Abstract
Objectives
Advances in biopsychosocial science have underlined the importance of taking social history and life course perspective into consideration in primary care. For both clinical and research purposes, this study aims to develop and validate a standardised instrument measuring both material and social deprivation at an individual level.
Methods
We identified relevant potential questions regarding deprivation using a systematic review, structured interviews, focus group interviews and a think-aloud approach. Item response theory analysis was then used to reduce the length of the 38-item questionnaire and derive the deprivation in primary care questionnaire (DiPCare-Q) index using data obtained from a random sample of 200 patients during their planned visits to an ambulatory general internal medicine clinic. Patients completed the questionnaire a second time over the phone 3 days later to enable us to assess reliability. Content validity of the DiPCare-Q was then assessed by 17 general practitioners. Psychometric properties and validity of the final instrument were investigated in a second set of patients. The DiPCare-Q was administered to a random sample of 1898 patients attending one of 47 different private primary care practices in western Switzerland along with questions on subjective social status, education, source of income, welfare status and subjective poverty.
Results
Deprivation was defined in three distinct dimensions: material (eight items), social (five items) and health deprivation (three items). Item consistency was high in both the derivation (Kuder-Richardson Formula 20 (KR20) =0.827) and the validation set (KR20 =0.778). The DiPCare-Q index was reliable (interclass correlation coefficients=0.847) and was correlated to subjective social status (rs=−0.539).
Conclusion
The DiPCare-Q is a rapid, reliable and validated instrument that may prove useful for measuring both material and social deprivation in primary care.
Article summary
Article focus
This study aims to identify and test the relevance of existing indicators of deprivation to help clinicians investigate social status.
We constructed and validated an individual-level measurement of deprivation for patients attending their general practitioner: the deprivation in primary care questionnaire (DiPCare-Q).
Key messages
The DiPCare-Q proposes a reliable, validated instrument for screening and measuring deprivation among patients in developed countries.
Compared with usual indicators of socioeconomical status, the DipCare-Q index gives important additional information on subjective social status and state of deprivation.
Social deprivation is an important aspect of deprivation in general and needs to be distinguished from material deprivation.
Strengths and limitations of this study
Compared with socioeconomical status, self-reported perceived signs of deprivation are more relevant in identifying potential underlying social distress. However, the DiPCare-Q only identifies signs of deprivation without highlighting their reasons.
To improve public health and limit effects of health disparities, detecting deprivation also requires physicians to know how this is to affect their relation with their patient's in a beneficial way.
Background
Social determinants have been identified as risk factors for many diseases or behaviours that have an important global impact on health.1–4 This fact affects not only the most disadvantaged but can be observed throughout the social gradient5 6 and is not explained by health behaviour differences alone.7 Stress engendered by an individual's social environment is suggested to be an alternative biological explanation.8–10 In the early 1990s, Townsend11 identified material or social inequities that could engender such stress. These conditions of deprivation are reversible. Therefore focusing on these social conditions and their impact on health is a promising field for diminishing the total health burden.12 13 This has been promoted at the community level,14 15 but little is known about handling deprivation on an individual level which nevertheless seems to be part of a general practitioner's (GP's) daily work.16 GPs undeniably also play a central role in healthcare by adapting treatments and prevention to their patients' state of deprivation.17 18 Detecting and questioning patients on their state of deprivation, objective and subjective, is therefore the first step towards developing future social interventions.19 A validated individual deprivation index is becoming an essential consideration for clinicians, epidemiologists and public health workers in order to relate social aspects to overall health.
Using Townsend's11 20 concepts of deprivation and selecting factors compatible with Marmot's health determinants,21 this project aims to develop and evaluate a psychometric individual-level measurement of deprivation for patients attending their GP: the deprivation in primary care questionnaire (DiPCare-Q) index.
Methods
The development of the DiPCare-Q was planned in six stages running from March 2008 to April 2011. These were item generation, questionnaire construction and face validity, derivation and reliability study (reduction, consistency, test–retest reliability), content validity, translation and a validation study of the final instrument (consistency, concurrent validity). All patients gave their informed consent to participate. Ethical approval was obtained from the official state Biomedical Ethical Committee under reference number 157/09 for the derivation study and reference number 155/10 for the validation study.
Stage 1: item generation
We identified potential items related to the concept of deprivation through a systematic review and extracted existing questions investigating deprivation at an individual level. Medline, Cochrane, Scopus, ISI web, PsycINFO and Francis were searched. Our methodology identified 12 articles that studied individual-level indicators of deprivation. Two authors extracted data independently and identified a total of 199 different questions related to deprivation.
Stage 2: questionnaire construction and face validity
Items extracted from each study were categorised and organised to respect Townsend's definition of deprivation.11 20 Labels for subcategories were chosen in respect to factors identified as health related by Marmot's21 structure of social determinants (table 1). Using judgemental item quality, four authors discussed, modified and selected items to be retained. They discarded questions, basing their judgement on clarity of expression, the question's relevance to patients attending a GP, the fact that people with low literacy levels must be able to answer, appropriateness at an individual level, simplicity of answers, gender specificity, the potential invasiveness of an item and the risk of response bias if the question would be asked by a GP.
Table 1.
Conceptual construction of components defining deprivation in primary care
| Dimensions of deprivation | Categories | Number of items |
||
| Retrieved from systematic review | DiPCare-Q38 | DiPCare-Q16 | ||
| Material deprivation | Dietary | 9 | 1 | 1 |
| Clothing | 5 | 1 | 1 | |
| Housing | 53 | 4 | 2 | |
| Transport | 6 | 1 | ||
| Environmental | 13 | 1 | ||
| Financial burden | 10 | 3 | 3 | |
| Societal security | Healthcare | 3 | 1 | 1* |
| Work | 5 | 2 | ||
| Access to social welfare | 3 | 1 | ||
| Criminality | 3 | – | ||
| Education | 4 | 1 | ||
| Social relationship | Social isolation | 17 | 4 | 2† |
| Discrimination | 3 | 1 | ||
| Family/friends | 21 | 5 | 1 | |
| Work | 13 | 2 | ||
| Leisure/recreational | 6 | 3 | 2 | |
| Health deprivation | Physical | 3 | 1 | 1 |
| Psychiatry | 6 | 2 | 2 | |
| Time perspective | 9 | 1 | ||
| Self-esteem/autonomy | 7 | – | ||
| Health literacy | – | 3 | ||
| Total | 199 | 38 | 16 | |
Was retained as an indicator of material deprivation.
Not having access to the internet revealed itself to be a good indicator of social deprivation but was initially falsely presumed to be related to material deprivation (housing).
DiPCare-Q, deprivation in primary care questionnaire.
Face validity of the 38 retained questions was first assessed by three separate groups: 20 GPs working in private practices, five experienced researchers in the field of general practice and 10 individual patients from different socioeconomic backgrounds. Based on their comments, questions were rephrased and validated by six authors. This final version was tested by eight hospital cleaning employees using a thinking aloud approach.22 The final version of the deprivation questionnaire was validated by all authors.
Stage 3: derivation and reliability study
The aim of this stage was to reduce the number of questions required to assess deprivation and to measure the consistency and the reliability of the derived instrument. This monocentric test–retest study recruited 200 randomly selected patients attending their GP during their planned visits to a general internal medicine clinic at an academic medical institution in Switzerland during 2 months. The study was expressly designed not to exclude patients with psychiatric comorbidities, cognitive disorders or reading difficulties. Once the questionnaire was completed, a second appointment was scheduled within the following 3 days, so that the 38 questions related to deprivation could be asked again over the phone by an independent researcher blinded to the first set of answers. All data were manually entered into the database. Double entry prevented transcription errors.
Stage 4: content validity
Content validity was assured by asking by mail a convenient sample of 50 GPs professionally active in the French speaking part of Switzerland to subjectively rate the ‘quality’ of each item on a 8-point Likert scale.
Stage 5: translation of the instrument
Professional interpreters translated the DiPCare-Q into English, German and Italian (available online as supplementary material). Each translated version was then reverse translated into French again by another interpreter blinded to the original text. When reverse translation was discordant with original text, translators discussed the discrepancy until the issue was solved.
Stage 6: validation study
Forty-seven GPs working independently in primary care practices in Switzerland (cantons of Geneva, Vaud, Fribourg, Valais and Neuchâtel) were recruited to serve as investigators. A random sample of 1898 patients was questioned between September 2010 and February 2011. To be included, patients had to be over 16 years of age and have a prescheduled day visit to the GP's office. Patients also had to understand French, German, Italian or English. They were invited to fill out the self-administered questionnaire in the waiting room. Physicians were blinded to the responses that were returned in a sealed envelope. Data management staff checked returned material and obtained missing data by phone, including for material sent back by patients who could not read or write. All questionnaires were scanned for data entry.
Data analysis
For the derivation study, we first discarded questions with Cohen's κ coefficients <0.4 or those with an item-rest correlation (IRC) of ≥0.2. Assuming that indicators of material, social and health deprivation can be ordered in degree of difficulties (hierarchical property), we used Mokken Scale Procedure (MSP) to select items for each subscale. Items with a Loevinger Hi coefficient <0.3 were ruled out. Internal consistency and reliability of retained items for the overall index were measured using Kuder-Richardson Formula 20 (KR20). Coefficients for each item were calculated to best-fit patients' subjective social status using regression analysis. Test–retest reliability of the DiPCare-Q was measured using one-way random effect interclass correlation coefficients (ICC2,1). Content validity was estimated by averaging 17 physicians' appreciations of representativeness for each item on an 8-point Likert scale ranging from 1 (not at all representative) to 8 (extremely representative). For concurrent validity, we used the international definition of relative poverty adapted to family income using the modified equivalence scale from the Organisation for Economic Co-operation and Development (OECD)23 and using the yearly income of Swiss Francs CHF 28 700—as a cut-off point for relative poverty.
Sample size for the derivation study was calculated24 to assure that the κ coefficient would be different from 0.6 with power set at 0.8 and significance level at 0.05, expecting a κ of 0.9 for traits present in at least 10% of patients. The number of patients calculated to be included in the analysis would be 149. Expecting 8% missing data and 25% of patients lost in follow-up, the number of patients to be recruited was set at 200. The validation study was nested in a transversal survey that required 2000 participants in order to detect differences in the prevalence of deprivation between physicians.
Results
Derivation and reliability study
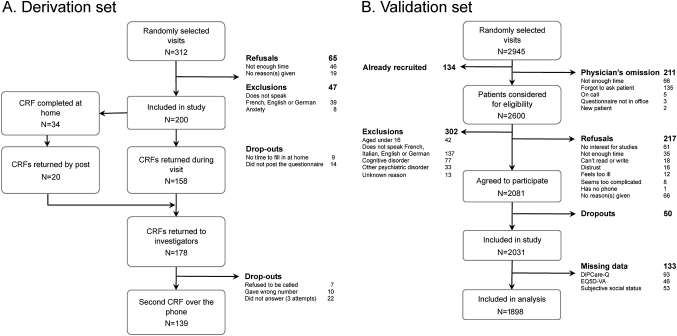
Data were available from 178 patients. Reasons for refusal and/or dropout are given in figure 1A. Patients were aged between 17 and 89 years with a mean and median of 47 years of age. Both genders were equally represented (45.7% female). Twenty-three per cent (41 of 178) of the patients required assistance to answer the questionnaire due to poor literacy or psychiatric comorbidities. A slight majority of patients (50.9%) did not have Swiss nationality. Sixty-two patients (34.8%) were receiving social benefits.
Figure 1.
Flow chart giving reasons for refusals and dropouts. (A) Derivation study, (B) validation study. N, number of patients; CRF, case report form.
Deriving the DiPCare-Q index
The first step was item number reduction. Three items showed poor test–retest reliability and were therefore set aside: understanding the physician (κ=0.175), being a single parent (κ=0.191) and living in overcrowded conditions (κ=0.266). Eleven items had an IRC <0.2 and were set aside stepwise: being an elderly person living alone (IRC=−0.09), experiencing difficulty at work (IRC=−0.02), not knowing where to obtain social aid (IRC=0.06), having no associative activity (IRC=0.07), lack of transport (IRC=0.12), having more than two children (IRC=0.13), not having completed compulsory education (IRC=0.13), having difficulties in reading (IRC=0.14), moving home frequently (IRC=0.15), having an elderly or handicapped person at home (IRC=0.17) and having difficulties with numbers (IRC=0.17).
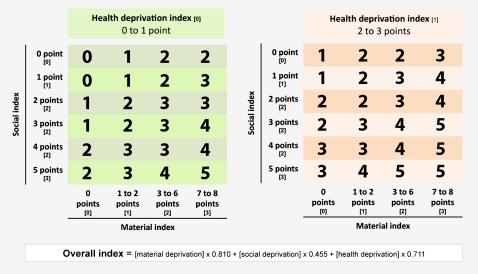
Non-parametrical Mokken scaling identified societal security deprivation not to be a relevant dimension for the studied population as items from this dimension were not related to each other. Items from this dimension were therefore tested as indicators of other dimensions of deprivation. MSP identified eight items which were not related to material, social or health deprivation: inappropriate housing, conflict with a partner, having lost his/her job, having a sick family member, suffering from discrimination, suffering from post-traumatic syndrome, benefiting from paid annual leave and being appropriately insured for his/her retirement. Our analysis revealed that financial barriers to accessing healthcare were more related to material deprivation than to societal security deprivation, and not having access to the internet was consistent with social and not material deprivation. Sixteen items were therefore retained to constitute the DiPCare-Q: eight for material deprivation, five for social deprivation and three for health deprivation. The overall internal consistency of the DiPCare-Q was KR20=0.827 (equivalent to Cronbach's α for binomial variables). Table 2 provides frequency of positive answers, item variance, IRC, Loevinger H coefficients, item test–retest reliability and items weight for each subindex (material, social and health deprivation). Subindexes for material, social and health deprivation were calculated adding one point for each positive answer. Social deprivation and health indexes could be assumed to be linearly correlated to subjective social status, whereas material deprivation could not. Using linear regression, the DiPCare-Q index was constructed and simplified for clinical use (figure 2). This final model was linearly correlated to subjective social status (rP=0.613).
Table 2.
Retained items included in the DiPCare-Q with psychometric values
| Dimensions | Items (question number) | Item frequency (prevalence) |
Loevinger H coefficients |
Item-rest correlation |
Reliability | Content validity* | Subindex coefficients | |||
| Derivation set (%) | Validation set (%) | Derivation set | Validation set | Derivation set | Validation set | Cohen's κ | Mean (SD) | |||
| Material | Difficulties paying bills (D1) | 55.6 | 25.7 | 0.614 | 0.651 | 0.480 | 0.546 | 0.570 | 7.2 (1.0) | 1 |
| Need to borrow money for daily expense (D2) | 38.8 | 13.6 | 0.506 | 0.469 | 0.496 | 0.412 | 0.755 | 7.4 (0.8) | 1 | |
| Limited access to healthcare (D3) | 19.1 | 10.7 | 0.448 | 0.422 | 0.422 | 0.375 | 0.597 | 7.4 (0.8) | 1 | |
| Scared of losing housing (D4) | 23.0 | 4.5 | 0.448 | 0.458 | 0.419 | 0.328 | 0.727 | 7 (1.6) | 1 | |
| Can't afford clothes (D5) | 40.5 | 17.3 | 0.553 | 0.529 | 0.564 | 0.561 | 0.675 | 6.9 (1.2) | 1 | |
| Can't afford furniture (D6) | 38.8 | 19.1 | 0.530 | 0.501 | 0.564 | 0.475 | 0.550 | 6.2 (1.3) | 1 | |
| Not enough to eat at home (D10) | 17.4 | 5.6 | 0.638 | 0.434 | 0.579 | 0.326 | 0.571 | 7.9 (0.8) | 1 | |
| Difficulties reimbursing loan(s) (D13) | 29.2 | 13.8 | 0.492 | 0.503 | 0.471 | 0.504 | 0.573 | 5.9 (1.6) | 1 | |
| Social | No holidays (D7) | 60.1 | 39.1 | 0.365 | 0.372 | 0.324 | 0.430 | 0.801 | 5.2 (2.3) | 1 |
| No evening(s) spent with family or friends (D8) | 29.2 | 16.1 | 0.493 | 0.502 | 0.562 | 0.428 | 0.719 | 5.5 (2.3) | 1 | |
| No cultural activities (D9) | 61.2 | 49.4 | 0.444 | 0.468 | 0.398 | 0.427 | 0.804 | 5.2 (2.3) | 1 | |
| No access to the internet (D11) | 42.1 | 25.5 | 0.369 | 0.360 | 0.303 | 0.192 | 0.791 | 3.4 (2.1) | 1 | |
| No one to turn to for material support (D12) | 43.3 | 31.8 | 0.344 | 0.309 | 0.283 | 0.284 | 0.545 | 6.1 (2.1) | 1 | |
| Health | Physical handicap (D14) | 29.2 | 21.5 | 0.339 | 0.308 | 0.339 | 0.266 | 0.515 | 6.6 (1.2) | 1 |
| Psychic handicap (D15) | 33.2 | 17.0 | 0.398 | 0.355 | 0.398 | 0.343 | 0.565 | 7 (1.1) | 1 | |
| Addiction (D16) | 16.9 | 5.5 | 0.370 | 0.222 | 0.370 | 0.154 | 0.593 | 7.2 (1.0) | 1 | |
Content validity was measured on an 8-point Likert scale ranging from 1 to 8. Consistency was measured for 178 patients for the derivation set and for 1898 patients for the validation set, reliability for 139 and content validity by 17 physicians.
Figure 2.
Calculation table for the DiPCare-Q index ranging from 0 to 5 using subindexes corresponding to material, social and health deprivation.
Reliability of the DiPCare-Q
Data for reliability analysis were available for 139 patients. Overall, the DiPCare-Q index showed a good test–retest reliability with an ICC=0.847 (95% CI 0.79 to 0.89). Reliability was better for material (ICC=0.852) and social (ICC=0.865) deprivation indexes than for the health deprivation index (ICC=0.606), which was measured before and after the visit to the GP.
Content validity
Eighteen physicians agreed to participate. Seventeen sent back their appreciation of the appropriateness of every item on an 8-point Likert scale (table 2). Overall, items from material deprivation (mean=7.0; 95% CI 6.7 to 7.3) and health deprivation (mean=7.0; 95% CI 6.5 to 7.4) were considered more appropriate than those from social deprivation (mean=5.1; 95% CI 4.2 to 5.9).
Validation study
The total number of patients included in the study was 2031. Full data were, however, only available for 1898 patients. Details on exclusions, refusals and dropouts are given in figure 1B. Patients' age ranged from 16 to 94 years (median 57 years), 58.4% were women, 18.9% did not have the Swiss nationality but only 1.7% of questionnaires (n=32) were answered in another language than French. 73.4% of patients completed their education after compulsory school including apprentices and 61.1% lived with a partner. Using the definition OECD definition of poverty, 7.3% of patients (n=118) lived in a household that was considered as poor.
In the validation study, the overall internal consistency of the DiPCare-Q was KR20=0.778. Item frequency, IRC and Loevinger H coefficients are reported in table 2. Material, social and health deprivation indexes had a total Loevinger H coefficients of 0.505, 0.394 and 0.310, respectively, supporting the hierarchical properties of each subindex.
Material (rs=−0.486), social (rs=−0.432) and health (rs=−0.263) deprivation were all correlated to subjective social status to a greater extent than to family income or education level. The DiPCare-Q index showed higher correlations to subjective social status (rs=−0.539) than to family income (rs=−0.480), OECD's definition of relative poverty (rs=0.202), receiving welfare benefits (rs=0.288) or education level (rs=−0.328). Finally, when modelling subjective social status, adding the DiPCare-Q index to age, education, gender, family income, poverty and receiving welfare assistance increased the proportion of explained variance from 27.0% to 38.4% (p<0.0001).
Translated versions of the questionnaire
The French version—and professionally translated versions in English, German and Italian—of the final 16-item DiPCare-Q are available online (supplementary material). They can be used free of charge, without the express authorisation of the authors, if the present article is referred to.
Discussion
Before proposing a new measuring instrument, we critically investigated the true need for a new deprivation index adapted to primary care. Three existing instruments were identified through our systematic review: the NZiDep, the Factor Weighted Index of Deprivation and the EPICES score (table 3). These instruments were found to be poorly adapted to our Swiss primary care setting; they included items that were specific to other social or cultural habits and were therefore inapplicable to our multicultural population.
Table 3.
Items included in different deprivation measuring instruments (classified by the authors of this article)
| NZiDep25 | FWID26 | EPICES27 | DiPCare-Q | |
| Material deprivation |
|
|
|
|
| Social deprivation |
|
|
|
|
| Societal security/working conditions |
|
|
||
| Health deprivation |
|
|
|
DiPCare-Q, deprivation in primary care questionnaire; FWID, factor weighted index of deprivation.
Using Townsend's concept of deprivation, the NZiDep25 constructed an eight-item score adapted to populations from different cultural backgrounds in New Zealand. This instrument, however, exclusively investigates material deprivation and does not therefore correspond to the broader definition of deprivation developed by Lee and Townsend20 and perceived by GPs.28 Including social aspects of deprivation is particularly important to healthcare, as psychosocial context has been shown to affect health.29 The same criticism can be made of the Factor Weighted Index of Deprivation,26 which only investigated monetary, consumption and work-related deprivation. Eroglu's fieldwork however supports our observations regarding the importance of including subjective questions and household-level questions when measuring deprivation. The EPICES score was designed to identify deprived individuals in French Health Examination Centres.30 It was constructed on the same conceptual basis as the DiPCare-Q. Compared with the DiPCare-Q, the EPICES score included more items on social deprivation. It also showed lower internal consistency (Cronbach's α=0.410) compared with other instruments. The EPICES score was nevertheless much more relevant in predicting unhealthy behaviours than either the administrative legal definition of deprivation or socioeconomic characteristics.27
Using pre-existing questions on deprivation issued from this systematic review, we therefore conceptualised, identified and constructed a 38-item questionnaire to be reduced in size following data collection from patients attending a general internal medicine clinic at an academic medical institution. MSP then made it possible to retain 16 questions and to organise the DiPCare-Q in three dimensions: material deprivation, social deprivation and health deprivation. Our instrument showed acceptable psychometric properties. Items were consistent with one another (KR20=0.778) and all of them reached moderate levels of agreement; the DiPCare-Q seems highly reliable (ICC=0.847), and concurrent validity showed the DiPCare-Q to be an important indicator of patients' subjective social status5 compared with other social status indicators. Like subjective social status, deprivation is a culturally based subjective state as its definition depends greatly upon what we expect to have under normal circumstances. This allows us to believe the DiPCare-Q to be a better surrogate of ‘deprivation’ than measures of income when used on populations requiring healthcare. Finally, the high heterogeneity of the profiles of patients within the study improves the DiPCare-Q's external validity. Apart from asylum seekers and undocumented migrants (who were included in the derivation study), all Swiss residents have access to private practices whose costs are covered by their compulsory health insurance. The studied population is therefore representative of many different cultural backgrounds and this leads us to believe that the DiPCare-Q could show similar psychometric properties in clinical settings for most Western European countries.
Townsend's conceptual separation of material and social deprivation31 and its importance in defining deprivation seems, for patients from developed countries but also characterised by social inequalities, to be confirmed by our study. Social deprivation could even be, in countries with very high standards of living such as Switzerland, more important than material deprivation as lack of social support from the community and family32 is more frequent in places where living standards are higher. This aspect underlines the effects on individual health of the personal state of isolation and anxiety resulting from a lack of social integration (anomy). Furthermore, helping patients handle psychosocial stress has been shown to be effective in improving their health,33 34 whereas improving their financial situation has revealed itself to be much more complicated.35
In clinical practice, relying on a standardised questionnaire for detecting deprivation could have its downfalls. Improving the detection of social difficulties assumes that this will change the way physicians relate to their patient. In a public healthcare perspective, this could be positive if physicians favour behaviours against existing disparities.36 37 On the other hand, it could increase health disparities if physicians tend to disfavour the most deprived. Inappropriate response to poverty has been recognised as a major barrier in preventing its negative effects on health.38 This underlines physicians' responsibility of correctly handling such information. Therefore, detecting deprivation also requires physicians to express empathy and adapt their behaviour for their patient's benefit.39 40
Our study has several limitations. First, we cannot exclude other phenomenon from being implicated in deprivation such as work conditions. Contrarily to the Whitehall and the GAZEL studies,7 our study also included the retired, housewives, the self-employed and students who often do not feel deprived even if they do not benefit from favourable working conditions. This might have confounded the true relationship between working conditions and workers' feeling of deprivation. Our observations should therefore not prevent clinicians from investigating working conditions for those who are employed or those who experience unemployment. Second, our conceptual framework was designed for patients in primary care in developed countries. Given the multiplicity of deprivation factors, the psychometric properties of the deprivation index questionnaire could however be applicable to other populations characterised by objective and subjective deprivation. Third, relevant items might have been falsely discarded due to the lack of power of the derivation study. The sample size (n=178) is below the recommended number of 200 for using MSP. However, the studied sample being highly deprived, we believe that this small difference does not affect the internal validity of our results. Finally, we cannot exclude social desirability bias from having influenced responses on health deprivation status before and after the visit to the physician.
Conclusions
The promising psychometric properties of the DiPCare-Q allow us to believe that it could be used as an indicator of the patient's material and social state of deprivation. This deprivation index is a promising screening instrument to improve clinical investigations by measuring potential underlying social problems which could affect health.41 42 Furthermore, this instrument could improve more broadly the understanding of social and material deprivation by serving as a reliable individual measure in future observational and experimental studies.
Supplementary Material
Acknowledgments
We thank Adelaïde Rosset who contacted patients over the phone for the derivation study and Catherine Delafontaine who managed and completed data for the validation study. We also thank David Brook who revised and corrected our English through his English Language Coaching service (ELCS). We especially thank the 47 GPs, coinvestigators for the validation study, who recruited patients and offered us their precious time without receiving any financial return: Gilbert Abetel, Jacques Aubert, Elisabeth Becciolini-Lebas, Corinne Bonard, Robert Bourgeois, Jacques Carrel, Georges Conne, Christian Cuendet, Michel Dafflon, Gabrielle de Torrente, Pierre De Vevey, Maryse De Vevey, Hedy Decrey, Charles Dvorak, Frédéric Fellrath, Elisabeth Flammer, Francine Glassey-Perrenoud, Nils Gueissaz, Jean-Luc Held, Lilli Herzig, Blaise Ingold, Nicole Jaunin, Sébastien Jotterand, Michel Junod, Philippe Krayenbuhl, Maxime Mancini, Jacques Meizoz, Alain Michaud, Marie Neeser, Marie-Amélie Pernet, Antonio Petrillo, François Pilet, Michel Ravessoud, Laurent Rey, Joël Rilliot, Xavier Risse, Pierre-Yves Rodondi, Olivier Rubli, Laurent Schaller, Pierre-Alain Schmied, Alain Schwob, Paul Sébo, Johanna Sommer, Anne-Lise Tesarik-Vouga, Rodrigo Vasquez, François Verdon, Daniel Widmer.
Footnotes
To cite: Vaucher P, Bischoff T, Diserens EA, et al. Detecting and measuring deprivation in primary care: development, reliability and validity of a self-reported questionnaire: the DiPCare-Q. BMJ Open 2012;2:e000692. doi:10.1136/bmjopen-2011-000692
Contributors: PV designed the systematic review; PV, E-AD and PB selected articles; PV and E-AD extracted data from articles; PV, E-AD, PB and TB validated the categorisation of items and formulated the initial questionnaire. E-AD interviewed patients and hospital cleaning personnel to validate and improve questionnaire. PV, TB and PB planned and collected data for face validity with general practitioners. For the derivation study, PV, E-AD, PB, TB, CS, GM-A and BF participated to the design of the study; PV wrote the protocol; PV and E-AD recruited patients and collected data, Adelaide Rosset contacted patients over the phone 3 days after enrolment. For the validation study, PV, PB, TB, FP, LH and BF participated to the design of the study; PV wrote grant applications and the protocol; LH recruited physicians; Catherine Delafontaine trained physicians and managed data entry and quality control; Isabelle Cardoso entered data and Estelle Martin managed the forms for scanned entry. PV analysed the data; all authors discussed the results and participated to the draft outline. PV wrote the manuscript under the supervision of PB. All authors read and approved the final manuscript. The final manuscript was corrected by David Brooks's English Language Coaching service (ELCS). PV serves as guarantors of the paper and accepts full responsibility for the work and the conduct of the study.
Funding: Swiss Academy of Medical Science, by the Department of Social Action and Health of the Canton of Vaud and by the Faculty of Biology and Medicine from the University of Lausanne.
Competing interests: None.
Patient consent: Signed consent was obtained during the derivation study. For the validation study, oral and written information were given to participants. The physician obtained oral consent before handing out the questionnaire. Patients were clearly informed that returning the questionnaire meant they approved participating.
Ethics approval: Ethical approval was obtained from the official state Biomedical Ethical Committee under reference number 157/09 for the derivation study and reference number 155/10 for the validation study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The DiPCare-Q in English, French, German and Italian is made openly accessible to all on the web with a link on http://bmj.com. Instructions and STATA commands to calculate the DiPCare-Q index are also provided.
References
- 1.Marmot M, Friel S, Bell R, et al. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008;372:1661–9 [DOI] [PubMed] [Google Scholar]
- 2.Ansari Z, Carson NJ, Ackland MJ, et al. A public health model of the social determinants of health. Soz Praventivmed 2003;48:242–51 [DOI] [PubMed] [Google Scholar]
- 3.Feinstein JS. The relationship between socioeconomic status and health: a review of the literature. Milbank Q 1993;71:279–322 [PubMed] [Google Scholar]
- 4.Egan M, Tannahill C, Petticrew M, et al. Psychosocial risk factors in home and community settings and their associations with population health and health inequalities: a systematic meta-review. BMC Public Health 2008;8:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: its determinants and its association with measures of ill-health in the Whitehall II study. Soc Sci Med 2003;56:1321–33 [DOI] [PubMed] [Google Scholar]
- 6.Goldberg M, Melchior M, Leclerc A, et al. Epidemiologie et determinants sociaux des inegalites de sante. Rev Epidemiol Sante Publique 2003;51:381–401 [PubMed] [Google Scholar]
- 7.Stringhini S, Dugravot A, Shipley M, et al. Health behaviours, socioeconomic status, and mortality: further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med 2011;8:e1000419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaufman JS, Cooper RS. Seeking causal explanations in social epidemiology. Am J Epidemiol 1999;150:113–20 [DOI] [PubMed] [Google Scholar]
- 9.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 2001;30:668–77 [DOI] [PubMed] [Google Scholar]
- 10.Lorant V, Croux C, Weich S, et al. Depression and socio-economic risk factors: 7-year longitudinal population study. Br J Psychiatry 2007;190:293–8 [DOI] [PubMed] [Google Scholar]
- 11.Townsend P. Deprivation and ill health. Nursing (Lond) 1991;4:11–15 [PubMed] [Google Scholar]
- 12.Krieger N. Why epidemiologists cannot afford to ignore poverty. Epidemiology 2007;18:658–63 [DOI] [PubMed] [Google Scholar]
- 13.Barten F, Mitlin D, Mulholland C, et al. Integrated approaches to address the social determinants of health for reducing health inequity. J Urban Health 2007;84(3 Suppl):i164–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Whitehead M. The concepts and principles of equity and health. Health Promot Int 1991;6:217–28 [Google Scholar]
- 15.Salmela R. Health policies and health for all strategies in the Nordic countries. Health Policy 1991;18:207–18 [DOI] [PubMed] [Google Scholar]
- 16.McCally M, Haines A, Fein O, et al. Poverty and ill health: physicians can, and should, make a difference. Ann Intern Med 1998;129:726–33 [DOI] [PubMed] [Google Scholar]
- 17.Flores P, Falcoff H. Social inequalities in health: what could be done in general practice? Rev Prat 2004;54:2263–70 [PubMed] [Google Scholar]
- 18.Fritzsche K, Armbruster U, Hartmann A, et al. Psychosocial primary care—what patients expect from their General Practitioners A cross-sectional trial. BMC Psychiatry 2002;2:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bodenmann P, Jackson Y, Bischoff T, et al. Precarite et determinants sociaux de la sante: quel(s) role(s) pour le medecin de premier recours? Rev Med Suisse 2009;5:845–9 [PubMed] [Google Scholar]
- 20.Lee P, Townsend P. Trends in Deprivation in the London Labour Market: A Study of Low Incomes and Unemployment in London. Geneva: International Labour Organization, 1993 [Google Scholar]
- 21.Marmot M. Social determinants of health inequalities. Lancet 2005;365:1099–104 [DOI] [PubMed] [Google Scholar]
- 22.Dillman DA. Mail and Telephone Surveys. New York: John Wiley and Sons, 2000 [Google Scholar]
- 23.Anyaegbu G. Using the OECD equivalence scale in taxes and benefits analysis. Econ Labour Market Rev 2010;4:49–54 [Google Scholar]
- 24.Shoukri MM, Asyali MH, Donner A. Sample size requirements for the design of reliability study: review and new results. Stat Methods Med Res 2004;13:251–71 [Google Scholar]
- 25.Salmond C, Crampton P, King P, et al. NZiDep: a New Zealand index of socioeconomic deprivation for individuals. Soc Sci Med 2006;62:1474–85 [DOI] [PubMed] [Google Scholar]
- 26.Eroglu S. Developing an index of deprivation which integrates objective and subjective dimensions: extending the work of Townsend, Mack and Lansley, and Halleröd. Soc Indicators Res 2007;80:493–510 [Google Scholar]
- 27.Sass C, Gueguen R, Moulin JJ, et al. Comparaison du score individuel de précarite des Centres d'examens de santé, EPICES, à la définition socio- administrative de la précarité. [Comparaison of the individual deprivation index of the French Health Examination Centres and the administrative definition of deprivation]. Santé Publique 2006;18:513–22 [DOI] [PubMed] [Google Scholar]
- 28.Willems SJ, Swinnen W, De Maeseneer JM. The GP's perception of poverty: a qualitative study. Fam Pract 2005;22:177–83 [DOI] [PubMed] [Google Scholar]
- 29.Bortolotti B, Menchetti M, Bellini F, et al. Psychological interventions for major depression in primary care: a meta-analytic review of randomized controlled trials. Gen Hosp Psychiatry 2008;30:293–302 [DOI] [PubMed] [Google Scholar]
- 30.Sass C, Moulin JJ, Guéguen R, et al. Le score Epices: un score individuel de précarité. Construction du score et mesure des relations avec des données de santé, dans une population de 197 389 personnes. Bull Épidemiol Heb 2006;14:93–6 [Google Scholar]
- 31.Townsend P. Poverty in the United Kingdom. Harmondsworth: Allen Lane and Penguin Books, 1979 [Google Scholar]
- 32.Abbott S, Freeth D. Social capital and health: starting to make sense of the role of generalized trust and reciprocity. J Health Psychol 2008;13:874–83 [DOI] [PubMed] [Google Scholar]
- 33.Gellis Z, Kenaley B. Problem-solving therapy for depression in adults: a systematic review. Res Soc Work Pract 2008;18:117 [Google Scholar]
- 34.Mynors-Wallis LM, Gath DH, Day A, et al. Randomised controlled trial of problem solving treatment, antidepressant medication, and combined treatment for major depression in primary care. BMJ 2000;320:26–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jackson L, Langille L, Lyons R, et al. Does moving from a high-poverty to lower-poverty neighborhood improve mental health? A realist review of ‘Moving to Opportunity’. Health Place 2009;15:961–70 [DOI] [PubMed] [Google Scholar]
- 36.Alexander GC, Casalino LP, Meltzer DO. Patient-physician communication about out-of-pocket costs. JAMA 2003;290:953–8 [DOI] [PubMed] [Google Scholar]
- 37.Franks P, Fiscella K. Reducing disparities downstream: prospects and challenges. J Gen Intern Med 2008;23:672–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bloch G, Rozmovits L, Giambrone B. Barriers to primary care responsiveness to poverty as a risk factor for health. BMC Fam Pract 2011;12:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alexander GC, Casalino LP, Tseng CW, et al. Barriers to patient-physician communication about out-of-pocket costs. J Gen Intern Med 2004;19:856–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hardee JT, Platt FW, Kasper IK. Discussing health care costs with patients: an opportunity for empathic communication. J Gen Intern Med 2005;20:666–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ben-Shlomo Y, White I, McKeigue PM. Prediction of general practice workload from census based social deprivation scores. J Epidemiol Community Health 1992;46:532–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Balarajan R, Yuen P, Machin D. Deprivation and general practitioner workload. BMJ 1992;304:529–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.