Abstract
Context:
Snake bites are the common cause of morbidity and mortality in tropical countries.
Aims:
To analyze the outcome of snake bite victims
Settings and Design:
Retrospective analysis of data from Intensive care unit, Department of Anesthesiology.
Materials and Methods:
All the patients admitted in the intensive care unit for snake bite management during the year May 2004 - April 2009 were retrospectively reviewed. The data included age, sex, month and time of incident, site of bite, dose of anti--snake venom, time of anti--snake venom, administration, duration of mechanical ventilation, complications and death of a victim.
Statistical analysis used:
Pearson's correlation test, paired samples t-test.
Results and Conclusions:
113 patients reported to the Accident and Emergency with history of snake bite. 26 patients were referred to other hospital, 17 patients were brought dead, and 70 patients were admitted to the intensive care unit. In 59 snake-bite victims, maximum data could be recovered. Krait was the most common type of snake bite reported. There was a male preponderance (69.4%) with age ranging between 20 and 40 years (52.5%). The mean lag time (time elapsed between bite and first dose of anti--snake venom) was 5.3 ± 1.4 h and the mean anti-snake venom dose was 12.3 ± 2.4 vials. There was a positive and significant correlation between lag time and total dose of anti--snake venom (correlation coefficient =0.956, P<0.0001). Overall 72.9% patients required mechanical ventilation with a mean duration of 56.2 ± 16.1 h. 10.2% patients sustained cardiac arrest, 8.7% patients developed ventilator associated pneumonia, 6.7% suffered mild anti-snake venom reaction, 6.7% had hypotension and 5.1% patients developed renal failure. The overall mortality was 5.1%.
Keywords: Anti-snake venom, lag time, snake-bite
Introduction
Mortality after snakebites is preventable if the victim is treated without losing too much time. Every year 50,000 Indians die in 250,000 incidents of snakebite despite the fact that it is not the home of largest number of venomous snakes in the world, nor is there a shortage of anti--venom in the country. The main cause of this “unacceptable incidence” of snakebite fatalities is that people try out all kinds of “bizarre remedies” initially, instead of going to the nearest hospital.[1]
Even qualified doctors are at times not clear about symptoms and are unable to manage the snake bite cases properly. Anti--snake venom (ASV) is often needlessly administered, even when there is no need for it, which can result in more trauma as the antidote has severe side effects. Quite often it is not possible for a villager to get to a hospital within 10 min, which is necessary when methods such as pressure immobilization are used.[2,3]
Concerned about this situation, World Health Organization, in collaboration with leading Indian experts, is in the process of formulating a “National Protocol” for management of snakebites in India. Recently, Anil et al[4] reported a prospective study on eighty-nine patients with an effort to streamline the management of snake bite victims applicable to Indian scenario.
In India, the commonest type of snake bite is Elapid (cobra and krait) which cause neurotoxic envenomation and leads to muscle paralysis. Bungarotoxins present in neuroparalytic snake venom, blocks the pre-synaptic and post-synaptic acetylcholine receptors[5], depletes the synaptic vesicles at the synaptic sites[6] and cause structural damage of the motor end plate.[7] The polyvalent ASV can only neutralize the free-flowing snake venom but cannot reverse the block once the venom is attached to the receptors.[8] Respiratory failure has to be managed with ventilatory assistance for a variable period of time along with supportive measures despite administration of ASV[7,9].
The aim of this retrospective analysis was to evaluate the major factors that influenced the morbidity and mortality of snake bite victims admitted in a tertiary care hospital in Northern India.
Materials and Methods
The management of snake bite victims reported during the year May 2004 - April 2009 in the 65 bedded Accident and Emergency (A and E) unit and 8 bedded intensive care unit (ICU), was retrospectively reviewed. Ethical clearance was obtained from the Board of Studies of the Department of Anesthesiology for disclosure of the records which were purely for academic purpose. The data were collected from the record - keeping register maintained by the A and E nurses, ICU nurse and the central record - keeping section. Confidentiality of the patients was maintained by not mentioning the name, registration number, and date of birth of the patient. The patients were coded with an alphabet.
All the snake bite victims attending in the A and E were screened from the stored data, by one of the researchers, and recorded on an Excel sheet. Various parameters were then subsequently noted against each patient. Accordingly the data were initially recorded under three major groups:
Group 1: victims who were brought dead.
Group 2: victims who were referred to other hospitals because of unavailability of beds.
Group 3: victims who were managed in A and E and transferred to ICU.
Only data of patients of group 3, who were admitted to the ICU after the initial management in the A and E, were further analyzed for the following parameters-:
Number of patients admitted with history of snake bite
Number of patients developed cardiac or respiratory arrest in A and E or ICU
Site of bite
Visible bite mark present or absent
Type of snake bite
Time elapsed between the bite and ASV administration (lag time)
History of mild ASV reaction
Life threatening reactions developed after the ASV (hypotension and bronchospasm)
Total dose of ASV received
Average number of days mechanically ventilated
Morbidity developed during ICU stay (ventilator-acquired pneumonia, acute renal failure, etc.)
Mortality
Results
Over a period of 5 years, from May 2004 to April 2009, a total of 113 patients reported to the A and E with history of snake bite, of whom 17 patients were brought dead to the A and E, 26 patients were referred to other hospitals due to unavailability of beds and ventilators in the ICU, and 70 patients were admitted to the ICU. Maximum parametric and non--parametric data that could be recovered in every snake bite victims were recorded. Out of all the 70 patients admitted in the ICU, in 59 patients all the mentioned parameters could be retrieved. These patients were screened and analyzed.
Majority (36/59, 61.1 %) of snake bite victims reported during month of July to September. We divided patients on the basis of severity of snake bite [Table 1]. Out of 59 patients, 41 (69.4%) were male and 18 were female, their age ranged from 11 to 60 years with majority of patients in the age range of 20 – 40 years (31, 52.5 %) [Table 2 and Figure 1].
Table 1.
Classification of the severity of snake bite
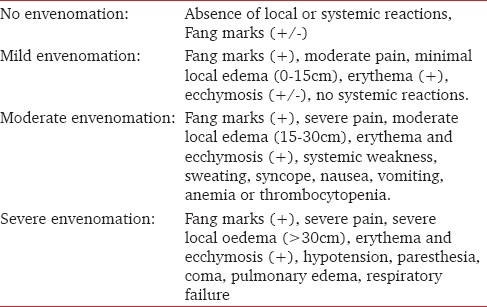
Table 2.
Annual incidences of snake-bite and the demographic data
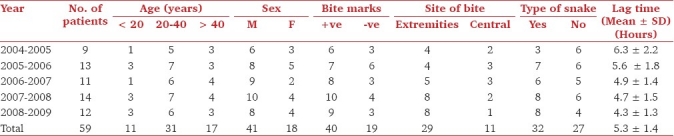
Figure 1.
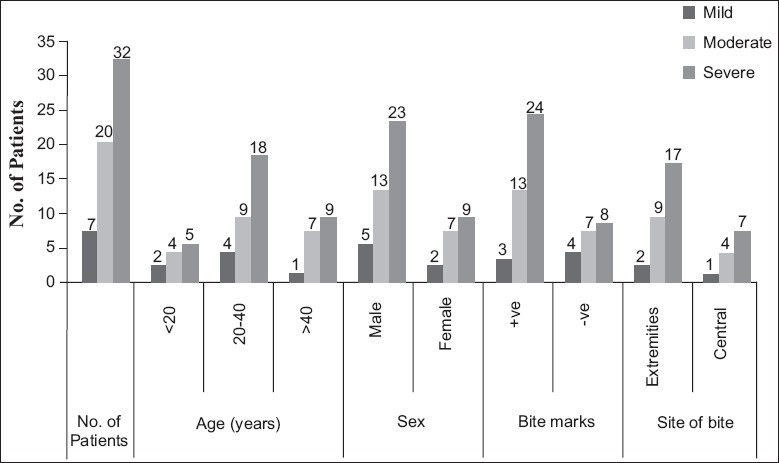
Distribution of patient according to the severity of envenomation
The bite mark was detected in 40 (67.8 %) victims. The type of snake was not identified in 27 (45.7 %) patients and in 32 (54.3%) it could be identified as Krait. Bite was recorded relatively more (72.5%) in the extremities (hand or feet) [Table 2, and Figure 1].
The time elapsed between snake bite and administration of first dose of ASV in A and E was calculated from the recorded time mentioned in the register and was considered as lag time. This time period ranged between 3 and 9 h approximately (mean ±SD was 5.3 ±1.4). The lag time gradually decreased from 2004 to 2009 (6.3 ± 2.2 in 2004to 4.3 ± 1.3 in2009, Table 2).
Majority (32/59, 54.2%) of the patients suffered severe envenomation of which 71.8% (23/32) were male, most of them in age range 20 – 40 years (18/32, 57.6%, Table 3). The lag time was slightly more in patients with mild envenomation in comparison to moderate and severe envenomation. The total dose of ASV ranged from 5 to 23 vials and the mean ± SD dose of ASV was (12.3 ± 2.4). ASV dose was significantly more in patients with severe envenomation (19.6 ± 3.2 vials) than in mild (6.7 ± 1.9) vials) and moderate (10.7 ± 2.1) vials) [Table 4, and Figure 2].
Table 3.
Distribution of patients according to the severity of envenomation
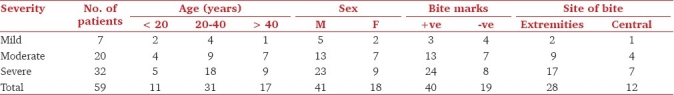
Table 4.
Comparison between the severity of bites in relation to lag time, duration of mechanical ventilation and ASV dose
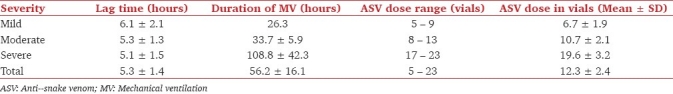
Figure 2.
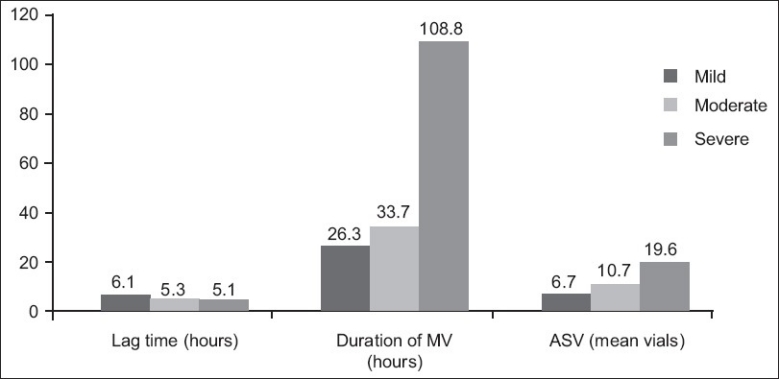
The comparison between the severity of bites in relation to lag time, duration of mechanical ventilation, and ASV dose with severity of snakebite
All the patients reported with ptosis. Overall 61.0% (36/59) patients required mechanical ventilation, of which 54.2 % (32/59) patients were with severe envenomation as compared to 5.84 % (3/59) and 1.7 % (1/59) patients with moderate and mild envenomation, respectively. The duration of mechanical ventilation ranged from 26 h to 150 h with a mean ± SD of 56.2 ± 16.1 h [Table 5, and Figure 3].
Table 5.
Incidences of complications according to the severity of envenomation
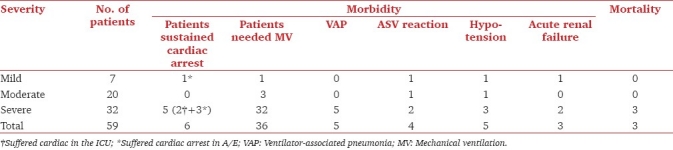
Figure 3.
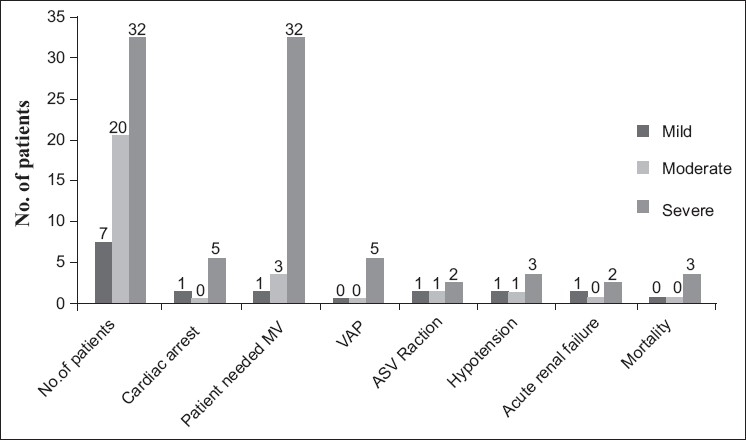
Incidences of complications according to the severity of envenomation
Cardiac arrest was recorded in 10.2% (6/59) victims of whom 6.7% (4/59) sustained cardiac arrest in the A/E, resuscitated and shifted to the ICU. 8.7% (5/59) victims developed ventilator- associated pneumonia, four (6.7%) suffered ASV reaction, five (8.5%) had hypotension and three (5.1%) victims developed renal failure. 3 (5.1%) out of 59 snake bite victims died. All the 3 victims suffered severe bite [Table 5, and Figure 3].
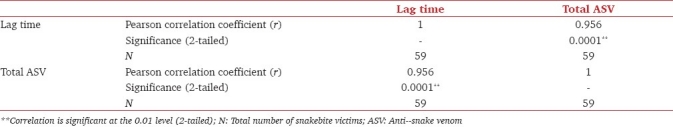
The Pearson correlation test was applied between lag time and total ASV dose required. Both were found to be positively correlated (Pearson correlation coefficient = 0.956). The relationship between the lag time and total ASV dose was found to be highly significant as the Pearson correlation was approaching 1 [Table 6].
Table 6.
The correlation between lag time and the total dose of ASV required
Discussion
In this retrospective review most of the victims were young adult male (69.4%) residing in the villages surrounding the district town. The male preponderance was similar to the findings of previous authors.[4,9] In India, men are the dominant earning member of the family. Working outdoors and sleeping in the farmyard during harvesting probably could be the cause of male preponderance. Further, in northern part of the country, agriculture labor mainly comprises of migrated men from other parts of the country.[4] They migrate without their family, reside in a dormitory accommodation, and sleep on the floor. Majority of the victims suffered neurotoxic envenomation. Most victims had a typical history of early morning bite while the victims were sleeping. The victims developed ptosis and blurring of vision on awakening. This is a classical history associated with krait bite probably because they are usually found near human habitat looking for their pray in the cracks of the houses.[4,10] Cobra also causes neurotoxic envenomation but their habitat is usually in the fields and they bite men working in fields.
The maximum incidence of snake bites was recorded during the months July to September. In Northern India monsoon usually arrives during these months. Flooding of the dwelling places of snakes force them to come out and cause accidental human victimization. Similar timing has been reported by the previous authors.[9,11,12]
Fang marks were not seen in 32.2% of patients despite positive history. This could be because most of the patients were victims of Krait. Krait has pin point teeth and even scratch can cause envenomation. Further, since there is generally no inflammation in krait bite so the identification of scratch mark might have been missed.[4]
The bite marks were mostly in the extremities of the body which was contrary to the finding of Kularatne,[10] Kulkarni and Anees,[11] and Sharma et al.[12] No definite reasons for this difference could be identified. However, it could be probably because most victims were bitten while sleeping. The slightest movement of their extremities during sleep might have been assumed as an attack on the snake by the victim and hence the snake counterattacked.
An interesting finding in this retrospective analysis was the lag time. The mean time taken by the patients, to arrive to the hospital was 6.3 ± 2.2 in 2004. Most of the previous studies in the literature are silent about the lag time other than Anil et al.,[4] Kularatne,[10] and Harsoor et al.,[13] who reported a time range from 0.5 to 10 h. However, in the later years (2009) the lag time in our study decreased to 4.3 ± 1.3. No definite reasons of this decrease could be identified. Better awareness about treatment of snake bite and awareness that such facility was available in the Medical College Hospital helped to reduce this. Instead of loosing time in bizarre remedies, victims were probably rushed to the hospital [Table 2].
The management of neurotoxic snake bite victim is primarily ASV administration along with mechanical ventilation as supportive therapy. According to the national protocol, the recommended initial dose is 10 vials (100 ml) of polyvalent ASV. If there is no improvement or deterioration in muscle power, this is followed by another 10 vials within 2 h (in all 20 vials). In addition to this, single dose of injection neostigmine along with atropine is administered.[14] The total dose of ASV administered in our patients ranged from 5 to 23 vials with a mean dose of 12.3 ± 2.4 vials. This was not in accordance to the national guideline for neurotoxic snake bite although the mean ASV dose was within the recommended range. The difference in the ASV administration schedule could be due to the absence of well - established national protocol in the early period of this retrospective study (2004 – 2006) and as per our institution protocol, during those days, the dose of ASV was based on the severity of bite.[15]
The mean dose of ASV administered in our patients was less than that of earlier studies. Harsoor et al.[13] reported a mean dose of 146 ml which was much less than that reported by Agarwal et al.[9] and Sharma et al.[12] Most of their victims probably suffered severe degree envenomation and therefore needed large doses of ASV. Further, the previous studies[9,12,13,16] were silent about the lag time. The lag time probably was long, resulting in more profound effect of snake venom and hence requiring large doses of ASV. Use of neostigmine to all our patients could be another reason.
Harsoor et al.[13] and Bomb et al.[16] recommend that administration of neostigmine probably could reduce the ASV requirement. However, Pawar and Singh[17] recommend that ASV and neostigmine should be avoided in victims with muscle paralysis. Anil et al.[4] did not find any improvement of muscle power in patients despite administering three doses of neostigmine at 30 min interval and were of the opinion that it does not have any role in pre-synaptic envenoming and may be avoided in established biting species. A number of studies[7,11,18] are silent regards the administration of neostigmine. All the patients received neostigmine empirically but the exact dose schedule could not be retrieved from the treatment records. No fixed protocol for neostigmine administration was found to have been followed in this analysis. No remark was documented regarding the improvement of motor function after the administration of neostigmine in the data available.
ASV administration was not devoid of complications. Adverse drug reactions were recorded infour patients. All the four patients suffered hypotension. Four patients, one with mild and three with severe degree envenomation suffered cardiac arrest in the A and E. These patients were revived successfully, but three of them subsequently developed acute renal failure.
Mechanical ventilation was required in 61.0% patients with its duration of ventilation ranging between 26 to 150 h. Kularatne[10] reported a duration ranging from 12 h to 29 days. Our finding was comparable with most of the previous studies,[9,10,11,12,13] but the duration was comparatively higher than that reported by Anil et al.[4] This could be probably because most of our patients had severe envenomation. Five patients developed ventilator-associated lung infection needing prolonged ventilator support. One patient with mild envenomation received mechanical ventilation because the patient had sustained a cardiac arrest. Three patients with moderate degree envenomation on admission subsequently developed severe symptoms and required mechanical ventilation [Table 5].
Six victims sustained cardiac arrest. All could be initially resuscitated but subsequently three (5.1%) victims expired because of multiple organ failure. All the three patients had severe envenomation [Table 5]. The incidence of mortality was similar to the previous authors.[4,10]
When analyzing the patients with severe envenomation it was observed that majority of the victims who had been bitten in the proximal parts of the body (head and neck) suffered from severe envenomation. This group of patients suffered from maximum complications (cardiac arrest, renal failure, and VAP) and had maximum mortality. These patients required maximum dose of ASV and prolonged mechanical ventilation [Table 4]. One patient, a snake charmer by profession was bitten on the tongue while demonstrating his tricks. He became unconscious and sustained cardiac arrest in the A and E.
Retrospective analysis was one of the major limitations of this study since some of the important data were incomplete or insufficient and might not reflect the exact statistics. However, the strengths of this retrospective review outnumbered the limitations. It identified the critical months, the common type of snake bite and the factors that influence the outcome of the victims. The hospital administration could incorporate necessary measures and be prepared during those months. An effective line of management, such as, the dose of ASV, neostigmine and ventilatory support could be laid down. Further, the findings of this analysis could enable the clinicians to emphasize the importance of early report to the hospital, avoidance of bizarre remedies and the risk in sleeping on the floor and in the farmyard.
To conclude, this retrospective review highlights that the outcome of neurotoxic snake bite victim was good if managed in time with ASV and ventilatory support. The outcome worsens in case of delay in treatment and in case the bite is more severe. Most of the victims can be managed well with ASV dose recommended in the national guidelines. Administration of neostigmine may be tried but its role is not well established.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Simpson ID, Norris RL. Snakes of Medical Importance in India: Is the Concept of the “Big 4” Still Relevant and Useful? Wilderness Environ Med. 2007;18:2–9. doi: 10.1580/06-weme-co-023r1.1. [DOI] [PubMed] [Google Scholar]
- 2.Norris RL, Ngo J, Nohan K, Hooker G. Physicians and lay people are unable to apply pressure immobilisation properly in a simulated snakebite scenario. Wilderness Environ Med. 2005;16:16–21. doi: 10.1580/PR12-04.1. [DOI] [PubMed] [Google Scholar]
- 3.Howarth DM, Southee AS, Whytw IM. Lymphatic flow rates and first aid in simulated peripheral snake or spider envenomation. Med J Australia. 1994;161:695–700. [PubMed] [Google Scholar]
- 4.Anil A, Singh S, Bhalla A, Sharma N, Agarwal R, Simpson ID. Role of neostigmine and polyvalent antivenom in Indian common krait (Bungarus caeruleus) bite. J Infect Public Health. 2010;3:83–7. doi: 10.1016/j.jiph.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 5.Mebs D, Claus I. Amino acid sequences and toxicities of snake venom components. In: Harvey AL, editor. Snake toxins. New York: Pergamon Press; 1991. pp. 425–47. [Google Scholar]
- 6.Chiappinelli VA. K-neurotoxins and α-neurotoxins: Effect on neuronal nicotinic acetylcholine receptors. In: Harvey AL, editor. Snake toxins. New York: Pergamon Press; 1996. pp. 223–58. [Google Scholar]
- 7.Dixon RW, Harris JB. Nerve terminal damage by β- bungarotoxin. Its clinical significance. Am J Pathol. 1999;154:447–55. doi: 10.1016/s0002-9440(10)65291-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Theakston RD, Phillips RD, Warrell DA, Galagade Y, Abeyseikera DT, Dissanayake P. Envenoming by the common krait (Bungarus caeruleus) and Srilankan cobra (Naja naja naja), efficacy and complication of therapy with Haffkine antivenom. Trans R Soc Trop Med Hyg. 1990;84:301–8. doi: 10.1016/0035-9203(90)90297-r. [DOI] [PubMed] [Google Scholar]
- 9.Aggarwal PN, Aggarwal AN, Gupta D, Behera D, Prabhakar S, Jindal SK. Management of respiratory failure in severe neuroparalytic snake envenomation. Neurol India. 2005;49:25–8. [PubMed] [Google Scholar]
- 10.Kularatne SA. Common krait (Bungarus Caeruleus) bite in Anuradhapura, Sri Lanka - a prospective clinical study 1996-98: Postgrad Med J. 2002;78:276–80. doi: 10.1136/pmj.78.919.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kulkarni ML, Anees S. Snake venom Poisoning, experience with 633 patients. Indian Paediatr. 1994;31:1239–43. [PubMed] [Google Scholar]
- 12.Sharma N, Chauhan S, Faruqi S, Bhatt P, Varma S. Snake envenomation in north Indian hospital. Emerg Med J. 2005;22:118–20. doi: 10.1136/emj.2003.008458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harsoor SS, Gurudatta CL, Balabhaskar S, Kiranchand N, Bhosale R. Ventilatory managent of patient with neuroparalytic envenomation. Indian J Anaesth. 2006;50:452–5. [Google Scholar]
- 14.National snake bite protocol. New Delhi: Health and Family Welfare Department; 2007. Government of India. [Google Scholar]
- 15.Ahmed SM, Ahmed M, Nadeem A, Mahajan J, Choudhary A, Pal J. Emergency management of snake bite – Pearls from literature. J Emerg Trauma Shock. 2008;1:97–105. doi: 10.4103/0974-2700.43190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bomb BS, Roy S, Kumawat DC, Bharjatya M. Do we need anti snake venom (ASV) for management of elapid ophitoxaemia. J Assoc Physicians India. 1996;44:31–3. [PubMed] [Google Scholar]
- 17.Pawar DK, Singh H. Elapid snake bite. Br J Anaesth. 1987;59:385–7. doi: 10.1093/bja/59.3.385. [DOI] [PubMed] [Google Scholar]
- 18.Seneviratne U, Dissanayake S. Neurological manifestations of snakebite in Sri Lanka. J Postgrad Med. 2002;48:275–8. [PubMed] [Google Scholar]


