Abstract
The metabolic syndrome was designed to identify individuals at high risk for the development of type 2 diabetes and cardiovascular disease. Compared with whites, blacks have higher rates of diabetes and cardiovascular disease. Paradoxically, blacks have a lower prevalence of the metabolic syndrome. According to the criteria set by National Cholesterol Education Treatment Program–Adult Treatment Panel III, to diagnose the metabolic syndrome, 3 of 5 characteristics must be present. These characteristics are low high-density lipoprotein levels, increased triglyceride levels, central obesity, hypertension, and fasting hyperglycemia. Examining each of these factors individually, blacks are more likely than whites to have obesity, hypertension, and diabetes. In contrast, blacks are less likely than whites to have either elevated triglyceride or low high-density lipoprotein levels. Ethnic differences in lipid levels may largely explain why blacks have a lower than expected prevalence of the metabolic syndrome. In this review we will describe in children and adults ethnic differences in the epidemiologic study of conditions associated with the metabolic syndrome, as well as focus on each of the parameters of the metabolic syndrome. Overall, we conclude that an ethnic-specific formulation of the lipid criteria in the metabolic syndrome may lead to better identification of blacks at high risk for development of diabetes and cardiovascular disease.
The metabolic syndrome was designed to predict the development of cardiovascular disease and type 2 diabetes.1 In the presence of the metabolic syndrome there is a 2-fold increased risk of cardiovascular disease and a 5-fold increased risk of diabetes.2 Using the criteria set by National Cholesterol Education Treatment Program–Adult Treatment Panel III, the diagnosis of the metabolic syndrome requires that 3 of 5 characteristics be present.3 These characteristics are low high-density lipoprotein (HDL) levels, increased triglyceride levels, central obesity, hypertension, and fasting hyperglycemia. Insulin resistance not only promotes each of the features of the metabolic syndrome, it is considered to be a major etiologic factor in the development of the metabolic syndrome.1
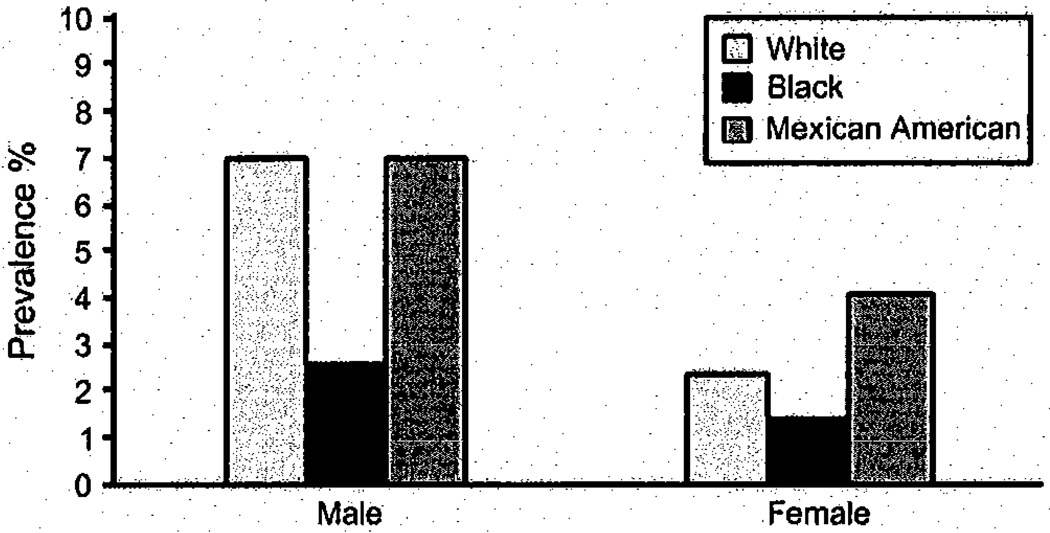
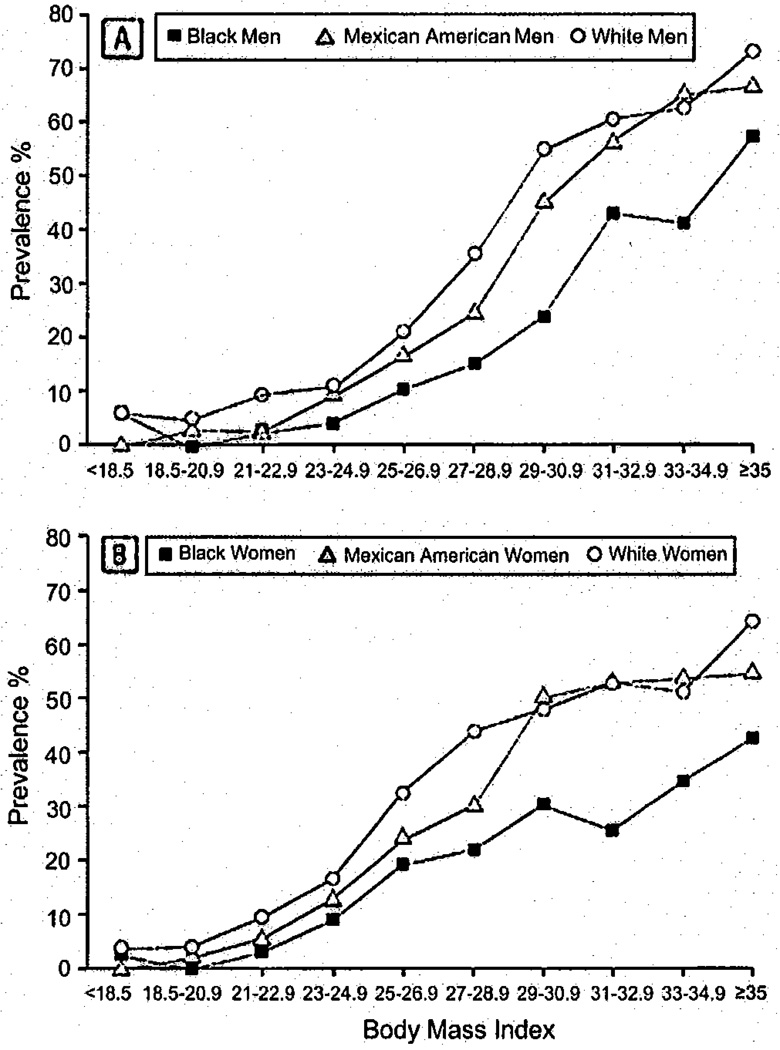
Obesity, insulin resistance, diabetes, and hypertension are more common in blacks than whites.4–8 However, the dyslipidemia associated with the metabolic syndrome, specifically hypertriglyceridemia and low HDL levels, are observed less frequently in blacks than in whites.9,10 It appears that the dyslipidemia associated with the metabolic syndrome, also referred to as the dyslipidemia of insulin resistance, has a disproportionate effect on metabolic syndrome diagnosis. We make this claim because even though conditions the metabolic syndrome are supposed to predict are more common in blacks than in whites, the prevalence of the metabolic syndrome is lower in blacks than in whites (Figures 1 and 2).11,12 Our concept of the “underdiagnosis” of the metabolic syndrome in blacks is based on this lower-than-expected prevalence of the metabolic syndrome. Because the metabolic syndrome occurs in both children and adults, in this review we will describe ethnic differences throughout the life span in the epidemiologic study of conditions and parameters associated with the metabolic syndrome. Because obesity often precedes the development of diabetes and cardiovascular disease, we will discuss obesity first.
Figure 1.
Prevalence of the metabolic syndrome in adolescents: age 12 to 19 years NHANES III. Reproduced with permission from Cook S, et al. Arch Pediatr 2003;157:821–827. (Permission obtained.)
Figure 2.
Prevalence of the metabolic syndrome in adults: NHANES III. Reproduced with permission from Park, Y-W, Arch Intern Med 2003; 163:427–436.
Obesity
In children, obesity is defined as a body mass index (BMI) above the 95th percentile determined from age- and sex-specific growth charts.13 For adults, obesity is defined as a BMI ≥ 30 kg/m2.14
Ethnic differences in BMI begin early in life, persist throughout the life span, and are more pronounced in girls than in boys. Data from the National Health and Nutrition Examination Survey (NHANES) have demonstrated that in each age category (2 to 5 years, 6 to 11 years, and 12 to 19 years), mean BMI is higher in black girls than in white girls.13 Similarly, the National Health and Growth Study (NHGS), a 10-year longitudinal study that enrolled black and white girls at age 9, found that black girls at age 9 had a median BMI that was 0.4 kg/m2 units higher than white girls.15 By age 19, this difference in BMI had increased to 2.3 kg/m2 units.15 Because BMI measures total body size and does not account for body fat content, NHGS investigators used the sum of skinfold (SSF) thicknesses as a measure of body fat content. The skinfolds measured were triceps, subscapular, and suprailiac. The investigators found that SSF thicknesses were greater in black girls at baseline and that this ethnic difference widened between ages 9 and 19 years. Recently it was reported in the United States that the prevalence of childhood obesity rose between 1980 and 1999 and then plateaued between 1999 and 2006.13 Even with this plateau in the prevalence of pediatric obesity, the tendency for black girls to have a higher BMI than white girls did not change.13
In the development of adult obesity, the NHGS investigators found that overweight girls were 10 to 30 times more likely to become obese adults.16 Therefore it is not surprising that in adulthood, black women have a higher prevalence of obesity than white women. By age 20, 47% of black women are obese, compared with 25% of white women.8 By age 40, the prevalence of obesity is 51% in black women and 35% in white women.8
For boys and men, the ethnic difference in BMI is much less pronounced.8,13 Nevertheless, throughout the life span there is a tendency for black males to have a higher BMI than white males.8,13
Central Obesity
In adults the measure of adiposity used by the metabolic syndrome is central obesity rather than BMI. Evidence is accumulating that central obesity, measured by waist circumference (WC), is a better predictor of cardiovascular outcomes than BMI.17–20 However, WC and BMI are highly Correlated.21,22 Therefore it is not surprising that because black women are more obese than white women, black women have a higher prevalence of central obesity (62% in black women vs 44% in white women).9 In contrast, the prevalence of central obesity is similar in black and white men.9
Defining central obesity in children is controversial. This is because there is no consensus on the best method to define the WC threshold of risk in children. Depending on how the WC of risk is determined, some investigators have found major ethnic differences in adolescents in the WC of risk, but others have not.23,24 To avoid this controversy in the diagnosis of metabolic syndrome in children, BMI is often substituted for WC.25
Insulin Resistance
Insulin resistance and obesity are linked. Insulin resistance promotes both adipocyte hypertrophy and hyperplasia, as well as intracellular abnormalities leading to endoplasmic reticulum dysfunction and mitochondrial stress.26 In an insulin-resistant milieu, adipocytes produce and release adipokines, free fatty acids, and inflammatory mediators. These in turn promote fatty infiltration of muscle and liver and more insulin resistance.
Insulin resistance causes heart disease in myriad ways. We specifically focus on the 3 mechanisms that directly relate to the metabolic syndrome. First, insulin resistance promotes the development of a highly atherogenic lipid profile including increased levels of triglycerides, small dense low-density lipoprotein (LDL), glycated LDL, and highly oxidized LDL, as well as low levels of HDL. Second, insulin resistance facilitates the development of hypertension by stimulating renal tubular sodium reabsorption, augmenting sympathetic nervous system reactivity and activating the renin-angiotensin system.27 Third, insulin resistance leads to hyperglycemia by impairing peripheral glucose uptake, promoting hepatic glucose output and facilitating beta-cell failure.28 The relationship between insulin resistance and progressive beta-cell failure has been characterized as a “vicious cycle.”28 As beta-cells fail there is a decline in insulin secretion. Decreased insulin secretion directly leads to an increase in both hyperlipidemia and hyperglycemia. As hyperlipidemia and hyperglycemia worsen, beta-cell cell function deteriorates further. The close relationship of insulin resistance to the metabolic syndrome is based on the observation that dyslipidemia, hypertension and hyperglycemia are not only consequences of insulin resistance; they also perpetuate each other.
There are ethnic differences in insulin resistance. In both children and adolescents, insulin resistance is greater in blacks than whites.29 This ethnic difference in insulin resistance is greater in girls than boys and occurs even before differences in obesity develop.29,30 Similarly, black adults have more insulin resistance than whites.6,10 Even when normal-weight adults are compared, insulin resistance is greater in blacks than in whites.31
Diabetes and Fasting Hyperglycemia
Compared with the vast amount of knowledge available about type 2 diabetes in adults, there is a relative paucity of data about type 2 diabetes in children.32 Nevertheless, it is clear that under the age of 10, type 2 diabetes is unusual.33 With our current epidemic of obesity in children, the prevalence of diabetes is rising in peripubertal and adolescent children. Blacks are disproportionately affected. Per 1000 youth in the age range of 10 to 19 years, the incidence of type 2 diabetes is 1.06 for whites and 3.22 for blacks.33 There is considerable concern that as type 2 diabetes occurs in youth, the medical complications of diabetes, particularly cardiovascular disease, nephropathy, and retinopathy will occur in young adulthood.
In terms of glucose management, glycosylated hemoglobin, a measure of chronic glucose control, is higher in black children than in white children.34 Yet, fasting glucose, a metabolic syndrome criterion, has not been found to be different in black and white youth.25,35 In general fasting hyperglycemia is considered a marker of hepatic insulin resistance.36 Diabetes occurs because of a combination of beta-cell failure and insulin resistance. Insulin resistance, in turn, is a combination of hepatic and peripheral insulin resistance. The relative lack of fasting hyperglycemia in blacks suggests that, in black adolescents, beta-cell failure and peripheral insulin resistance may be more important than hepatic insulin resistance.37,38
In adults, ample data are available on the prevalence of type 2 diabetes. From NHANES 1999 to 2002, it is known that compared with whites, black adults have twice the prevalence of type 2 diabetes.4 As seen in children, impaired fasting glucose was less common in black adults than in white adults.4 In contrast, Ford et al,9 in an analyses of NHANES 1988 to 1994, reported that fasting hyperglycemia occurred twice as often in black adults than in white adults. This contradiction is explained by a difference in study design. Ford et al9 included diabetics in the definition of impaired fasting glucose, and Cowie et al4 excluded them. Therefore, although diabetes is more common in blacks than in whites, fasting hyperglycemia, a metabolic syndrome criterion, may be similar in blacks and whites.
Hypertension and Cardiovascular Disease
In adolescence, blood pressure is higher in black adolescent girls than in white adolescent girls.34 In male adolescents the ethnic difference in blood pressure is not significant.34 However, in male and female adults there are major ethnic differences in the prevalence of hypertension. Fifty percent of black men have hypertension compared with 37% of white men.9 For women, 43% of blacks have hypertension compared with 28% of whites.9 Overall hypertension in blacks occurs at a younger age than in whites and is associated with greater complications such as heart and kidney failure, myocardial infarction, and stroke.9,39,40 Additionally, evidence is emerging that suggests hypertension is a risk factor for diabetes.41 Therefore in blacks, high rates of diabetes may be linked to their even higher rate of hypertension.
The Dyslipidemia of Insulin Resistance
In its simplest form the dyslipidemia of insulin resistance consists of both high trigiyceride levels and low HDL levels. High trigiyceride and low HDL levels are both metabolic syndrome parameters.3 HDL participates in reverse cholesterol transport and is both an antiinflammatory and antioxidant agent.42 Consequently, low HDL levels represent the absence of this cardioprotection and constitute a cardiovascular risk.42
High trigiyceride levels are highly correlated with cardiovascular disease and are characteristic of diabetes and insulin resistance.43 Insulin resistance promotes free fatty acid release from visceral fat into the portal circulation. In the presence of insulin resistance when these free fatty acids reach the liver, hepatic triglyceride production increases.44 Subsequently there is increased hepatic secretion of the triglyceride-rich particles called very low-density lipoprotein.
High triglyceride and low HDL levels occur together because they are reciprocally cleared from the circulation.45 The enzyme that clears TG is lipoprotein lipase (LPL). The enzyme that clears HDL is hepatic lipase (HL). In the presence of insulin resistance lipoprotein lipase (LPL) activity decreases and HL activities increases leading to a decreased LPL/HL ratio.46 The consequence of this decreased LPL/HL ratio is indeed the dyslipidemia of insulin resistance, high triglyceride levels, and decreased HDL levels.
Compared with white adults and children, black adults and children have a better lipid profile specifically lower triglyceride levels and higher HDL levels.9–11,25,29 If the effect of insulin resistance on the lipid profile were the same in whites and blacks, then TG would be higher in blacks than in whites and HDL lower. Yet it is reversed. Why insulin resistance does not appear to adversely affect the lipid profile in blacks is under intense investigation. Differences in diet do not account for the lower TG and higher HDL observed in blacks than whites.47 However, it is known that LPL levels are higher and HL levels are lower in blacks than whites.48,49 Furthermore, in blacks insulin resistance does not appear to impair LPL activity, so that even in the presence of insulin resistance blacks can clear triglyceride from the circulation.50
Even though the cause of lower triglyceride and higher HDL levels in blacks is unknown, the relative absence of the dyslipidemia of insulin resistance in blacks may explain their lower-than-expected prevalence of the metabolic syndrome. It is also possible that the adult thresholds used to define hypertriglyceridemia (triglyceride level ≥ 150 mg/dL) and low HDL (<40 mg/dL in men, <50 mg/dL in women) are not set at the appropriate level to identify high risk for diabetes and cardiovascular disease in blacks.
Discussion
Cross-sectional studies have clearly revealed in both children and adults, that the prevalence of the metabolic syndrome is lower in blacks than whites. Yet the prevalence of diabetes, obesity, hypertension, cardiovascular disease, and cardiovascular risk factors are higher in blacks than whites. Therefore the lower prevalence of the metabolic syndrome in blacks is contradictory to our concept of the metabolic syndrome as an early warning system for these conditions. The leading culprit for this unexpected finding is the relative absence of the dyslipidemia of insulin resistance (ie, high triglyceride level and low HDL) in blacks. It may be that the triglyceride and HDL thresholds currently defined by the metabolic syndrome guidelines as abnormal, (triglyceride ≥ 150 mg/dL and HDL <40 mg/dL in men, <50 mg/dL in women) are not appropriate for blacks. Ethnic-specific guidelines for lipids may be necessary. Alternatively, blacks with the metabolic syndrome may transition so quickly from having the metabolic syndrome into cardiovascular disease and diabetes that a cross-sectional prevalence study does not capture the true rate of the metabolic syndrome in blacks. Another possibility is that in blacks the metabolic syndrome may not precede the development of diabetes and cardiovascular disease. To determine the significance of the metabolic syndrome in blacks and address the issue of underdiagnosis, carefully designed prospective studies that start in childhood and last for decades are needed.
Acknowledgments
This work was supported by the intramural research program of NIDDK. The contents of this publication do not represent to views or policies of the National Institutes of Health.
Glossary
- BMI
Body mass index
- HDL
High-density lipoprotein
- HL
Hepatic lipase
- LDL
Low-density lipoprotein
- LPL
Lipoprotein lipase
- NHANES
National Health and Nutrition Examination Survey
- NHGS
National Health and Growth Study
- SSF
Sum of skinfold
- WC
Waist circumference
Footnotes
Author Disclosures
Anne E. Sumner, MD, has no financial arrangement or affiliation with a corporate organization or a manufacturer of a product discussed in this supplement.
References
- 1.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 2.Grundy SM. Metabolic syndrome pandemic. Arterioscler Thromb Vasc Biol. 2008;28:629–636. doi: 10.1161/ATVBAHA.107.151092. [DOI] [PubMed] [Google Scholar]
- 3.Expert Panel. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 4.Cowie CC, Rust KF, Byrd-Holt D, Eberhardt MS, Flegal KM, Engelgau MM, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population, National Health and Nutrition Examination Survey 1999–2002. Diabetes Care. 2006;29:1263–1268. doi: 10.2337/dc06-0062. [DOI] [PubMed] [Google Scholar]
- 5.Ferdinand KC. Coronary artery disease in minority racial and ethnic groups in the United States. Am J Cardiol. 2006;97S:12A–19A. doi: 10.1016/j.amjcard.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 6.Haffner SM, Ralph D’Agostino J, Saad MF, Rewers M, Mykkanen L, Selby J, et al. Increased insulin resistance and insulin secretion in nondiabetic African-Americans and Hispanics compared with non-Hispanic whites, The Insulin Resistance Atherosclerosis Study. Diabetes. 1996;45:742–748. doi: 10.2337/diab.45.6.742. [DOI] [PubMed] [Google Scholar]
- 7.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment and control of hypertension in the United States, 1988–2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 8.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents and adults 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 9.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults, findings from the Third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 10.Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis. 2008;196:696–703. doi: 10.1016/j.atherosclerosis.2006.12.018. [DOI] [PubMed] [Google Scholar]
- 11.Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents, findings from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med. 2003;157:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 12.Park Y-W, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome, prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2003;163:427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 14.NHLBI Expert Panel on the Identification E, and Treatment of Overweight and Obesity in Adults: clinical guidelines on the identification, evaluation and treatment of overweight and obesity in adults. Obes Res. 1998;6 Suppl 2:51S–209S. [PubMed] [Google Scholar]
- 15.Kimm SYS, Barton BA, Obarzanek E, McMahon RP, Sabry ZI, Waclawiw MA, et al. Racial divergence in adiposity during adolescence: The NHLBI Growth and Health Study Pediatrics. 2001;107:e34. doi: 10.1542/peds.107.3.e34. [DOI] [PubMed] [Google Scholar]
- 16.Thompson DR, Obarzanek E, Franko DL, Barton BA, Morrison JA, Biro FM, et al. Childhood overweight and cardiovascular disease risk factors: The National Heart, Lung and Blood Institute Growth and Health Study. J Pediatr. 2007;150:18–25. doi: 10.1016/j.jpeds.2006.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu FB. Obesity and mortality, watch your waist, not just your weight. Arch Intern Med. 2007;167:875–876. doi: 10.1001/archinte.167.9.875. [DOI] [PubMed] [Google Scholar]
- 18.Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al. Waist circumference and cardiometabolic risk: a consensus statement from shaping America’s health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society, the American Society for Nutrition; and the American Diabetes Association. Obesity. 2007;15:1061–1967. doi: 10.1038/oby.2007.632. [DOI] [PubMed] [Google Scholar]
- 19.Menke A, Muntner P, Wildman RP, Reynolds K, He J. Measures of adiposity and cardiovascular disease risk factors. Obesity. 2007;15:785–795. doi: 10.1038/oby.2007.593. [DOI] [PubMed] [Google Scholar]
- 20.Xianglan Z, Xiao-Ou S, Yang G, Li H, Cai H, Gao Y-T, et al. Abdominal adiposity and mortality in Chinese women. Arch Intern Med. 2007;167:886–892. doi: 10.1001/archinte.167.9.886. [DOI] [PubMed] [Google Scholar]
- 21.Lean MEJ, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–161. doi: 10.1136/bmj.311.6998.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sumner AE, Sen S, Ricks M, Frempong BA, Sebring NG, Kushner H. Determining the waist circumference in African Americans which best predicts insulin resistance. Obesity. 2008;16:841–846. doi: 10.1038/oby.2008.11. [DOI] [PubMed] [Google Scholar]
- 23.Fernandez JR, Redden DT, Pietrobelli A, Allison DB. Waist circumference percentiles in nationally representative samples of African-American, European-American and Mexican-American children and adolescents. J Pediatrics. 2004;145:439–444. doi: 10.1016/j.jpeds.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 24.Katzmarzyk PT, Srinivasan SR, Chen W, Malina RM, Bouchard C, Berenson GS. Body mass index, waist circumference and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescents. Pediatrics. 2004;114:e198–e205. doi: 10.1542/peds.114.2.e198. [DOI] [PubMed] [Google Scholar]
- 25.Weiss R, Dziura J, Burget TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004;350:2362–2374. doi: 10.1056/NEJMoa031049. [DOI] [PubMed] [Google Scholar]
- 26.deFerranti S, Mozaffarian D. The perfect storm: obesity, adipocyte dysfunction and metabolic consequences. Clin Chem. 2008;54:945–955. doi: 10.1373/clinchem.2007.100156. [DOI] [PubMed] [Google Scholar]
- 27.Yanai H, Tomono Y, Ito K, Furutani N, Yoshida H, Tada N. The underlying mechanisms for development of hypertension in the metabolic syndrome. Nutr J. 2008;7:10. doi: 10.1186/1475-2891-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bonora E. Protection of pancreatic beta-cells: is it feasible? Nutr Metab Cardiovasc Dis. 2008;18:74–83. doi: 10.1016/j.numecd.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 29.Chen W, Bao W, Begum S, Elkasabany A, Srinivasan SR, Berenson GS. Age-related patterns of the clustering of cardiovascular risk variables of syndrome X from childhood to young adulthood in a population made up of black and white subjects, The Bogalusa Heart Study. Diabetes. 2000;49:1042–1048. doi: 10.2337/diabetes.49.6.1042. [DOI] [PubMed] [Google Scholar]
- 30.Klein DJ, Schreiber GB, Friedman LA, Cohen RM, Harlan WR, Harlan LC, et al. Obesity and the development of insulin resistance and impaired fasting glucose in black and white adolescent girls: a longitudinal study. Diabetes Care. 2004;27:378–383. doi: 10.2337/diacare.27.2.378. [DOI] [PubMed] [Google Scholar]
- 31.Norman JE, Bild D, Lewis CE, Liu K, Smith West D. The impact of weight change on cardiovascular disease risk factors in young black and white adults: the CARDIA Study. Int J Obes Relat Metab Disord. 2003;27:369–376. doi: 10.1038/sj.ijo.0802243. [DOI] [PubMed] [Google Scholar]
- 32.Pinhas-Hamiel O, Zeitler P. Acute and chronic complications of type 2 diabetes mellitus in children and adolescents. Lancet. 2007;369:1823–1831. doi: 10.1016/S0140-6736(07)60821-6. [DOI] [PubMed] [Google Scholar]
- 33.SEARCH for Diabetes in Youth Study Group. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118:1510–1518. doi: 10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- 34.Winkleby MA, Robinson TN, Sundquist J, Kraemer HC. Ethnic variation in cardiovascular disease risk factors among children and young adults, findings from the Third NHANES, 1988–1994. JAMA. 1999;281:1006–1013. doi: 10.1001/jama.281.11.1006. [DOI] [PubMed] [Google Scholar]
- 35.Cook S, Alinger P, Li C, Ford ES. Metabolic syndrome rates in the United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J Pediatr. 2008;152:165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 36.Nathan DM, Henry RR, Davidson MB, Pratley R, DeFronzo RA, Zinman B, et al. Impaired fasting glucose and impaired glucose tolerance, implications for care. Diabetes Care. 2007;30:753–759. doi: 10.2337/dc07-9920. [DOI] [PubMed] [Google Scholar]
- 37.Bacha F, Saad R, Gungor N, Janosky J, Arslanian SA. Obesity, regional fat distribution and syndrome X in obese black versus white adolescents: race differential in diabetogenic and atherogenic risk factors. J Clin Endocrinol Metab. 2003;88:2534–2540. doi: 10.1210/jc.2002-021267. [DOI] [PubMed] [Google Scholar]
- 38.Ball GDC, Huang TT-K, Gower BA, Cruz ML, Shaibi GQ, Weigensberg MJ, et al. Longitudinal changes in insulin sensitivity, insulin secretion and beta-cell function during puberty. J Pediatr. 2006;148:16–22. doi: 10.1016/j.jpeds.2005.08.059. [DOI] [PubMed] [Google Scholar]
- 39.Albert MA, Torres J, Glynn RJ, Ridker PM. Perspective on selective issues in cardiovascular research with a focus on black Americans. Circulation. 2004;110:e7–e12. doi: 10.1161/01.CIR.0000135583.40730.21. [DOI] [PubMed] [Google Scholar]
- 40.Cooper R, Rotimi C. Hypertension in blacks. Am J Hypertens. 1997;7:804–812. doi: 10.1016/s0895-7061(97)00211-2. [DOI] [PubMed] [Google Scholar]
- 41.Gress TW, Nieto J, Shahar E, Wofford Mr, Brancati FL. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. N Engl J Med. 2000;342:905–912. doi: 10.1056/NEJM200003303421301. [DOI] [PubMed] [Google Scholar]
- 42.Mooradian AD, Haas MJ, Wehmeier KR, Wong NCW. Obesity-related changes in high-density lipoprotein metabolism. Obesity. 2008;16:1152–1160. doi: 10.1038/oby.2008.202. [DOI] [PubMed] [Google Scholar]
- 43.St. Pierre J, Lemieux I, Perron P, Brisson D, Santure M, Vohl M-C, et al. Relationship of the “hypertriglyceridemic waist” phenotype to earlier manifestations of coronary artery disease in patients with glucose intolerance and type 2 diabetes mellitus. Am J Cardiol. 2007;99:369–373. doi: 10.1016/j.amjcard.2006.08.041. [DOI] [PubMed] [Google Scholar]
- 44.Despres J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 45.Eckel RH. Lipoprotein lipase, a multifunctional enzyme relevant to common metabolic diseases. N Engl J Med. 1989;320:1060–1068. doi: 10.1056/NEJM198904203201607. [DOI] [PubMed] [Google Scholar]
- 46.Maheux P, Azhar S, Kern PA, Chen Y-DI, Reaven GM. Relationship between insulin-mediated glucose disposal and regulation of plasma and adipose tissue lipoprotein Lipase. Diabetologia. 1997;40:850–858. doi: 10.1007/s001250050759. [DOI] [PubMed] [Google Scholar]
- 47.Prewitt TE, Haynes SG, Graves K, Haines PS, Tyroler HA. Nutrient intake, lipids and lipoprotein cholesterols in black and white children: The Lipid Research Clinics Prevalence Study. Prev Med. 1988;17:247–262. doi: 10.1016/0091-7435(88)90001-1. [DOI] [PubMed] [Google Scholar]
- 48.Despres J-P, Couillard C, Gagnon J, Bergeron J, Leon AS, Rao DC, et al. Race, visceral adipose tissue, plasma lipids, and lipoprotein lipase activity in men and women, The Health, Risk Factors, Exercise Training, and Genetics (HERITAGE) Family Study. Arterioscler Thromb Vasc Biol. 2000;20:1932–1988. doi: 10.1161/01.atv.20.8.1932. [DOI] [PubMed] [Google Scholar]
- 49.Vega GL, Clark LT, Tang A, Marcovina S, Grundy SM, Cohen JC. Hepatic lipase activity is lower in African American men than in white American men: effects of 5’ flanking polymorphism in the Hepatic Lipase Gene (LIPC) J Lipid Res. 1998;39:228–232. [PubMed] [Google Scholar]
- 50.Sumner AE, Vega GL, Genovese DJ, Finley KB, Bergman RN, Boston RC. Normal triglyceride levels despite insulin resistance in African Americans: role of lipoprotein lipase. Metabolism. 2005;54:902–909. doi: 10.1016/j.metabol.2005.03.001. [DOI] [PubMed] [Google Scholar]