Abstract
Estrogen deficiency is a major risk factor for osteoporosis in postmenopausal women. Although hormone replacement therapy (HRT) has been rampantly used to recompense for the bone loss, but the procedure is coupled with severe adverse effects. Hence, there is a boost in the production of newer synthetic products to ward off the effects of menopause-related osteoporosis. As of today, there are several prescription products available for the treatment of postmenopause osteoporosis; most of these are estrogenic agents and combination products. Nevertheless, in view of the lack of effect and/or toxicity of these products, majority of the postmenopausal women are now fascinated by highly publicized natural products. This is an offshoot of the generalized consensus that these products are more effective and free from any adverse effects. Recently, certain plant-derived natural products, mostly phytoestrogens (isoflavones, lignans, coumestanes, stilbenes, flavonoids) and many more novel estrogen-like compounds in plants have been immensely used to prevent menopause-related depletion in bone mineral density (BMD). Although, a number of papers are published on menopause-related general symptoms, sexual dysfunction, cardiovascular diseases, Alzheimer's disease, diabetes, colon, and breast cancers, there is paucity of literature on the accompanying osteoporosis and its treatment. In view of the controversies on synthetic hormones and drugs and drift of a major population of patients toward natural drugs, it was found worthwhile to investigate if these drugs are suitable to be used in the treatment of postmenopausal osteoporosis. Preparation of this paper is an attempt to review the (a) epidemiology of postmenopausal osteoporosis, (b) treatment modalities of postmenopausal osteoporosis by hormones and synthetic drugs and the associated drawbacks and adverse effects, and (c) prevention and treatment of postmenopausal osteoporosis by phytoestrogens, their drawbacks and toxicity. It is apparent that both the categories of treatment are useful and both have adverse effects, but the plant products are nonscientific and hence are not advised to be used till more studies are undertaken to ensure that the benefits clearly outweigh the risk, in addition to recognition by Food and Drug Administration.
Keywords: Menopause, osteoporosis, phytoestrogens
INTRODUCTION
Hormonal changes in a woman's body are conspicuous by the beginning of fertility at puberty with the onset of first menstrual bleeding and ending at menopause. The average age for the onset of the menopause is 45-51 and it is defined as having taken place when the woman completes 12 menstrual cycles without any menstrual bleeding. Following menopause, the ovaries stop producing estrogen, a hormone that helps prevent bone loss. The estrogen deficiency is known to cause significant alterations in bone metabolism. Some people may develop osteopenia, a condition characterized by low bone density. Osteopenia can eventually lead to osteoporosis, a more severe condition with lower bone density. Threat of osteoporosis is one of the most important health issues for menopausal women. Menopause, coupled with hypogonadism in women, strongly predisposes them to osteoporosis.[1] The condition apparently diminishes the quality of life in this population and gives rise to severe morbidity. In osteoporosis, the bones become thin, fragile, and highly prone to increase in the frequency of fractures.[2–4] Although osteoporosis-related bone fractures during postmenopause can occur in almost any skeletal bone, the most common are a compression fracture of the vertebrae in the spine and fractures of the spine, ribs, hip, and wrists.[5]
To compensate the bone loss due to deficiency of estrogen in postmenopausal women, hormone replacement therapy (HRT) has been the major therapeutic approach. Nevertheless, HRT has been considered as an unfavorable procedure due to its nonavailability to poor and the rural masses and severe adverse effects. Hence, to recompense the estrogen deficiency and manage the related osteoporosis, there is an uprising in the production of synthetic drugs and hormonal preparations to fend off the adverse effects of menopause-related osteoporosis. However, these products are not very popular among majority of the women, in view of their deficient impact on the target and known adverse effects including malignancy. Hence, these women are now enthralled by the extremely publicized natural products to prevent menopause-related depletion in bone mineral density (BMD).
Although, a number of papers are published on menopause-related symptoms (climacteric syndrome, hot flashes, loss of libido, vaginal dryness and atrophy, pain in intercourse, mood disturbance or emotional instability, depression, sleep disturbances, memory loss cognitive decline sexual dysfunction, cardiovascular diseases, Alzheimer's disease, diabetes, colon, and breast cancers,[6–9] there is paucity of literature on the accompanying osteoporosis. This paper is an attempt to review the (a) epidemiology of postmenopausal osteoporosis, (b) treatment modalities of postmenopausal osteoporosis by hormones and synthetic drugs and the associated drawbacks and adverse effects, (c) treatment of postmenopausal osteoporosis by phytoestrogens, their drawbacks and toxicity, and finally (d) the individual merits.
METHODOLOGY
Published articles selected for inclusion in this review were based on the significance, and understanding of research on different hormones used to cure bone diseases in postmenopausal women. To meet this requirement, Pub Med, Pub Med Central, Science Direct, Uptodate, Med Line, Natural Medicines Comprehensive databases, International Pharmaceutical Abstracts, Cochrane library, the International Bibliographic Information on Dietary Supplements, the Cumulative Index to Nursing and Allied Health, and Herb Med and the internet were thoroughly searched, using terms that included the title with their relevant physiological and biochemical aspects. Although some older articles that were decisive in evolving the current understanding of osteoporosis and endocrinology were difficult to be dispensed with, but most of the references used are from articles which were published during last 10-15 years.
EPIDEMIOLOGY OF POSTMENOPAUSAL OSTEOPOROSIS
It is estimated that majority of the postmenopausal women get osteoporotic at the hip, lumbar spine and wrist or forearm with advancement in age.[10] Extensive differences in the epidemiological pattern of osteoporosis among geographic and ethnic groups have been reported,[11] but there is lack of information about the incidence of postmenopausal osteoporosis and related protective and risk factors in developing countries. Nevertheless, most available data in the literature are from western countries.
More than half of postmenopausal women in western countries lived in rural areas. The incidence of obesity, hypertension, hypothyroidism, diabetes, and osteoporosis was found to be more in these women due to a particular style of life they live.[12] It is estimated that 10 million Americans >50 years old have osteoporosis and approximately 34 million are at risk of the disease.[10] The incidence of fragility fractures is estimated to be 1.5 million per year. Most of the American women under the age of 50 have normal BMD. However, between 35-50% of women over 50 have at least one vertebral fracture.[13,14] By the age of 80 years, 27% are osteopenic and 70% are osteoporotic at the hip, lumbar spine or forearm,[10,13] and wrist fractures are the third most common type of osteoporotic fracture. These fractures are about 20% in women who have reached 70 years of age.[13] The incidence of osteoporosis in Northern European countries is very high. The incidence of hip fractures is common among women who have reached their 65th year of age. Majority of the incidents are associated with climate, which limits physical activity and exposure to sunlight. Nevertheless, despite the increased incidence of osteoporosis, strict preventive measures are not being adopted.[15] Among the postmenopausal Mexican women, the prevalence of lumbar spine and/or hip has been related to osteoporosis beyond the age of 50 years. However, it is reported to be much lower than those reported for Caucasian women (30%).[16] Furthermore, it was found that women are prone to osteoporosis two to three times more than men, due to lower “peak” bone mass and the accelerated loss that occurs after the menopause.
In a study on vertebral osteoporosis on German residents, Raspe et al.[17] have shown that the prevalence of back-, neck- and joint-pain is consistently higher in females than in males in all age groups. The prevalence in postmenopausal females (55-64) showed a peak. The total number of osteoporotic fractures in the Czech Republic is close to that in the developed western countries. The fractures of vertebrae and of the proximal femur are common.[18]
The incidence of osteoporosis is reported in 1/3 of the Turkish postmenopausal women. The different etiological factors were habitual tea, coffee, tobacco, and milk product consumption. Advanced age (> 65) and being illiterate were negative factors, while high education levels, being overweight, and being treated with HRT had a positive effect on BMD.[19] A study on the influence of educational level on BMD in Turkish postmenopausal women revealed that there is a significant correlation between educational level and BMD. Losses in BMD for women of lower educational level tend to be relatively high, and losses in spine and femur BMD showed a decrease with increasing educational level.[20] In a study on Caucasian premenopausal women, Gulbahar et al.[21] reported that the women with joint hyper mobility have lower BMD when compared to the controls and hyper mobility increases the risk for low bone mass.
Osteoporosis with postmenopause in Jordanian women is extremely high, and is even found in younger age categories. The age, years of menopause, low-density lipoprotein and follicle-stimulating hormone have strong independent associations with BMD at all lumbar and femoral neck regions. It is also reported that these women experience many potential risk factors including associated medical illnesses, and other hormonal alterations experienced during menopausal period. Therefore, increased health awareness and intensive screening programs are mandatory for early detection of low bone mass.[11] There were smaller postmenopausal decreases in femoral and radial BMD in Lebanese women compared with US/European women.[22] The prevalence of osteoporosis in Israel among postmenopause women (aged 45-74) is estimated to be 13.7%, which is similar to that for the United States. The association of osteoporosis with risk factors is age dependent.[23] The Jewish Menopausal women were more knowledgeable and showed great interest in physical activities.[24]
The exact age of menopause in African women is not known, but it is reported to occur earlier than European or American women. Although, multiple parity in a short period of time is the main reason, but social, economic, and nutritional factors may also influence the biological pattern.[25] The Egyptian women are shown to get menopause at 46 years approximately, which is low compared to many countries. Generally, they have a lower BMD compared to western women. Most of them suffer from osteoporosis after menopause, which is regarded by them as “just a physiological change”. There exists a need for an awareness campaign in order to educate them about this important stage of their lives.[26] The approximate age at menopause in women from Kenya is shown to be 48 years. However, a review of the current and past records show that the average age of menopause in women of Kenya, has remained relatively constant at 50 years, but almost all women are menopausal before they reach 55. Clinical symptoms include osteoporosis and increased incidence of bone fractures, in addition to other general symptoms of menopause.[27]
The age of menopause in Saudi women is 48 years approximately. This is similar to other Arab countries, but lower than western countries. This may be due to cultural differences, in addition to the role of genetics. Although, the incidence of osteoporosis is common among postmenopausal Saudi women, it is often associated with either, early or late onset of menopause.[28] Sadat-Ali et al.[29] found that osteoporosis and osteopenia are common (60%) among postmenopausal Saudi Arabian women. The causative factors are pregnancy, multiparity, and prolonged lactation. In a study on the prevalence of vertebral fractures in postmenopausal women in Saudi Arabia, Sadat-Ali et al.[30] showed that the mean age of the women getting the fractures was around 65. The reported incidence varies between 50-60% in Al-Khobar, an Eastern region of the Kingdom of Saudi Arabia. The results indicated that postmenopausal Saudi women in Alkhobar suffer from osteoporosis and osteopenia higher than those from other parts of the country.[31]
In Iran, regular consumption of cheese, milk, chicken, egg, fruit, consumption of tea, HRT and calcium supplements were found to be significant protective factors, while steroid therapy and consumption of red meat were the prominent risk factors for postmenopausal osteoporosis.[32] The average age for Indian women to get menopause is between 40-41 years, which is much earlier than the women in Egypt, Saudi Arabia and western countries. Most of the Indian women are from low-income groups and hence consume diets that have inadequate calories, proteins and micronutrients. Furthermore, the nourishment lacks calcium supplementation. Hospital-based data suggest that these women have osteoporotic hip fractures at a much earlier age than western women.[33] Regular consumption of soya, almonds, fish, fruits and milk tea appeared to be significant protective factors in India. Furthermore, pure vegetarianism in India was reported as one of the risk factors for osteoporosis among postmenopausal women.[32] In a tropical country, such as Thailand, women showed different age-related changes in bone metabolism.[34] The age-specific prevalence of osteoporosis among Thai women rose progressively with increasing age to more than 50% after the age of 70.[35]
There are some studies on comparison of postmenopausal osteoporosis between different countries. The available literature has depicted limited and scattered information on Asian and western populations, Jewish and Arab women and Iranian and Indian women. In a study on comparison of osteoporosis between Asian and western populations, Huang[36] found that the awareness and use of HRT among Asians were significantly low. A comparison between the Jewish and Arab menopausal women showed less concern for physical activity and calcium intake among the Arab women, while the Jewish menopausal women were more knowledgeable and show great interest in physical activities. However, expanding knowledge about osteoporosis may prove beneficial for increasing participation in preventive behavior in both Israeli-Jewish and Arab women groups.[24] There were no significant differences in association of risk factors and osteoporosis between Iranian and Indian subjects. A protective role of certain nutritional dietary components and also exercises are reported in both populations. These attributes can be exploited in preventive educational strategies on osteoporosis in both the countries. Consumption of red meat and steroid therapy in Iran and pure vegetarianism in India were observed to be risk factors in these two countries. The different protective factors were regular consumption of cheese, milk, chicken, egg, fruit, consumption of tea, in addition to calcium consumption and HRT in Iran, while in India the protective factors were regular consumption of Soya, almonds, fish, fruits and milk tea.[32]
TREATMENT OF POSTMENOPAUSAL OSTEOPOROSIS BY HORMONES AND SYNTHETIC DRUGS
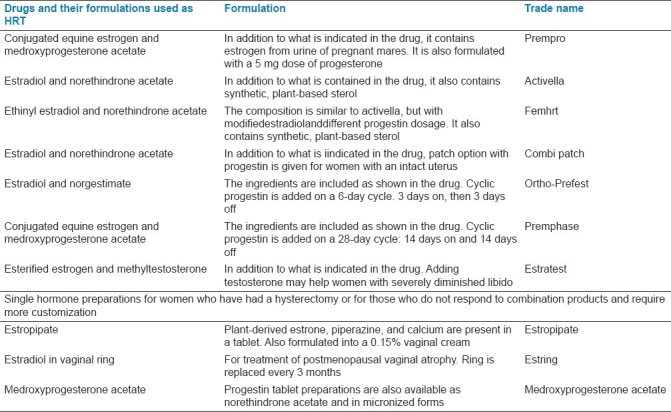
With the advent of menopause, the levels of reproductive hormones fluctuate causing the symptoms of menopause including osteoporosis. These symptoms are regulated by HRT in the form of medication. Most of the hormones prescribed for HRT include estrogen, progestin, progesterone, testosterone in different combination products such as prempro, activella, femhrt, combi patch, ortho-prefest, premphase, estratest, estropipate, estring, medroxyprogesterone acetate.[37] (The generic names and formulation of these drugs[37] are detailed in Table 1. Treatment with estrogens blocks the osteoclastic resorption and conserves the bone mass. Anabolic hormones, including progesterone, stimulate osteoblastic building of bone. The combination of estrogen and progesterone is known to lower the risk of uterine malignancy, besides curing the osteoporosis. In addition to estrogen therapy and progesterone replacement, the victims of fracture may benefit from androgen replacement to increase their bone mass. Furthermore, replacing androgens using nandrolone decanoate in women may cure the natural loss of their adrenal hormones.[38] There is an increase in the potential role for androgen supplementation in postmenopausal health. Androgen replacement is reported to provide additional relief of menopausal symptoms with a positive impact on bone density.[39] The HRT has been rampantly used to recompense for the bone loss, but the procedure is coupled with severe adverse effects. Hence, there is a boost in the production of newer synthetic products to ward off the effects of menopause-related osteoporosis.
Table 1.
List of HRT medications and their formulations
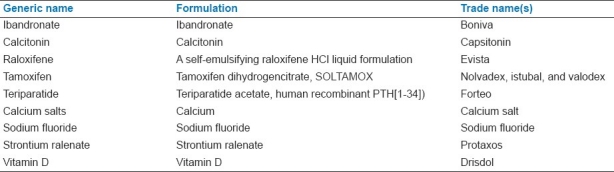
As of today, there are several prescription products available for the treatment of postmenopause osteoporosis. The different prescription products [Table 2] that are given wide publicity include antiresorptive agents (bisphosphonates, ibandronate, calcitonin and selective estrogen receptor modulators -- SERMs (raloxifene, tamoxifen), bone anabolic agents (teriparatide, calcium salts, sodium fluoride) and some other agents (RANKL inhibitors, strontium ralenate; nutrition (calcium, vitamin D).[40–44] Bisphosphonates and strontium ralenate are good choices for first- or second-line treatment and estrogen/progestin is no longer a first-line approach for the treatment of osteoporosis in postmenopausal women.[45] SERMs are defined as a group of compounds that behave both like estrogen agonists in some tissues and antagonists in other tissues,[46] while parathyroid hormone is used for the second-line treatment of osteoporosis in the elderly.[47]
Table 2.
Synthetic or extracted products used to compensate HRT
ADVERSE EFFECTS AND DRAWBACKS OF HORMONES AND SYNTHETIC DRUGS
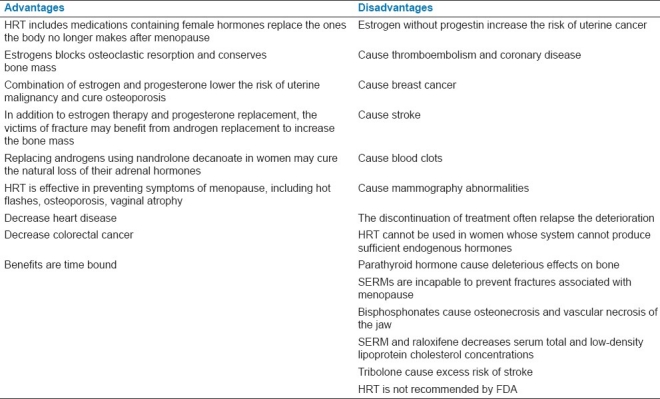
Although HRT and synthetic hormones are shown to recompense for the depletion of the hormone and to impede the bone loss, the treatment is controversial and has been associated with a number of complications and adverse effects.[48–53] The major toxicity of hormones is their carcinogenic potential. This et al.[54] reported that estrogens promote the growth of malignant cells. No authors listed[55] interpreted that the risk of breast cancer is increased in women using HRT; the incidence is directly proportional to the duration of use. The benefits derived from the synthetic hormones are time bound; the discontinuation of treatment often relapse the deterioration.[56] Moreover, the therapy is not advised in case menopausal women who are unable to produce sufficient natural hormones. Estrogen-progestin therapy in treatment of osteoporosis in postmenopausal women caused increased risk of breast cancer, stroke, venous thromboembolism, and coronary disease.[45] Parathyroid hormone is discouraged because of its deleterious effects on bone.[57] SERMs are reported to be incapable to prevent fractures associated with menopause.[58] Bisphosphonate therapy is shown to cause osteonecrosis and a vascular necrosis of the jaw. Tissue SERM, Raloxifene, decreases serum total and low-density-lipoprotein cholesterol concentrations.[57] Although it is known to reduce breast cancer risk, it increases thromboembolic events and hot flashes.[59] Tibolone is a synthetic steroid whose metabolites have estrogenic, androgenic, and progestagenic properties. It is used in the management of osteoporosis in some countries; however, it was discontinued early due to an excess risk of stroke.[60] Because of the reported carcinogenic potentials of hormones and the adverse effects of synthetic drugs, majority of the postmenopausal women were reluctant to be exposed to exogenous hormones and toxic drugs and are shifting to natural products (importantly, phytoestrogens) for relief.[45,61] The advantages and disadvantages of HRT and synthetic drugs are presented in Table 3.
Table 3.
Advantages and disadvantages of hormone replacement therapy and synthetic drugs
TREATMENT OF POSTMENOPAUSAL OSTEOPOROSIS BY PHYTOESTROGENS
Phytoestrogens are plant-derived polyphenol compounds that show a structural similarity to steroid hormone (17-beta-estradiol). Although phytoestrogens are not as potential as the endogenous estrogens, they are widely self-prescribed against the treatment of menopause and postmenopausal osteoporosis and are considered safe and beneficial throughout the world.[62,63] Most of the flavonoids (isoflavones) are classified as phytoestrogens, based on their ability to mimic estrogen.[64] The classical phytoestrogens constitute a group of compounds (isoflavones, lignans, coumestanes, stilbenes, flavonoids quercetin and kaempherol) of plant origin [Table 4].
Table 4.
List of plants and herbs used to compensate HRT
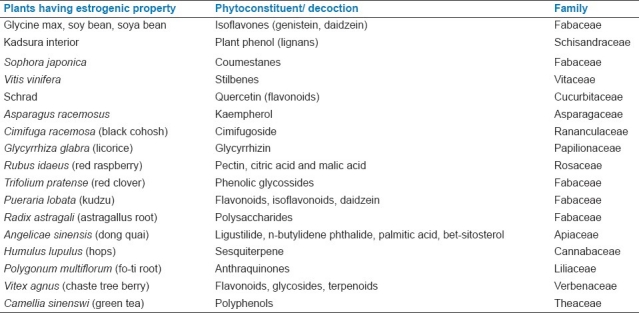
Isoflavones are natural endocrine active phytoestrogens found in Leguminosae and are generally considered to prevent osteoporosis by promoting bone health. Exposure to these products is through soy foods and soy protein, in addition to processed foods or through supplements.[65] They may be useful as dietary alternative or supplement to postmenopausal HRT, because of their beneficial effects on atherosclerosis and cancer risk.[66] Soy isoflavones are structurally and functionally related to 17-beta-estradiol and are known to act on both osteoblasts and osteoclasts through genomic and nongenomic pathways and have beneficial effects on BMD, bone turnover markers, and bone mechanical strength in postmenopausal women.[65,67] The effect of isoflavones on bone formation is by binding on estrogen receptors on the target cell surface; hence it is believed that isoflavones may help in the treatment of patients by estrogen replacement therapy for osteoporosis.[68]
Genistein and daidzein are the other isoflavones of soy that have been shown to conserve bone in ovariectomized rodent models and probably have similar conservatory effects in higher mammalian species.[69] Hooshmand et al.[70] reported genistin-rich isoflavones to prevent loss of BMD in the rat model of ovaridectomy. Isoflavone-containing soy intake was found to physiologic fluctuations in bone turnover, thereby preventing osteoporosis, in addition to protection against breast cancer and cardiovascular diseases.[71] [Table 4]
There are yet some other plants (black cohosh, licorice, red raspberry, red clover, and kudzu) that contain phenolic compounds and are suggested to have estrogenic potential for relieving menopausal symptoms.[72] In a study to assess the estrogen bioactivity of some herbs, Oerter Klein et al.[73] found that soy, clover, licorice, hops, and fo-ti to have high estrogen activity, while chaste tree berry, black cohosh and dong quai did not have measurable estrogen activity. They further found that removal of the glycone group from soy increases its estrogen bioactivity significantly. Many more novel estrogen-like compounds in the plant kingdom are being discovered, thus expanding the spectrum of phytoestrogens in nature.[74,75] Danggui Buxue Tang, a Chinese medicinal decoction containing Radix astragali and Radix angelicae sinensis, was found to stimulate osteoblast proliferation, estrogen promoter activation, in addition to increasing the anti-platelet aggregation activity.[76] Red clover (Trifolium pratense), a phytoestrogen is shown to improve deteriorating bone health during menopause. It was also found to improve arterial compliance, a risk factor for atherosclerosis.[77] Whelan et al.[78] showed natural health products to prevent and treat osteoporosis in postmenopausal women. Das et al.[79] found that the supplementation of the phytoestrogen (Camellia sinensi) showed a significant improvement in the markers of osteoporosis, such as bone resorption and osteoclastic activity, collagen degradation, bone loss, and bone density [Table 4].
ADVERSE EFFECTS AND DRAWBACKS OF PHYTOESTROGENS
Laboratory studies in animals showed that the treatment with phytoestrogens (soy isoflavones) has serious adverse effects.[80] The extensive use of supplemental phytoestrogens is shown to cause grade 1 endometrioid adenocarcinoma of the endometrium.[81] McLachlan et al.[82] found that ingestion of phytoestrogens affects breast growth and lactation and has a role in uterine diseases such as fibroids and endometriosis. Chaparral, an estrogen-containing product, is shown to be associated with acute nonviral toxic hepatitis.[83]
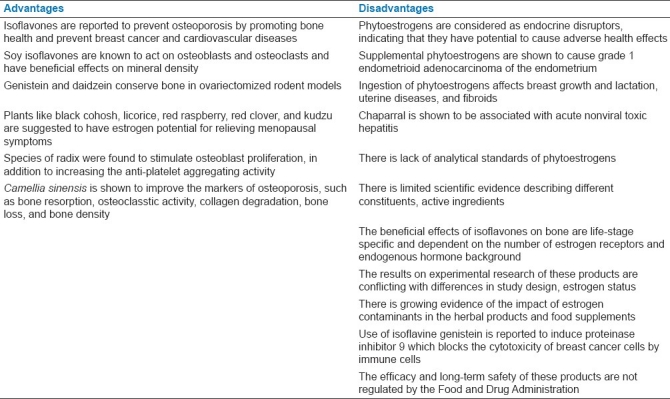
In addition to the adverse effects of phytoestrogens, they are associated with some serious drawbacks: (1) There is lack of analytical standards of phytoestrogens with no adequate methods for measurement of their levels in foods and the individual variability of metabolism of precursors introduced with the diet. Thus, there is utter confusion about the effectiveness of these products.[84] (2) There is limited scientific evidence describing different constituents, active ingredients, the dose, in addition to the presence of some unexpected agents.[84,85] (3) The beneficial effects of isoflavones on bone are life-stage specific and dependent on the number of estrogen receptors and endogenous hormone background.[80] (4) The results on experimental research of these products are haphazard. They are conflicting with differences in study design, estrogen status of the body, and metabolism.[67] (5) There is growing evidence of the impact of estrogenic contaminants in the herbal products and food supplements and the ingestion of which might induce feminizing potentials in the male population too.[82] (6) Use of isoflavine genistein is reported to induce proteinase inhibitor 9, which is known to block the cytotoxicity of breast cancer cells by immune cells.[86] Finally, (7) the efficacy and long-term safety of these products are not regulated by the Food and Drug Administration.[64] The advantages and disadvantages of plants and herbs used to compensate HRT are presented in Table 5.
Table 5.
Advantages and disadvantages of plants and herbs used against HRT
CONCLUSION
Deficiency of estrogen is known to cause significant alterations in bone metabolism. HRT therapy is considered as the major option to recompense the estrogen deficits. However, several reports associate it with serious adverse effects, in addition to an unfavorable and expensive procedure. Hence, several new drugs and hormonal preparations are being produced and marketed in order to substitute the HRT therapy. Nevertheless, in view of their deficient impact on the target and known toxicity including malignancy, most women are now enthralled by the extremely publicized natural products, including, phytoestrogens. These products are shown to be health protective in menopausal complaints associated with osteoporosis. Nonetheless, ingestion of phytoestrogens is shown to affect breast growth and lactation and has a role in uterine diseases such as fibroids and endometriosis. Furthermore, extensive use of supplemental phytoestrogens is reported to cause nonviral toxic hepatitis, grade 1 endometrioid adenocarcinoma of the endometrium. The effect of phytoestrogen is shown to be dependent on the number of estrogen receptors and endogenous hormone background. There is lack of scientific evidence on active constituents and definite dose; hence, the effectiveness of these products is uncertain. Moreover, their efficacy and long-term safety are not synchronized by the Food and Drug Administration. Taken together, it is apparent that both the synthetic hormones and drugs and phytoestrogens can be used against postmenopausal osteoporosis and both have adverse effects. Nevertheless, the synthetic hormones and drugs are scientific and regulated by the Food and Drug Administration, while the plant products are nonscientific and are not advised to be used till more studies are undertaken to ensure that the amount of benefit clearly outweighs the amount of risk, in addition to recognition by Food and Drug Administration.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Wark JD. Osteoporotic fractures: Background and prevention strategies. Maturitas. 1996;2:193–207. doi: 10.1016/0378-5122(95)00974-4. [DOI] [PubMed] [Google Scholar]
- 2.Dempster DW, Lindsay R. Pathogenesis of osteoporosis. Lancet. 1996;341:797–801. doi: 10.1016/0140-6736(93)90570-7. [DOI] [PubMed] [Google Scholar]
- 3.Fitzpatrick LA. Phytoestrogens-mechanism of action and effect on bone markers and bone mineral density. Endocrinol Metab Clin North Am. 2003;32:233–52. doi: 10.1016/s0889-8529(02)00085-3. VIII. [DOI] [PubMed] [Google Scholar]
- 4.Cook A, Pennington G. Phytoestrogen and multiple vitamin/mineral effects on bone mineral density in early postmenopausal women: A pilot study. J Womens Health Gend Based Med. 2002;11:53–60. doi: 10.1089/152460902753473462. [DOI] [PubMed] [Google Scholar]
- 5.Khosla S. Update on estrogens and the skeleton. J Clin Endocrinol Metab. 2010;95:3569–77. doi: 10.1210/jc.2010-0856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rotem C, Kaplan B. Phyto-Female Complex for the relief of hot flushes, night sweats and quality of sleep: Randomized, controlled, double-blind pilot study. Gynecol Endocrinol. 2007;23:117–22. doi: 10.1080/09513590701200900. [DOI] [PubMed] [Google Scholar]
- 7.Hirata JD, Swiersz LM, Zell B, Small R, Ettinger B. Does dong quai have estrogenic effects in postmenopausal women? A double-blind, placebo-controlled trial. Fertil Steril. 1997;68:981–6. doi: 10.1016/s0015-0282(97)00397-x. [DOI] [PubMed] [Google Scholar]
- 8.Tempfer CB, Froese G, Heinze G, Bentz EK, Hefler LA, Huber JC. Side effects of phytoestrogens: A meta-analysis of randomized trials.2009;122:939-46. Am J Med. 2009;122:939–46. doi: 10.1016/j.amjmed.2009.04.018. e9. [DOI] [PubMed] [Google Scholar]
- 9.Aubertin-Leheudre M, Lord C, Khalil A, Dionne IJ. Effect of 6 months of exercise and isoflavone supplementation on clinical cardiovascular risk factors in obese postmenopausal women: A randomized, double-blind study. Menopause. 2007;14:624–9. doi: 10.1097/gme.0b013e31802e426b. [DOI] [PubMed] [Google Scholar]
- 10.Cooper C. Epidemiology of osteoporosis. Osteoporos Int. 1999;9:S2–8. doi: 10.1007/pl00004156. [DOI] [PubMed] [Google Scholar]
- 11.Shilbayeh S. Prevalence of osteoporosis and its reproductive risk factors among Jordanian women: A cross-sectional study. Osteoporos Int. 2003;14:929–40. doi: 10.1007/s00198-003-1458-4. [DOI] [PubMed] [Google Scholar]
- 12.Navarro Rodríguez MC, Saavedra Santana P, de Pablos Velasco P, Sablón González N, de Miguel Ruiz E, Castro Medina R, et al. Lifestyle, socioeconomic status and morbidity in postmenopausal women with grade II and III obesity. Endocrinol Nutr. 2009;56:227–32. doi: 10.1016/S1575-0922(09)71405-6. [DOI] [PubMed] [Google Scholar]
- 13.MerckMedicus Modules: Osteoporosis – Epidemiology”. [Last accessed on 2007 Dec 28]. Available from: (http://web.archive.org/web/200.712.28030929. /http://www.merckmedicus.com/pp/us/hcp/diseasemodules/osteoporosis/epidemiology.jsp. ) Merck and Co., Inc. Archived from the original (http://www.merckmedicus.com/pp/us/hcp/diseasemodules/osteoporosis/epidemiology.jsp. )
- 14.Cauley JA, Hochberg MC, Lui LY. “Long-term Risk of Incident Vertebral Fractures”. JAMA. 2007;298:2761–7. doi: 10.1001/jama.298.23.2761. [DOI] [PubMed] [Google Scholar]
- 15.Fogarty P, O’Beirne B, Casey C. Epidemiology of the most frequent diseases in the European a-symptomatic post-menopausal women. Is there any difference between Ireland and the rest of Europe? Maturitas. 2005;52(Suppl 1):S3–6. doi: 10.1016/j.maturitas.2005.06.018. [DOI] [PubMed] [Google Scholar]
- 16.Murrillo-Uribe A, Delezé-Hinojosa M, Aguirre E, Villa A, Calva J, Cons F, et al. Osteoporosis in Mexican postmenopausal women. Magnitude of the problem. Multicenter study. Ginecol Obstet Mex. 1999;67:227–33. [PubMed] [Google Scholar]
- 17.Raspe A, Matthis C, von Domarus U, Scheidt-Nave C, Abendroth K, Reisinger W, et al. Current musculoskeletal symptoms in peri and postmenopausal women: Results of a multicenter population epidemiological study. The EVOS Study Group. Soz Praventivmed. 1994;39:379–86. doi: 10.1007/BF01299669. [DOI] [PubMed] [Google Scholar]
- 18.Gaja A, Zmrzlík P, Gajová B. Contribution to the social importance and the epidemiology of osteoporosis. Acta Univ Palacki Olomuc Fac Med. 1993;135:13–5. [PubMed] [Google Scholar]
- 19.Hamdi Kara I, Aydin S, Gemalmaz A, Aktürk Z, Yaman H, Bozdemir N, et al. Habitual tea drinking and bone mineral density in postmenopausal Turkish women: investigation of prevalence of postmenopausal osteoporosis in Turkey (IPPOT Study) Int J Vitam Nutr Res. 2007;77:389–97. doi: 10.1024/0300-9831.77.6.389. [DOI] [PubMed] [Google Scholar]
- 20.Gur A, Sarac AJ, Nas K, Cevik R. The relationship between educational level and bone mineral density in postmenopausal women. BMC Fam Pract. 2004;5:18. doi: 10.1186/1471-2296-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gulbahar S, Sahin E, Baydar M, Bircan C, Kizil R, Manisali M, et al. Hypermobility syndrome increases the risk for low bone mass. Clin Rheumatol. 2006;25:511–4. doi: 10.1007/s10067-005-0103-3. [DOI] [PubMed] [Google Scholar]
- 22.Maalouf G, Salem S, Sandid M, Attallah P, Eid J, Saliba N, et al. Bone mineral density of the Lebanese reference population. Osteoporos Int. 2000;11:756–64. doi: 10.1007/s001980070054. [DOI] [PubMed] [Google Scholar]
- 23.Nitzan-Kaluski D, Chinich A, Ifrah A, Merom D, Green MS. Correlates of osteoporosis among Jewish and Arab women aged 45-74 in Israel: National women's health interview survey. J Gend Specif Med. 2003;6:17–23. [PubMed] [Google Scholar]
- 24.Werner P, Olchovsky D, Vered I. Osteoporosis health-related behavior among healthy peri-menopausal and post-menopausal Israeli Jewish and Arab women. Aging Clin Exp Res. 2005;17:100–7. doi: 10.1007/BF03324581. [DOI] [PubMed] [Google Scholar]
- 25.Sidibe EH. Menopause in Africa. Ann Endocrinol (Paris) 2005;66:105–7. doi: 10.1016/s0003-4266(05)81706-8. [DOI] [PubMed] [Google Scholar]
- 26.Sallam H, Galal AF, Rashed A. Menopause in Egypt: Past and present perspectives. Climacteric. 2006;9:421–9. doi: 10.1080/13697130601030170. [DOI] [PubMed] [Google Scholar]
- 27.Noreh J, Sekadde-Kigondu C, Karanja JG, Thagana NG. Median age at menopause in a rural population of western Kenya. East Afr Med J. 1997;74:634–8. [PubMed] [Google Scholar]
- 28.Addar M, El Desouki M, Babay Z. Correlates of age at menopause and osteoporosis in Saudi women. Clin Exp Obstet Gynecol. 2005;32:135–7. [PubMed] [Google Scholar]
- 29.Sadat-Ali M, Al-Habdan I, Al-Mulhim AA, El-Hassan AY. Effect of parity on bone mineral density among postmenopausal Saudi Arabian women. Saudi Med J. 2005;26:1588–90. [PubMed] [Google Scholar]
- 30.Sadat-Ali M, Gullenpet AH, Al-Mulhim F, Al Turki H, Al-Shammary H, Al-Elq A, et al. Osteoporosis-related vertebral fractures in postmenopausal women: Prevalence in a Saudi Arabian sample. East Mediterr Health J. 2009;15:1420–5. [PubMed] [Google Scholar]
- 31.Sadat-Ali M, Al-Habdan IM, Al-Mulhim FA, El-Hassan AY. Bone mineral density among postmenopausal Saudi women. Saudi Med J. 2004;25:1623–5. [PubMed] [Google Scholar]
- 32.Keramat A, Patwardhan B, Larijani B, Chopra A, Mithal A, Chakravarty D, et al. The assessment of osteoporosis risk factors in Iranian women compared with Indian women. BMC Musculoskelet Disord. 2008;9:28. doi: 10.1186/1471-2474-9-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shatrugna V, Kulkarni B, Kumar PA, Rani KU, Balakrishna N. Bone status of Indian women from a low-income group and its relationship to the nutritional status. Osteoporos Int. 2005;16:1827–35. doi: 10.1007/s00198-005-1933-1. [DOI] [PubMed] [Google Scholar]
- 34.Chailurkit LO, Piaseu N, Rajatanavin R. Influence of normal ageing on mechanism of bone loss in women and men in Bangkok. J Med Assoc Thai. 2002;85:915–21. [PubMed] [Google Scholar]
- 35.Limpaphayom KK, Taechakraichana N, Jaisamrarn U, Bunyavejchevin S, Chaikittisilpa S, Poshyachinda M, et al. Prevalence of osteopenia and osteoporosis in Thai women. Menopause. 2001;8:65–9. doi: 10.1097/00042192-200101000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Huang KE. Menopause perspectives and treatment of Asian women. Semin Reprod Med. 2010;28:396–403. doi: 10.1055/s-0030-1262899. [DOI] [PubMed] [Google Scholar]
- 37.Khan A. Advances in osteoporosis therapy. 2003 Can Fam Physician. 2003;49:441–7. [PMC free article] [PubMed] [Google Scholar]
- 38.Alden JC. Osteoporosis – A review. Clin Ther. 1989;11:3–14. [PubMed] [Google Scholar]
- 39.Hoeger KM, Guzick DS. The use of androgens in menopause. Clin Obstet Gynecol. 1999;42:883–94. doi: 10.1097/00003081-199912000-00016. [DOI] [PubMed] [Google Scholar]
- 40.Ebeling PR. “Clinical practice. Osteoporosis in men”. N Engl J Med. 2008;358:1474–82. doi: 10.1056/NEJMcp0707217. [DOI] [PubMed] [Google Scholar]
- 41.Davis S, Sachdeva A, Goeckeritz B, Oliver A. Approved treatments for osteoporosis and what's in the pipeline. Drug Benefit Trends. 2010;22:121–4. [Google Scholar]
- 42.National Prescribing Service. “Zoledronic Acid for osteoporosis” Medcines Update. 2009. [Last accessed on 2011 Jan 27]. Available from: http://www.nps.org.au/consumers/publications/medicine_update/issues/Zoledronic_acid .
- 43.Meunier PJ, Roux C, Seeman E. “The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis”. N Engl J Med. 2004;350:459–68. doi: 10.1056/NEJMoa022436. [DOI] [PubMed] [Google Scholar]
- 44.Report of a joint WHO/FAO/UNU Expert consultation. Protein and amino acid requirements in human nutrition. 2007. pp. 224–6. Available from: (http://whqlibdoc.who.int/trs/WHO_TRS_935_eng.pdf. ) [PubMed]
- 45.Rossouw JE, Anderson GL, Prentice RL. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: Principal results from the Women's Health Initiative randomized controlled trial. JAMA. 2002;288:321. doi: 10.1001/jama.288.3.321. [DOI] [PubMed] [Google Scholar]
- 46.Cosman F, Lindsay R. Selective estrogen receptor modulators: Clinical spectrum. Endocr Rev. 1999;20:418–34. doi: 10.1210/edrv.20.3.0371. [DOI] [PubMed] [Google Scholar]
- 47.Verhaar HJ. Treatment of osteoporosis in the elderly: What is the evidence? Tijdschr Gerontol Geriatr. 2008;39:168–75. doi: 10.1007/BF03078150. [DOI] [PubMed] [Google Scholar]
- 48.Bretler DM, Hansen PR, Abildstrom SZ, Jorgensen CH, Sorensen R, Hansen ML, et al. Use and discontinuation of hormone replacement therapy in women with mnyocardial infarction: A nationwide study. Br J Clin Pharmacol. 2011;71:105–15. doi: 10.1111/j.1365-2125.2010.03790.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Johannes CB, Crawford SL, Posner JG, McKinlay SM. Longitudinal patterns and correlates of hormone replacement therapy use in middle-aged women. Am J Epidemiol. 1994;140:439. doi: 10.1093/oxfordjournals.aje.a117266. [DOI] [PubMed] [Google Scholar]
- 50.Grodstein F, Manson JE, Stampfer MJ. Postmenopausal hormone use and secondary prevention of coronary events in the nurses’ health study. a prospective, observational study. Ann Intern Med. 2001;135:1–8. doi: 10.7326/0003-4819-135-1-200107030-00003. [DOI] [PubMed] [Google Scholar]
- 51.Battaglioli T, Martinelli I. Hormone therapy and thromboembolic disease. Curr Opin Hematol. 2007;14:488–93. doi: 10.1097/MOH.0b013e32825f5302. [DOI] [PubMed] [Google Scholar]
- 52.Studd J. Profox – the post HRT nightmare. Climacteric. 2011;14:217–9. doi: 10.3109/13697137.2010.529199. [DOI] [PubMed] [Google Scholar]
- 53.Chlebowski RT, Anderson GL, Gass M, Lane DS, Aragaki AK, Kuller LH, et al. Estrogen plus progestin and breast cancer incidence and mortality in postmenopausal women. JAMA. 2010;304:1684–92. doi: 10.1001/jama.2010.1500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.This P, De La Rochefordiere A, Clough K, Fourquet A, Magdelenat H. Breast Cancer Group of the Institut Curie. Phytoestrogens after breast cancer. Endocr Relat Cancer. 2001;8:129–34. doi: 10.1677/erc.0.0080129. [DOI] [PubMed] [Google Scholar]
- 55.Breast cancer and hormone replacement therapy: Collaborative reanalysis of data from 51 epidemiological studies of 52,705 women with breast cancer and 108,411 women without breast cancer. Collaborative Group on Hormonal Factors in Breast Cancer. Lancet. 1997;350:1047–59. [PubMed] [Google Scholar]
- 56.McVeigh C. Withdrawal of synthetic hormones during the perimenopause: A case study. J Psychosom Obstet Gynaecol. 2000;21:175–8. doi: 10.3109/01674820009075625. [DOI] [PubMed] [Google Scholar]
- 57.Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, et al. Effect of para thyroid hormone (1-34) on frasctures and bone m.neral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344:1434–41. doi: 10.1056/NEJM200105103441904. [DOI] [PubMed] [Google Scholar]
- 58.Pickar JH, Mirkin S. Tissue-selective agents: Selective estrogen receptor modulators and the tissue-selective estrogen complex. Menopause Int. 2010;16:121–8. doi: 10.1258/mi.2010.010033. [DOI] [PubMed] [Google Scholar]
- 59.Barrett-Connor E, Mosca L, Collins P. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355:125. doi: 10.1056/NEJMoa062462. [DOI] [PubMed] [Google Scholar]
- 60.Modelska K, Cummings S. Tibolone for postmenopausal women: Systematic review of randomized trials. J Clin Endocrinol Metab. 2002;87:16. doi: 10.1210/jcem.87.1.8141. [DOI] [PubMed] [Google Scholar]
- 61.Smolinski D, Wollner D, Orlowski J, Curcio J, Nevels J, Kim LS. A pilot study to examine a combination botanical for the treatment of menopausal symptoms. J Altern Complement Med. 2005;11:483–9. doi: 10.1089/acm.2005.11.483. [DOI] [PubMed] [Google Scholar]
- 62.Limer JL, Speirs V. Phyto-oestrogens and breast cancer chemoprevention. Breast Cancer Res. 2004;6:119–27. doi: 10.1186/bcr781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ha H, Lee YS, Lee JH, Choi H, Kim C. High performance liquid chromatographic analysis of isoflavones in medicinal herbs. Arch Pharm Res. 2006;29:96–101. doi: 10.1007/BF02977475. [DOI] [PubMed] [Google Scholar]
- 64.Grippo AA, Capps K, Rougeau B, Gurley BJ. Analysis of flaonoid phytoestrogens in botanical and ephedra-containing dietary supplements. Ann Pharmacother. 2007;41:1375–82. doi: 10.1345/aph.1H497. [DOI] [PubMed] [Google Scholar]
- 65.Franke AA, Halm BM, Kakazu K, Li X, Custer LJ. Phytoestrogenic isoflavonoids in epidemiologic and clinical research. Drug Test Anal. 2009;1:14–21. doi: 10.1002/dta.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Foth D, Cline JM, Römer T. Effect of isoflavones on mammary gland and endometrium of postmenopausal macaques (Macaca fascicularis) Zentralbl Gynakol. 2000;122:96–102. [PubMed] [Google Scholar]
- 67.Atmaca A, Kleerekoper M, Bayraktar M, Kucuk O. Soy isoflavones in the management of postmenopausal osteoporosis. Menopause. 2008;15:748–57. doi: 10.1097/gme.0b013e31815c1e7f. [DOI] [PubMed] [Google Scholar]
- 68.Joo SS, Won TJ, Kang HC, Lee DI. Isoflavones extracted from Sophorae fructus upregulate IGF-I and TGF-beta and inhibit osteoclastogenesis in rat bone marrow cells. Arch Pharm Res. 2004;27:99–105. doi: 10.1007/BF02980054. [DOI] [PubMed] [Google Scholar]
- 69.Anderson JJ, Garner SC. Phytoestrogens and bone. Baillieres Clin Endocrinol Metab. 1998;12:543–57. doi: 10.1016/s0950-351x(98)80003-7. [DOI] [PubMed] [Google Scholar]
- 70.Hooshmand S, Juma S, Arjmandi BH. Combination of genistin and fructo oligosaccharides prevents bone loss in ovarian hormone deficiency. J Med Food. 2010;13:320–5. doi: 10.1089/jmf.2009.0059. [DOI] [PubMed] [Google Scholar]
- 71.Zittermann A, Geppert J, Baier S, Zehn N, Gouni-Berthold I, Berthold HK, et al. Short-term effects of high soy supplementation on sex hormones, bone markers, and lipid parameters in young female adults. Eur J Nutr. 2004;43:100–8. doi: 10.1007/s00394-004-0447-5. [DOI] [PubMed] [Google Scholar]
- 72.Ju YH, Doerge DR, Helferich WG. A dietary supplement for female sexual dysfunction, Avlimil, stimulates the growth of estrogen-dependent breast tumors (MCF-7) implanted in ovariectomized athymic nude mice. Food Chem Toxicol. 2008;46:310–20. doi: 10.1016/j.fct.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 73.Oerter Klein K, Janfaza M, Wong JA, Chang RJ. Estrogen bioactivity in fo-ti and other herbs used for their estrogen-like effects as determined by a recombinant cell bioassay. J Clin Endocrinol Metab. 2003;88:4077–9. doi: 10.1210/jc.2003-030349. [DOI] [PubMed] [Google Scholar]
- 74.Ganry O. Phytoestrogens and prostate cancer risk. Prev Med. 2005;41:1–6. doi: 10.1016/j.ypmed.2004.10.022. [DOI] [PubMed] [Google Scholar]
- 75.Moutsatsou P. The spectrum of phytoestrogens in nature: Our knowledge is expanding. Hormones (Athens) 2007;6:173–93. [PubMed] [Google Scholar]
- 76.Dong TT, Zhao KJ, Gao QT, Ji ZN, Zhu TT, Li J, et al. Chemical and biological assessment of a chinese herbal decoction containing Radix Astragali and Radix Angelicae Sinensis: Determination of drug ratio in having optimized properties. J Agric Food Chem. 2006;54:2767–74. doi: 10.1021/jf053163l. [DOI] [PubMed] [Google Scholar]
- 77.Booth NL, Piersen CE, Banuvar S, Geller SE, Shulman LP, Farnsworth NR. Clinical studies of red clover (Trifolium pratense) dietary supplements in menopause: A literature review. Menopause. 2006;13:251–64. doi: 10.1097/01.gme.0000198297.40269.f7. [DOI] [PubMed] [Google Scholar]
- 78.Whelan AM, Jurgens TM, Bowles SK. Natural health products in the prevention and treatment of osteoporosis: Systematic review of randomized controlled trials. Ann Pharmacother. 2006;40:836–49. doi: 10.1345/aph.1G226. [DOI] [PubMed] [Google Scholar]
- 79.Das AS, Das D, Mukherjee M, Mukherjee S, Mitra C. Phytoestrogenic effects of black tea extract (Camellia sinensis) in an oophorectomized rat (Rattus norvegicus) model of osteoporosis. Life Sci. 2005;77:3049–57. doi: 10.1016/j.lfs.2005.02.035. [DOI] [PubMed] [Google Scholar]
- 80.Reinwald S, Weaver CM. Soy isoflavones and bone health: A double-edged sword? J Nat Prod. 2006;69:450–9. doi: 10.1021/np058104g. [DOI] [PubMed] [Google Scholar]
- 81.Johnson EB, Muto MG, Yanushpolsky EH, Mutter GL. Phytoestrogen supplementation and endometrial cancer. Obstet Gynecol. 2001;98:947–50. doi: 10.1016/s0029-7844(01)01542-3. [DOI] [PubMed] [Google Scholar]
- 82.McLachlan JA, Simpson E, Martin M. Endocrine disrupters and female reproductive health. Best Pract Res Clin Endocrinol Metab. 2006;20:63–75. doi: 10.1016/j.beem.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 83.Obermeyer WR, Musser SM, Betz JM, Casey RE, Pohland AE, Page SW. Chemical studies of phytoestrogens and related compounds in dietary supplements: Flax and chaparral. Proc Soc Exp Biol Med. 1995;208:6–12. doi: 10.3181/00379727-208-43824. [DOI] [PubMed] [Google Scholar]
- 84.Albertazzi P, Purdie D. The nature and utility of the phytoestrogens: A review of the evidence. Maturitas. 2002;42:173–85. doi: 10.1016/s0378-5122(02)00024-5. [DOI] [PubMed] [Google Scholar]
- 85.Geller SE, Studee L. Botanical and dietary supplements for menopausal symptoms: What works, what does not. J Womens Health (Larchmt) 2005;14:634–49. doi: 10.1089/jwh.2005.14.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jiang X, Patterson NM, Ling Y, Xie J, Helferich WG, Shapiro DJ. Low concentrations of the soy phytoestrogen genistein induce proteinase inhibitor 9 and block killing of breast cancer cells by immune cells. Endocrinology. 2008;149:5366–73. doi: 10.1210/en.2008-0857. [DOI] [PMC free article] [PubMed] [Google Scholar]


