Abstract
Background
In Ethiopia, utilization of health services remains low and unevenly distributed. To ensure appropriate health care use, we need to understand factors affecting health care use, and the reasons for low levels of utilization among our community. The objective of the study was to assess utilization of health services and associated factors in Jimma zone, south west Ethiopia.
Methods
A cross sectional data was collected from January 15 to February 08, 2007 in Jimma zone. First, four districts were selected by lottery method. Then 2 ‘kebeles’ from each district were selected randomly and households were selected by systematic sampling. A total of 836 households were studied. The data were cleaned, coded and entered into computer and analyzed using SPSS for windows version 12.0. Bivariate analysis and logistic regression were conducted and a significance level of 5% was considered for interpretation.
Results
The health services utilization rate was found to be 45.6%. After controlling confounders using logistic regression; sex (OR=0.23), marital status (OR=8.1), household income (OR=0.70), socioeconomic status (OR=3.5), presence of disabling health problem (OR=3.3), presence of an illness episode (OR=28.3), perceived transport cost (OR=3.6), perceived treatment cost (OR=0.15) and distance to the nearest health center or hospital (OR=2.9) were found to be predictors of utilization of health care.
Conclusion
It has been shown that utilization level was not satisfactory. Thus, we recommend that the level of health service utilization should be improved by improving predictors of health care use like physical accessibility.
Keywords: Health services utilization, accessibility, health status
Introdution
Utilization of health care services is an important public health and policy issue in developing countries. However, the level of health care services is not satisfactory in many countries of the world (1). In Ethiopia, the health care system is decentralized and free health service for those who cannot afford is being delivered. Though health service coverage is 86.7%, the availability of free service for the poor, remains very low (32%) and unevenly distributed (2). In a study undertaken in Amhara region of Ethiopia, 995 (5.6%) respondents were sick over the two weeks period preceding the survey and only 38.7% of them visited health institutions (3).
Actual utilization of health services will differ in accordance with various factors. Hence, if we are interested in not merely providing physical access, but also ensuring that modern health services are used by the population, we need to understand factors affecting health care utilization. According to Andersen, factors associated with utilization of health services include need factors (health status), predisposing factors, and enabling factors (4).
Need factors: Intensity of illness and number of spells significantly affect utilization of health care services. The higher the severity or number of illness episodes the higher the degree of utilization of services (5, 6). The way people report their health status is directly related to their use of medical services. In a study undertaken in southern Brazil in 2000, the probability of visiting a doctor was 30% for persons reporting excellent health, compared to those with poor health (7).
Predisposing factors: As the need for health care changes with age, gender, and marital status, utilization of health services also conforms accordingly. Studies in general found U-shaped relationship between age of patients and utilization of health care services (8). Other predisposing factors like education and family income have been seen to affect utilization of health services. For instance, a study in Ethiopia revealed that educational status of the mothers has a statistically significant association with the utilization of safe delivery services (10). Lack of money may lead to self-medication using modern pharmaceuticals and traditional medicines as observed in North West Ethiopia (13).
Enabling Factors: Researches have shown that increased distance between residents and health care providers decreases the utilization of health care (14). The analysis of user perception of quality offers a useful complement to those evaluations conducted from the point of view of professionals or public health authorities. In Saudi Arabia, the majority (79.0%) of the interviewees were satisfied with the primary health center services and reported that they preferred always to use the health services provided by the centre (15). Thus, the objective of the study was to assess utilization of health services and associated factors in Jimma zone, south west Ethiopia.
Materials and Methods
The survey was conducted in Jimma zone, south west Ethiopia from January 30 to February 08, 2007. The study design used was cross sectional. The sample size was calculated using Epi-Info 3.3.2 version statistical soft ware (Statcalc) using the single population proportion formula. A 95% confidence level; a health service utilization rate estimate of 0.5; a margin of error of 0.05 were taken to reach to a sample size of 384. A design effect of 2 was taken making the sample size 768. Finally, non-response rate of 10% was assumed to have a sample size of 845 households.
Multistage sampling was used. First four districts (Limu Kosa, Kersa, Mana and Dedo) were selected by lottery method. Then a total of 8 kebeles (2 from each of the selected districts) were included in the study randomly. Sample size of 845 households was proportionately distributed based on population size of the kebele. Then households were included in the survey by using systematic sampling. Finally, one individual from each of the sampled households was selected randomly. Whenever, the selected individual was less than 15 years of age, the caretaker was interviewed for the child.
The questionnaire was prepared after thorough literature search to suite the local needs and translated into Amharic. Furthermore, the questionnaire was pre-tested on 40 respondents outside of the study area before the start of actual data collection. Appropriate modifications of questionnaire were done based on the experience of the pre-test. Data were collected by high school completed individuals who were trained for 3 days. The data collectors were supervised and the collected data were reviewed on each data collection day for accuracy and consistency.
The main outcome variable: Utilization of health services.
Explanatory variables: Socio-demographic and behavioral factors were age, sex, marital status, occupation, education and perceived health status. Variables related to health services utilization were the presence of illness, and usual source of care. Health services access variables were time required to reach the nearest health facility, cultural acceptability and affordability of the services and family income.
Data were edited, cleaned, coded and entered into computer and analyzed by SPSS-version 12.0. First bivariate analysis was conducted. Then, to identify predictor variables binary logistic regression was performed. Tests of interactions and collinearity (VIF <10) were also undertaken. Variables were included into the model based on their level of significance (p<0.05 in the bivariate analysis) and scientific plausibility.
Before the start of data collection, the proposal was submitted to the ethical clearance committee of Jimma University and permission was obtained. Cooperation letter was delivered to Jimma Zone, the four districts' and the eight kebeles' administration. Oral consent was obtained from the respondents and confidentiality was assured for any information provided.
The following operational definitions were used;
Utilization: If a person visited a health care giver in the previous 12 months.
Utilization rate: refers to the number of times in the previous 12 months the population used health services.
-
Income: The annual family income was classified with reference to the poverty line adopted for Ethiopian situation that is approximately 3 birr per person per day.
Below poverty line = annual per capita income less than 1,095 birr.
Above poverty line =annual per capita income greater than 1,095 birr (16).
Results
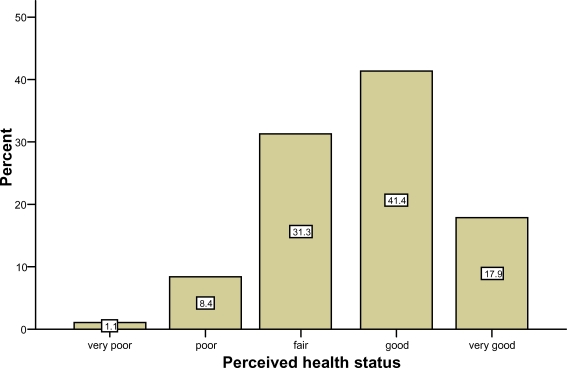
Out of the predetermined sample size of 845 households, a total of 836 responded with a response rate of 98.9%. Out of this 452 are males and 384 are females. Sixty-seven respondents (8.0%) were under fives while only 23 (2.8%) were above the age of 65. About half of the study participants were found to be illiterate. Out of the respondents greater than 18 years of age, 434 (76.8%) were married while 97 (17.2%) were single. When economical status was self-assessed by participants of the study, only 41 (4.9%) perceived their economical status to be very poor. The average family size was 5.22 (not in the tables). Perceived health status was rated to be good and very good in 345 (41.4%) and 149 (17.9%), respectively (Figure 1).
Fig 1.
Perceived health status of participants in Jimma zone, Southwest Ethiopia, February 2007
Concerning accessibility to health services, 286 (34.2%) participants claimed that it will take them less than an hour to travel to the nearest health center or hospital on foot. Only 251 (30.0%) of the participants perceived that distance to the nearby health center or hospital was near. However, in 635 (76.7%) of the cases actual distance to the nearby institutions was found to be 10 kilometers or less (Table 1).
Table 1.
Health services access in Jimma zone, Southwest Ethiopia, February 2007.
| Health services access measures | Number | Percentage | |
| Travel time to the nearest Health Center or Hospital on foot |
Less than half an hour | 34 | 4.1 |
| Half to one hour | 252 | 30.1 | |
| One to two hours | 413 | 49.4 | |
| 2 hours to three hours | 123 | 14.7 | |
| More than three hours | 13 | 1.6 | |
| Total | 835 | 100.0 | |
| Distance to the nearby Health center/Hospital (in kilometers) |
Less than or equal to 10 | 635 | 76.7 |
| Greater than 10 | 193 | 23.3 | |
| Total | 828 | 100.0 | |
| Perceived distance to nearby Health Center or Hospital |
Very near | 7 | 0.8 |
| Near | 244 | 29.2 | |
| Medium | 294 | 35.2 | |
| far | 278 | 33.3 | |
| Very far | 13 | 1.6 | |
| Total | 836 | 100.0 |
Regarding the utilization of health services, 398 (48.7%) of the respondents had visited any type of health care facility including the traditional medicine in the previous 12 months. The government and the private health services utilization rates were 35.5% and 18.5% respectively (Table 2).
Table 2.
Health services utilization in Jimma zone, Southwest Ethiopia, February 2007
| Health services factors | Number | Percentage | |
| Visited any health care facility | Yes | 398 | 48.7 |
| No | 419 | 51.3 | |
| Total | 817 | 100.0 | |
| Visited a governmental health facility |
Yes | 297 | 35.5 |
| No | 539 | 64.5 | |
| Total | 836 | 100.0 | |
| Visited a private health facility | Yes | 155 | 18.5 |
| No | 681 | 81.5 | |
| Total | 836 | 100.0 | |
| Visited a traditional healer | Yes | 3 | 0.7 |
| No | 416 | 99.3 | |
| Total | 419 | 100.0 | |
| Visited a drug vendor | Yes | 10 | 2.4 |
| No | 409 | 97.6 | |
| Total | 419 | 100.0 |
Out of the respondents who had been ill in the previous 12 months, only 245 (53.7%) visited to a modern health institution in the last episode of illness. The most common reasons cited for not visiting public and private health institution during the illness were mild illness, shortage of money and visit to a drug vendor in 102 (47.0%), 59 (27.2%) and 47 (21.7%) of the cases respectively (Table 3).
Table 3.
Reasons for not visiting a health institution during the last illness episode in Jimma zone, South west Ethiopia, February 2007.
| Reasons for not visiting health institutions | Number | Percentage | |
| The illness was not severe | Yes | 102 | 47.0 |
| No | 115 | 53.0 | |
| Total | 217 | 100.0 | |
| Shortage of money | Yes | 59 | 27.2 |
| No | 158 | 72.8 | |
| Total | 217 | 100.0 | |
| Bought medicine from a shop | Yes | 47 | 21.7 |
| No | 170 | 78.3 | |
| Total | 217 | 100.0 | |
| Long Service time | Yes | 37 | 17.1 |
| No | 180 | 82.9 | |
| Total | 217 | 100.0 | |
| Providers are not welcoming | Yes | 24 | 11.1 |
| No | 193 | 88.9 | |
| Total | 217 | 100.0 | |
| Visited a traditional healer | Yes | 8 | 3.6 |
| No | 209 | 96.4 | |
| Total | 217 | 100.0 | |
| Lack of laboratory facilities | Yes | 4 | 1.8 |
| No | 213 | 98.2 | |
| Total | 217 | 100.0 | |
Utilization of government health services was found to be associated with age, sex, education, occupation and marital status. The under-fives were 3.5 times highly likely to use the services as compared to those above the age of 65. Males were 0.46 times likely to use the services than females. Respondents with primary and below level of education were 2.0 times more likely to use government health institutions. With regard to occupation, housewives were 2.9 times more likely to visit the health institutions than farmers. Married respondents were 2.2 times more likely to utilize the health services than unmarried ones (Table 4).
Table 4.
Socio-demographic factors associated with utilization of health services in Jimma Zone, South west Ethiopia, February 2007
| Associated factors | Utilization | Odds ratio (Crude) |
Odds ratio (adjusted) |
|||
| Yes No. (%) |
No No. (%) |
Total No. (%) |
||||
| Age | (in <5 years) |
37(55.2) | 30(44.8) | 67(100.0) | 3.494 (1.225, 9.965) |
|
| 5–14 | 31(20.5) | 120(79.5) | 151(100.0) | 0.732 (0.266, 2.012) |
||
| 15–24 | 51(27.4) | 135(72.6) | 186(100.0) | 1.070 (0.400, 2.866) |
||
| 25–44 | 132(44.7) | 163(55.3) | 295(100.0) | 2.294 (0.880, 5.984) |
||
| 45–65 | 40(35.1) | 74(64.9) | 114(100.0) | 1.532 (0.559, 4.193) |
||
| >65 | 6(26.1) | 17(73.9) | 23(100.0) | 1 | ||
| Sex | Male | 125(27.5) | 329(72.5) | 454(100.0) | 0.464 (0.348, 0.619) |
0.227 (0.105, 0.490) |
| Female | 172(45.0) | 210(55.0) | 382(100.0) | 1 | ||
| Educational status |
<=Primary | 243(36.7) | 419(63.3) | 662(100.0) | 2.017 (1.236, 3.292) |
|
| > Primary | 23(22.3) | 80(77.7) | 103(100.0) | 1 | ||
| Occupation | Farmer | 81(30.3) | 186(69.7) | 267(100.0) | 1 | |
| Student | 53(23.5) | 173(76.5) | 226(100.0) | 0.703 (0.470, 1.053) |
||
| Housewife | 114(55.9) | 90(44.1) | 204(100.0) | 2.909 (1.989, 4.254) |
||
| Others | 7(17.5) | 33(82.5) | 40(100.0) | 0.487 (0.207, 1.147) |
||
| Marital status |
Married | 187(43.1) | 247(56.9) | 434(100.0) | 2.160 (1.399, 3.335) |
8.055 (2.387, 27.18) |
| Unmarried | 34(26.0) | 97(74.0) | 131(100.0) | 1 | ||
| Household income (annual) |
< 1095 | 11(13.6) | 70(86.4) | 81(100.0) | 0.257 (0.134, 0.493) |
0.700 (0.020, 0.251) |
| > 1095 | 275(38.0) | 449(62.0) | 724(100.0) | 1 | ||
| Social support |
Extensive | 168(31.9) | 358(68.1) | 526(100.0) | 0.638 (0.476, 0.855) |
|
| Minimal | 128(42.4) | 174(57.6) | 302(100.0) | 1 | ||
| Socioeconomic status |
Low | 133(35.5) | 242(64.5) | 375(100.0) | 1.147 (0.785, 1.678) |
2.625 (1.018, 6.768) |
| Medium | 80(47.1) | 90(52.9) | 170(100.0) | 1.856 (1.200, 2.871) |
3.469 (1.171, 10.28) |
|
| High | 57(32.4) | 119(67.6) | 176(100.0) | 1 | ||
Annual household income was found to be associated with utilization, where the low-income group (annual income of < 1095) was 0.26 times likely to use the health services. Respondents from households with an extensive social support were 0.64 times likely to utilize the services when compared to those with minimal social support. Furthermore, it was found out that medium socioeconomic status was associated with a 1.9 times higher chance of utilization of the government health services as compared to the high socioeconomic group (Table 4).
Perceived health status was also found to be associated with utilization of the health services. When compared to those with a very good perceived health status, those with a poor and very poor health status were 11.7 and 13.1 times more likely to visit the facilities, respectively. Respondents who claimed to have disabling health problem were 3.8 times more likely to use the services. Similarly, those who had a history of illness in the previous 12 months were 10.5 times more likely to visit the health institutions (Table 5). Distance to the nearest health center or hospital was also associated with utilization where those who were residing in 10 kilometers or less to the nearby institution were 1.5 times more likely to use the health services. Similarly, those with a perceived distance to the nearby institutions of ‘near’ and ‘medium’ were 1.6 and 1.2 times more likely to visit the institutions as compared to those who perceived it as ‘far’. Moreover, perceived transport and treatment cost were associated with utilization on the bivariate analysis. Accordingly, those who perceived the transport cost to be ‘cheap’ were 2.5 times more likely to utilize the services than those who perceived it as ‘expensive’. Similarly, those respondents with a perceived treatment cost of ‘expensive’ were 0.18 times likely to use the services as compared to those who said the cost was ‘cheap’ (Table 6).
Table 5.
Health status factors associated with utilization of health services in Jimma Zone, South west Ethiopia, February 2007
| Associated factors | Utilization | Odds ratio (crude) |
Odds ratio (adjusted) |
|||
| Yes No. (%) |
No No. (%) |
Total No. (%) |
||||
| Perceived health status |
Very poor | 5(55.6) | 4(44.4) | 9(100.0) | 13.077 (3.121, 54.79) |
|
| Poor | 37(52.9) | 33(47.1) | 70(100.0) | 11.730 (5.61, 24.524) |
||
| Average | 122(46.7) | 139(53.3) | 261(100.0) | 9.182 (4.946, 17.05) |
||
| Good | 120(34.8) | 225(65.2) | 345(100.0) | 5.579 (3.030, 10.28) |
||
| Very good | 13(8.7) | 136(91.3) | 149(100.0) | 1 | ||
| Chronic disease (diagnosed) |
Yes | 51(53.1) | 45(46.9) | 96(100.0) | 2.308 (1.503, 3.548) |
|
| No | 241(32.9) | 491(67.1) | 732(100.0) | 1 | ||
| Disabling health problem |
Yes | 134(58.5) | 95(41.5) | 229(100.0) | 3.841 (2.790, 5.288) |
3.257 (1.267, 8.375) |
| No | 159(26.9) | 433(73.1) | 592(100.0) | 1 | ||
| Illness episode in the previous 12 months |
Yes | 250(58.3) | 179(41.7) | 429(100.0) | 10.505 (7.311, 15.10) |
28.245 (9.495, 84.02) |
| No | 46(11.7) | 346(88.3) | 392(100.0) | 1 | ||
Table 6.
Health services access indicators associated with utilization of health services in Jimma zone, South west Ethiopia, February 2007
| Associated factors | Utilization | Odds ratio (Crude) |
Odds ratio (Adjusted) |
|||
| Yes No. (%) |
No No. (%) |
Total No. (%) |
||||
| Distance to health center or hospital (in kilometers) |
<= 10 | 238(37.5) | 397(62.5) | 635(100.0) | 1.467 (1.034, 2.081) |
2.908 (1.121, 7.540) |
| >10 | 56(29.0) | 137(71.0) | 193(100.0) | 1 | ||
| Perceived distance to the nearby center |
Near | 104(41.4) | 147(58.6) | 251(100.0) | 1.580 (1.110, 2.250) |
|
| Medium | 103(35.0) | 191(65.0) | 294(100.0) | 1.204 (0.853, 1.701) |
||
| Far | 90(30.9) | 201(69.1) | 291(100.0) | 1 | ||
| Perceived transport cost |
Expensive | 229(37.5) | 381(62.5) | 610(100.0) | 1 | |
| Medium | 31(31.0) | 69(69.0) | 100(100.0) | 0.747 (0.475, 1.177) |
0.423 (0.151, 1.190) |
|
| Cheap | 12(60.0) | 8(40.0) | 20(100.0) | 2.496 (1.005, 6.197) |
3.587 (0.301, 42.761) |
|
| No transport |
18(19.6) | 74(80.4) | 92(100.0) | 0.405 (0.236, 0.695) |
0.052 (0.009, 0.298) |
|
| Perceived treatment cost |
Expensive | 31(26.5) | 86(73.5) | 117(100.0) | 0.182 (0.105, 0.317) |
0.100 (0.002, 0.045) |
| Medium | 178(46.4) | 206(53.6) | 384(100.0) | 0.437 (0.287, 0.667) |
0.145 (0.043, 0.492) |
|
| Cheap | 83(66.4) | 42(33.6) | 125(100.0) | 1 | ||
On binary logistic regression, age, sex, educational status, occupation, marital status, income, socioeconomic status, social support, perceived health status, presence of chronic disease, presence of chronic health problem, presence of a disabling health problem, any history of illness in the previous 12 months, perceived distance to nearby hospital or health center, perceived transport cost, perceived treatment cost and distance to the health institutions were entered into the model. Then after controlling for confounders; sex, marital status, presence of disabling health problem, presence of an illness episode, perceived transport and treatment cost, distance to the nearest health center or hospital, household income and socioeconomic status were found to have a significant association with utilization.
Males were found to utilize the government health services 0.23 times likely than females while married respondents were 8.1 times more likely to visit the health facilities as compared to unmarried ones. It was also shown that participants below the poverty line were 0.7 times likely to use the government health services as compared to those above the poverty line. Moreover, it was found out that the low and medium socioeconomic groups were 2.6 and 3.5 times more likely to visit the health institutions than the high socioeconomic group (Table 4).
Presence of a disabling health problem increased the likelihood of utilization of health services 3.3 times more. Similarly, respondents who had an illness episode were 28 times more likely to utilize the services (Table 5).
Those respondents residing 10 kilometers or less from the nearby health center and hospital were 2.9 times more likely to utilize the health care delivered in the institutions. Regarding perceived transport cost, it was seen that 3.6 times difference in the likely hood of utilization as we compare the cheap and the expensive group. While, those who did not have transportation service to the health facilities were 0.05 times likely to utilize the services. Similarly, those who perceived the treatment cost to be expensive and medium had a 0.1 and 0.15 times chance of utilization (Table 6).
Discussion
The government and the private health services utilization rates were 35.5% and 18.5% respectively. Presence of a disabling health problem and an illness episode were associated with increased utilization of health services. Besides, sex, marital status, household income and socioeconomic status were found to be associated with use of the health care. Distance to the nearest health center or hospital, perceived transport cost and perceived treatment cost were shown to be predictors of utilization of health services.
Like any other study, this one also has its own limitations. First, as the questions were administered by an interviewer there is a possibility of social desirability bias. For example, the modern health service utilization rate might be overestimated, as many people might be afraid to admit that they visited a traditional practitioner. To minimize this bias, interviewers were trained not to favor a certain practice or experience.
The second limitation worth mentioning is recall bias since evaluation of self-reported behavior patterns was retrospective. We used 12 months period of recall that has been used in other similar studies. When we measured satisfaction of the respondents on a previous visit to one of the government health institutions, participants might forget some of their experiences in the health facilities. Similarly, prevalence of illness episode might be underestimated due to recall bias.
On the other hand, the instrument was prepared after thorough literature search and pre-tested before the start of the actual data collection. Then appropriate modifications were undertaken based on the experience of the pre-test. The data collectors were high school complete individuals who were trained adequately. Besides, they were being supervised daily. Furthermore, we used an adequately large sample size using a probability sampling technique that contributes for the generalizability of the findings.
In this study, the government health services utilization rate in the previous 12 months was found to be 35.5% This is lower than findings from other countries. In the countries of the former Soviet Union (1), 57 % of all respondents visited a medical professional in the year preceding the study. Thus, efforts should be strengthened to improve the level of health care use in Jimma Zone. According to Andersen, factors affecting utilization of health services include health status, predisposing factors and enabling factors (4). Severity of an illness was seen to be important in utilization of health services. The most common reason (47%) cited for not visiting a health institution during the illness was the fact that the illness was mild. This finding is consistent with other studies in Ethiopia (3).
Males were found to utilize the government health services 0.23 times likely than females. This might be explained by the fact that women are more prone to illness due to peculiar reproductive health needs. Moreover, women would be more likely to accompany their children to health institutions where they seek treatment for themselves too.
This study has revealed that the low and the medium socioeconomic groups were 2.6 and 3.5 times more likely to visit the health institutions than the high socioeconomic group. But a research performed in Brazil, has shown that the lowest un-educated socioeconomic group made 62% fewer doctor visits (7). This might be due to the fact that there is a free health service to the poor in Ethiopia and the high socioeconomic group might have a better health status.
Service related factors like perceived transport cost, distance to the nearest health center or hospital and perceived treatment cost were seen to predict use of the health services. Similarly, physical access was found to be a significant determinant in decisions about outpatient visits. Those individuals located less than or equal to 10 kilometers from the nearest health center or hospital had a 2.9 times higher chance of using the health services as compared to those residing more than 10 kilometers away. Besides, absence of transportation was associated with a 0.05 chance of service utilization as compared to those who perceived the transport cost to be expensive.
In conclusion the level of health services utilization rate was found to be unsatisfactory. Distance to the nearest health center or hospital, perceived transport cost and perceived treatment cost were shown to be predictors of utilization of health services. This clearly indicates that improving physical accessibility of health services will possibly result in a better utilization of health care.
Acknowledgements
We would like to thank Jimma University for providing the financial support to undertake the research. Our gratitude also goes to the Jimma Zone and Mana, Kersa, Dedo and Limu Kosa district administrations and health offices for their cooperation during data collection period. Last but not least, our appreciation goes to the participants of the study for their cooperation and sincere response.
References
- 1.Balabanova D, Mackee M, Pomerleau J, Rose R, Haerpfer C. Health Service Utilization in the Former Soviet Union: Evidence from Eight Countries. Health Services Research. 2004;39:6. doi: 10.1111/j.1475-6773.2004.00326.x. Part II. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ethiopian Ministry of Health, author. Health and Health Related Indicators. 2006/07. [Google Scholar]
- 3.Fantahun M, Degu G. Health Service Utilization in Amhara Region of Ethiopia. Ethiop J Health Dev. 2003;17(2):141–147. [Google Scholar]
- 4.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behaviour. 1995;36:1–10. [PubMed] [Google Scholar]
- 5.Pathak M, Ketkar Y A, Majumdar R D. Perceived morbidity, utilization of health services and factor affecting it in a rural area. Health and Population - Perspective and Issues. 1981;4(1):79–85. [PubMed] [Google Scholar]
- 6.Sauerborn R, Nougtara A, Diesfeld HJ. Low Utilization of Community Health Workers: Results from a Household Interview Survey in Burkina Faso. Social Science and Medicine. 1989;29(10):1163–1174. doi: 10.1016/0277-9536(89)90359-6. [DOI] [PubMed] [Google Scholar]
- 7.Mendoza-Sassi R, Jorge U, Sevilla J. Factors Associated with Health Services Utilization: A Population-based Study Assessing the Characteristics of people that visit Doctors in Southern Brazil. Available at. www.hsph.harvard.edu/takemi/RP18485. Referred on 17 May 2007.
- 8.Faizi AA. Planning Of Health Services in Madhubani District of Bihar: A Study of Availability, Accessibility, Utilization and Location of Future PHCs. Mumbai: International Institute for Population Sciences; 1996. [Google Scholar]
- 9.Morettin D, Kazanjian A, Savoie I. Gender and utilization of health services in British Columbia: A pilot study using linked data. 2000. Poster presentation at the Building Bridges Conference Victoria, British Columbia. [Google Scholar]
- 10.Nigussie M, Haile Mariam D, Mitike G. Assessment of safe delivery service utilization among women of childbearing age in north Gondar Zone, North West Ethiopia. Ethiop J Health Dev. 2004;18(3):145–152. [Google Scholar]
- 11.Dunlop S, Coyte PC, Mclsaac W. Socioeconomic status and the utilization of physicians' services: results from the Canadian National Population Health Survey. Social Science and Medicine. 2000;51(1):123–133. doi: 10.1016/s0277-9536(99)00424-4. [DOI] [PubMed] [Google Scholar]
- 12.Abu-Zeid H, William M. Health Services Utilization and Cost in Ismailia, Egypt. Social Science and Medicine. 1985;29(4):451–461. doi: 10.1016/0277-9536(85)90225-4. [DOI] [PubMed] [Google Scholar]
- 13.Abula T, Worku A. Self medication in three towns of North West Ethiopia. Ethiop J Health Dev. 2001;1(15):25–30. [Google Scholar]
- 14.Magnus L. Understanding spatial variation in the utilization of health services: does quality matter? Vol. 212. The Centre for the Study of African Economies; 2004. p. 2. Working Paper Series. [Google Scholar]
- 15.Mahfouz A, Al-Sharif A, El-Gamal M, Kisha A. Primary health care services utilization and satisfaction among the elderly in Asir region, Saudi Arabia. Eastern Meditranean Journal. 2004;10(3):365–371. [PubMed] [Google Scholar]
- 16.Ministry of Finance and Economic Development of Federal and Democratic Republic of Ethiopia and United Nations. 2004. [Google Scholar]