or neighbor’, ‘other’, and ‘no one would help or take care of me’. Responses were mapped into three mutually exclusive variables indicating support from spouse, family and friends (apart from the spouse), or no one.
In addition to patient characteristics, we also controlled for disease characteristics and symptoms. Stage at diagnosis, a categorical variable, was included in the model. To assess symptom severity within the last six months, C-CARES contained validated PROMIS scales for depression, fatigue, and impact of pain.17,18 A t-score for each scale was calculated for every respondent. PROMIS scale t-score distributions are standardized such that the mean for the general U.S. population is 50 and the standard deviation around this mean is ten.18 Higher scores indicated greater severity of symptoms. In order for PROMIS scales to be meaningful, patients must respond to all survey items. PROMIS scale calculation would not be possible with incomplete data; surveys with missing information on any PROMIS symptom survey item were excluded from analysis.
To assess fatigue, the C-CARES survey contained the validated PROMIS fatigue scale that included six questions targeting presence of fatigue.17,23 “How often did you experience extreme exhaustion?” and “How often did you run out of energy?” are examples of two fatigue-related questions. Patients responded in one of the following categories for each fatigue question: ‘never’, ‘rarely’, ‘sometimes’, ‘often’, or ‘always’.
Similarly, the six validated PROMIS pain scale items were included in C-CARES.17,23 Two examples of pain questions include, “How much did pain interfere with your enjoyment of life?” and, “How much did pain interfere with your ability to concentrate?” Patients indicated either: ‘not at all’, ‘a little bit’, ‘somewhat’, ‘quite a bit’, or ‘very much’.
Depression was assessed using the eight questions from the validated PROMIS depression scale to assess problems with mood.17,23 Expressions of mood or depression problems included, “I felt worthless” and, “I felt that I had nothing to look forward to.” Response options included: ‘never’, ‘rarely’, ‘sometimes’, ‘often’, or ‘always’. The PROMIS scale t-scores were then calculated separated for pain, fatigue, and depression.18
Analysis
Statistical analyses were performed using Stata (StataCorp. 2007. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP). We conducted multivariable logistic regression analysis to determine the likelihood that patients with certain personal, disease, and symptom characteristics would report transportation-related barriers to receiving cancer treatment.
RESULTS
The respondents ranged in age from 26 to 90 years of age (Table 1). The mean age of respondents was 68 years, with a standard deviation of approximately 10. Respondents were predominately white (76%). Approximately 13% of respondents were black, 6% were Hispanic, and 5% reported another race. The majority of survey respondents reported their spouse as their primary source of social support (50%). Approximately 40% of survey respondents reported that another, non-spousal family member or friend cares for them. Nearly 5% reported no source of social support. The majority of respondents reported having a high school diploma or higher as their level of education (83%). Half of respondents reported an income of $10,000 to $20,000. However, 82% of respondents reported that they did not have either full- or part-time employment at the time of the survey response.
Table 1.
Characteristics of survey respondents (n=954)
| Percent | SD | Min | Max | |
|---|---|---|---|---|
| Patient Characteristics | ||||
| Age | 68.3 | 10.01 | 26 | 90 |
| Male | 100.0 | -- | -- | -- |
| White race | 76.4 | -- | -- | -- |
| Black race | 13.1 | -- | -- | -- |
| Hispanic | 5.6 | -- | -- | -- |
| Other race | 4.9 | -- | -- | -- |
| Employment and Educational Status | ||||
| Employed | 17.9 | -- | -- | -- |
| Not employed | 82.1 | -- | -- | -- |
| High school or higher education | 82.5 | -- | -- | -- |
| Less than high school education | 17.5 | -- | -- | -- |
| Annual Income | ||||
| < $10,000 | 16.0 | -- | -- | -- |
| $10,000 - $20,000 | 50.0 | -- | -- | -- |
| $20,001 - $40,000 | 23.6 | -- | -- | -- |
| > $40,000 | 10.4 | -- | -- | -- |
| Social Support | ||||
| Spouse | 50.1 | -- | -- | -- |
| Family and friends | 40.1 | -- | -- | -- |
| No one | 4.6 | -- | -- | -- |
| Stage at Diagnosis | ||||
| Stage I | 36.0 | -- | -- | -- |
| Stage II | 25.6 | -- | -- | -- |
| Stage III | 21.1 | -- | -- | -- |
| Stage IV | 17.4 | -- | -- | -- |
| Symptoms | ||||
| Fatigue | 52.9 | 9.7 | 32.5 | 82.7 |
| Pain | 51.1 | 10.6 | 41.0 | 78.3 |
| Mood problems | 50.5 | 10.9 | 37.1 | 81.1 |
Disease characteristics and symptoms were also examined. The greatest proportion of patients were diagnosed with Stage I disease (36%), followed by Stage II (26%), Stage III (21%), and Stage IV (17%). Respondents reported symptom levels of pain (mean=51.1, SD=10.6), fatigue (mean=52.9, SD=9.7), and depression (mean=50.5, SD=10.9) comparable to the mean PROMIS scale values.
A minority (19%) of respondents reported transportation barriers. While this number is relatively low, it is slightly higher than the 13-14% estimates among the broader cancer population.6 This number of patients suggests that transportation may be a meaningful barrier for one in five Veterans attempting to access cancer care within the VA healthcare system.
Multivariable logistic regression was utilized to examine determinants of experiencing transportation as a barrier to accessing cancer care. Having access to an informal caregiver had a strong statistically significant effect on the odds of transportation being a barrier to cancer care. Respondents who reported that a friend or family member would take care of them had two-times greater odds (OR=2.00, 95% CI=1.40, 2.87) of experiencing transportation problems than respondents who reported that their spouse would help them. Similarly, respondents who indicated that no one would take care of them had six-times greater odds (OR=6.13; 95% CI=3.10, 12.14) of experiencing transportation problems than patients who would rely on their spouse (Table 2).
Table 2.
Multivariate logistic regression results describing factors affecting transportation to cancer treatment (n=954)
| OR | 95% CI | p | |
|---|---|---|---|
| Patient Characteristics | |||
| Age | 1.00 | (0.98, 1.02) | 0.85 |
| Race | 1.21 | (0.99, 1.49) | 0.06 |
| Not employed† | 1.14 | (0.69, 1.90) | 0.60 |
| Less than high school education†† | 0.72 | (0.43, 1.20) | 0.21 |
| Annual Income ††† | |||
| < $10,000 | 1.86 | (0.89, 3.85) | 0.10 |
| $10,000 - $20,000 | 1.54 | (0.79, 3.00) | 0.20 |
| $20,001 - $40,000 | 1.16 | (0.56, 2.36) | 0.69 |
| Social Support †††† | |||
| Family and friends | 2.00 | (1.40, 2.87) | 0.00* |
| No one | 6.13 | (3.10-12.14) | 0.00* |
| Disease Characteristics & Symptoms | |||
| Stage | 0.96 | (0.82, 1.12) | 0.59 |
| Fatigue | 1.02 | (0.99, 1.05) | 0.10 |
| Pain | 1.04 | (1.02, 1.06) | 0.00* |
| Mood problems | 1.02 | (0.99, 1.04) | 0.11 |
Indicates statistical significance.
The referent employment status category is part- or full-time employment.
The referent educational category is completion of high school or greater.
The referent annual income category is >$40,000.
The referent social support category is spouse.
The effect of symptoms on experiencing a transportation barrier was also assessed. There was a statistically significant association between uncontrolled pain (OR=1.04; 95% CI=1.02, 1.06) and experiencing a transportation barrier. However, fatigue (OR=1.02; 95% CI=0.99, 1.05) and depression (OR=1.02; 95% CI=0.99, 1.04) were not associated with greater odds of experiencing a transportation problem.
Patient demographic characteristics and cancer stage were not found to have a statistically significant effect on the transportation barrier. Further, there was no association between age, race, stage at diagnosis, having attained less than a high school equivalent level of education, not having full- or part-time employment, or income on experiencing a transportation problem (Table 2).
DISCUSSION
Transportation is an important, yet often overlooked, element in the delivery of high quality and accessible cancer care.1,5,6,8,10,11,13 Patients with colorectal cancer may undergo surgery, chemotherapy, and in some cases, radiation therapy.24,25 Patients undergoing different types of treatment, based on stage and other disease characteristics, will interact with the healthcare system with varying frequency. As a result, transportation needs may vary at different points along the cancer care continuum. Receiving each of these services hinges on the patient’s ability to get to the needed care. Patients who may already be disadvantaged due to lack of social support or uncontrolled pain symptoms have increased odds of experiencing transportation barriers that limit access to cancer care.10,13,26,27
The results of the C-CARES survey indicate that VA colorectal cancer patients may experience transportation problems at an increased rate, approximately 19%, compared to the general U.S. cancer population. Among non-VA cancer patients, an estimated 13 to 14 percent report transportation as a barrier to receiving care.6 This may, in part, be due to where Veteran cancer patients live. The literature suggests that transportation barriers are highly associated with the geographic location where the patient resides.11,28,29 Further analyses are needed to assess whether region of the country or distance to care are predictors of transportation barriers among the VA cancer patient population.
Patients who are currently experiencing symptoms related to their cancer or cancer care may need ongoing treatment even more than asymptomatic patients. However, respondents who report problems with fatigue, pain, or their mood are more likely to have problems getting the needed transportation. This may place them at increased risk for ongoing, poorly controlled symptoms.
This study has limitations that should be considered. The C-CARES survey focused on patients with colorectal cancer. It is possible that patients with other forms of cancer may experience different transportation challenges. Additionally, the C-CARES survey was mailed to patients’ home addresses. Homeless and transient patients may not have a home address and therefore would not have been surveyed. Patients responding to this survey were not the sickest of all cancer patients in the VA. In order to be mailed a survey, patients must have survived a minimum of approximately nine months post-diagnosis and had to be well enough to respond. Furthermore, patients undergoing different types of treatment modalities may have differing transportation needs. Among C-CARES respondents, relatively few patients (19%) reported that transportation was a problem in getting to their cancer treatment. Future studies with a larger patient cohort should assess differences in experiencing a transportation barrier based on type of treatment received. The C-CARES survey was designed to globally understand patients’ experiences with cancer care. Assessing transportation was not a core element in the C-CARES instrument. As a result, several important variables were not included. C-CARES did not ask patients about their usual source of transportation to care (e.g. private car, public transportation), whether patients lived in a rural or urban area or region of the country. C-CARES also did not ask for patients’ service connected status. This is an important factor for determining patient eligibility for certain VA services at reduced or no cost. Furthermore, the analyses were based on cross-sectional data. Thus, the direction of the relationship between symptoms and transportation barriers is uncertain. It is possible that higher transportation barriers may result in worse symptom management. For example, clinicians may be more willing to prescribe opiates to the cancer patient in their examination room than for the cancer patient who telephone calls the clinic, but cannot be physically present for an appointment.
Based on the current analysis, it is not possible to determine that transportation is a causal barrier to cancer care. It is also feasible that poorly managed cancer care could result in transportation problems. Additional research is needed in this area.
CONCLUSION
VA colorectal cancer patients may experience transportation as a barrier to receiving cancer treatment. Patients who lack of social support or have poorly managed pain symptoms are more likely to experience problems with transportation to treatment. Screening patients for transportation problems should become a routine part of VA primary care or early cancer visits, particularly for elderly patients, minorities, and those known to reside in rural areas.
VA cancer care providers should be equipped to inform patients about available public and volunteer transportation options available. VA has widely offered transportation services including the Disabled American Veterans (DAV) transportation network and other hospital-driven or voluntary services.30
CLINICAL PRACTICE POINTS
Transportation is a known barrier to care for many cancer patients. Previous literature has documented that elderly patients8,9, those who live in rural areas1,5,8,10-12, minorities9, patients with lower annual household income 6,9,10,13, and patients with reduced social support.1,9,10,13 may be at increased risk for experiencing a transportation barrier. Much previous work focuses on cancer screening. This study suggests that VA colorectal cancer patients experience transportation as an access barrier to cancer care throughout their initial cancer treatment. This finding should impact the way that clinicians approach their colorectal cancer patients. Clinicians should be mindful that transportation is a problem for many patients and should screen them accordingly. Clinicians should also be equipped to inform patients about available public and volunteer transportation options available.
ACKNOWLEDGEMENTS
The authors acknowledge the statistical support and calculations provided by Deborah Finstad in Department of Family Medicine & Community Health and the University of Minnesota. This work was supported by the Inter-agency Quality of Cancer Care Committee, Applied Research Branch, National Cancer Institute through an Interagency Agreement with the Veterans Health Administration (IAG V246S-00054). During part of this work, Dr. Jackson held a Merit Review Entry Program award from the Veterans Affairs Health Services Research & Development Service (MRP-05-312). Dr. Provenzale was supported by an NIH K24 (DK002926-07).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Conflict of Interest: All authors have no conflicts of interest.
References
- 1.Arcury TA, Preisser JS, Gesler WM, Powers JM. Access to transportation and health care utilization in a rural region. J Rural Health. 2005;21(1):31–38. doi: 10.1111/j.1748-0361.2005.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 2.Guidry JJ, Greisinger A, Aday LA, Winn RJ, Vernon S, Throckmorton TA. Barriers to cancer treatment: a review of published research. Oncol Nurs Forum. 1996;23(9):1393–1398. [PubMed] [Google Scholar]
- 3.Heitman SJ, Au F, Manns BJ, Pattison P, Hilsden RJ. Nonmedical costs of colorectal cancer screening using CT colonography. J Am Coll Radiol. 2010;7(12):943–948. doi: 10.1016/j.jacr.2010.07.002. 10.1016/j.jacr.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 4.Peipins LA, Graham S, Young R, et al. Time and Distance Barriers to Mammography Facilities in the Atlanta Metropolitan Area. J Community Health. 2011 doi: 10.1007/s10900-011-9359-5. 10.1007/s10900-011-9359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldwin LM, Cai Y, Larson EH, et al. Access to cancer services for rural colorectal cancer patients. J Rural Health. 2008;24(4):390–399. doi: 10.1111/j.1748-0361.2008.00186.x. 10.1111/j.1748-0361.2008.00186.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shelby RA, Taylor KL, Kerner JF, Coleman E, Blum D. The role of community-based and philanthropic organizations in meeting cancer patient and caregiver needs. CA Cancer J Clin. 2002;52(4):229–246. doi: 10.3322/canjclin.52.4.229. [DOI] [PubMed] [Google Scholar]
- 7.Siegel K, Raveis VH, Houts P, Mor V. Caregiver burden and unmet patient needs. Cancer. 1991;68(5):1131–1140. doi: 10.1002/1097-0142(19910901)68:5<1131::aid-cncr2820680541>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 8.Goins RT, Williams KA, Carter MW, Spencer M, Solovieva T. Perceived barriers to health care access among rural older adults: a qualitative study. J Rural Health. 2005;21(3):206–213. doi: 10.1111/j.1748-0361.2005.tb00084.x. [DOI] [PubMed] [Google Scholar]
- 9.Mandelblatt JS, Yabroff KR, Kerner JF. Equitable access to cancer services: A review of barriers to quality care. Cancer. 1999;86(11):2378–2390. [PubMed] [Google Scholar]
- 10.Guidry JJ, Aday LA, Zhang D, Winn RJ. Cost considerations as potential barriers to cancer treatment. Cancer Pract. 1998;6(3):182–187. doi: 10.1046/j.1523-5394.1998.006003182.x. [DOI] [PubMed] [Google Scholar]
- 11.Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008;112(4):909–918. doi: 10.1002/cncr.23229. 10.1002/cncr.23229. [DOI] [PubMed] [Google Scholar]
- 12.Sankaranarayanan J, Watanabe-Galloway S, Sun J, Qiu F, Boilesen EC, Thorson AG. Age and rural residence effects on accessing colorectal cancer treatments: a registry study. Am J Manag Care. 2010;16(4):265–273. [PubMed] [Google Scholar]
- 13.Guidry JJ, Aday LA, Zhang D, Winn RJ. Transportation as a barrier to cancer treatment. Cancer Pract. 1997;5(6):361–366. [PubMed] [Google Scholar]
- 14.U.S. Census Bureau [Accessed March 12, 2011];Veterans - American FactFinder. http://factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_pageId=tp12_veterans.
- 15.U.S. Department of Veterans Affairs [Accessed November 7, 2010];VA National Transplant Program. http://www1.va.gov/TRANSPLANT/index.asp.
- 16.Bjordal K, Kaasa S. Psychometric validation of the EORTC Core Quality of Life Questionnaire, 30-item version and a diagnosis-specific module for head and neck cancer patients. Acta Oncol. 1992;31(3):311–321. doi: 10.3109/02841869209108178. [DOI] [PubMed] [Google Scholar]
- 17.DeWalt DA, Rothrock N, Yount S, Stone AA, PROMIS Cooperative Group Evaluation of item candidates: the PROMIS qualitative item review. Med Care. 2007;45(5 Suppl 1):S12–21. doi: 10.1097/01.mlr.0000254567.79743.e2. 10.1097/01.mlr.0000254567.79743.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reeve BB, Hays RD, Bjorner JB, et al. Psychometric evaluation and calibration of health-related quality of life item banks: plans for the Patient-Reported Outcomes Measurement Information System (PROMIS) Med Care. 2007;45(5 Suppl 1):S22–31. doi: 10.1097/01.mlr.0000250483.85507.04. 10.1097/01.mlr.0000250483.85507.04. [DOI] [PubMed] [Google Scholar]
- 19.Sprangers MA, te Velde A, Aaronson NK. The construction and testing of the EORTC colorectal cancer-specific quality of life questionnaire module (QLQ-CR38). European Organization for Research and Treatment of Cancer Study Group on Quality of Life. Eur J Cancer. 1999;35(2):238–247. doi: 10.1016/s0959-8049(98)00357-8. [DOI] [PubMed] [Google Scholar]
- 20.Cella D, Riley W, Stone A, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005-2008. J Clin Epidemiol. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jackson GL, Melton LD, Abbott DH, et al. Quality of nonmetastatic colorectal cancer care in the Department of Veterans Affairs. J Clin Oncol. 2010;28(19):3176–3181. doi: 10.1200/JCO.2009.26.7948. 10.1200/JCO.2009.26.7948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Friedemann-Sanchez G, Griffin JM, Partin MR. Gender differences in colorectal cancer screening barriers and information needs. Health Expect. 2007;10(2):148–160. doi: 10.1111/j.1369-7625.2006.00430.x. 10.1111/j.1369-7625.2006.00430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institute of Health [Accessed March 12, 2011];Patient-Reported Outcome Measurement Information System. http://www.nihpromis.org/default.aspx.
- 24.Engstrom PF, Arnoletti JP, Benson AB, 3rd, et al. NCCN Clinical Practice Guidelines in Oncology: colon cancer. J Natl Compr Canc Netw. 2009;7(8):778–831. doi: 10.6004/jnccn.2009.0056. [DOI] [PubMed] [Google Scholar]
- 25.Engstrom PF, Arnoletti JP, Benson AB, 3rd, et al. NCCN Clinical Practice Guidelines in Oncology: rectal cancer. J Natl Compr Canc Netw. 2009;7(8):838–881. doi: 10.6004/jnccn.2009.0057. [DOI] [PubMed] [Google Scholar]
- 26.van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, Schouten HC, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18(9):1437–1449. doi: 10.1093/annonc/mdm056. 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- 27.Ward SE, Goldberg N, Miller-McCauley V, et al. Patient-related barriers to management of cancer pain. Pain. 1993;52(3):319–324. doi: 10.1016/0304-3959(93)90165-L. [DOI] [PubMed] [Google Scholar]
- 28.Wallace AE, MacKenzie TA, Wright SM, Weeks WB. A cross-sectional, multi-year examination of rural and urban Veterans Administration users: 2002-2006. Mil Med. 2010;175(4):252–258. doi: 10.7205/milmed-d-09-00048. [DOI] [PubMed] [Google Scholar]
- 29.Cully JA, Jameson JP, Phillips LL, Kunik ME, Fortney JC. Use of psychotherapy by rural and urban veterans. J Rural Health. 2010;26(3):225–233. doi: 10.1111/j.1748-0361.2010.00294.x. 10.1111/j.1748-0361.2010.00294.x. [DOI] [PubMed] [Google Scholar]
- 30.Disabled American Veterans [Accessed March 12, 2011];Disabled American Veterans - Need a Ride? http://www.dav.org/volunteers/Ride.aspx.


