Abstract
The oral cavity appears as an open ecosystem, with a dynamic balance between the entrance of microorganisms, colonization modalities, and host defenses aimed to their removal: To avoid elimination, bacteria need to adhere to either hard dental surfaces or epithelial surfaces. The oral biofilm formation and development, and the inside selection of specific microorganisms have been correlated with the most common oral pathologies, such as dental caries, periodontal disease, and peri-implantitis. The mechanical removal of the biofilm and adjunctive use of antibiotic disinfectants or various antibiotics have been the conventional methods for periodontal therapy. Ozone (O3) is a triatomic molecule, consisting of three oxygen atoms, and its application in medicine and dentistry has been indicated for the treatment of 260 different pathologies. The ozone therapy has been more beneficial than present conventional therapeutic modalities that follow a minimally invasive and conservative application to dental treatment. The exposition of molecular mechanisms of ozone further benefits practical function in dentistry.
Keywords: Biofilm, dental, ozone
INTRODUCTION
Periodontitis is a destructive inflammatory disease of the supporting tissues of the teeth and is caused either by specific microorganisms or by a group of specific microorganisms, resulting in progressive destruction of periodontal ligament and alveolar bone with periodontal pocket formation, gingival recession, or both.[1] Bacteria are the prime etiological agents in periodontal disease, and it is estimated that more than 500 different bacterial species are capable of colonizing the adult mouth[2] and the lesions of the oral cavity have an immense impact on the quality of life of patient with complex advance diseases.[3] Periodontitis has been proposed as having an etiological or modulating role in cardiovascular and cerebrovascular disease, diabetes, respiratory disease and adverse pregnancy outcome and several mechanisms have been proposed to explain or support such theories.[4] The oral cavity appears as an open ecosystem, with a dynamic balance between the entrance of microorganisms, colonization modalities and host defenses aimed to their removal: To avoid elimination, bacteria need to adhere to either hard dental surfaces or epithelial surfaces. The oral biofilm formation and development, and the inside selection of specific microorganisms have been correlated with the most common oral pathologies, such as dental caries, periodontal disease and peri-implantitis.[5] The cooperative communal nature of a microbial community provides advantages to the participating microorganisms. These advantages include a broader habitat range for growth, an enhanced resistance to antimicrobial agents and host defence, and an enhanced ability to cause disease.[6] Dental biofilm pathogenicity in the oral cavity is magnified by two biofilm characteristics: Increased antibiotic resistance and the inability of the community to be phagocytized by host inflammatory cells.[7] The mechanical removal of the biofilm and adjunctive use of antibiotic disinfectants or various antibiotics have been the conventional methods for periodontal therapy.[8,9] As the periodontal researchers is looking for alternatives to antibiotic treatments (biofilm resistance), the emergence of ozone therapy seems to be a promising future.
History
In 1839, Christian Friedrich Schonbein, first noticed the emergence of a pungent gas with an electric smell. According to the Greek language, he called it ozone and presented a lecture entitled “On the smell at the positive electrode during electrolysis of water” at the Basel Natural Science Society.[10] Oxygen/ozone therapy has a long history of research and clinical application with humans. The first medical application was in 1870 when Dr. C. Lender purified blood in test tubes. Medical applications became widespread throughout Europe and America. As of 1929, more than 114 diseases were listed for treatment with oxygen/ozone therapy. Interestingly enough, in 1930, a German dentist, Dr. E.A. Fisch, used ozone on a regular basis in his dental practice in Zurich, Switzerland, and published numerous papers on the subject.
Ozone therapy: Chemistry and apparatus
Ozone (O3) is a triatomic molecule, consisting of three oxygen atoms. Its molecular weight is 47, 98 g/mol and thermodynamically highly instable compound that, dependent on system conditions like temperature and pressure, decompose to pure oxygen with a short half-life.[11] Ozone is 1.6-fold denser and 10-fold more soluble in water (49.0 mL in 100 mL water at 0° C) than oxygen. Although ozone is not a radical molecule, it is the third most potent oxidant (E_ 5 12.076 V) after fluorine and per sulfate. Ozone is an unstable gas that cannot be stored and should be used at once because it has a half-life of 40 min at 20 °C.[12] Ozone (O3) is naturally produced by the photo dissociation of molecular oxygen (O2) into activated oxygen atoms, which then react with further oxygen molecules. This transient radical anion rapidly becomes protonated, generating hydrogen trioxide (HO3), which, in turn, decomposes to an even more powerful oxidant, the hydroxyl radical (OH). It is the fundamental form of oxygen that occurs naturally as a result of ultraviolet energy or lightning, causing a temporary recombination of oxygen atoms into groups of three. In the clinical setting, an oxygen/ozone generator simulates lightning via an electrical discharge field. Ozone gas has a high oxidation potential and is 1.5 times greater than chloride when used as an antimicrobial agent against bacteria, viruses, fungi, and protozoa. It also has the capacity to stimulate blood circulation and the immune response. Such features justify the current interest in its application in medicine and dentistry and have been indicated for the treatment of 260 different pathologies.[13]
Applications
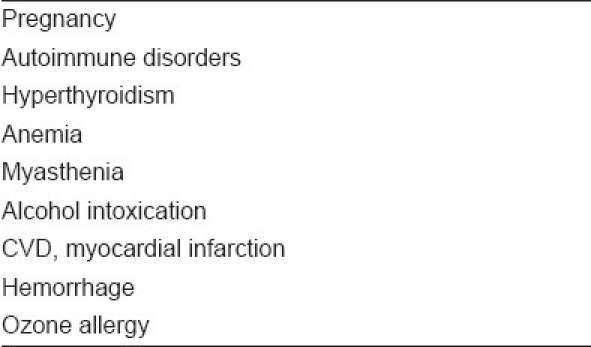
The potential application of ozone therapy in human body and its biological horizons are listed in Table 1. Antimicrobial effect of ozone is the most studied. Oxygen/ozone therapy in dentistry contains a multiplicity of protocols to deal with dental infection. Three fundamental forms of application to oral tissue are applied — (1) ozonated water, (2) ozonated olive oil, and (3) oxygen/ozone gas. Ozonated water and olive oil have the capacity to entrap and then release oxygen/ozone, an ideal delivery system. These forms of application are used singly or in combination to treat dental disease. The different clinical application of ozone therapy in combating the dental disease and their treatment modalities are listed in Table 2. The ozone therapy has also certain limitations and contraindications as listed in Table 3.
Table 1.
Potential applications of ozone therapy

Table 2.
Dental treatment modalities of ozone therapy

Table 3.
Contraindications of ozone therapy
CONCLUSION
In contrast with traditional medicine modalities such as antibiotics and disinfectants, ozone therapy is quite economical; it will markedly reduce both medical cost and invalidity. Dentistry is varying with induction of modern science to practice dentistry. The ozone therapy has been more beneficial than present conventional therapeutic modalities that follow a minimally invasive and conservative application to dental treatment. The exposition of molecular mechanisms of ozone further benefits practical function in dentistry. Treating patients with ozone therapy lessens the treatment time with an immense deal of variation and it eradicates the bacterial count more specifically. The treatment is painless and increases the patients’ tolerability and fulfillment with minimal adverse effects. Contraindications of this controversial method should not be forgotten. Further research is needed to regulate indications and treatment procedures of ozone therapy.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Saini R, Saini S, Sharma S. Periodontal disease linked to cardiovascular disease. J Cardiovasc Dis Res. 2010;1:161–2. doi: 10.4103/0975-3583.70925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saini R, Marawar PP, Shete S, Saini S. Periodontitis a true infection. J Global Infect Dis. 2009;1:149–51. doi: 10.4103/0974-777X.56251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saini R, Marawar PP, Shete S, Saini S, Mani A. Dental expression and role in palliative treatment. Indian J Palliat Care. 2009;15:26–9. doi: 10.4103/0973-1075.53508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saini R, Saini S, Sharma S. Periodontitis: A risk factor to respiratory diseases. Lung India. 2010;27:189. doi: 10.4103/0970-2113.68313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bortolaia C, Sbordone L. Biofilms of the oral cavity. Formation, development and involvement in the onset of diseases related to bacterial plaque increase. Minerva Stomatol. 2002;51:187–92. [PubMed] [Google Scholar]
- 6.Marsh PD. Dental plaque: Biological significance of a biofilm and community life-style. J Clin Periodontol. 2005;32:7–15. doi: 10.1111/j.1600-051X.2005.00790.x. [DOI] [PubMed] [Google Scholar]
- 7.Thomas JG, Nakaishi LA. Managing the complexity of a dynamic biofilm. J Am Dent Assoc. 2006;137:10–5. doi: 10.14219/jada.archive.2006.0409. [DOI] [PubMed] [Google Scholar]
- 8.Walker CB. The acquisition of antibiotic resistance in the periodontal micro flora. Periodontol 2000. 1996;10:79–88. doi: 10.1111/j.1600-0757.1996.tb00069.x. [DOI] [PubMed] [Google Scholar]
- 9.Feres M, Haffajee AD, Allard K, Som S, Goodson JM, Socransky SS. Antibiotic resistance of sub gingival species during and after antibiotic therapy. J Clin Periodontol. 2002;29:724–35. doi: 10.1034/j.1600-051x.2002.290809.x. [DOI] [PubMed] [Google Scholar]
- 10.Stübinger S, Sader R, Filippi A. The use of ozone in dentistry and maxillofacial surgery: A review. Quintessence Int. 2006;37:353–9. [PubMed] [Google Scholar]
- 11.Burns DT. Early problems in the analysis and the determination of ozone. Fresenius J Anal Chem. 1997;357:178–83. [Google Scholar]
- 12.Bocci VA. Scientific and Medical Aspects of Ozone Therapy: State of the Art. Arch Med Res. 2006;37:425–35. doi: 10.1016/j.arcmed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 13.Nogales CG, Ferrari PH, Kantorovich EO, Lage-Marques JL. Ozone therapy in medicine and dentistry. J Contemp Dent Pract. 2008;9:75–84. [PubMed] [Google Scholar]


