Abstract
Objective:
To study the effectiveness of three predictors of successful caudal block in children, viz. swoosh test, heart rate response to injection, and laxity of anal sphincter tone.
Aim:
To improve the success rates of caudal block in children by identifying the best predictor.
Background:
Caudal blocks in children are placed after induction of anesthesia. Although simple to learn and perform, the success rate of the blocks may be variable especially in teaching hospitals where trainee anesthetists perform these blocks.
Materials and Methods:
223 patients, aged 2–12 years, undergoing lower abdominal and urologic surgery were studied. 0.25% Bupivacaine was administered after induction of general anesthesia according to the Armitage regimen.
Results:
The sensitivity and specificity were highest with the sphincter tone test (sensitivity 95.22%, specificity 92.86%), followed by the heart rate response (sensitivity 92.82%, specificity 78.57%) and the swoosh test (sensitivity 66.51%, specificity 35.71%). The anal sphincter tone test had the highest positive predictive value (99.5%) and positive likelihood ratio (13.33). The heart rate response had a positive predictive value of 98.48% and a positive likelihood ratio of 4.33. The swoosh test, in our study, had a positive predictive value of 93.92% and a positive likelihood ratio of 1.035.
Conclusion:
The anal sphincter tone test was the best predictor of successful caudal block. We recommend the use of these additional simple predictors of accurate needle placement to increase the success rate of caudal block especially in teaching hospitals.
Keywords: Anal sphincter tone, caudal block, heart rate response, swoosh test
Introduction
Caudal epidural block is a commonly performed procedure in pediatric age group. It offers excellent analgesia without the side effects of intravenous opioid medications, viz. nausea, sedation, and respiratory depression. Caudal blocks are generally performed after induction of general anesthesia in children. Traditional teaching relies on the subjective sensation of “give” or “pop” felt by the operator as the advancing needle pierces the sacrococcygeal ligament and the lack of resistance to injection of the local anesthetic. Although the block is easily performed, the success rate is less than 100% and varies with the experience of the operator. Objective parameters of successful caudal needle placement will increase the success of the block. In a large teaching hospital such as ours, with a number of residents in training, additional methods to predict correct needle placement would increase accuracy.
Several studies have evaluated the accuracy of parameters to predict correct caudal needle placement. These include an audible “swoosh” on auscultation over the lower back during injection,[1] a reduction in heart rate during drug injection[2] and a lax anal sphincter[3] at the end of the procedure. This study was undertaken to compare the sensitivity, specificity, positive predictive value, and negative predictive value of the following predictors of successful caudal block, viz. swoosh test, heart rate reduction during drug injection, and laxity of anal sphincter following procedure.
Materials and Methods
After Institutional Ethics Committee permission, a prospective study was undertaken including 223 consecutive patients who received a caudal epidural block. Sample population included patients between the ages of 2–12 years, of either sex, belonging to ASA grade I or II who received a caudal epidural block as part of their routine anesthetic regimen. Surgeries performed were elective surgeries below the umbilicus where caudal block was administered for perioperative analgesia. Patients in whom consent was not obtained or had contraindications to caudal block, viz. coagulopathy, sacral deformity, and local site infection were excluded from the study. Patients undergoing anorectal surgery, where it was not possible to reliably test anal sphincter tone, were also excluded from the study.
All patients were premedicated with 0.05 mg/kg midazolam intravenously (IV). Caudal blocks were performed after induction of general anesthesia. Anesthesia was induced with thiopentone and endotracheal intubation performed after administration of IV atracurium. Baseline heart rate was recorded after induction. Anesthesia was maintained using nitrous oxide and oxygen in a concentration of 50:50 and 1% isoflurane. Ventilation was controlled throughout the surgery and atracurium was administered for muscle relaxation. The blocks were performed by resident anesthetists as well as by consultants. Under due aseptic conditions, with the patient in the left lateral position, a 22 G hypodermic needle was used to locate the sacral hiatus. After the “give” of the sacrococcygeal ligament was obtained, 0.25% bupivacaine in a volume of 0.5–1 ml/kg was injected, depending on the site of surgery based on the Armitage regimen. Absence of tissue swelling and resistance to injection of the drug were used as clinical criteria of successful needle placement. During injection of the drug, the area over the lower lumbar spine corresponding to the needle tip was auscultated for an audible “swoosh” sound. The drug was injected at a rate of about 1 ml/3 s. After initial negative aspiration for blood, slow incremental injection with intermittent negative aspiration was performed to prevent intravascular injection. Heart rate reduction, if any, during the course of drug injection was noted. These observations were made by an independent anesthesiologist not performing the block. At the end of surgery, after reversal of the neuromuscular block, anal sphincter tone was assessed by an independent observer (the pediatric surgeon). The sphincter tone, whether lax or tight, was noted.
Number of attempts used to locate the caudal epidural space, experience of the anesthetist administering the block, and occurrence of any complications during performance of the block (dural puncture, bleeding, etc.) were noted. The success of the block was judged by the postoperative pain scores and the need for rescue analgesia. Analgesia was assessed using the objective pain scale. Patients with a pain score greater than 4 were judged to be in pain and administered IV fentanyl 1 μg/kg as rescue analgesic.
The following were computed for each predictor: sensitivity, the proportion of actual positives (working caudal block) which are correctly identified as such (swoosh positive, heart rate reduction, and lax anal sphincter); specificity, the proportion of actual negatives (caudal block inadequate) which are correctly identified (swoosh negative, no reduction in heart rate, and tight anal sphincter); positive predictive value (PPV), proportion of patients with positive test result (working caudal block) which are correctly identified; negative predictive value (NPV), proportion of patients with negative test result (inadequate caudal block) which are correctly identified. Likelihood ratio for each predictor was computed; positive likelihood ratio (LR+), how much the odds of the outcome (working caudal block) increase when a test is positive; negative likelihood ratio (LR-), how much the odds of the outcome (inadequate caudal block) decrease when a test is negative. 95% confidence intervals were also calculated for each parameter.
Results
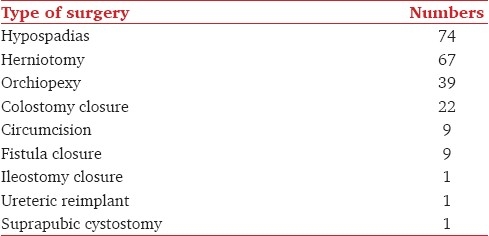
A total of 223 patients were studied. The age ranged between 2 and 12 years, with a mean of 48.5 months (SD 32.1). 74% patients were less than 5 years of age. The weight ranged between 4 and 35 kilograms, with a mean of 15.35 kg (SD 4.08). 202 patients (90.58%) were male. 190 blocks (85.2%) were administered by residents at various levels of training, and 33 blocks (14.8%) were administered by consultants. 88% of the blocks were administered in 1 or 2 attempts (60.75% in 1st attempt; 27.25% in 2nd attempt). Surgeries performed included herniotomy, orchiopexy, hypospadias repair, and circumcision [Table 1].
Table 1.
List of surgeries performed (n = 223)
Of the 223 patients studied, 209 were judged to have an adequate caudal block on the basis of post operative pain scores. 14 patients needed rescue analgesic and were judged to have failed/inadequate block.
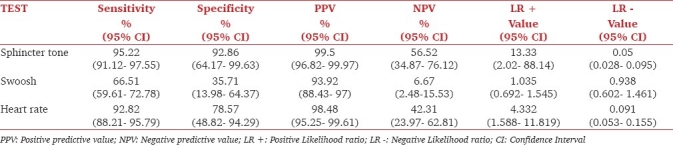
The swoosh test had a sensitivity of 66.51% (95% CI 59.61–072.78), specificity of 35.71% (95% CI 13.98– 64.37), positive predictive value of 93.92% (95% CI 88.43–97), and a negative predictive value of 6.67% (95% CI 2.48–15.53).
The heart rate response had a sensitivity of 92.82% (95% CI 88.21–95.79), specificity of 78.57% (95% CI 48.82–94.29), positive predictive value of 98.48% (95% CI 95.25–99.61), and a negative predictive value of 42.31% (95% CI 23.97–62.81).
The sphincter tone test had a sensitivity of 95.22% (95% CI 91.12–97.55), specificity of 92.86% (95% CI 64.17–99.63), positive predictive value of 99.5% (95% CI 96.82–99.97), and a negative predictive value of 56.52% (95% CI 34.87–76.12).
The swoosh test had a LR+ of 1.035 (95% CI 0.692–1.545) and a LR- of 0.938 (95% CI 0.602–1.461). The heart rate response had a LR+ of 4.332 (95% CI 1.588–11.819) and a LR- of 0.091 (95% CI 0.053- 0.155). The sphincter tone test had a LR+ of 13.33 (95% CI 2.02- 88.14) and a LR- of 0.05 (95% CI 0.028- 0.095) [Table 2].
Table 2.
Sensitivity, specificity, positive predictive value, negative predictive value, positive and negative likelihood ratio for sphincter tone test, swoosh test, and heart rate reduction following caudal block
Discussion
Caudal epidural blocks in children are usually placed after induction of general anesthesia. Traditionally, the operator relies on the subjective sensation of “give” or “pop” of the sacrococcygeal ligament as the advancing needle pierces it. Additional predictors of correct needle placement will increase accuracy and is especially useful in teaching hospitals where trainees perform such blocks.
Several groups have studied the effectiveness of additional predictors of accurate needle placement, viz. use of ultrasound,[4,5] nerve stimulation,[6] heart rate response to injection; swoosh test and anal sphincter tone test. We compared three simple predictors of accurate needle placement—the swoosh test, heart rate response, and the anal sphincter tone test.
“Swoosh” test is an audible sound heard on auscultation over lower back during injection of saline or the local anesthetic drug. It has been studied as a safer alternative to the original “whoosh” test where injection of air into the epidural space produced an audible whoosh on auscultation.[1,7] Our study showed a sensitivity of 66.51% and a specificity of 35.71% for the swoosh test.
Verghese et al.[3] correlated laxity of patient's anal sphincter with the effectiveness of caudal block. The anal sphincter tone test in their study had a sensitivity of 98.1% and a specificity of 94.4%. Our results were similar with a sensitivity of 95.22% and specificity of 92.86%. A lax anal sphincter at the end of surgery thus implies a “working” caudal block and obviates the need for supplemental analgesia.
Fall in heart rate has been evaluated as an objective predictor of successful block. A reduction in heart rate of more than 3 beats per minute has been cited as sign of correct needle placement.[8] The mechanism proposed is the effect of the injectate on the pressure receptors in the caudal epidural space. Our results showed a sensitivity of 92.82% for heart rate response and a specificity of 78.57%. Thus the heart rate response is an immediate predictor of successful needle placement. This result, however, is within the context of our study, i.e., in the setting of general anesthesia with isoflurane in 50% nitrous oxide after midazolam premedication and thiopentone sodium induction.
The LR+ was greatest with the anal sphincter tone test (13.33), followed by the heart rate response (4.332) and the swoosh test (1.035). The LR- was least with the anal sphincter tone test (0.05). The LRs- for the heart rate response and the swoosh test were 0.091 and 0.938, respectively. The results of our study indicate that the anal sphincter tone test, i.e., a lax anal sphincter best predicts a working caudal block. This was followed by the heart rate response, i.e., a reduction in heart rate of at least 3 beats per minute during injection. Our results indicate that, of the 3 predictors studied, the swoosh test was the least effective predictor of caudal block.
In conclusion, we studied three simple, cost effective predictors of caudal block; these are easy to use and require no special equipment or training of personnel. On the basis of our results, we recommend the use of the heart rate response as an early predictor of successful needle placement and the anal sphincter tone test as a sign of working caudal block.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Orme RM, Berg SJ. The ‘swoosh’ test—an evaluation of a modified ‘whoosh’ test in children. Br J Anaesth. 2003;90:62–5. [PubMed] [Google Scholar]
- 2.Krishna HM, Sehgal R, Kumar Rakesh. Heart Rate changes with Test Dose and Total Dose during Caudal Epidural block in Children as a test to predict correct needle placement. J Anaesth Clin Pharmacol. 2004;20:283. [Google Scholar]
- 3.Verghese ST, Mostello LA, Patel RI, Kaplan RF, Patel KM. Testing Anal Sphincter Tone Predicts the Effectiveness of Caudal Analgesia in Children. Anesth Analg. 2002;94:1161–4. doi: 10.1097/00000539-200205000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz DA, Dunn SM, Connelly NR. Ultrasound and caudal blocks in children. Paediatr Anaesth. 2006;16:900–1. doi: 10.1111/j.1460-9592.2006.01939.x. [DOI] [PubMed] [Google Scholar]
- 5.Schwartz D, Raghunathan K. The “Doppler-swoosh” test—a further modification to the “swoosh” test [letter] Paediatr Anaesth. 2007;17:600–1. doi: 10.1111/j.1460-9592.2006.02163.x. [DOI] [PubMed] [Google Scholar]
- 6.Tsui BC, Tarkkila P, Gupta S, Kearney R. Confirmation of caudal needle placement using nerve stimulation. Anaesthesiology. 1999;91:374–8. doi: 10.1097/00000542-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Chan SY, Tay HB, Thomas E. “Whoosh” test as a teaching aid in caudal block. Anaesth Intensive Care. 1993;21:414–5. doi: 10.1177/0310057X9302100407. [DOI] [PubMed] [Google Scholar]
- 8.Ghai B, Makkar JK, Behra BK, Rao KP. Is a fall in baseline heart rate a reliable predictor of a successful single shot caudal epidural in children? Paediatr Anaesth. 2007;17:552–6. doi: 10.1111/j.1460-9592.2006.02179.x. [DOI] [PubMed] [Google Scholar]


