Abstract
Marijuana abuse has been on an increasing trend worldwide in the last decade. We hereby report a case of severe bullous emphysema resulting in pneumothorax in a patient with few years of marijuana abuse. We also review the major conditions in the differential diagnosis of bullous emphysema in adults.
KEYWORDS: Emphysema, marijuana, pneumothorax, VATS
INTRODUCTION
Marijuana abuse has been on an increasing trend worldwide in the last decade. We hereby report a case of severe bullous emphysema resulting in pneumothorax in a patient with a few years of marijuana abuse.
CASE REPORT
We hereby report a case of a 25-year-old African American male who presented to the emergency room with sudden onset of shortness of breath and right-sided chest pain. His social history is significant for smoking two to four cigarettes and two to three joints of marijuana/day for the last 8 years. There is no history of significant occupational or animal exposure, intravenous drug use, or use of any medications. His past medical history is significant for sarcoidosis diagnosed 10 years back by bronchoscopy and biopsy. He was started on steroids for sarcoidosis, but was noncompliant to treatment.
On physical examination, the patient was afebrile with normal vital signs. The chest exam revealed decreased breath sounds as well as hyper-resonance on percussion over the right lung field. The cardiovascular examination was normal. There was no cyanosis or clubbing. There was no hepatomegaly or signs of chronic liver disease.
A chest radiograph was performed, which showed a right-sided pneumothorax with no mediastinal lymphadenopathy [Figure 1]. Subsequently, a chest computerized tomography (CT) was performed, which showed severe emphysematous bulla in the bilateral lungs with upper lobe predominance [Figure 2].
Figure 1.
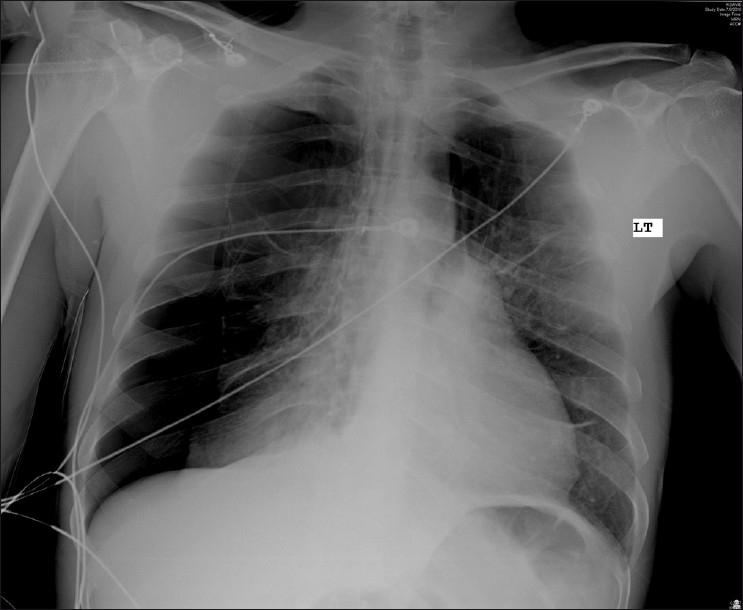
Chest radiograph showing right-sided pneumothorax on presentation
Figure 2.
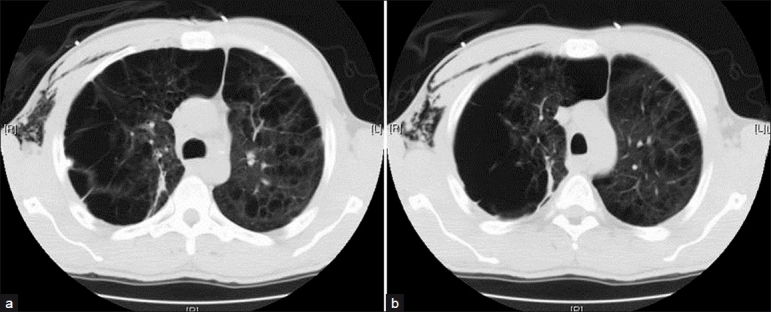
Computerized tomographic scan showing severe bilateral upper lobe bullous lung disease
The full-blood examination was normal, with no eosinophilia. The erythrocyte sedimentation rate was not elevated. An angiotensin-converting enzyme level was performed, which was normal (44; reference range: 12–68). Alpha-1-antitrypsin was also within the normal range (151; reference range: 90–200). Sputum microscopy and culture for bacteria, acid-fast bacilli, and fungi were negative.
Pulmonary function testing revealed a severe obstructive ventilatory defect, with a possible associated restrictive ventilator defect, and no response to the bronchodilator. Gas transfer was significantly reduced.
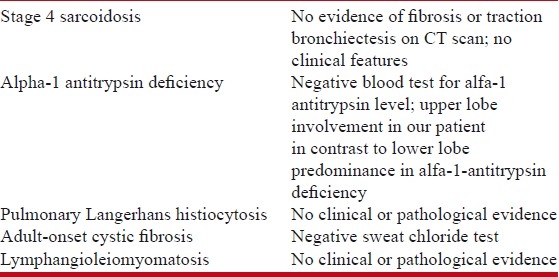
After excluding all the potential causes of cystic lung disease [Table 1] and taking into consideration his new-onset marijuana smoking in the last 8 years, marijuana abuse was thought to be the cause of his bullous lung disease. The patient was treated with a chest tube and subsequently discharged with advice to quit marijuana smoking and further referral to general surgery for bullous resection.
Table 1.
Main differential diagnoses of bullous lung disease in adults and features, from the current case, against these diagnoses
DISCUSSION
The harmful effects of tobacco smoking, especially over a period of several years, leading to large emphysematous lung bulla have been well documented.[1] However, the chronic pulmonary effects of marijuana smoking are less well described and there are very few reports demonstrating the association of marijuana smoking with large lung bulla.[2]
In 1972, Miller et al. reported a case of pneumomediastinum resulting from performing high-pressure valsalva maneuvers during marijuana smoking.[3] In 2000, Johnson et al. described four cases of large lung bulla in young men with significant exposure to marijuana but low exposure to tobacco.[4] According to the more recent data in 2008, Hii et al. conducted a prospective case series consisting of 10 patients who regularly used marijuana and who developed new respiratory symptoms. Nine of these patients showed severe asymmetrical and variably sized bulla on CT scan.[5] Similarly, in 2008, Beshay et al. conducted a retrospective case series in which, among the 102 patients who presented with spontaneous pneumothorax at the emergency unit within a 2.5-year period, 17 patients who had relevant pulmonary emphysema and history of marijuana abuse were retrospectively evaluated systematically. The study concluded marijuana abuse as one of the important differentials in case of emphysema in young individuals.[6]
Marijuana smoking frequently, known as “POT,” is of significant concern because of its frequent use among young adults. The exact mechanism for bulla formation in marijuana abuse is not well known. It may be a combination of direct pulmonary toxicity from components in marijuana in susceptible smokers and airway barotrauma related to the high inspiratory pressure and prolonged breath-hold generated during marijuana smoking.[7] Studies have shown that marijuana smoking involves a two-thirds larger puff volume, a one-third greater depth of inhalation, and four-times longer breath-holding time than tobacco smoking.[3] This inhalation pattern can result in an increased risk of spontaneous pneumothorax, as seen in marijuana smokers. Besides spontaneous pneumothorax, regular marijuana users also experience more cough, sputum, and wheezes than nonsmokers. Three to four “joints” of marijuana per day have been reported to give as many symptoms as an average of 24 cigarettes.
CONCLUSION
We affirm that in all cases of bullous emphysema in young individuals, marijuana abuse should be included in the differential diagnosis. The period of marijuana smoking plays an important role in the development of lung emphysema. Most of the patients are asymptomatic and present with spontaneous pneumothoraces. Video-assisted thoracoscopic surgery (VATS) should be considered as one of the options for resection of bulla and prevention of recurrent pneumothoraces.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.A report of the Surgeon General. Washington, DC: Office of the Assistant Secretary for Health, Office of Smoking and Health; 1984. US Department of Health and Human Services. Chronic obstructive lung disease. The health consequences of smoking. DHHS Publication No. 84-2677. [Google Scholar]
- 2.Phan TD, Lau KK, Li X. Lung bullae and pulmonary fibrosis associated with marijuana smoking. Australas Radiol. 2005;49:411–4. doi: 10.1111/j.1440-1673.2005.01472.x. [DOI] [PubMed] [Google Scholar]
- 3.Miller WE, Spiekerman RE, Hepper NG. Pneumomediastinum resulting from performing Valsalva maneuvers during marihuana smoking. Chest. 1972;62:233–4. doi: 10.1378/chest.62.2.233. [DOI] [PubMed] [Google Scholar]
- 4.Johnson MK, Smith RP, Morrison D, Laszlo G, White R. Large lung bullae in marijuana smokers. Thorax. 2000;55:340–2. doi: 10.1136/thorax.55.4.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hii SW, Tam JD, Thompson BR, Naughton MT. Bullous lung disease due to marijuana. Respirology. 2008;13:122–7. doi: 10.1111/j.1440-1843.2007.01186.x. [DOI] [PubMed] [Google Scholar]
- 6.Wu TC, Tashkin DP, Djahed B, Rose JE. Pulmonary hazards of smoking marijuana as compared with tobacco. N Engl J Med. 1988;318:347–51. doi: 10.1056/NEJM198802113180603. [DOI] [PubMed] [Google Scholar]
- 7.Tashkin DP, Coulson AH, Clark VA, Simmons M, Bourque LB, Duann S, et al. Respiratory symptoms and lung function in habitual heavy smokers of marijuana alone, smokers of marijuana and tobacco, smokers of tobacco alone and nonsmokers. Am Rev Respir Dis. 1987;135:209–16. doi: 10.1164/arrd.1987.135.1.209. [DOI] [PubMed] [Google Scholar]


