Abstract
Postoperative vision loss, a rare but devastating complication, has been reported after spine, cardiac, and head–neck surgeries. Its incidence following spine surgeries exceeds that after cardiothoracic surgeries. Various causes attributed to postoperative blindness include ischemic optic neuropathy, central or branch retinal artery occlusion, cortical blindness, and rarely external ocular injury. Other contributory factors described are microvascular diseases and intraoperative hemodynamic compromise. However, the exact association of these factors with postoperative blindness has not yet been confirmed. In this review, we describe causes, presentation, and treatment of postoperative blindness and also recommend practical guidelines to avoid this complication. The search strategies for this review included both search of electronic databases as well as manual search of relevant articles.
Keywords: Postoperative blindness, spine surgery, vision loss
Introduction
Postoperative vision loss (POVL) is a rare but unexpected and devastating complicationthat is most often associated with cardiac, spine, and head and neck operations. Residual effects of anesthetic agents may mask the initial signs and symptoms of visual loss in the postoperative period. Spine and cardiac surgeries appear to be associated with a higher incidence of perioperative visual loss than other operative procedures. The American Society of Anesthesiologists (ASA) Postoperative Visual Loss Registry reported on 93 cases of visual loss after spine surgery submitted anonymously to the ASA Closed Claims Study.[1] Ischemic optic neuropathy was the cause of visual loss in 83 (89%) of these 93 cases, of which 56 were diagnosed with PION (posterior ischemic optic neuropathy), 19 were diagnosed with AION (anterior ischemic optic neuropathy), and 8 were diagnosed with unspecified ION (ischemic optic neuropathy ) . Estimates of the incidence of POVL after spinal surgery range from 0.028 to 0.2%, but with advances in complex spinal instrumentation and the rise in annual spinal operations, POVL may see an ominous increase in its incidence.[2]
The search strategies for this review included both search of electronic databases as well as manual search of relevant publications or cross references. Electronic search included both PUBMED searches and searches using other search engines. Cross-searches of key references (both electronic and manual search) often yielded other relevant material. The search terms used (in various combinations) were postoperative, vision loss, blindness, spine surgery, and POVL. An attempt was made to include all the articles referring to blindness after spine surgery in various contexts.
Causes of Vision Loss After Spine Surgery
Vision loss after spinal surgery can be categorized into five groups:
External ocular injury (corneal abrasion or sclera injury)
Cortical blindness
Retinal Ischemia
IONs whose subtype, PION is most frequently associated with lumbar operations and thus designated as LION (Lumbar ION).
Acute glaucoma[3]
External ocular injuries
Corneal trauma can result in irritation, abrasion, or even laceration. It can be a self-limiting process or can increase the risk of ocular inflammation and infection. Patients usually present with pain and foreign body sensation in the eye. Ophthalmic consultation is recommended as and when detected.
Cortical blindness
Total cortical blindness is usually accompanied by signs of stroke in the parieto-occipital region. The patient may suffer agnosia, an inability to interpret sensory stimuli. Pupillary reflexes are preserved and most of the visual field is restored within days, but impairment in spatial perception and in the relationship between sizes and distances may remain. Visual attention may be restricted, and images formed on all parts of retina may not be visualized at one time.
Cortical blindness can result from global or focal ischemia, cardiac arrest, hypoxemia, intracranial hypertension and exsanguinating hemorrhage, vascular occlusion, thrombosis, intracranial hemorrhage, vasospasm, and emboli.[4]
Retinal ischemia: Branch and central retinal artery occlusion
Central retinal artery occlusion (CRAO) decreases the blood supply to the entire retina, while occlusion of a retinal arterial branch (BRAO) is a localized injury affecting only a portion of the retina. In most instances this injury is unilateral. Retinal ischemia can be due to external compression of the eye, decreased blood supply to the retina (embolism to the retinal arterial circulation or decreased blood flow from a systemic cause), and impaired venous drainage of the retina. Occasionally, retinal arterial thrombosis may occur due to a coagulation disorder.
The most common cause of perioperative retinal arterial occlusion is improper patient positioning resulting in external compression of the eye. External compression of the eye produces sufficient intraocular pressure (IOP) to stop flow in the central retinal artery. It is seen in spine surgery performed with the patient in prone position.[5–7] Various factors which increase the vulnerability for external compression include altered facial anatomy, osteogenesis imperfecta, and exophthalmos. Patients belonging to Asian descent tend to have lower nasal bridges, which may increase the risk of external compression.[8]
Emboli, though rare, can directly impair blood flow in the central retinal artery (CRA) itself or a branch of it. Paradoxical embolism originating from the operative site and reaching the arterial circulation through a patent foramen ovale has rarely been reported as a cause of perioperative retinal vascular occlusion.[9] Hypotension per se seems to be a rare cause of retinal ischemia.
Patients have painless visual loss and abnormal pupil reactivity. There may be unilateral loss of vision usually with loss of light perception, afferent pupil defect, periorbital and/or eyelid edema, chemosis, proptosis, ptosis, paresthesias of the supraorbital region, hazy/cloudy cornea, and corneal abrasion. Loss of eye movements, ecchymosis, or other trauma near the eye has also been reported.
Fundoscopic examination shows opacification or whitening of the ischemic retina, and narrowing of retinal arterioles.[10,11] BRAO is characterized by cholesterol emboli (bright yellowish, glistening), calcific emboli (white, nonglistening), or migrant pale emboli of platelet and fibrin (dull, dirty white). A cherry-red macula with a white ground-glass appearance of the retina and attenuated arterioles is a “classic” diagnostic sign in CRAO.
Early orbital computed tomography (CT) or magnetic resonance imaging (MRI) showed proptosis and extra ocular muscle swelling, although most cases did not have imaging studies to confirm the diagnosis.[12] Findings were similar to the syndrome of “Saturday night retinopathy” in intoxicated individuals who slept while their eyes were compressed.[13]
Orbital compartment syndrome causes compression of the arterial and venous circulations resulting in CRAO and optic nerve injury. It is an acute ophthalmologic injury requiring prompt decompression to relieve the increased IOP. Ischemic ocular compartment syndrome has been reported in a patient undergoing spine surgery in the prone position. Other proposed mechanisms causing retinal ischemia include excitotoxicity,[14] hyperemia[15] and hypoperfusion.[16]
Branch Retinal Artery Occlusion(BRAO) causes permanent ischemic retinal damage with partial visual field loss. BRAO is primarily the result of emboli, and in few cases vasospasm. Most of emboli come from intravascular injections and circulating embolic material from the surgical field or cardiopulmonary bypass (CPB) equipment in cardiac surgery. BRAO has also been reported in a patient in prone position for spine surgery. After surgery a patent foramen ovale was discovered and it was believed that he had sustained a paradoxical air, fat, or bone marrow embolization from the operative site in the lumbar spine.[9]
Ischemic optic neuropathy
Ischemic optic neuropathy, without warning signs, is the leading cause of sudden visual loss in patients above 50 years of age. Most perioperative cases of ION are in adults, although there are some reports in children. The estimated annual incidence of nonarteritic ION in the United States is 2.3/100,000.[17] ION can be of two types anterior (AION) and posterior (PION). It can be arteritic or non-arteritic. ION is termed “arteritic” when it is secondary to inflammations of blood vessels, chiefly giant cell arteritis (temporal arteritis). The term nonarteritic is used when it is secondary to occlusive disease or other noninflammatory disorders of blood vessels. Nonarteritic ION (NAION), more common than arteritic, is overwhelmingly the type found perioperatively. The annual incidence of NAION was reported as 82 per 100,000 persons.[18] It has been reported after various surgical procedures, with most after cardiothoracic surgery,[19,20] instrumented spinal fusion operations,[21–23] head and neck surgery,[24,25] and surgery on the nose or sinuses,[26,27] vascular surgery, urologic and general surgical procedures including liposuction, cesarean section, and gynecologic surgery.[28–33]
Ischemia of the optic nerve in vitro leads to axonal destruction. When oxygen delivery decreases, adenosine triphosphate is depleted, leading to membrane depolarization, influx of Na+ and Ca2+ through specific voltage-gated channels, and reversal of the Na+–Ca2+ exchange pump.[34] Ca2+ overload damages cells from activation of proteolytic and other enzymes. ION may lead to neuronal injury by apoptotic cell death, which may be stimulated in vitro with reduced oxygen delivery.[35]
Anatomic or physiologic variations in the circulatory supply of the optic nerve may predispose some patients to the development of AION. The “watershed concept,” which states that impaired perfusion and distribution within a posterior ciliary artery predisposes the optic disc to infarction, is disputed. Arnold and Hepler showed that delayed filling of watershed zones was more common in normal eyes than in patients with AION.[36] Thus, reduced perfusion pressure in the region of the paraoptic branches of the short posterior ciliary arteries results in optic disc hypoperfusion, rather than a watershed event.[37]
A small optic disc may play a role in a subject's susceptibility to AION.[38] Mechanisms include mechanical obstruction of axoplasmic flow, axoplasmic stasis, stiff cribriform plate, and decreased availability of neurotrophic factors to retinal ganglion cells after ischemia.[39]
Possible factors of perioperative ION include decreased systemic blood pressure; blood loss; anemia or hemodilution; altered venous hemodynamics; flow of cerebrospinal fluid in the optic nerve; abnormal auto regulation in the optic nerve; anatomic variants in blood supply to the optic nerve; small cup-to-disc ratio; and the use of vasopressors. The systemic vascular risk factors include hypertension, diabetes, atherosclerosis, hyperlipidemia, and smoking history; prone positioning; lengthy surgery for spinal fusion; and other preexisting systemic abnormalities, such as sleep-apnea syndrome and hypercoagulability.[40–43]
AION and PION have been reported in the setting of massive fluid replacement. Most of these case reports include patients who were operated on in the prone position. Excessive fluid administration could result in increased IOP or accumulation of fluid in the optic nerve, or both. So internal “compartment syndrome” may occur in the optic nerve because the central retinal vein exits out of the optic nerve. Fluid may accumulate in the vicinity of the lamina cribrosa that compress axons as they transit this region. Patients in the ASA Postoperative Visual Loss Registry received on average 9.7 L of crystalloids intraoperatively, suggesting, although not proving, that fluid replacement may play a role.[21,22,40]
Facial edema is often seen after spinal fusion in many patients.[44] Some case reports found it to be associated with vision loss, but others did not find any association of facial edema with vision loss. Therefore, its relevance remains unclear and the notion that facial edema is a risk factor is unproved.
Various case reports suggest that use of vasopressors such as epinephrine and phenylephrine intraoperatively can increase the risk of vision loss.[45] However, α-adrenergic receptors are not known to be located in the optic nerve and the blood–brain barrier prevents entry of systemically administered agents, except possibly in the prelaminar zone of the nerve. Therefore, the role of vasopressors use in ION remains unclear and no clear inference can be drawn at present.
Acute glaucoma
Acute angle-closure glaucoma has been described rarely after general anesthesia. Patients present with a painful red eye and cloudy or blurred vision, accompanied by headache, nausea, and vomiting. This condition is often bilateral. It should be differentiated from corneal abrasion, which also produces pain but without the papillary signs, increased IOP, subjective visual loss, and headache.[46]
Prevention
Corneal injuries can be prevented by the common practice of applying lubricants and taping the patient's eyes shut prior to positioning.[47,48] Cortical damage can be prevented by the maneuvers that decrease the chances of embolization.[49] To prevent CRAO, the anesthesiologist must avoid compression of the globe. Pressure on the eyes from anesthetic masks is avoidable. If surgery is near the face, the surgeon's arm must not be allowed to rest on the patient's eyes. In patients positioned prone for surgery, a foam headrest should be used with the eyes properly placed in the opening of the headrest; the position of the head and the eyes should be checked intermittently by palpation or visualization. The horseshoe headrest for the prone-positioned patient must be used with great caution, and there are safer choices available at present. For the patient positioned prone for cervical spine surgery, this headrest should not be used because of the greater chance of head movement by the surgeon, leading to compression of the eye.
It is advisable to check eyes intermittently while the patient is prone. Considering results in rodent models of elevated IOP, it is advisable to examine eyes after change in position and the absence of external compression at least every 20 min. If the patient's head does not fit the headrest adequately or for surgery on the cervical spine, a pinhead holder should be considered. When a transparent headpiece is in use on the operating table, a mirror can be positioned underneath to indirectly view the eyes on the headrest. The use of goggles to cover the eyes is not advised when the head is positioned prone in a conventional square foam headrest.[50]
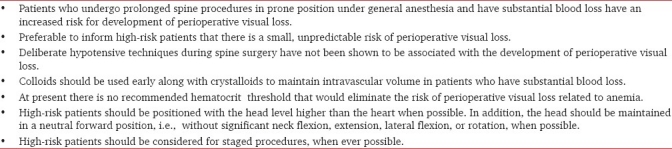
The summary of ASA task force recommendations to prevent perioperative blindness for patients undergoing spine fusion surgeries is shown as Table 1.[51]
Table 1.
Summary recommendations of the American Society of Anesthesiologists Task Force on perioperative blindness
Treatment
The consensus of the Task Force is that a high-risk patient's vision should be assessed when the patient becomes awake. If there is an evidence of potential visual loss, an urgent ophthalmologic consultation should be obtained to determine its cause. Further management may include optimizing hematocrit levels, hemodynamic status, and arterial oxygenation. To rule out intracranial causes of visual loss, magnetic resonance imaging may be considered. The Task Force does not suggest any role for anti platelet agents, steroids, or intraocular pressure lowering agents in the treatment of perioperative ischemic optic neuropathy.
Currently available methods of treatment are not satisfactory. Treatment of CRAO includes ocular massage to lower IOP (contraindicated if glaucoma cannot be ruled out) and thereby dislodge an embolus. Intravenous acetazolamide, 5% CO2 in oxygen inhalation have been attempted to enhance dilation and increase oxygen delivery from retinal and choroidal vessels.[52] Further treatment should be prescribed by the ophthalmologist and may include thrombolysis. A preliminary clinical study showed that fibrinolysis through a catheter in the ophthalmic artery within 6–8 h after spontaneous CRAO was associated with improved visual outcome.[53] Localized application of hypothermia to the affected eye has also been tried.[54]
There is no definitive treatment of ION. Few case reports have proven the benefit of acetazolamide.[55] Diuretics such as mannitol or furosemide reduce IOP and edema. Benefit of steroids is not yet proven. Hypotension and anemia should be corrected. Patient should be kept in a head-up position if increased ocular venous pressure is suspected. If visual loss is due to ocular compartment syndrome, immediate decompression (lateral canthotomy) is indicated. Few case reports recommend application of hyperbaric oxygen[43], use of neuroprotective agents[56] or drugs that lower IOP, but without any proven efficacy
Acute glaucoma is an emergency, and ophthalmologic consultation should be obtained immediately. Patients are treated with β-adrenergic antagonists, α-adrenergic agonists, carbonic anhydrase inhibitors, cholinergic agonists, and corticosteroids. Peripheral iridectomy should be performed if needed.[57]
To conclude, perioperative vision loss is a serious complication with medicolegal implications. Anesthetists, especially those associated with high end major spinal procedures in prone position, must take adequate precautions during positioning, maintain adequate hematocrit and intravascular volume.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Lee LA, Roth S, Posner KL, Cheney FW, Caplan RA, Newman NJ. The American society of anesthesiologists postoperative visual loss registry: Analysis of 93 spine surgery cases with postoperative visual loss. Anesthesiology. 2006;105:652–9. doi: 10.1097/00000542-200610000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Chang SH, Miller NR. The incidence of vision loss due to peri- operative ischemic optic neuropathy associated with spine surgery: The Johns Hopkins Hospital Experience. Spine. 2005;30:1299–302. doi: 10.1097/01.brs.0000163884.11476.25. [DOI] [PubMed] [Google Scholar]
- 3.Gartner S, Billet E. Acute glaucoma: As a complication of general surgery. Am J Ophthalmol. 1958;45:668–71. doi: 10.1016/0002-9394(58)92174-3. [DOI] [PubMed] [Google Scholar]
- 4.Siesjö BK. Pathophysiology and treatment of focal cerebral ischemia, II: Mechanisms of damage and treatment. J Neurosurg. 1992;77:337–54. doi: 10.3171/jns.1992.77.3.0337. [DOI] [PubMed] [Google Scholar]
- 5.Sys J, Michielsen J, Mertens E, Verstreken J, Tassignon MJ. Central retinal artery occlusion after spinal surgery. Eur Spine J. 1996;5:74–5. doi: 10.1007/BF00307832. [DOI] [PubMed] [Google Scholar]
- 6.Grossman W, Ward WT. Central retinal artery occlusion after scoliosis surgery with a horseshoe headrest: Case report and literature review. Spine. 1993;18:1226–28. doi: 10.1097/00007632-199307000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Hollenhorst RW, Svien HJ, Benoit CF. Unilateral blindness occurring during anesthesia for neurosurgical operations. Arch Ophthalmol. 1954;52:819–30. doi: 10.1001/archopht.1954.00920050825002. [DOI] [PubMed] [Google Scholar]
- 8.Bradish CF, Flowers M. Central retinal artery occlusion in association with osteogenesis imperfecta. Spine. 1987;12:193–94. doi: 10.1097/00007632-198703000-00018. [DOI] [PubMed] [Google Scholar]
- 9.Katz DA, Karlin LI. Visual field defect after posterior spine fusion. Spine. 2005;30:83–5. doi: 10.1097/01.brs.0000152169.48117.c7. [DOI] [PubMed] [Google Scholar]
- 10.Hayreh SS, Kolder HE, Weingeist TA. Central retinal artery occlusion and retinal tolerance time. Ophthalmology. 1980;87:75–8. doi: 10.1016/s0161-6420(80)35283-4. [DOI] [PubMed] [Google Scholar]
- 11.Wray SH. The management of acute visual failure. J Neurol Neurosurg Psychiatry. 1993;56:234–40. doi: 10.1136/jnnp.56.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar N, Jivan S, Topping N, Morrell AJ. Blindness and rectus muscle damage following spine surgery. Am J Ophthalmol. 2004;138:889–91. doi: 10.1016/j.ajo.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 13.Jayam AV, Hass WK, Carr RE, Kumar AJ. Saturday night retinopathy. J Neurol Sci. 1974;22:413–8. doi: 10.1016/0022-510x(74)90077-x. [DOI] [PubMed] [Google Scholar]
- 14.Louzada P, Dias JJ, Santos WF, Bradford HF, Lachat JJ, Coutinho NJ. Glutamate release in experimental ischaemia of the retina: An approach using microdialysis. J Neurochem. 1992;59:358–63. doi: 10.1111/j.1471-4159.1992.tb08912.x. [DOI] [PubMed] [Google Scholar]
- 15.Roth S, Pietrzyk Z. Blood flow after retinal ischemia in cats. Invest Ophthalmol Vis Sci. 1994;35:3209–17. [PubMed] [Google Scholar]
- 16.Hughes WF. Quantitation of ischemic damage in the rat retina. Exp Eye Res. 1991;53:573–82. doi: 10.1016/0014-4835(91)90215-z. [DOI] [PubMed] [Google Scholar]
- 17.Johnson LJ, Arnold AC. Incidence of nonarteritic and arteritic anterior ischemic optic neuropathy: A population-based study in the state of Missouri and Los Angeles County, California. J Clin Neuro-ophthalmol. 1994;14:38–44. [PubMed] [Google Scholar]
- 18.Lee MS, Grossman D, Arnold AC, Sloan FA. Incidence of nonarteritic anterior ischemic optic neuropathy: Increased risk among diabetic patients. Ophthalmology. 2001;118:959–63. doi: 10.1016/j.ophtha.2011.01.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Slavin ML. Ischemic optic neuropathy after cardiac arrest. Am J Ophthalmol. 1987;104:435–6. doi: 10.1016/0002-9394(87)90247-9. [DOI] [PubMed] [Google Scholar]
- 20.Tice DA. Ischemic optic neuropathy and cardiac surgery. Ann Thorac Surg. 1987;44:677. doi: 10.1016/s0003-4975(10)62171-6. [DOI] [PubMed] [Google Scholar]
- 21.Ho VTG, Newman NJ, Song S, Suzan S, Ksiazek S, Steven Roth. Ischemic optic neuropathy following spine surgery. J Neurosurg Anesthesiol. 2005;17:38–44. [PMC free article] [PubMed] [Google Scholar]
- 22.Cheng MA, Sigurdson W, Tempelhoff R, Lauryssen C. Visual loss after spine surgery: A survey. Neurosurgery. 2000;46:625–31. doi: 10.1097/00006123-200003000-00020. [DOI] [PubMed] [Google Scholar]
- 23.Murphy MA. Bilateral posterior ischemic optic neuropathy after lumbar spine surgery. Ophthalmology. 2003;110:1454–7. doi: 10.1016/S0161-6420(03)00480-9. [DOI] [PubMed] [Google Scholar]
- 24.Kirkali P, Kansu T. A case of unilateral posterior ischemic optic neuropathy after radical neck dissection. Ann Ophthalmol. 1990;22:297–8. [PubMed] [Google Scholar]
- 25.Schobel GA, Schmidbauer M, Millesi W, Undt G. Posterior ischemic optic neuropathy following bilateral radical neck dissection. Int J Oral Maxillofac Surg. 1995;24:283–7. doi: 10.1016/s0901-5027(95)80030-1. [DOI] [PubMed] [Google Scholar]
- 26.Buus DR, Tse DT, Farris BK. Ophthalmic complications of sinus surgery. Ophthalmology. 1990;97:612–9. doi: 10.1016/s0161-6420(90)32535-6. [DOI] [PubMed] [Google Scholar]
- 27.Maniglia AJ. Fatal and major complications secondary to nasal and sinus surgery. Laryngoscope. 1989;99:276–83. doi: 10.1288/00005537-198903000-00008. [DOI] [PubMed] [Google Scholar]
- 28.Brown RH, Schauble JF, Miller NR. Anemia and hypotension as contributors to perioperative loss of vision. Anesthesiology. 1994;80:222–6. doi: 10.1097/00000542-199401000-00033. [DOI] [PubMed] [Google Scholar]
- 29.Chun DB, Levin DK. Ischemic optic neuropathy after hemorrhage from a cornual ectopic gestation. Am J Obstet Gynecol. 1997;177:1550–2. doi: 10.1016/s0002-9378(97)70111-x. [DOI] [PubMed] [Google Scholar]
- 30.Gupta M, Puri P, Rennie IG. Anterior ischemic optic neuropathy after emergency caesarean section under epidural anesthesia. Acta Anaesthesiol Scand. 2002;46:751–2. doi: 10.1034/j.1399-6576.2002.460621.x. [DOI] [PubMed] [Google Scholar]
- 31.Minagar A, Schatz NJ, Glaser JS. Liposuction and ischemic optic neuropathy: Case report and review of literature. J Neurol Sci. 2000;181:132–6. doi: 10.1016/s0022-510x(00)00409-3. [DOI] [PubMed] [Google Scholar]
- 32.Williams GC, Lee AG, Adler HL, Coburn A, Rosas AL, Tang RA, et al. Bilateral anterior ischemic optic neuropathy and branch retinal artery occlusion after radical prostatectomy. J Urol. 1999;162:1384–5. [PubMed] [Google Scholar]
- 33.Weber E, Coyler M, Lesser R, Subramanian P. Posterior ischemic optic neuropathy after minimally invasive prostatectomy. J Neuro Ophthalmol. 2007;27:285–7. doi: 10.1097/WNO.0b013e31815b9f67. [DOI] [PubMed] [Google Scholar]
- 34.Brown AM, Wender R, Ransom BR. Ionic mechanisms of aglycemic axon injury in mammalian central white matter. J Cereb Blood Flow Metab. 2001;21:385–95. doi: 10.1097/00004647-200104000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Levin LA, Louhab A. Apoptosis of retinal ganglion cells in anterior ischemic optic neuropathy. Arch Ophthalmol. 1996;114:488–91. doi: 10.1001/archopht.1996.01100130484027. [DOI] [PubMed] [Google Scholar]
- 36.Arnold AC, Hepler RS. Fluorescein angiography in acute nonarteritic anterior optic neuropathy. Am J Ophthalmol. 1994;117:222–30. doi: 10.1016/s0002-9394(14)73080-6. [DOI] [PubMed] [Google Scholar]
- 37.Olver JM, Spalton DJ, McCartney AC. Microvascular study of the retrolaminar optic nerve in man: The possible significance in anterior ischaemic optic neuropathy. Eye. 1990;4:7–24. doi: 10.1038/eye.1990.3. [DOI] [PubMed] [Google Scholar]
- 38.Beck RW, Servais GE, Hayreh SS. Anterior ischemic optic neuropathy, IX: Cup-to-disc ratio and its role in pathogenesis. Ophthalmology. 1987;94:1503–8. [PubMed] [Google Scholar]
- 39.Arnold AC. Pathogenesis of nonarteritic anterior ischemic optic neuropathy. J Neuro-ophthalmol. 2003;23:157–63. doi: 10.1097/00041327-200306000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Buono LM, Foroozan R. Perioperative posterior ischemic optic neuropathy: Review of the literature. Surv Ophthalmol. 2005;50:15–26. doi: 10.1016/j.survophthal.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 41.Glueck CJ, Wang PG, Bell H, Rangaraj V, Goldenberg N. Nonarteritic anterior ischemic optic neuropathy: Associations with homozygosity for the C677T methylenetetrahydrofolate reductase mutation. J Lab Clin Med. 2004;143:184–92. doi: 10.1016/j.lab.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 42.Williams EL, Hart WM, Tempelhoff R. Postoperative ischemic optic neuropathy. Anesth Analg. 1995;80:1018–29. doi: 10.1097/00000539-199505000-00029. [DOI] [PubMed] [Google Scholar]
- 43.Roth S. Postoperative blindness. In: Miller RD, editor. Textbook of Anesthesia. 6th ed. New York: Elsevier; 2005. pp. 2991–3020. [Google Scholar]
- 44.Dunker S, Hsu HY, Sebag J, Sadun AA. Perioperative risk factors for ischemic optic neuropathy. J Am Coll Surg. 2002;194:705–10. doi: 10.1016/s1072-7515(02)01210-3. [DOI] [PubMed] [Google Scholar]
- 45.Hayreh SS, Joos KM, Podhajsky PA, Long CR. Systemic diseases associated with nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol. 1994;118:766–80. doi: 10.1016/s0002-9394(14)72557-7. [DOI] [PubMed] [Google Scholar]
- 46.Roth S, Thisted RA, Erickson JP, Black S, Schreider BD. Eye injuries after non-ocular surgery: A study of 60, 965 anesthetics from 1988 to 1992. Anesthesiology. 1996;85:1020–7. doi: 10.1097/00000542-199611000-00009. [DOI] [PubMed] [Google Scholar]
- 47.Stambough JL, Dolan D, Werner R, Godfrey E. Ophthalmologic complications associated with prone positioning in spine surgery. J Am Acad Orthop Surg. 2007;15:156–65. doi: 10.5435/00124635-200703000-00005. [DOI] [PubMed] [Google Scholar]
- 48.Grover VK, Kumar KV, Sharma S, Sethi N, Grewal SPS. Comparison of methods of eye protection under general anaesthesia. Can J Anaesth. 1998;45:575–7. doi: 10.1007/BF03012712. [DOI] [PubMed] [Google Scholar]
- 49.Pugsley W, Klinger L, Paschalis C, Treasure T, Harrison M, Newman S. The impact of microemboli during cardiopulmonary bypass on neuropsychological functioning. Stroke. 1994;25:1393–9. doi: 10.1161/01.str.25.7.1393. [DOI] [PubMed] [Google Scholar]
- 50.Roth S. Postoperative vision loss. In: Miller RD, editor. Textbook of Anesthesia. 7th ed. New York: Elsevier; 2010. p. 2826. [Google Scholar]
- 51.Arens JF, Connis RT, Domino KB, Lee LA, Miller NR, Mirza SK. Practice advisory for perioperative visual loss associated with spine surgery. A report by the American society of anesthesiologists task force on perioperative blindness. Anesthesiology. 2006;104:1319–28. doi: 10.1097/00000542-200606000-00027. [DOI] [PubMed] [Google Scholar]
- 52.Alm A, Bill A. Ocular circulation. In: Adler FH, editor. Adler's Physiology of the Eye. 8th ed. St. Louis: CV Mosby; 1987. pp. 183–203. [Google Scholar]
- 53.Feltgen N, Neubauer A, Jurklies B, Schmoor C, Wanke J, Maier-Lenz H. Multicenter study of the European Assessment Group for Lysis in the Eye (EAGLE) for the treatment of central retinal artery occlusion: Design issues and implications. EAGLE Study report no. 1. Graefes Arch Clin Exp Ophthalmol. 2006;244:950–6. doi: 10.1007/s00417-005-0140-2. [DOI] [PubMed] [Google Scholar]
- 54.Faberowski N, Stefansson E, Davidson RC. Local hypothermia protects the retina from ischemia: A quantitative study in the rat. Invest Ophthalmol Vis Sci. 1989;30:2309–13. [PubMed] [Google Scholar]
- 55.Hayreh SS. Anterior ischaemic optic neuropathy: III, Treatment, prophylaxis, and differential diagnosis. Br J Ophthalmol. 1974;58:981–9. doi: 10.1136/bjo.58.12.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Arnold AC, Levin LA. Treatment of ischemic optic neuropathy. Semin Ophthalmol. 2002;17:39–46. doi: 10.1076/soph.17.1.39.10292. [DOI] [PubMed] [Google Scholar]
- 57.Riordan EP. Glaucoma. In: Vaughan DG, editor. General Ophthalmology. 14th ed. Norwalk: Appelton and Lange; 1995. pp. 208–55. [Google Scholar]


