Abstract
Objective
To examine prospectively the natural course of bulimia nervosa (BN) and eating disorder not-otherwise-specified (EDNOS) and test for the effects of stressful life events (SLE) on relapse after remission from these eating disorders.
Method
117 female patients with BN (N = 35) or EDNOS (N = 82) were prospectively followed for 72 months using structured interviews performed at baseline, 6- and 12-months, and then yearly thereafter. ED were assessed with the structured clinical interview for DSM-IV, and monitored over time with the longitudinal interval follow-up evaluation. Personality disorders were assessed with the diagnostic interview for DSM-IV-personality-disorders, and monitored over time with the follow-along-version. The occurrence and specific timing of SLE were assessed with the life events assessment interview. Cox proportional-hazard-regression-analyses tested associations between time-varying levels of SLE and ED relapse, controlling for comorbid psychiatric disorders, ED duration, and time-varying personality-disorder status.
Results
ED relapse probability was 43%; BN and EDNOS did not differ in time to relapse. Negative SLE significantly predicted ED relapse; elevated work and social stressors were significant predictors. Psychiatric comorbidity, ED duration, and time-varying personality-disorder status were not significant predictors.
Discussion
Higher work and social stress represent significant warning signs for triggering relapse for women with remitted BN and EDNOS.
Keywords: bulimia nervosa, eating disorder not otherwise specified, stress, personality, relapse, work stress
Introduction
Although an increasing number of studies have investigated the course of eating disorders (ED),1 most are treatment-outcome studies. Notable exceptions include Herzog et al.s’2 long-term study of bulimia nervosa (BN) and anorexia nervosa (AN), Milos et al.s’3 follow-up study of a mixed clinical/community sample of AN, BN, and ED not-otherwise-specified (EDNOS)., and Agras et al.s’4 multi-site follow-up study of a mixed sample of AN, BN, and EDNOS. Herzog et al.,2 studying the natural course at 7.5 years of women with BN and AN, found AN had a lower recovery rate than BN. Milos et al.,3 in their naturalistic 30-month follow-up study in Zurich, found that EDs are characterized by a fluctuating temporal course with instances of remissions followed by relapses both within and between diagnoses.
While research has established that AN has a worse course than other ED in both naturalistic1 and treatment5 literatures, questions remain regarding the course of other diagnoses, particularly EDNOS. EDNOS is by far the most prevalent ED diagnosis in most outpatient settings,6,7 has demonstrated clinical significance but has received, except for the specific sub-example of binge eating disorder, little research attention.8 Agras et al.4 reported that over 4 years of prospective follow-along EDNOS remitted more quickly than AN and BN but that time to relapse among remitted cases did not differ significantly between EDNOS and either AN and BN. Ben-Tovim et al.9 reported that the 5-year course of BN and EDNOS were nearly identical, with remission rates of 74 and 78%, respectively. In our previous analysis of 5-year course,10 BN and EDNOS differed little with both categories showing similar patterns of remissions (74 and 83%, respectively) and relapses (47 and 42%, respectively). Thus, emerging data for BN and EDNOS suggest that their longer-term outcomes appear comparable.1
A related research need is to identify prognostic factors for BN and EDNOS outcomes. While some predictors have emerged for AN, such as older onset, longer duration, and lower weight,2,11 reliable predictors for the natural course or treatment outcomes of BN and EDNOS have not been identified.2,10 The literature contains hints that for BN, psychiatric comorbidity, personality disturbances, general psychosocial distress, and poor self-esteem may predict poorer outcomes.1,9,12,13 Other long-term studies, however, have failed to support hypothesized clinical predictors. In the case of EDNOS, Ben-Tovim et al.9 were unable to identify any predictors of 5-year outcomes, and for BN and EDNOS, Grilo et al.10 reported that personality disorders were unrelated to remissions or relapses.
The inconsistent literature on the impact of personality disturbances on ED outcomes10,13 may reflect several factors including, for example, different assessment instruments, varied personality classification models, and different recruitment methods.14 Personality disturbances may also exert their effects on the course of ED indirectly, perhaps by influencing other factors that increase the risk of poor outcomes (i.e., accelerated relapse) such as increased tendency to experience stressful life events. For example, Daley et al.15 found that certain personality disorders (Cluster A and B diagnoses) predicted interpersonal and episodic stressful life events, which—in turn—predicted a worse course of depressive symptoms even after controlling for initial depression severity. This seems a logical line of investigation to pursue further with EDs. Small early studies reported that stressful events were associated with BN relapse16 and that both personality disturbance and stressful events17 were associated with worse course at 1-year follow-up. Most recently, in a large and long-term longitudinal study, Keel et al.12 found that poor psychosocial function increased the risk of post-remission relapse in women with BN. Keel et al.12 speculated that poor psychosocial functioning might partly reflect personality disturbances that increase risk for stressful events and/or relapse but emphasized that longitudinal studies would need to assess these constructs directly (personality psychopathology and stressful events) after ED remission, to definitely test their roles on precipitating relapse.
The present study examined prospectively the 6-year natural course of BN and EDNOS with the aim of testing the effects of stressful life events (SLEs) on relapse after remission from these ED. The present study aimed to test prospectively the association between post-remission time-varying levels of SLEs and relapse while controlling for two severity markers (psychiatric comorbidity and ED duration),1 and time-varying status of two contrasting forms of PD psychopathology—BPD and obsessive-compulsive (OCPD). We focused on time-varying changes or fluctuations in these two forms of PD given1: this dimensional approach may have greater conceptual relevance and empirical validity18,19 while providing greater statistical power2; BPD and OCPD reflect contrasting behaviors (instability and impulsivity versus control and rigidity, respectively) associated with different patterns of ED,14 functioning19 and stressful life events20; and cluster-B PD and OCPD have been found to be associated prospectively with higher versus lower rates, respectively, of alcohol use relapse.21 We hypothesized that time-varying increases in negative life events would prospectively predict ED relapse and that, when considered jointly, time-varying increases in BPD criteria would increase ED relapse risk whereas increases in OCPD criteria would decrease ED relapse risk.
Method
Participants
Participants were enrolled in a NIMH-funded multi-site prospective naturalistic study (Collaborative Longitudinal Personality Disorders Study); the aims, methods, and characteristics of participants have been published.22,23 The overall study enrolled 668 participants aged 18–45 years with at least one PD or with major depressive disorder. Exclusion criteria included schizophrenia/schizoaffective disorders; active psychosis; organic disorders, post-ECT status, or substance intoxication or withdrawal; IQ below 85, or inability to read English. Of the participants, 64% were female, 76% were Caucasian, 11% African-American, 9% Hispanic-American, and 4% “other ethnicity.” Mean age was 32.8 (SD = 8.1) years. Participants were well-distributed across social classes except for small representation from the lowest socioeconomic class. Forty-five percent were out-patients and 11% were inpatients in various mental health settings, 5% were from medical settings, and 39% were self-referred (from advertisements) and were either in or seeking psychiatric treatment. This study received IRB approval at all participating sites. All participants signed written informed consent after procedures had been fully explained.
This study is based on 117 female participants (N = 35 with BN and N = 82 with EDNOS). Of the overall N = 688 enrolled in CLPS, N = 132 females met criteria for either BN or EDNOS—of which N = 117 were selected for this study because they achieved a remission from their ED and had at least 6 months of follow-up data. Our previous report10 was based on 92 of these patients who met criteria for current BN or EDNOS at baseline. Of those 92 patients, 77 (N = 18 with BN and N = 59 with EDNOS) remitted from their ED and are included in this study. In addition, we included 40 females with history but not current ED (N = 17 with BN and N = 23 with EDNOS) at baseline. We focused on females since the majority of ED cases are female and the limited number of males with ED diagnoses and follow-up data (N = 11) precluded analysis. Overall, the 117 female ED patients had a mean age of 31.2 (SD = 8.1) years, 95 (81%) were Caucasian, and 94 (80%) had at least some college education. Participants had a mean of 1.96 (SD = 1.4) additional lifetime Axis I psychiatric disorders, a mean of 1.84 (SD = 1.7) PDs (89% met criteria for at least one PD), and a mean duration of ED prior to remission of 12.6 (SD = 9.2) years. BN and EDNOS groups did not differ significantly on any of these variables. Of the 35 BN participants, 4 (11.4%) had a history of AN and 10 (28.6%) had a history of EDNOS. Of the 82 EDNOS participants, 7 (8.5%) had a history of AN and 15 (18.3%) had a history of BN.
Procedures
Participants were interviewed in person by experienced interviewers with masters or doctoral degrees in mental health disciplines. Research interviewers underwent extensive standardized training to achieve reliability in the administration of the major diagnostic measures for both Axis I psychiatric and Axis II personality disorders.24 The research interviewers were monitored and received ongoing supervision by investigators at each site, as well as supervision across sites to prevent drift.
To establish diagnoses at baseline entry into the study, interviewers administered the Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Version (SCID-I/P)25 to assess Axis I psychiatric disorders, and the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV)26 to assess all PD diagnoses and their criteria. In this longitudinal study, participants were re-interviewed at 6 and 12 months and then annually thereafter. The course of BN and EDNOS was assessed using the Longitudinal Interval Follow-up Evaluation (LIFE).27 The course of PD was assessed using a modified version of the DIPD-IV—the DIPD-FAV.28 The occurrence and specific timing of stressful life events was assessed using the Life Events Assessment (LEA;20) administered at baseline, 6 and 12 months, then annually thereafter. During each of the follow-up assessments, interviewers used a calendar for the exact follow-up interval and oriented participants to the interval by first using major time points, such as birthdays, holidays, vacations, and any other major events specific to each participant.
Assessment Instruments
Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Version (SCID-I/P)
The SCID-I/P25 is a widely-used diagnostic interview to assess current and lifetime Axis I psychiatric disorders. When assessing the ED diagnoses, assessors strictly adhered to the SCID-I/P and DSM-IV criteria and principles. The SCID-I/P specifically assesses BN; the diagnosis of EDNOS was assigned, following the DSM-IV principles, if ED features were present and resulted in clinically meaningful levels of impairment (despite failure to meet criteria for the “formal” diagnoses of BN or AN). In the current study, median kappa coefficients for inter-rater reliability for psychiatric disorders ranged from 0.57 to 1.0, and the median kappa coefficient was 0.77 for ED diagnoses.24
Longitudinal Interval Follow-Up Evaluation
The LIFE,27 a semi-structured interview rating system with demonstrated reliability and validity,29 assesses the longitudinal course of psychiatric disorders, including ED. The LIFE has served as the primary measure of major longitudinal studies of AN and BN2,11 and other psychiatric disorders, including depressive30 and anxiety disorders.29 The present study administered the LIFE to measure the presence and severity of psychopathology on a weekly basis for the prior interval period (using the calendar recall method). The LIFE quantifies the severity of psychopathology on weekly “Psychiatric Status Ratings” (PSRs), which are made for each disorder present. For ED, PSRs use the following three-point scale: PSR = 1 signifies no symptoms; PSR = 2 correspond to subthreshold symptoms with up to moderate functional impairment; and PSR = 3 indicate symptoms meeting full diagnostic criteria. Studies have reported good to excellent reliability for the LIFE.29,31 Assessors in this study were trained and certified by the LIFE developers and official training staff at Brown University. Official LIFE trainers provided ongoing training and consultation regarding the LIFE and we followed methods that have been demonstrated to maintain long-term reliability.31
Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV)
The DIPD-IV26 is a semi-structured diagnostic interview for assessing PD. Each of the criteria for all PD diagnoses is assessed with one or more questions, which are then rated on a three-point scale (0 = not present; 1 = present but of uncertain clinical significance; 2 = present and clinically significant). The DIPD-IV requires that criteria be present and pervasive for at least 2 years and be characteristic of the person for most of his/her adult life to be counted toward a diagnosis. In the present study, inter-rater reliability (based on 84 pairs of raters) kappa coefficients for PD ranged from 0.58 to 1.0.24
DIPD-IV-Follow-Along Version (DIPD-IV-FAV)
The DIPD-FAV28 is a modified version of the DIPD-IV developed specifically for assessing the longitudinal course of PD. Each PD is assessed longitudinally with ratings made on a scale (0, 1, 2) for each month during the specific interval time period assessed. Reliability on the DIPD-IV-FAV based on the ratings of two overlapping time points (i.e., Month 6 was rated twice for N = 453 cases) resulted in kappa coefficients ranging 0.68–0.78.
Life Events Assessment
The LEA20 assesses the occurrence of stressful life events including their specific timing during the specific interval period facilitated by the use of the calendar recall method. The LEA was empirically established20 and has been used in longitudinal studies of other psychiatric problems, including alcohol use disorders.21 Participants are asked if any of a list of 82 events or circumstances occurred since the last follow-up interview. For any endorsed stressful events, participants are asked to provide the start and end dates for each specific event using the calendar for the interval period. The LEA assesses 59 negative events and 23 positive events subcategorized into stress domain domains (see Table 1): work, school, social/friendship, love, family, health, and financial; two other domains—crime/legal and children—were infrequently endorsed and therefore not analyzed.26 Pagano et al.20 found low associations between items within stress domain categories and between stress domain categories (r = 0.07–0.34).
TABLE 1.
Stressful life events as time-varying predictors of eating disorder (ED) relapse
| Strength of Effect on Predicting Time to Eating Disorder Relapsea |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| SLEb | Duration of ED | # Axis I Disorders | BPD Criteriac | OCPD Criteriad | ||||||
| Stressful life event | HRe | p | HR | p | HR | p | HR | p | HR | p |
| Total positive events | 1.08 | 0.89 | 1.02 | 0.14 | 0.95 | 0.65 | 1.86 | 0.25 | 0.51 | 0.33 |
| Total negative events | 1.52 | 0.04 | 1.03 | 0.11 | 0.93 | 0.48 | 1.98 | 0.23 | 0.49 | 0.29 |
| Work | 3.04 | 0.01 | 1.02 | 0.11 | 0.94 | 0.58 | 1.66 | 0.35 | 0.61 | 0.49 |
| School | 1.93 | 0.37 | 1.02 | 0.12 | 0.95 | 0.62 | 1.82 | 0.27 | 0.49 | 0.29 |
| Social/friendship | 3.13 | 0.04 | 1.02 | 0.13 | 0.95 | 0.59 | 1.94 | 0.23 | 0.48 | 0.29 |
| Love/marriage | 1.11 | 0.89 | 1.02 | 0.14 | 0.95 | 0.65 | 1.87 | 0.25 | 0.51 | 0.32 |
| Family | 0.36 | 0.31 | 1.02 | 0.15 | 0.96 | 0.69 | 1.81 | 0.27 | 0.51 | 0.33 |
| Health | 2.13 | 0.22 | 1.02 | 0.13 | 0.95 | 0.62 | 1.83 | 0.26 | 0.45 | 0.25 |
| Financial | 2.23 | 0.44 | 1.02 | 0.13 | 0.95 | 0.63 | 1.89 | 0.24 | 0.49 | 0.31 |
Of the 117 patients with eating disorders (comprising bulimia nervosa and eating disorder not otherwise specified), 50 (43%) relapsed during the 6-year period of prospective follow-up.
SLE = stressful life events, which were tested as time-varying predictors
Time-varying proportion of number of borderline personality disorder (BPD) criteria met.
Time-varying proportion of number of obsessive compulsive personality disorder (OCPD) criteria met.
HR = hazard ratio, shown with p = significance level for two-tailed test.
Definitions of Remission and Relapse
Remission from BN and EDNOS was defined as eight consecutive weeks with PSR ratings on the LIFE less than two. Relapse was defined as eight consecutive weeks with PSR ratings of two or greater (reflecting any ED). Thus, in defining relapse we aimed to determine a return of any clinically-meaningful ED symptoms with impairment without regard to whether participants relapsed to the “same” ED diagnosis (BN versus EDNOS) or “migrated” to a different ED diagnosis (see Ref. 3). These definitions of remission and relapse parallel those used in studies of other psychiatric disorders.30
Data Analyses
Statistical analyses were conducted using SAS version 8.0, using PROC FREQ, PROC ANOVA, PROC LIFETEST, and PROC PHREG. Lifetable survival methods32 were used to analyze time to ED relapse among patients with remitted ED. The Kaplan–Meier33 method, which is well suited for analyzing longitudinal data for psychiatric problems,34 was used to estimate cumulative relapse rates. Wilcoxon chi-square test was used to compare proportion of BN and EDNOS that relapsed. Cox proportional hazards regression (PHREG) tests for significance35 were used for the omnibus predictor analysis of time to ED relapse (determined using the LIFE). PHREG tested stressful life events as time-varying predictors of time to ED relapse jointly along with two predictor variables reflecting severity (number of psychiatric disorders and ED duration, determined using the SCID-I/P) and two time-varying covariates reflecting dimensional changes in PD (i.e., changes in number of criteria for BPD and OCPD, determined using the DIPD-IV-FAV). Analyses were able to examine time-varying changes in the predictor variables (SLE and PD-status) prior to ED relapse because of the nature of the LIFE-FAV, DIPD-FAV, and LEA structured interview assessments that pinpointed events and changes facilitated by the use of calendar recall methods. In predicting time to ED relapse in these PHREG analyses, we collapsed together BN and EDNOS given the absence of differences in time to relapse between these two diagnoses.
Results
Relapse Among BN and EDNOS Over 60 Months
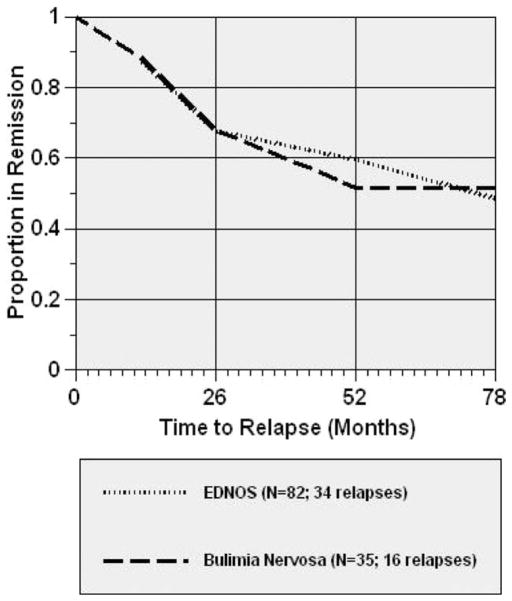
Figure 1 represents the survival curves showing time to ED relapse for those patients who had remitted. For BN, 16 (46%) of the 35 remitted patients subsequently relapsed. For EDNOS, 34 (41%) of the 82 remitted patients subsequently relapsed. Time to relapse did not differ between BN and EDNOS (Wilcoxon X2 = 0.02, p = 0.88).
FIGURE 1.
Figure shows survival curves representing time to relapse for remitted cases of BN and EDNOS. In this analysis, 78 months of data were analyzed comprising 6 months of ED data obtained retrospectively at baseline and 72 months of data obtained prospectively through repeated assessments at 6, 12 months, and annually (6 years) thereafter. Time 0 represents the first prospectively observed day of remission for all cases.
Stressful Life Events Predicting Time to ED Relapse: Omnibus Analyses
Table 1 summarizes Cox PHREG analyses testing stressful life events as time-varying predictors of time to ED relapse jointly along with predictor variables reflecting severity and time-varying covariates reflecting PD psychopathology. Cox PHREG analyses revealed that the total number of stressful negative life events significantly predicted time to relapse (hazard ratio (HR) = 1.52, p < 0.04). Specific types of stressful life events that predicted ED relapse were elevated work stressors (HR = 3.04, p < 0.01) and social/friendship stressors (HR = 3.13, p <0.04). In the nine sets of PHREG (conducted separately for each class of stressful life events), none of the covariates (psychiatric comorbidity, ED duration, dimensional changes in BPD/OCPD status) were statistically significant. The hazard ratio was close to 1.0 for both psychiatric disorder comorbidity (HR range = 0.93–0.95, p-value range: 0.48–0.69) and ED duration (HR range = 0.93–0.95, p-value range: 0.48–0.69), indicating no meaningful association between these covariates and time to ED relapse. Although not statistically significant, higher proportions of BPD criteria increased the speed to ED relapse (HR range = 1.66–1.98, p-value range = 0.23–0.35) whereas higher proportions of OCPD criteria decreased the speed to ED relapse (HR range = 0.45–0.61, p-value range = 0.25–0.33).
Discussion
The present report represents a novel contribution to the literature on the prospective associations between time-varying fluctuations in stressful life events and PD psychopathology and subsequent relapse among women who had remitted from BN and EDNOS. First, the 6-year natural course of post-remission relapse in BN and EDNOS differed little, with both ED categories showing similar proportions of relapses and time to relapse. These findings add to the growing literature regarding the clinical significance of EDNOS36 and the need for further research on this most common ED diagnosis.6,7 Second, higher work stress (e.g., serious difficulties at work, laid off or fired) and higher social/friendship stress (e.g., broke up with a friend, lost a friend) represent significant warning signs for triggering relapse for women in remission from BN and EDNOS. Third, two clinical severity predictors with mixed support in the literature,1 psychiatric disorder co-morbidity and ED duration, were unrelated to ED relapse. Time-varying dimensional changes of co-occurring PD psychopathology were not statistically significantly related to relapse but inspection of effect sizes suggests that higher BPD scores may increase chances while higher OCPD scores may decrease chances of ED relapse when considered jointly with SLEs.
Over the 6-year period of prospective follow-up in this study, the probability of post-remission relapse was 46% for BN and 41% for EDNOS. These findings suggest that EDNOS is a clinically-meaningful category that has roughly the same course as BN over 6 years. Thus, the current EDNOS construct, although flawed, does capture a clinically meaningful group of persons with ED-related problems (see Ref. 36). The challenge for DSM-V is to define more useful categories for clinicians and researchers.
Our findings suggest that the occurrences of negative stressful life events, most notably higher work stress and higher social stress, represent significant warning signs for relapse among women in remission from BN and EDNOS. These specific stressors (work or unemployment issues and social-interpersonal issues) have been found to impact negatively on other health outcomes in previous prospective studies37 and our findings increase their generalizability to predicting worse course in patients with ED. These findings might suggest that clinicians working with these ED patient groups consider integrating relapse prevention and coping skills methods for dealing with stressful life events.
We note several methodological issues as context for interpreting our findings as well as for informing future research efforts. We focused on BN and EDNOS and therefore cannot address the course of AN. As our participants were patients recruited for a longitudinal study with a primary focus on PD and MDD, our findings may not generalize to non-treatment-seeking community samples of individuals with ED or patients who present to ED specialty clinics, which themselves might have different forms of clinical biases. Given our recruitment methods, the rates of PD in our ED patients are higher than reported for some clinic-based samples14 although the high proportion of EDNOS observed in our study group is consistent with findings reported by both general psychiatric services6 and by other studies of patients with PD.38 We note our findings regarding stress and relapse may also not generalize to ED patient groups largely or completely free of PD psychopathology. It is possible, for example, that ED patients without PD experience fewer stressful life events or cope with them differently than ED patients with PD. Our sample size may have precluded us from identifying other significant predictors. While the hazards ratios for psychiatric co-morbidity and ED duration were close to 1.0 (indicating no association), the hazard ratios for time-varying changes in BPD (range 1.66–1.98) and OCPD (range 0.45–0.61) criteria—while not statistically significant are perhaps clinically meaningful.
Another methodological limitation concerns the ED assessments. We relied on the LIFE, the primary assessment instrument used in major longitudinal studies of psychiatric disorders30 and in landmark ED studies.2,11 This assessment instrument, however, did not allow examination of changes in the core features of ED (i.e., overvaluation of shape/weight39) during relapses or examination of specific examples of EDNOS, such as binge eating disorder or subsyndromal variants of specific ED. Although other assessment instruments can provide more detailed data regarding ED features at specific time-points,40 those approaches—unlike the LIFE—do not lend themselves well to survival analyses. A related issue is that the LIFE definitions of remission and relapse (i.e., 8 consecutive weeks with no symptoms) while representing widely-used research conventions across psychiatric disorders including ED2,11 do not reflect formal (e.g., DSM-IV) nomenclature.
A final limitation is the potential for confounding by treatment, a characteristic of all naturalistic longitudinal studies of clinically ascertained participants. We have previously documented that PD severity was positively associated prospectively with treatment utilization.41 These findings, which converge with most naturalistic studies,42 indicate that clinical severity drives treatment use. These findings parallel reports of intensive (inpatient) treatments predicting worse ED outcomes, which likely reflects greater severity.9 We emphasize that our study was designed to examine prospectively the impact of stressful life events on relapse in women in real-world clinical settings who had remitted from BN or EDNOS, not with experimentally manipulated treatments (controlled treatment trials). Indeed, in contrast to naturalistically-delivered treatments in the community, which tend to be unrelated to BN/EDNOS outcomes,9 empirically-supported treatments for these diagnoses at specialty programs tends to produce robust outcomes.5
Several notable methodological strengths also provide context for our findings. Our design was prospective and experienced and highly trained assessors administered well-established structured diagnostic and clinical interviews annually over a 6-year period. Our analyses represent a novel contribution to the longitudinal literature in examining time-varying changes in both the occurrence of stressful life events and in the fluctuating nature of dimensional scores of two contrasting forms of PD psychopathology (i.e., BPD and OCPD). Our analyses were able to examine time-varying changes in these predictor variables (stressful life events and PD-status) prior to ED relapse because of the nature of the three structured interview assessments repeated annually that pin-pointed the timing of events and changes using detailed calendar recall methods. These prospective analyses support the potential role of negative stressful life events, and specifically higher work stress and higher social stress, in increasing risk for relapse among women in remission from BN/EDNOS.
Acknowledgments
Supported by MH 50837, 50838, 50839, 50840, 50850, K24 DK070052, UL1 DE019586, K01 AA 015137, K23 MH80221, K23 MH80221 from NIH.
References
- 1.Keel PK, Brown TA. Update on course and outcome in eating disorders. Int J Eat Disord. 2010;43:195–204. doi: 10.1002/eat.20810. [DOI] [PubMed] [Google Scholar]
- 2.Herzog DB, Dorer DJ, Keel PK, Selwyn SE, Ekeblad ER, Flores AT, et al. Recovery and relapse in anorexia and bulimia nervosa: A 7. 5-year-follow-up study. J Am Acad Child Adolesc Psychiatry. 1999;38:829–837. doi: 10.1097/00004583-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 3.Milos G, Spindler A, Schnyder U, Fairburn CG. Instability of eating disorder diagnoses: Prospective study. Br J Psychiatry. 2005;187:573–578. doi: 10.1192/bjp.187.6.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agras WS, Crow S, Mitchell JE, Halmi KA, Bryson S. A 4-year prospective study of EDNOS compared with full eating disorder syndromes. Int J Eat Disord. 2009;42:565–570. doi: 10.1002/eat.20708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson GT, Grilo CM, Vitousek K. Psychological treatments for eating disorders. Am Psychol. 2007;62:199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman M, Francione-Witt C, Chelminski I, Young D, Tortolani C. Problems applying the DSM-IV eating disorders diagnostic criteria in a general psychiatric outpatient practice. J Clin Psychiatry. 2008;69:381–384. doi: 10.4088/jcp.v69n0306. [DOI] [PubMed] [Google Scholar]
- 7.Rockert W, Kaplan AS, Olmsted MP. Eating disorder not otherwise specified: The view from a tertiary care treatment center. Int J Eat Disord. 2007;40:S99–S103. doi: 10.1002/eat.20482. [DOI] [PubMed] [Google Scholar]
- 8.Grilo CM. What treatment research is needed for eating disorder not otherwise specified and binge eating disorder. In: Grilo CM, Mitchell JE, editors. Treatment of Eating Disorders: A Clinical Handbook. New York: Guilford Press; 2010. pp. 554–568. [Google Scholar]
- 9.Ben-Tovin DI, Walker K, Gilchrist P, Freeman R, Kalucy R, Esterman A. Outcome in patients with eating disorders: A 5-year study. Lancet. 2001;357:1254–1257. doi: 10.1016/S0140-6736(00)04406-8. [DOI] [PubMed] [Google Scholar]
- 10.Grilo CM, Pagano ME, Skodol AE, Sanislow CA, McGlashan TH, Gunderson JG, et al. Natural course of bulimia nervosa and of eating disorder not otherwise specified: 5-year prospective study of remissions, relapses, and the effects of personality disorder psychopathology. J Clin Psychiatry. 2007;68:738–746. doi: 10.4088/jcp.v68n0511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Strober M, Freeman R, Morrell W. The long-term course of severe anorexia nervosa in adolescents: Survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int J Eating Disord. 1997;22:339–360. doi: 10.1002/(sici)1098-108x(199712)22:4<339::aid-eat1>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 12.Keel PK, Dorer DJ, Franko DL, Jackson SC, Herzog DB. Postremission predictors of relapse in women with eating disorders. Am J Psychiatry. 2005;162:2263–2268. doi: 10.1176/appi.ajp.162.12.2263. [DOI] [PubMed] [Google Scholar]
- 13.Thompson-Brenner H, Eddy KT, Franko DL, Dorer DJ, Vashchenko M, Kass AE, et al. A personality classification system for eating disorders: A longitudinal study. Comp Psychiatry. 2008;49:551–560. doi: 10.1016/j.comppsych.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 14.Grilo CM. Recent research of relationships among eating disorders and personality disorders. Curr Psychiatry Rep. 2002;4:18–24. doi: 10.1007/s11920-002-0007-8. [DOI] [PubMed] [Google Scholar]
- 15.Daley SE, Hammen C, Davilla J, Burge D. Axis II symptomatology, depression, and life stress during the transition from adolescence to adulthood. J Consult Clin Psychol. 1998;66:595–603. doi: 10.1037//0022-006x.66.4.595. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell JE, Davis L, Goff G. The process of relapse in patients with bulimia. Int J Eat Disord. 1985;4:457–463. [Google Scholar]
- 17.Sohlberg S. Personality, life stress and the course of eating disorders. Acta Psychr Scand. 1990;82:29–33. [PubMed] [Google Scholar]
- 18.Grilo CM, Shea MT, Sanislow CA, et al. Two-year stability and change of schizotypal, borderline, avoidant, and obsessive-compulsive personality disorders. J Consult Clin Psychol. 2004;72:767–775. doi: 10.1037/0022-006X.72.5.767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skodol AE, Oldham JM, Bender DS, et al. Dimensional representations of DSM-IV personality disorders: Relationships to functional impairment. Am J Psychiatry. 2005;162:1919–1925. doi: 10.1176/appi.ajp.162.10.1919. [DOI] [PubMed] [Google Scholar]
- 20.Pagano ME, Skodol AE, Stout RL, Shea MT, Yen S, Grilo CM, et al. Stressful life events as predictors of functioning: findings from the Collaborative Longitudinal Personality Disorders Study. Acta Psychiatr Scand. 2004;110:421–429. doi: 10.1111/j.1600-0447.2004.00398.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reyes CD, Pagano ME, Ronis RJ. The impact of stressful life events on alcohol use relapse. J Dual Diagn. 2009;5:226–232. doi: 10.1080/15504260902886505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gunderson JG, Shea MT, Skodol AE, et al. The Collaborative Longitudinal Personality Disorders Study: Development, aims, designs and sample characteristics. J Pers Disord. 2000;14:300–315. doi: 10.1521/pedi.2000.14.4.300. [DOI] [PubMed] [Google Scholar]
- 23.McGlashan TH, Grilo CM, Skodol AE, et al. The collaborative longitudinal personality disorders study: Baseline axis I/II and axis II/II co-occurrence. Acta Psychiatr Scand. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- 24.Zanarini MC, Skodol AE, Bender D, et al. The Collaborative Longitudinal Personality Disorders Study: Reliability of axis I and II diagnoses. J Pers Disord. 2000;14:291–229. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]
- 25.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- 26.Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders. Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- 27.Keller MB, Lavori PW, Friedman B, et al. The longitudinal interval follow-up evaluation. Arch Gen Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 28.Zanarini MC, Shea MT. The Diagnostic Interview for DSM-IV Personality Disorders-Follow-Along-Version (DIPD-IV-FAV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- 29.Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. J Psychiatr Res. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 30.Solomon DA, Keller MB, Leon AC, et al. Recovery from major depression: A 10-year prospective follow-up across multiple episodes. Arch Gen Psychiatry. 1999;54:1001–1006. doi: 10.1001/archpsyc.1997.01830230033005. [DOI] [PubMed] [Google Scholar]
- 31.Warshaw MG, Dyck I, Allsworth J, Stout RL, Keller MB. Maintaining reliability in a long-term psychiatric study: An ongoing inter-rater reliability monitoring program using the longitudinal interval follow-up evaluation. J Psychiatr Res. 2001:297–305. doi: 10.1016/s0022-3956(01)00030-9. [DOI] [PubMed] [Google Scholar]
- 32.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. New York: Wiley; 1980. [Google Scholar]
- 33.Kaplan EL, Maier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [Google Scholar]
- 34.Fleiss JL, Dunner DL, Stallone F, et al. The life table: A method for analyzing longitudinal studies. Arch Gen Psychiatry. 1976;33:107–112. doi: 10.1001/archpsyc.1976.01770010067013. [DOI] [PubMed] [Google Scholar]
- 35.Cox DR. Regression models and life tables. J R Stat Soc. 1972;34:187–220. [Google Scholar]
- 36.Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, et al. Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- 37.Cohen S, Frank E, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM. Types of stressors that increase susceptibility to the common cold in healthy adults. Health Psychol. 1998;17:214–223. doi: 10.1037//0278-6133.17.3.214. [DOI] [PubMed] [Google Scholar]
- 38.Zanarini MC, Reichman CA, Frankenburg FR, Reich DB, Fitzmaurice G. The course of eating disorders in patients with borderline personality disorder: A 10-year follow-up study. Int J Eat Disord. 2010;43:226–232. doi: 10.1002/eat.20689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grilo CM, Crosby RD, Masheb RM, et al. Overvaluation of shape and weight in binge eating disorder, bulimia nervosa, and sub--threshold bulimia nervosa. Behav Res Ther. 2009;47:692–696. doi: 10.1016/j.brat.2009.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Grilo CM, Masheb RM, Wilson GT. A comparison of different methods for assessing the features of eating disorders in patients with binge eating disorder. J Consult Clin Psychol. 2001;69:317–322. doi: 10.1037//0022-006x.69.2.317. [DOI] [PubMed] [Google Scholar]
- 41.Bender DS, Skodol AE, Pagano ME, et al. Prospective assessment of treatment use by patients with personality disorders. Psychiatr Serv. 2006;57:254–257. doi: 10.1176/appi.ps.57.2.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cochran W. Planning and Analysis of Observational Studies. New York: Wiley; 1983. [Google Scholar]