Abstract
Standing posterior–anterior (PA) radiographs from our clinical practice show that the concave and convex ilia are not always symmetrical in patients with adolescent idiopathic scoliosis (AIS). Transverse pelvic rotation may explain this observation, or pelvic asymmetry may be responsible. The present study investigated pelvic symmetry by examining the volume and linear measurements of the two hipbones in patients with AIS. Forty-two female patients with AIS were recruited for the study. Standing PA radiographs (covering the thoracic and lumbar spinal regions and the entire pelvis), CT scans and 3D reconstructions of the pelvis were obtained for all subjects. The concave/convex ratio of the inferior ilium at the sacroiliac joint medially (SI) and the anterior superior iliac spine laterally (ASIS) were measured on PA radiographs. Hipbone volumes and several distortion and abduction parameters were measured by post-processing software. The concave/convex ratio of SI–ASIS on PA radiographs was 0.97, which was significantly < 1 (P < 0.001). The concave and convex hipbone volumes were comparable in patients with AIS. The hipbone volumes were 257.3 ± 43.5 cm3 and 256.9 ± 42.6 cm3 at the concave and convex sides, respectively (P > 0.05). Furthermore, all distortion and abduction parameters were comparable between the convex and concave sides. Therefore, the present study showed that there was no pelvic asymmetry in patients with AIS, although the concave/convex ratio of SI–ASIS on PA radiographs was significantly < 1. The clinical phenomenon of asymmetrical concave and convex ilia in patients with AIS in preoperative standing PA radiographs may be caused by transverse pelvic rotation, but it is not due to developmental asymmetry or distortion of the pelvis.
Keywords: adolescent idiopathic scoliosis, distortion, hipbone, pelvic rotation, volume
Introduction
There is evidence of pelvic abnormalities in patients with adolescent idiopathic scoliosis (AIS) (Saji et al. 1995; Karski, 2005; Cheung et al. 2008). Patients with scoliosis have significantly greater femoral neck-shaft angles in both hips compared with normal subjects, and the increased femoral neck-shaft angle is related to the type and side of spinal curvature (Saji et al. 1995). Furthermore, an adduction range deficit of the right hip has been observed (Karski, 2005). This observation has been supported by another recent study (Cheung et al. 2008), in which the difference in hip adduction range between the right and left hips was shown to be 5° (P < 0.05). Of 102 patients, 64 had an adduction range deficit of the right hip, four of the left hip, and 34 showed no differences between the two hips (Cheung et al. 2008).
In our clinical practice, preoperative standing posterior–anterior (PA) radiographs show that concave and convex ilia are not always symmetrical in patients with AIS. The right ilium often appears to be wider than the left ilium in patients with major thoracic curves, while the left ilium often appears to be wider than the right ilium in patients with major thoracolumbar/lumbar curves. Gum et al. (2007) have also noted this phenomenon and interpreted it as the result of transverse pelvic rotation. They suggested that the transverse plane pelvic position that accompanies major thoracic curves is the fourth transverse plane compensation. The direction of transverse pelvic rotation is the same as that for the main thoracic curve in most patients with a compensatory thoracolumbar/lumbar curve.
This research on pelvic abnormalities in patients with AIS led us to wonder if such abnormalities and not transverse pelvic rotation also caused the asymmetry of the concave and convex ilia that can be seen in standing PA radiographs. Several pelvic abnormalities could cause this clinical observation. One possibility is that one hipbone is more developed (i.e. a greater hipbone volume is present). A second possibility is that one hipbone is more abducent. Finally, a third possibility is distortion of the hipbones. However, to the best of our knowledge, no study has examined the volumes, distortion or abduction of hipbones from patients with AIS. Are the concave and convex volumes of the hipbones comparable in patients with AIS? Is the abduction of one hipbone similar to that of the other? Is there any distortion of the hipbones? With these questions in mind, the present study was conducted to explore pelvic symmetry in patients with AIS, and to examine hipbone volume and linear measurements specifically.
Subjects and methods
Subjects and groupings
Forty-two female patients with AIS were recruited for the study. All patients had previously received standing PA spine radiographs and a pelvic CT scan for a large project in our centre. These previously acquired data were examined for this study. All patients met the following inclusion criteria: first, closure of triradiate cartilage; second, symmetrical Risser grade on the left and right sides; third, no prior pelvic surgery; and fourth, no developmental deformity of the lower extremities. The age of the subjects ranged from 13 to 18 years (mean: 15.4 ± 1.1 years). Ethical approval was obtained from the University and Hospital Research Ethics Committee. Informed consent was obtained from all study subjects and their parents or guardians before any of the examinations or measurements were conducted.
While the patients were in a standing position, posterior to anterior exposure coronal spine radiographs covering the thoracic and lumbar spinal regions and the whole pelvis were taken on 14 × 17 in. film at a 200-cm tube to film distance. Scoliosis curves were measured using the Cobb method.
In this study, the Cobb angles were not large enough to use the Lenke classification system. The subjects were divided into three groups: Group 1 subjects had a main thoracic curve; Group 2 subjects had a main thoracolumbar/lumbar curve; and Group 3 subjects had double major curves (thoracic curve and thoracolumbar/lumbar curve). In Group 3, the concave and convex sides were referred to as the large curve. Proximal thoracic curves were disregarded in this study.
Concave/convex ratio of hipbone widths in PA radiographs
The concave/convex ratio of hipbone widths in PA radiographs was determined as previously described (Gum et al. 2007). The inferior ilium at the sacroiliac joint (SI) medially and the anterior superior iliac spine (ASIS) laterally were determined on both sides. For each side, the linear distance between upright lines through these points (SI–ASIS) was measured and expressed as a concave/convex ratio (Fig. 1).
Fig. 1.
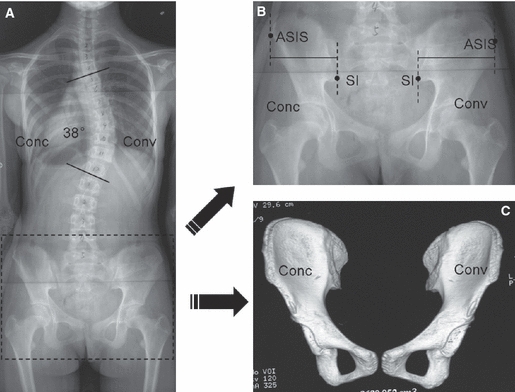
(A) The PA radiograph of a 14-year-old female patient with AIS with a main thoracic curve of 38°. (B) The location of the hipbone landmarks. The inferior ilium at the sacroiliac joint (SI) and anterior superior iliac spine (ASIS) are indicated. The distance between two plumb lines through the SI and ASIS was defined as the SI–ASIS. The concave/convex ratio of the SI–ASIS in this patient was 0.87. (C) The 3D reconstruction of the hipbones after the CT scan. The hipbone volume was 215.2 cm3 at the concave side and 215.7 cm3 at the convex side.
Measurement of hipbone volumes
Patients were scanned using a light speed 16 pro spiral CT scanner (GE, Connecticut, USA) with 0.625-mm CT slices at 300 mA and 120 kV. The images were imported into the ADW4.2 work platform. Three-dimensional reconstructions of the hipbones were generated (Fig. 1), and the hipbone volumes were measured by the post-processing software (Volume Viewer).
Distortion and abduction measurements of the hipbones
A reference coordinate system was established to measure the distortion and abduction of the reconstructed 3D pelvis. The line that passed through two anterior–superior iliac spines was defined as the y-axis and was orientated from right to left. The x-axis was perpendicular to the y-axis, passed through the middle point of the upper sacral plate and was oriented anteriorly. The z-axis was perpendicular to the y- and x-axes, passed through the intersection of the x- and y-axes and was oriented upward.
Three parameters were measured on both sides using the projection plane of the 3D pelvis into the yz-plane (Fig. 2).
Fig. 2.
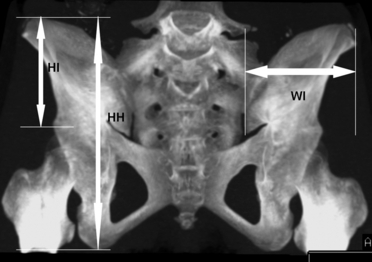
The projection plane of the 3D pelvis into the yz-plane and the measurements of the height of the hipbone (HH), height of the ilium (HI) and width of the ilium (WI).
Height of hipbone (HH): one line was passed through the upper margin of the ilium, parallel to the y-axis. The other line was passed through the ischial tuberosity, parallel to the y-axis. The distance between these two lines was defined as HH.
Height of ilium (HI): one line was passed through the upper margin of the ilium, parallel to the y-axis. The other line was passed through the upper margin of the femoral head, parallel to the y-axis. The distance between these two lines was defined as HI.
Width of ilium (WI): one line was passed through the inferior ilium at the SI, parallel to the z-axis. The other line was passed through the lateral margin of the ilium, parallel to the z-axis. The distance between these two lines was defined as WI.
The following parameters were measured on the transverse section (TS1) passing through two anterior–superior iliac spines and the middle point of the upper sacral plate (Fig. 3).
Fig. 3.
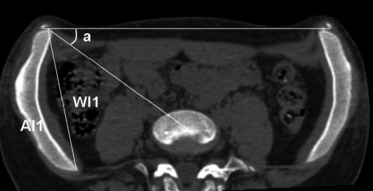
The measurements of the abduction of the ilium (a), the true width of the ilium 1 (WI1) and the area of the transverse section of the ilium 1 (AI1).
4. The abduction of the ilium (a): the angle between the line passing through the two anterior–superior iliac spines and the line passing through one anterior–superior iliac spine and the middle point of the upper sacral plate.
5. True width of the ilium 1 (WI1): the distance between the upper margin of the ilium and the lower margin of the ilium in TS1.
6. The area of the transverse section of the ilium 1 (AI1): the area of the transverse section of the ilium in TS1.
Transverse section 2 (TS2) was 1.5 cm below TS1 and parallel to TS1, and transverse section 3 (TS3) was 3.0 cm below TS1 and parallel to TS1. The following parameters were measured using TS2 and TS3.
7. True width of the ilium 2 (WI2): the distance between the upper margin of the ilium and the lower margin of the ilium in TS2.
8. The area of the transverse section of the ilium 2 (AI2): the area of the transverse section of the ilium in TS2.
9. True width of the ilium 3 (WI3): the distance between the upper margin of the ilium and the lower margin of the ilium in TS3.
10. The area of the transverse section of the ilium 3 (AI3): the area of the transverse section of the ilium in TS3.
Interobserver and intraobserver measurement variability
To test the interobserver and intraobserver variability of measurements other than the volume of the hipbone, the parameters of 10 patients were measured by two observers (Yang SW, QIU XS) on two different occasions.
Statistical analysis
Pearson's rank correlation coefficients were used to assess measurement variability. Paired t-tests were used to compare all the parameters between concave and convex hipbones, and correlation analysis was performed between SI–ASIS and Cobb angles.
Results
The average maximum Cobb angle of all patients was 25.3 ± 7.2°. The 12 subjects in Group 1 had an average Cobb angle of 23.4 ± 8.1°, the eight subjects in Group 2 had an average Cobb angle of 18.6 ± 5.6°, and the 22 subjects in Group 3 had an average maximum Cobb angle of 28.7 ± 5.0°.
Overall, the concave/convex ratio of SI–ASIS was 0.97, which was significantly < 1 (P < 0.001; Table 1). When subdivided into the three curve patterns, the concave/convex ratio of SI–ASIS remained significantly < 1 in Group 3.
Table 1.
Comparison of the concave/convex ratios of SI–ASIS in patients with AIS
| Concave/convex ratios of SI–ASIS | |||
|---|---|---|---|
| Curve type | N | Mean ± SD | P-value |
| All | 42 | 0.97 ± 0.03 | < 0.0001* |
| Group 1 | 12 | 0.98 ± 0.04 | 0.12 |
| Group 2 | 8 | 0.98 ± 0.03 | 0.06 |
| Group 3 | 22 | 0.97 ± 0.03 | 0.001* |
Group 1: thoracic curve group; Group 2: thoracolumbar/lumbar curve group; Group 3: double curve group.
SI–ASIS, the distance between two plumb lines through the inferior ilium at the sacroiliac joint (SI) and the anterior superior iliac spine (ASIS).
P (mean compared with 1).
Overall, the concave and convex hipbone volumes were comparable in patients with AIS (Table 2). When subdivided by curve pattern, the hipbone volumes were 254.4 ± 33.6 cm3 at the concave side and 251.7 ± 32.6 cm3 at the convex side for Group 1; 240.3 ± 33.2 cm3 at the concave side and 239.7 ± 32.6 cm3 at the convex side for Group 2; and 265.2 ± 50.7 cm3 at the concave side and 266.1 ± 49.2 cm3 at the convex side for Group 3. There were no significant differences in hipbone volume between the concave and convex sides for any group (P > 0.05).
Table 2.
Comparison of the concave and convex hipbone volumes in patients with AIS
| Hipbone volumes (cm3) mean ± SD (range) | ||||
|---|---|---|---|---|
| Curve type | N | Concave | Convex | P-value |
| All | 42 | 257.3 ± 43.5 (172.0–357.1) | 256.9 ± 42.6 (174.1–356.2) | 0.75 |
| Group 1 | 12 | 254.4 ± 33.6 (215.1–327.8) | 251.7 ± 32.6 (216.0–320.5) | 0.10 |
| Group 2 | 8 | 240.3 ± 33.2 (188.9–282.7) | 239.7 ± 32.6 (191.3–279.6) | 0.74 |
| Group 3 | 22 | 265.2 ± 50.7 (172.0–357.1) | 266.1 ± 49.2 (174.1–356.2) | 0.59 |
Group 1: thoracic curve group; Group 2: thoracolumbar/lumbar curve group; Group 3: double curve group.
Overall, all of the distortion and abduction parameters (HI, HH, WI, a, WI1, WI2, WI3, AI1, AI2, AI3) were comparable between the convex and concave sides (Table 3). The same results were found when the data were examined in the three groups (data not shown).
Table 3.
Comparison of the distortion and abduction parameters of the concave and convex sides in patients with AIS
| Parameters | N | Concave | Convex | P-value |
|---|---|---|---|---|
| HI (mm) | 42 | 89.2 ± 8.6 | 88.9 ± 8.9 | 0.38 |
| HH (mm) | 42 | 172.7 ± 11.3 | 172.8 ± 10.8 | 0.87 |
| WI (mm) | 42 | 80.1 ± 14.7 | 80.1 ± 14.0 | 0.94 |
| a (°) | 42 | 34.3 ± 5.2 | 34.2 ± 4.8 | 0.59 |
| WI1 (mm) | 42 | 126.6 ± 14.9 | 127.4 ± 14.2 | 0.38 |
| WI2(mm) | 42 | 130.4 ± 10.6 | 130.4 ± 11.0 | 0.99 |
| WI3(mm) | 42 | 127.8 ± 17.8 | 127.6 ± 18.5 | 0.75 |
| AI1 (mm2) | 42 | 1430.4 ± 255.9 | 1444.6 ± 250.0 | 0.53 |
| AI2 (mm2) | 42 | 1673.8 ± 433.2 | 1665.1 ± 423.4 | 0.78 |
| AI3 (mm2) | 42 | 2340.6 ± 395.5 | 2307.9 ± 385.4 | 0.08 |
HI, HH and WI, height of the ilium, height of the hipbone and width of the ilium, respectively; a, abduction of the ilium; WI1, AI1, WI2, AI2, WI3 and AI3, true width of the ilium and the area of the ilium in transverse sections 1, 2 and 3, respectively.
Correlation analysis showed that there was no correlation between SI–ASIS and Cobb angles (P > 0.05). The Pearson correlation coefficients of interobserver repeat measurements for SI–ASIS, HH, HI, WI, a, WI1, WI2, WI3, AI1, AI2 and AI3 ranged from 0.96 to 0.99, and the Pearson correlation coefficients of intraobserver repeat measurements for SI–ASIS, HH, HI, WI, a, WI1, WI2, WI3, AI1, AI2 and AI3 ranged from 0.94 to 0.99. All correlations were statistically significant, and the level of measurement reliability was excellent.
Discussion
Adolescent idiopathic scoliosis is typically defined as a structural, lateral, rotated curvature of the spine that arises in otherwise healthy children at or around puberty (Miller et al. 2001; Goldberg et al. 2008; Weinstein et al. 2008). Most treatments are related to the spine (Weiss & Goodall, 2008; Kim et al. 2009; Negrini et al. 2010). However, several extra-spinal left–right skeletal length asymmetries or other asymmetries have been described. Normelli et al. (1985) found left–right asymmetries in thoracic skin temperature, breast size and vascularity, and periapical rib lengths, although the rib length finding is controversial (Sevastik et al. 2003). Burwell et al. (2006a,b,c) found that the upper arm is relatively longer on convexity in thoracic idiopathic scoliosis, the right leg is relatively longer in lower spine scoliosis (thoracolumbar and lumbar), and ilio-femoral length asymmetry in girls is significantly greater in scoliotics (−4.3 mm) than in normal controls (0.42 mm).
In our clinical practice, concave and convex ilia have often been found to be asymmetrical in patients with AIS in standing PA radiographs. The present study confirmed that the ilium width (ASIS–SI) on PA radiographs is not equivalent between the convex and concave sides in patients with AIS. This finding is similar to that of Gum et al. (2007). There are two possible explanations for this phenomenon. The first is hipbone asymmetry or other asymmetries in patients with AIS, and the second explanation is transverse pelvic rotation, as described by Gum et al. (2007). The present study showed that: first, the concave and convex hipbone volumes were equivalent in patients with AIS; second, the height of the hipbone (HH), height of the ilium (HI), true width of the ilium (WI) and area of the transverse section of the ilium (AI) in three transverse sections were comparable between the concave and convex sides; third, the abduction of the ilia (a) were comparable between concave and convex sides on the transverse section (TS1), and the width of the ilium (WI) of the 3D pelvis on the projection plane into the yz-plane was comparable between the concave and convex sides. Therefore, first, the two hipbones are symmetrically developed in patients with AIS; second, no distortion of two hipbones exists; and third, the abduction of the two hipbones are similar. In other words, there is no hipbone asymmetry. Therefore, the clinical phenomenon of asymmetrical concave and convex ilia is probably related to transverse pelvic rotation, as suggested by Gum et al. (2007). Burwell et al. (2006b) have reported that the concave ilium was related to lengthening in lower spine scoliosis (thoracolumbar and lumbar). However, we found that the height of the ilium (HI) was similar in the concave and convex sides in patients with AIS. The different results may be due to differences in inclusion criteria, because the study by Burwell and colleagues included both idiopathic scoliosis and pelvic tilt scoliosis patients.
Gum et al. (2007) hypothesised that the pelvis is significantly rotated in the same direction as the thoracic curve, and thus in the opposite direction of the thoracolumbar/lumbar curve. They found that for the group as a whole, this hypothesis was true with a L/R ratio of 0.95, which was significantly < 1 (P < 0.0001). The present study showed that the concave/convex ratio was 0.98 for Group 1 (the thoracic curve group), which partially supported this hypothesis. When applying this hypothesis to each Lenke curve type, Gum and colleagues found that there was significant static pelvic transverse plane rotation in the same direction as the thoracic curve in patients with single thoracic, double thoracic or double AIS curves that was large enough to warrant surgery. However, for patients with AIS with major thoracolumbar/lumbar curves or triple curves, there was no predictable correlation between pelvic rotation and curve direction. The present study suggests that there might be a predictable correlation between pelvic rotation and curve direction among the patients overall. The concave/convex ratio of SI–ASIS was < 1, which suggests that the pelvic transverse plane rotates in the same direction as the major curve in patients with AIS. The differences between the present study and the study by Gum et al. (2007) could be due to differences in curve severity and the grouping of subjects.
The present study showed that transverse pelvic rotation (SI–ASIS) did not increase with an increasing Cobb angle. However, the patients in the present study suffered from relatively weak scoliosis, with a Cobb angle of < 40°. We cannot speculate about transverse pelvic rotation in patients with more severe scoliosis or hypothesise about whether the two hipbones are symmetrical in these patients. Further studies are needed to obtain this information.
Conclusion
The present study showed that there is no hipbone asymmetry in patients with AIS with any curve type, although the concave/convex ratio of SI–ASIS was significantly < 1 in patients with AIS. Therefore, the clinical phenomenon of concave and convex ilia that appear asymmetrical in preoperative patients with AIS in standing PA radiographs may be due to transverse pelvic rotation. The pelvic transverse plane is rotated in the same direction as the major curve in patients with AIS.
Acknowledgments
This work was supported by the Key Project of the Provincial Department of Public Health, Jiangsu, China (BK2002141), and the National Natural Science Foundation of China (30901570).
References
- Burwell RG, Aujla RK, Freeman BJ, et al. Patterns of extra-spinal left-right skeletal asymmetries and proximo-distal disproportion in adolescent girls with lower spine scoliosis: ilio-femoral length asymmetry & bilateral tibial/foot length disproportion. Stud Health Technol Inform. 2006a;123:101–108. [PubMed] [Google Scholar]
- Burwell RG, Aujla RK, Freeman BJ, et al. Patterns of extra-spinal left-right skeletal asymmetries in adolescent girls with lower spine scoliosis: relative lengthening of the ilium on the curve concavity & of right lower limb segments. Stud Health Technol Inform. 2006b;123:57–65. [PubMed] [Google Scholar]
- Burwell RG, Freeman BJ, Dangerfield PH, et al. Left-right upper arm length asymmetry associated with apical vertebral rotation in subjects with thoracic scoliosis: anomaly of bilateral symmetry affecting vertebral, costal and upper arm physes? Stud Health Technol Inform. 2006c;123:66–71. [PubMed] [Google Scholar]
- Cheung KMC, Chooi YS, Cheung WY, et al. Hip adduction differences in adolescent idiopathic scoliosis a cause or effect of scoliosis. J Orthop Surg (Hong Kong) 2008;16:24–26. doi: 10.1177/230949900801600106. [DOI] [PubMed] [Google Scholar]
- Goldberg CJ, Moore DP, Fogarty EE, et al. Scoliosis: a review. Pediatr Surg Int. 2008;24:129–144. doi: 10.1007/s00383-007-2016-5. [DOI] [PubMed] [Google Scholar]
- Gum JL, Asher MA, Burton DC, et al. Transverse plane pelvic rotation in adolescent idiopathic scoliosis: primary or compensatory? Eur Spine J. 2007;16:1579–1586. doi: 10.1007/s00586-007-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karski T. Biomechanical explanation of etiology of the so called idiopathic scoliosis. Two etiopathological groups – important for treatment and neo-prophylaxis. Pan Arab J Ortho Trauma. 2005;9:123–135. [Google Scholar]
- Kim HJ, Blanco JS, Widmann RF. Update on the management of idiopathic scoliosis. Curr Opin Pediatr. 2009;21:55–64. doi: 10.1097/MOP.0b013e328320a929. [DOI] [PubMed] [Google Scholar]
- Miller NH, Schwab DL, Sponseller PD, et al. Characterization of idiopathic scoliosis in a clinically well-defined population. Clin Orthop Relat Res. 2001;392:349–357. doi: 10.1097/00003086-200111000-00045. [DOI] [PubMed] [Google Scholar]
- Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2010;1:CD006850. doi: 10.1002/14651858.CD006850.pub2. [DOI] [PubMed] [Google Scholar]
- Normelli H, Sevastik J, Akrivos J. The length and ash weight of the ribs of normal and scoliotic persons. Spine (Phila Pa 1976) 1985;10:590–592. doi: 10.1097/00007632-198507000-00015. [DOI] [PubMed] [Google Scholar]
- Saji MJ, Upadhyay SS, Leong JC. Increased femoral neck-shaft angles in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:303–311. doi: 10.1097/00007632-199502000-00008. [DOI] [PubMed] [Google Scholar]
- Sevastik J, Burwell RG, Dangerfield PH. A new concept for the etiopathogenesis of the thoracospinal deformity of idiopathic scoliosis: summary of an electronic focus group debate of the IBSE. Eur Spine J. 2003;12:440–450. doi: 10.1007/s00586-002-0489-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein SL, Dolan LA, Cheng JC, et al. Adolescent idiopathic scoliosis. Lancet. 2008;371:1527–1537. doi: 10.1016/S0140-6736(08)60658-3. [DOI] [PubMed] [Google Scholar]
- Weiss HR, Goodall D. The treatment of adolescent idiopathic scoliosis (AIS) according to present evidence. A systematic review. Eur J Phys Rehabil Med. 2008;44:177–193. [PubMed] [Google Scholar]


