Abstract
Objectives
To present the results of a study of a worksite-based intervention to promote tobacco use cessation and improve weight management among motor freight workers.
Methods
This study used a pre-test/post-test, non-randomized design to assess the effectiveness of a four-month intervention that addressed the social context of the work setting. We evaluated 7-day tobacco quit prevalence among baseline tobacco users, and successful weight management, defined as no weight gain in workers with BMI < 25 at baseline and any weight loss among overweight and obese workers.
Results
At baseline, 40% were current tobacco users, and 88% had a BMI of 25 or greater. Of 542 workers invited to participate, 227 agreed to participate and received at least the first telephone call (42%). Ten months post-baseline, baseline tobacco users who participated in the intervention were more likely to have quit using tobacco than non-participants: 23.8% vs. 9.1% (p=0.02). There was no significant improvement in weight management.
Conclusions
Incorporating work experiences and job conditions into messages of health behavior change resulted in significant tobacco use cessation among participating motor freight workers.
Introduction
The work environment has potentially profound effects on workers’ health behaviors and related risks of disease. Prior research has demonstrated, for example, job stress, long hours at work, social norms supporting tobacco use, and shift work contribute to increased smoking and pose barriers to quitting. [1-5] Similarly, increasing evidence points to the role of work culture and work organization in obesity. [6, 7]
The work experiences of motor freight workers pose particularly significant challenges to their health behaviors. Their tobacco use rates are among the highest across occupational groups, between 34% and 46%, [8, 9] and overweight and obesity rates are also higher than for many other occupations. [8, 10] Work experiences, such as long work hours; irregular shifts; unsatisfactory sleeping accommodations; and demands of meeting deadlines [11-13] may contribute to poor diets, physical inactivity, and tobacco use. Because of the mobile nature of this work, worksite health promotion programs are generally inaccessible for these workers, who have among the lowest program participation rates of any industry group. [14]
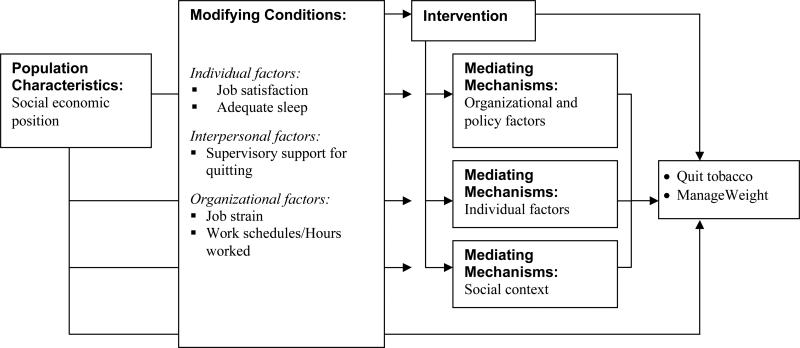
In response to these risks, we tested an intervention to promote tobacco use cessation and weight management among motor freight workers. The intervention was based on the social contextual model of health behavior change, which provides a framework for designing interventions in response to the work environment. [15-17] As illustrated in Figure 1, interventions may directly address the social context, thereby mediating the intervention effect, or may be informed by an understanding of factors in the worksite not amenable to change through the intervention. Accordingly, this model posits that the effectiveness of an intervention can be enhanced by attending to the social context, both by intervening to change modifiable aspects of the social context and by designing interventions to be responsive to those aspects of the social context that are not amenable to change. For example, although it may not be feasible to change work schedules, it may be possible to speak to workers’ concerns about work hours as part of intervention messages.
Figure 1.
Social contextual model of health behavior change
The purposes of this paper are to examine factors associated with participation in the intervention, and to estimate the effectiveness of the intervention in promoting tobacco use cessation and weight management among motor freight workers by comparing the outcomes among participants and non-participants in the intervention. An additional aim is to examine the prevalence of tobacco use and overweight/obesity in this population.
METHODS
DESIGN
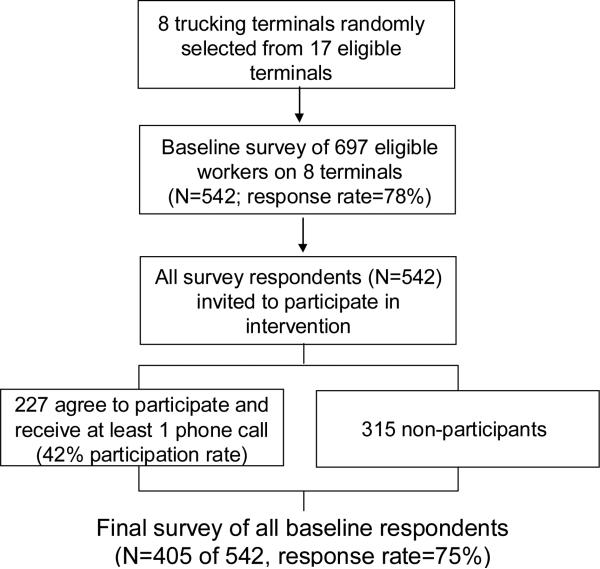
The Gear Up for Health Study tested a tobacco use cessation and weight management intervention among unionized truck drivers and dock workers, using a pre-test/post-test design (Figure 2). At baseline, we surveyed workers in eight trucking terminals to assess the prevalence of tobacco use and overweight. All respondents to the self-administered survey were invited to participate in the intervention. The baseline survey was conducted on-site in each terminal between November 2005 and August 2006, and the final survey was conducted 10 months later, or approximately 6 months after the completion of the 4-month intervention, between September 2006 and June 2007. Data collection and intervention staffs functioned independently, and data collection staff was blinded to workers’ participation status. We assessed change in tobacco use and weight between the baseline and final surveys in the entire study cohort, regardless of participation in the intervention, and compared change among program participants and non-participants. All study procedures were approved by the Cancer Center's Institutional Review Board. We followed the TREND Statement standards for reporting the results of non-randomized evaluations of behavioral and public health interventions. [18]
Figure 2.
Gear Up for Health Study Schema
SAMPLE
The eight participating trucking terminals were randomly selected from 17 eligible terminals in four states in the Eastern region of the US. Eligible terminals were affiliated with the Motor Freight Carriers Association, the industry trade association, and employed 75 to 150 workers who were members of the International Brotherhood of Teamsters (IBT). Eligible workers were employed for at least 15 hours/week, were permanent employees and IBT members, and had not been out of work on workers’ compensation for more than two weeks at the time of the survey. Across the eight terminals, 697 workers met the eligibility criteria, and were invited to participate in the survey; of those, 542 responded to the survey (response rate=78%). (See Figure 2.) Workers who completed the baseline survey were eligible to participate in the intervention regardless of their overweight or tobacco use status because the intervention focused on weight management, defined as either weight loss among those who were overweight or obese or weight gain prevention among those who were not overweight. Of the 542 survey respondents, 227 (42%) agreed to participate in the intervention and received at least one telephone call.
INTERVENTION
The intervention was a telephone-delivered health promotion program focusing on tobacco use cessation and weight management. We used the social contextual model (Figure 1) to guide our intervention development. We adapted a previously-tested intervention, designed for construction laborers and shown to be efficacious in a randomized controlled trial in promoting smoking cessation and fruit and vegetable consumption. [19] To identify elements of the social context of workers’ lives on and off the job that would influence their tobacco use and weight management practices, we conducted three focus groups with workers (n=18 total participants), one focus group with spouses (n=3 total participants), and three ‘ride-along’ participant observations, in which a staff member rode with drivers to observe health behaviors and working conditions. We identified positive work experiences (e.g. autonomy, pay, and benefits) as well as challenges and concerns within the work environment (e.g. hazardous working conditions, stresses in meeting deadlines, limited food and physical activity options). We reflected an understanding of these factors in both recruitment strategies and intervention messages and materials. The health counselors were trained to incorporate information on work experiences into their counseling calls.
The four-month intervention included telephone counseling sessions, a tailored feedback report and targeted written educational materials. The tailored feedback report introduced the program and offered brief personalized health messages, based on baseline survey responses, that were tailored on individual health behaviors (tobacco use; dietary patterns including consumption of fruits and vegetables, sugary sweetened beverages, sugary snacks, and fast food), intention to change, self-efficacy, risk perceptions, social support, and nicotine addition. Over the course of intervention delivery, we also mailed 11 written materials to all intervention participants, targeted to this population of workers utilizing themes that emerged from the focus groups.
Participants received up to five telephone counseling calls, which focused particularly on addressing factors in the work environment as part of the behavior change process. The telephone counselors were trained in the use of motivational interviewing techniques, [20, 21] and accordingly focused the discussion on participants’ choices, discrepancies between goals and behavior, personal responsibility for change, and enhancement of self-efficacy. This process was further guided by principles from the Transtheoretical Stages of Change model [22] and Social Cognitive Theory. [23] Counselors worked with participants to set goals for those interested in making changes, or simply monitored participants’ attitudes among those who were not ready to make changes. For example, the goals might have included weight maintenance for participants who were not overweight, weight loss for those overweight or obese, and/or smoking cessation for smokers. Counselors also discussed ways that health behavior changes might fit into their jobs and home lives. We also made available nicotine replacement therapy to participants interested in quitting tobacco. The project director provided on-going training, supervision and quality assurance for the health counselors through weekly staff meetings and review of process tracking reports from the computerized process tracking system. [24]
MEASURES
Primary outcomes
Tobacco use was measured by self-report, using standard measures. [25, 26] We measured current tobacco use by a positive response to either of the questions, “Have you used any tobacco products in the last 7 days” or “Have you used any cigarettes in the last 7 days”. Baseline tobacco users who responded positively to either of the tobacco use questions at follow-up were coded as continuing users, while those who said “no” to both questions were coded as quitters.
Anthropometric and self-reported measures of height and weight were obtained using standard methodology. Measured height and weight were used if available at both baseline and follow-up. Approximately 10% of the sample did not have measured height and weight values, although they did report height and weight on the survey. If measured values were not available for both time points, we used self-reported values. We computed body mass index (BMI) as: wt(kg)/(ht(m))2. Our primary outcome measure for weight was successful weight management, defined as no weight gain for people with BMI < 25 at baseline and any weight loss for all others. A secondary outcome was change in weight between baseline and follow-up for those with baseline BMI ≥ 25.
Program participation was measured by process tracking logs, and was defined as the participant completing one or more counseling calls. Non-participants declined to participate in the telephone intervention, although some received written materials.
Secondary outcomes
Fruit and vegetable consumption was assessed in a brief screener that measured consumption in seven categories. [27, 28] Participants also indicated how often they consumed sugar-sweetened beverages (1 question); and sugary snacks (1 question).
Covariates: Social Context of Work
Individual level factors
We assessed job satisfaction (“How satisfied are you with your job?”) and the extent to which these workers got adequate sleep ( “How often during the past 4 weeks did you get enough sleep to feel rested upon waking up?”).
Interpersonal level factors
We measured supervisory support by creating a sum of responses to five related items, creating a score ranging from 5 to 20 with a higher score indicating more supervisor support. (Cronbach's Alpha = 0.86.). [29]
Organizational factors
Job strain was assessed using the abbreviated version of the Job Content Questionnaire (JCQ),[29] focusing on the three sub-scales: psychological job demand (5 items); decision authority (3 items); and skill discretion (5 items). Decision latitude was created as a weighted sum of decision authority and skill discretion. A worker was defined to have job strain if his/her psychological demand was greater than the national median while decision latitude was below the national median. National medians [30, 31] were re-scaled to adjust for the different number of items used in our study.
We asked participants to report their work shift (day shift, versus afternoon, night, split, irregular or rotating), and hours worked in the last seven days. [32]
Sociodemographic characteristics
Sociodemographic variables were measured using standard items, including age, race/ethnicity and education. Main job categories included over-the-road truck driving, pick up and delivery truck driving, working on the docks and a combination of driving and dock work. Over-the-road truck drivers drive heavy trucks for extended periods of time and cover long distances; pick up and delivery truck drivers deliver freight within a local area; dockworkers load and unload freight from trucks.
STATISTICAL ANALYSIS
We proposed a sample of 560 workers in 8 terminals at baseline expecting 448 (80%) would complete the final survey. We assumed that 70% of those sampled would agree to participate in the intervention and the intra-class correlation of the participation rates would be 0.01. Based on these assumptions, this sample size provided 80% power to detect meaningful associations between worker characteristics and participation at the 5% significance level.
To evaluate factors associated with program participation, we compared worker characteristics and outcomes among participants and non-participants. To assess whether program participation was associated with outcome measures, we compared each outcome among participants and non-participants, controlling for terminal and any factors found to be statistically significantly associated with participation.
In all analyses we controlled for the clustering of workers in terminals, using mixed effect linear modeling methods with terminal as a random effect. For continuous measures we used mixed effect analysis of variance and for categorical measures we used iteratively re-weighted likelihoods to fit a binary distribution with a logit link function. We used SAS statistical software for all analyses. [33]
RESULTS
Program Participation
As illustrated in Figure 2, 42% of workers invited to participate agreed and received at least the first telephone call. We examined the associations of program participation with sociodemographics, individual factors and outcomes (Table 1). The factors most strongly associated with participation were working the day shift and getting adequate sleep. Participants were somewhat more likely to be white than non-participants.
Table 1.
Association of program participation and worker characteristics at baseline (n=541).
| Program Participation | P-value* | ||
|---|---|---|---|
| Worker characteristic | Participants (Counseling and materials) (n=227, 42%) | Non-Participants (Materials/survey only or survey only) n=314, 58%) | |
| Sociodemographics | |||
| Job category n (%) | 0.15 | ||
| Dock worker | 25 (11) | 53 (17) | |
| P&D driver | 161 (72) | 193 (62) | |
| OTR driver | 38 (17) | 67 (21) | |
| Mean Age (SD) | 48.5 (7.9) | 48.6 (8.8) | 0.65 |
| College or higher n (%) | 66 (29) | 86 (27) | 0.89 |
| White n (%) | 194 (86) | 253 (81) | 0.05 |
| Money Situation-comfortable, some extras n (%) | 118 (52) | 167 (54) | 0.61 |
| Social context of work | |||
| Individual factors | |||
| Job satisfaction-very, generally satisfied n (%) | 199 (89) | 274 (88) | 0.34 |
| Adequate sleep-often, very often n (%) | 100 (44) | 177 (57) | 0.01 |
| Interpersonal factors | |||
| Mean Supervisor support (SD) | 14.1 (3.3) | 14.3 (3.1) | 0.28 |
| Organizational factors | |||
| Job strain-yes n (%) | 74 (35) | 88 (30) | 0.40 |
| Mean Hours worked last 7 days (SD) | 46.9 (14.4) | 45.2 (15.2) | 0.20 |
| Works day shift n (%) | 128 (58) | 132 (42) | 0.006 |
| Outcome measures | |||
| Food choices | |||
| Mean Fruits and vegetables/ day (SD) | 2.8 (2.5) | 2.7 (2.2) | 0.85 |
| Mean Sugary Drinks/day (SD) | 1.1 (1.3) | 1.2 (1.3) | 0.52 |
| Mean Sugary Snacks/day (SD) | 0.6 (0.9) | 0.6 (0.7) | 0.30 |
| Tobacco measures | |||
| Tobacco user n (%) | 92 (41) | 124 (40) | 0.63 |
| Weight measures | |||
| Mean Weight, lbs (SD) | 213.7 (39.4) | 210.5 (36.8) | 0.30 |
| Mean BMI (SD) | 30.4 (4.9) | 29.8 (4.7) | 0.14 |
| BMI ≥ 25 n (%) | 205 (90) | 270 (87) | 0.14 |
| BMI ≥ 30 n (%) | 98 (43) | 126 (41) | 0.44 |
Adjusted for terminal
There were no statistically significant differences between participants and non-participants in the baseline levels of the outcome variables. At baseline, 41% of participants and 40% of non-participants used tobacco. For indicators of overweight and obesity, 90% of participants and 87% of non-participants had a BMI of 25 or greater (as the cut-point for overweight); 43% of participants and 41% of non-participants had a BMI of 30 or greater.
Tobacco use cessation
Among the 216 baseline tobacco users, 151 completed the final survey (70%). Among these respondents, 23 reported not using tobacco in the last 7 days resulting in a 7 day quit prevalence of 15% (95% CI 9.5% to 21.0%). Baseline tobacco users who participated in the intervention were more likely to have quit using tobacco than non-participants: 23.8% vs. 9.1% (site adjusted OR =3.13, 95% CI 1.22 to 7.98, p=0.02). When we controlled for terminal and factors associated with program participation - race/ethnicity, sleep adequacy, and job shift - the relationship between tobacco use cessation and program participation remained statistically significant, (OR = 3.07, 95% CI 1.16 to 8.09, p= 0.02); the adjusted quit rate was 23.9% for participants compared to 9.1% for non-participants. (See Table 2)
Table 2.
Association of tobacco use cessation with program participation controlling for race, sleep adequacy, job shift, and terminal among baseline tobacco users (n=147). Mixed model logistic regression analysis
| Slope (SE) | OR (95% CI) | |
|---|---|---|
| Race/ ethnicity: White vs. other | 0.20 (0.70) | 1.22 (0.31,4.87) |
| Sleep Adequacy: + 1 unit | 0.35 (0.48) | 1.43 (0.56,3.65) |
| Job Shift; Day vs. all other | -0.54 (0.48) | 0.59 (0.23,1.52) |
| Program participation vs. no participation | 1.12 (0.49) | 3.07 (1.16,8.09) |
Weight management
Among the 405 participants who completed both the baseline and final survey, 398 had measured or self-reported height and weight and of these 182 (46%) met the definition of successful weight management at final. The rate of successful weight management, adjusted for terminal was 45% (95% CI 38% to 53%). There was no difference between participants and non-participants in successful weight management. The adjusted successful management rates were 44% for participants and 46% for non-participants, p=0.74 (OR =0.93, 95% CI 0.62 to 1.40).
Eighty-five percent of the participants with baseline and final height and weight data (n=342 of 398) were overweight or obese (BMI ≥ 25) at baseline. Within this subsample, those who participated in the intervention had a mean weight loss of 0.06 lbs compared to a mean weight gain of 0.49 lbs among non-participants (p=0.62, controlling for terminal). After controlling for covariates (baseline weight, race/ethnicity, sleep adequacy, job shift and terminal), the association between weight change and program participation remained not statistically significant (p=0.49).
Because of the potential for weight gain among workers who were attempting to quit using tobacco, we added tobacco use status and the interaction of tobacco use status and participation to the multivariable model for weight management. Although the interaction of program participation and tobacco use was not significantly associated with weight change, we found that program participants who quit using tobacco gained an average of 6.3 pounds compared to workers in the other groups whose weight changed very little (Table 3).
Table 3.
Adjusted mean (standard error) weight change by tobacco use and program participation, adjusted for baseline weight, race/ethnicity, sleep adequacy job shift and terminal among participants with BMI ≥ 25 (n=333): Mixed model analysis of covariance.
| Program participants (n=158) | Program non-participants (n=184) | |
|---|---|---|
| Non-user | -0.70 (0.99) | 0.19 (0.96) |
| Quitter | 6.33 (2.32) | 1.37 (3.52) |
| Continuing user | -0.19 (1.38) | 0.93 (1.13) |
Diet
Overall, there was a significant decrease in the consumption of sugary drinks (mean decrease of 0.20 servings per day, p=0.003). There was also a non-significant decrease of 0.08 servings per day in sugary snack consumption, and a non-significant increase of 0.12 servings per day in fruits and vegetable consumption. Dietary changes were not associated with program participation, adjusting for site, baseline food choice, race, sleep adequacy, job shift and tobacco use status.
DISCUSSION
Gear Up for Health is a tailored, print- and telephone-delivered intervention for truck drivers and other motor freight workers. Using the social contextual model for health behavior change, we embedded messages about tobacco use cessation and weight management in the context of workers’ day-to-day work experiences, such as the challenges of finding healthful food options on the road and boredom during long drives that may prompt increased use of tobacco. Although it was not feasible to change these work conditions, the personalized intervention aimed to help workers identify strategies to address work experiences as part of the behavior change process.
This intervention resulted in successful tobacco use cessation rates; 24% of baseline tobacco users participating in the intervention were no longer tobacco users six months after the conclusion of the intervention, compared to only 9% of non-participants. We recognize that non-participants in this study are not comparable with participants given the non-randomized design. Nevertheless, the cessation rate among participants in the current study compares favorably with our findings in the Tools for Health study, which tested a similar intervention in a randomized controlled trial among construction workers; we observed a quit rate of 19% among these intervention participants and 8% among those workers randomly assigned to a non-intervention control group. [19] A recent Cochrane review of workplace interventions using individual counseling for smoking cessation [34] reported sustained cessation rates at six to 36 months post-intervention ranging from 8% to 21% among intervention participants. [19, 35-42]
We found no overall improvements in weight management or weight loss among overweight and obese workers, regardless of participation in the intervention. Baseline tobacco users who participated in the intervention program and quit using tobacco gained on average over 6 pounds (2.7kg). Although weight gain associated with tobacco use cessation is highly variable and may be related to other factors, such as number of cigarettes smoked, age, and race/ethnicity, our estimate of post-cessation weight gain is in line with other literature (e.g., weight gain of 2.8kg and 4.4kg among males). [43, 44] A growing literature describes the feasibility and potential efficacy of intervening with multiple risk behaviors. [45-48] These results suggest, however, that the combination of tobacco use cessation and weight management may pose particular challenges.
This study used a non-randomized, pre-test/post-test design. There is increasing recognition in the public health literature that the accumulation of evidence about effective interventions requires expanded use of research designs beyond the randomized controlled trial. [49-53] Kirkwood [50] outlines several appropriate circumstances for the use of a non-randomized design, which are applicable to this study. This intervention had been shown to be efficacious in a prior randomized controlled trial among construction laborers; in this study, we adapted this evidence-based intervention to another population (motor freight workers), and expanded its application to another risk factor (overweight/obesity). Following the guidelines outlined in the TREND statement for reporting the results of studies using non-randomized designs, [18] we have described the use of social and behavioral theory in the intervention design, provided information about the intervention, and described the research design.
It is important to note several additional limitations to this study. Tobacco use cessation was measured by self-report; collection of biochemical measures to validate self-report was not feasible in this setting, where testing for other drugs is not uncommon and would therefore likely raise concerns and reduce trust among participants. A work group synthesis of this issue concluded that biochemical verification may not be necessary for population studies with certain characteristics, such as those of workers using previously tested intervention strategies. [54] In order to minimize missing measured data on weight, we used mixed methods for collection of weight and height, although we consistently used the same type of measure for each individual participant. We measured tobacco use cessation and weight loss only once post-intervention, six months after the completion of the intervention, and may not have captured some initial changes in these outcomes as indicated on the self-reported surveys. Also, we defined participation in the intervention as receiving at least one telephone counseling call; we recognize that variations in intervention dose may be associated with changes in the outcome.
Despite these limitations, this study has important implications for the design and delivery of health promotion interventions for these high-risk workers. This study points to the considerable need for effective interventions in this population, which is at high risk for tobacco use and overweight/obesity. Overall, 40% were current tobacco users, and 42% overall had a BMI of 30 or greater, considered obese. By comparison, approximately 21% of adult Americans are current tobacco users and about one third of US adults are obese. [55, 56] Despite this elevated risk, few interventions have been designed for middle-aged, working men.
In conclusion, the Gear Up for Health intervention illustrates the importance of embedding messages about tobacco control in the larger context of work experiences. We applied the social contextual model to frame our intervention around an understanding of the unique work experiences and job conditions of motor freight workers, as we learned through our formative research. This study found significant rates of tobacco use cessation that compare favorably with other studies. These findings also underscore the need for ongoing research on weight management within the work setting. As the field of public health seeks to reduce disparities in health outcomes such as tobacco use cessation and weight loss, it is important that we recognize that one size does not fit all, and that work experiences and job conditions are important components in our efforts to tailor and target interventions to the needs of blue-collar workers.
ACKNOWLEDGMENTS
This work would not have been possible without the contributions of the members and leaders of the International Brotherhood of Teamsters and the Motor Freight Carriers Association. The authors thank Elizabeth Barbeau, Elizabeth Barna, Linnea Benson, Lamont Byrd, Joshua Gagne, Kerry Kokkinogenis, Timothy Lynch, Ruth Lederman, and Michael Massagli for their contributions to this study and the development of this manuscript.
This work was conducted with the support of a grant from the Centers for Disease Control and Prevention (grant number 5 R01 DP000099-03 to G.S.) and grants from the National Institutes of Health (grant numbers 5 K05 CA108663 and 2 R25 CA057713 to G.S.).
References
- 1.Sorensen G, Quintiliani LM, Pereira L, Yang M, Stoddard AM. Work Experiences and Tobacco Use: Findings from the Gear Up for Health Study. J Occup Environ Med. 2009;51(1):87–94. doi: 10.1097/JOM.0b013e31818f69f8. [DOI] [PubMed] [Google Scholar]
- 2.Janzon E, Engstrom G, Lindstrom M, Berglund G, Hedblad B, Janzon L. Who are the “quitters”? a cross-sectional study of circumstances associated with women giving up smoking. Scand J Public Health. 2005;33(3):175–182. doi: 10.1080/14034940410019244. [DOI] [PubMed] [Google Scholar]
- 3.Sanderson DM, Ekholm O, Hundrup YA, Rasmussen NK. Influence of lifestyle, health, and work environment on smoking cessation among Danish nurses followed over 6 years. Prev Med. 2005;41(3-4):757–760. doi: 10.1016/j.ypmed.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Eriksen W. Work factors and smoking cessation in nurses’ aides: a prospective cohort study. BMC Public Health. 2005;5:142. doi: 10.1186/1471-2458-5-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Albertsen K, Borg V, Oldenburg B. A systematic review of the impact of work environment on smoking cessation, relapse and amount smoked. Prev Med. 2006;43(4):291–305. doi: 10.1016/j.ypmed.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 6.Schulte PA, Wagner GR, Downes A, Miller DB. A framework for the concurrent consideration of occupational hazards and obesity. Ann Occup Hyg. 2008;52(7):555–566. doi: 10.1093/annhyg/men055. [DOI] [PubMed] [Google Scholar]
- 7.Schulte PA, Wagner GR, Ostry A, et al. Work, obesity, and occupational safety and health. Am J Public Health. 2007;97(3):428–436. doi: 10.2105/AJPH.2006.086900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Korelitz JJ, Fernandez AA, Uyeda VJ, Spivey GH, Browdy BL, Schmidt RT. Health habits and risk factors among truck drivers visiting a health booth during a trucker trade show. Am J Health Promot. 1993;8(2):117–123. doi: 10.4278/0890-1171-8.2.117. [DOI] [PubMed] [Google Scholar]
- 9.Division of Health Interview Statistics . 1997 National Health Interview Survey (NHIS) Public Use Data Release. National Center for Health Statistics; Hyattsville MD: 2000. [Google Scholar]
- 10.Whitfield Jacobson PJ, Prawitz AD, Lukaszuk JM. Long-haul truck drivers want healthful meal options at truck-stop restaurants. J Am Diet Assoc. 2007;107(12):2125–2129. doi: 10.1016/j.jada.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 11.LaDou J. In: The health of truck drivers. In Occupational medicine: Principles and practical applications. second edition Zenz C, Chicago IL, editors. Year Book Medical Publishers; 1988. pp. 958–970. [Google Scholar]
- 12.Ouellet LJ. Pedal to the metal: The work lives of truckers. Temple University Press; Philadelphia, PA: 1994. [Google Scholar]
- 13.Agar MH. Independents declared: The dilemmas of independent trucking. Smithsonian Institution Press; Washington, D.C.: 1986. [Google Scholar]
- 14.Grosch J, Alterman T, Petersen M, Murphy L. Worksite health promotion programs in the U.S.: Factors associated with availability and participation. Am J Health Promot. 1998;13(1):36–45. doi: 10.4278/0890-1171-13.1.36. [DOI] [PubMed] [Google Scholar]
- 15.Sorensen G, Emmons K, Hunt MK, et al. Model for incorporating social context in health behavior interventions: Applications for cancer prevention for working-class, multiethnic populations. Prev Med. 2003;37:188–197. doi: 10.1016/s0091-7435(03)00111-7. [DOI] [PubMed] [Google Scholar]
- 16.Sorensen G, Stoddard A, Dubowitz T, Barbeau EM, Berkman LF, Peterson KE. The influence of social context on changes in fruit and vegetable consumption: Results of the Healthy Directions Studies. Am J Public Health. 2007;97:1216–1227. doi: 10.2105/AJPH.2006.088120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorensen G, Barbeau E, Hunt MK, Emmons K. Reducing social disparities in tobacco use: A social contextual model for reducing tobacco use among blue-collar workers. Am J Public Health. 2004;94(2):230–239. doi: 10.2105/ajph.94.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Des Jarlais DC, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sorensen G, Barbeau E, Stoddard AM, et al. Tools for Health: The efficacy of a tailored intervention targeted for construction laborers. Cancer Causes and Control. 2007;18:51–59. doi: 10.1007/s10552-006-0076-9. [DOI] [PubMed] [Google Scholar]
- 20.Miller W, Rollnick S. Motivational interviewing: Preparing people to change addictive behaviors. Guildford Press; New York, NY: 1991. [Google Scholar]
- 21.VanWormer JJ, Boucher JL. Motivational interviewing and diet modification: A review of the evidence. Diabetes Educ. 2004;30(3):404–419. doi: 10.1177/014572170403000309. [DOI] [PubMed] [Google Scholar]
- 22.Prochaska JO, DiClemente CC. Self-change processes, self-efficacy and decisional balance across five stages of smoking cessation. Alan R. Liss, Inc.; New York, NY: 1983. [PubMed] [Google Scholar]
- 23.Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 24.Hunt MK, Harley A, Stoddard A, Lederman R, MacArthur MJ, Sorensen G. External validity and feasibility of a cancer prevention intervention for construction laborers. Am J Health Promot. doi: 10.4278/ajhp.080721-QUAN-130. in press. [DOI] [PubMed] [Google Scholar]
- 25.Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: Issues and recommendations. Nicotine Tob Res. 2003;5(1):13–25. [PubMed] [Google Scholar]
- 26.U.S. Department of Health and Human Services . Reducing the health consequences of smoking: 25 years of progress, A report of the Surgeon General. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Rockville, MD: 1989. [Google Scholar]
- 27.Havas S, Heimdinger J, Damron D, et al. 5-A-Day for Better Health: Nine community research projects to increase fruit and vegetable consumption. Public Health Rep. 1995;110(1):68–80. [PMC free article] [PubMed] [Google Scholar]
- 28.Thompson FE, Kipnis V, Subar AF, et al. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am JClin Nutr. 2000;71(6):1503–1510. doi: 10.1093/ajcn/71.6.1503. [DOI] [PubMed] [Google Scholar]
- 29.Karasek R, Theorell T. Healthy work: Stress, productivity, and the reconstruction of working life. Basic Books; New York, NY: 1990. [Google Scholar]
- 30.Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3:322–355. doi: 10.1037//1076-8998.3.4.322. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz JE, Pieper CF, Karasek RA. A procedure for linking psychosocial job characteristics data to health surveys. Am J Public Health. 1988;78:904–909. doi: 10.2105/ajph.78.8.904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Quality of worklife questionnaire. [ http://www.cdc.gov/niosh/pdfs/QWLsurvey.pdf]
- 33.SAS Institute Inc. SAS for Windows, Release 8.01. SAS Institute Inc.; Cary, N.C.: 1999-2000. [Google Scholar]
- 34.Cahill K, Moher M, Lancaster T. Workplace interventions for smoking cessation. Cochrane Database Syst Rev. 2008;(4):CD003440. doi: 10.1002/14651858.CD003440.pub3. [DOI] [PubMed] [Google Scholar]
- 35.Kornitzer M, Dramaix M, Kittel F, De Backer G. The Belgian heart disease prevention project: changes in smoking habits after two years of intervention. Prev Med. 1980;9(4):496–503. doi: 10.1016/0091-7435(80)90044-4. [DOI] [PubMed] [Google Scholar]
- 36.Cambien F, Richard JL, Ducimetiere P, Warnet JM, Kahn J. The Paris Cardiovascular Risk Factor Prevention Trial. Effects of two years of intervention in a population of young men. J Epidemiol Community Health. 1981;35(2):91–97. doi: 10.1136/jech.35.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li VC, Kim YJ, Ewart CK, et al. Effects of physician counseling on the smoking behavior of asbestos-exposed workers. Prev Med. 1984;13(5):462–476. doi: 10.1016/0091-7435(84)90015-x. [DOI] [PubMed] [Google Scholar]
- 38.Gomel M, Oldenburg B, Simpson JM, Owen N. Work-site cardiovascular risk reduction: a randomized trial of health risk assessment, education, counseling, and incentives. Am J Public Health. 1993;83(9):1231–1238. doi: 10.2105/ajph.83.9.1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kadowaki T, Watanabe M, Okayama A, Hishida K, Ueshima H. Effectiveness of smoking-cessation intervention in all of the smokers at a worksite in Japan. Ind Health. 2000;38(4):396–403. doi: 10.2486/indhealth.38.396. [DOI] [PubMed] [Google Scholar]
- 40.Lang T, Nicaud V, Slama K, et al. Smoking cessation at the workplace. Results of a randomised controlled intervention study. Worksite physicians from the AIREL group. J Epidemiol Community Health. 2000;54(5):349–354. doi: 10.1136/jech.54.5.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Terazawa T, Mamiya T, Masui S, Nakamura M. [The effect of smoking cessation counseling at health checkup]. Sangyo Eiseigaku Zasshi. 2001;43(6):207–213. doi: 10.1539/sangyoeisei.kj00002552512. [DOI] [PubMed] [Google Scholar]
- 42.Tanaka H, Yamato H, Tanaka T, et al. Effectiveness of a low-intensity intra-worksite intervention on smoking cessation in Japanese employees: a three-year intervention trial. J Occup Health. 2006;48(3):175–182. doi: 10.1539/joh.48.175. [DOI] [PubMed] [Google Scholar]
- 43.Hofstetter A, Schutz Y, Jequier E, Wahren J. Increased 24-hour energy expenditure in cigarette smokers. N Engl J Med. 1986;314(2):79–82. doi: 10.1056/NEJM198601093140204. [DOI] [PubMed] [Google Scholar]
- 44.Flegal KM, Troiano RP, Pamuk ER, Kuczmarski RJ, Campbell SM. The influence of smoking cessation on the prevalence of overweight in the United States. N Engl J Med. 1995;333(18):1165–1170. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- 45.Sorensen G, Barbeau E, Stoddard A, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working-class, multi-ethnic workers: Results of the Healthy Directions Small Business Study. Am J Public Health. 2005;95(8):1389–1395. doi: 10.2105/AJPH.2004.038745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prochaska JJ, Hall SM, Humfleet G, et al. Physical activity as a strategy for maintaining tobacco abstinence: a randomized trial. Prev Med. 2008;47(2):215–220. doi: 10.1016/j.ypmed.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Emmons KM, Stoddard AM, Fletcher R, et al. Cancer prevention among working-class, multi-ethnic adults: Results of the Healthy Directions Health Centers Study. Am J Public Health. 2005;95(7):1200–1205. doi: 10.2105/AJPH.2004.038695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Emmons KM, McBride CM, Puleo E, et al. Project PREVENT: a randomized trial to reduce multiple behavioral risk factors for colon cancer. Cancer Epidemiol Biomarkers Prev. 2005;14(6):1453–1459. doi: 10.1158/1055-9965.EPI-04-0620. [DOI] [PubMed] [Google Scholar]
- 49.Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ. 1996;312(7040):1215–1218. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kirkwood B. Making public health interventions more evidence based. BMJ. 2004;328(7446):966–967. doi: 10.1136/bmj.328.7446.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sorensen G, Emmons K, Hunt MK, Johnston D. Implications of the results of community intervention trials. Annu Rev Public Health. 1998;19:379–416. doi: 10.1146/annurev.publhealth.19.1.379. [DOI] [PubMed] [Google Scholar]
- 52.Smith PG. Evaluating interventions against tropical diseases. Int J Epidemiol. 1987;16(2):159–166. doi: 10.1093/ije/16.2.159. [DOI] [PubMed] [Google Scholar]
- 53.Kirkwood BR, Cousens SN, Victora CG, de Zoysa I. Issues in the design and interpretation of studies to evaluate the impact of community-based interventions. Trop Med Int Health. 1997;2(11):1022–1029. doi: 10.1046/j.1365-3156.1997.d01-188.x. [DOI] [PubMed] [Google Scholar]
- 54.Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4(2):149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- 55.Ogden CL, Carroll MD, McDowell MA, Flegal KM. NCHS Data Brief No 1. National Center for Health Statistics; Hyattsville, MD: 2007. Obesity among adults in the United States - no change since 2003-2004. [PubMed] [Google Scholar]
- 56.Cigarette smoking among adults--United States, 2006. MMWR Morb Mortal Wkly Rep. 2007;56(44):1157–1161. [PubMed] [Google Scholar]