Abstract
Context:
Studies have revealed high morbidity and mortality among agate stone workers of Shakarpur due to silicosis. Besides the fatal disease, the workers also suffer from debilitating co-morbidities especially tuberculosis and under nutrition.
Aims:
The present study describes few co-morbidities and their influence in mortality in cases of silicosis that were followed for 30 months at Shakarpur.
Settings and Design:
Shakarpur, Khambhat of Gujarat.
Materials and Methods:
Spirometry for lung function, chest X-ray, anthropometry, body fat % measurement, record of tuberculosis status and ILO classification of pneumoconiosis were done among 53 chest symptomatic patients above 15 years of age who were followed for 30 months.
Results:
Out of 53 participants (35 men), with an average duration of exposure to free silica of 16.8 years, more than half of the male workers were underweight (BMI<18.5 kg/m2) at enrollment. Thirteen participants died in less than 3 years of follow up. While 11 of them were silicosis positive out of which 10 had tuberculosis. The odds ratio for association between silicosis and tuberculosis was 2.75. A majority (81.1%) of the 37 silicosis positive cases showed a mixed pattern in spirometry suggesting co-existence of restrictive and obstructive pathology. On regression analysis, TB and nutritional status were found to have strong influence on mortality.
Conclusions:
Screening for early diagnosis of silicosis as well as co-morbid conditions and managing them would go a long way in prolonging the lives of the agate stone workers who are prone to die early due to silicosis.
KEYWORDS: Agate worker, co-morbidities, silicosis, tuberculosis
INTRODUCTION
Silicosis is known to shorten substantially the lifespan of a person exposed to fine silica dust over prolonged period.[1] In Agate stone polishing industries of India, about 38% of workers develop silicosis in their lifetime.[2] Not only workers in this industry develop silicosis due to the chronic exposure to the dust, their families and other nonoccupational groups that also reside within the area develop silicosis (6.8 – 11.8 %), Silico-tuberculosis (2.8 – 6.3%), and tuberculosis (TB) (19.7 – 20.1%).[3] In Shakarpur of Khambhat subdivision of Gujarat, India, unorganized laborers have been making ornaments and other decorative and showcase items from agate and other stones since several decades. Studies reveal that the concentration of respirable dust in these household industries is very high and contains more than 60% free silica in it.[4] A follow up study of 458 workers at sandstone quarries of Jodhpur reported that the average age at time of death was 51 ± 12.5 years.[5] However, it is difficult to comment based on these studies whether people working in these industries really die early from silicosis or due to a compounding effect of co-morbid conditions such as TB, chronic obstructive pulmonary disease (COPD), etc. Also, little is known about the relationship between nutritional status of the victims and fatality from silicosis.
The present study, conducted among critically ill chest symptomatic patients in an area of stone polishing industries, explores the presence of few known co-morbidities in confirmed cases of silicosis. The investigators intended to follow the confirmed cases for at least 3 years, but due to high mortality, decided to terminate before 3 years. This is a sequel to the analysis of clinic based data published by us in Lung India.[6]
MATERIALS AND METHODS
Sample
The study was carried out on chest symptomatic patients residing in Shakarpur village in the outskirts of Khambhat city who attended a specially arranged health clinic for the agate workers at Shakarpur on invitation, from June to December 2007 and were followed up till March 2010. The details of the method of recruitment of the patients in the clinic have been explained elsewhere.[6]
Inclusion criteria
Patients above 15 years of age of both genders living in Shakarpur, having symptoms of chronic cough for more than 3 months and/or breathlessness with a history of exposure to silica for more than a year, were invited to attend the clinic for diagnosis and treatment and follow up thereafter.
Exclusion criteria
Participants who were not ambulatory and those who could not blow into the spirometer due to severity or other disability of the morbid condition were excluded from the study.
Ethical issues
The study was approved by the Human Research Ethics Committee of a local medical college and teaching hospital. Written Informed consent was obtained from each participant before any data collection.
Study procedures and measures
Chest X-ray
During the study period, a visiting chest physician from a teaching hospital examined the participants and referred the cases suspected of silicosis for chest X-ray to a local hospital using a 300 mA machine. The X-rays were sent to the teaching hospital where they were examined for the presence or the absence of silicosis based on International Labor Organization's guidelines for diagnosis of Pneumoconiosis independently by a senior radiologist and a senior chest physician. Patients were diagnosed to have silicosis if either the chest physician and/or the radiologist rated them as positive for small or large opacities in the chest X-ray. The overall Kappa for inter rater agreement between chest physician and radiologist was fair (0.59).
Lung function
The clinical profiles of the participants were recorded and pulmonary function tests using a spirometer (Pony Fx V Edition 03/2005) were done at the clinic. The lung function tests were conducted by a physiologist and the reports were also verified by a senior chest physician. Lung function was interpreted as obstructive, restrictive, mixed pattern, or normal as per standard guidelines[7] based on the parameters — forced vital capacity (FVC), forced expiratory volume in 1 s, and the flow volume loop obtained from the spirometer. A post bronchodilator test with 200 μg salbutamol by aerosol followed by spirometry 20 min later was done to check for the presence of COPD. An increase of less than 12% or 200 ml in FEV1 was considered as sign of COPD.
History of tuberculosis
A detailed history about diagnosis of TB by the local District TB Centre (DTC) at the beginning of the follow up study was taken from the patients and/or their relatives. In newly suspected cases, volunteers accompanied the patients to the DTC for confirmation of diagnosis.
Anthropometry and body fat measurement
The nutritional status of the individuals was assessed in terms of body mass index and body fat percentage using a stadiometer and a segmental body composition analyzer (model: TBF 545 of TANITA),[8] respectively. A BMI of 18.5 kg/m2 up to 25 kg/m2 was considered normal while below the lower limit was considered underweight[9] and for operational definition, categorized as under nutrition. The normal ranges for total body fat were considered as per recommendations of the manufacturer of the instrument in the absence of specific guidelines for the Indian population. The purpose of measuring body fat was to look for a proxy measure of loss of lean mass over a prolonged period of under nutrition.
Record of mortality
The clinic followed up the participants till March 2010 and recorded fatalities if any.
Analysis
A total of 74 participants consented for the study after trained volunteers screened households and work sites of Agate stone polishing units at Shakarpur, and approached patients for the study based on inclusion criteria. Twenty people had died before they could be approached for spirometry while few others, who gave consent, were not in a position to perform the test due to severe illness. Ultimately, 53patients’ data were available on spirometric assessment of lung function, chest X-rays, anthropometry and body composition for analysis. Data were analyzed using SPSS 14 software.
RESULTS
Demographic profile
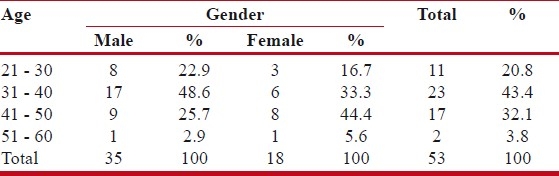
Table 1 shows the distribution of men and women across different age groups, who participated in the study. There was significantly lower participation from age groups above 50 years due to extremely debilitated condition and secondly, most people in that age group engaged in polishing work had already died.
Table 1.
Age–gender distribution of all participants
Exposure history
Proportions of participants with history of exposure to free silica for less than 10 years, 11 to 19 years, and more than or equal 20 years were 19.6%, 37%, and 47.8%, respectively. The minimum duration of exposure was 3 years while maximum was 40 years.
BMI
Figure 1 and Table 2 show the distribution of body mass index and total body fat percentages of the participants.
Figure 1.
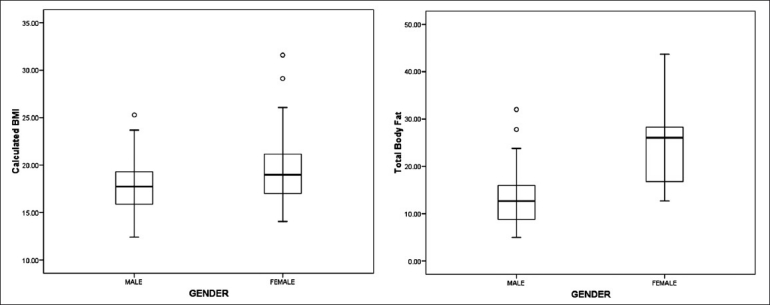
Box plot showing gender wise BMI distribution and body fat distribution
Table 2.
Body mass index and body fat percentage by gender
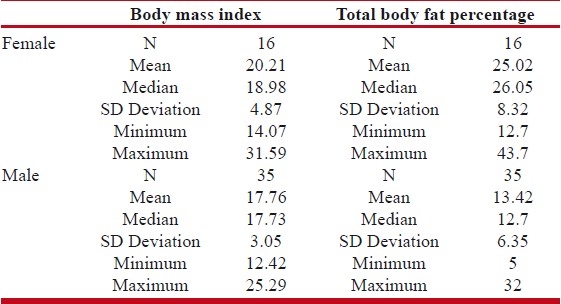
More than 50 % of male participants were underweight (median BMI is 17.73). The difference in mean BMI across males and females was significant (P<0.01). While the mean body fat percentage was highly significantly different (P<.0001) across two genders, the values were in normal limits for both genders as per international guidelines as defined in the methods section.
Chest X-ray
Out of 13 fatalities, 11 (84%) were already positive for silicosis as per the standard X-rays of International Labor Organization. They form 29% of the total silicosis positive participants. The age at death of the participants ranges from 28 years to 60 years, with both mean and median at 40 years. This indicates that more than half of the workers died young below 40 years of age.
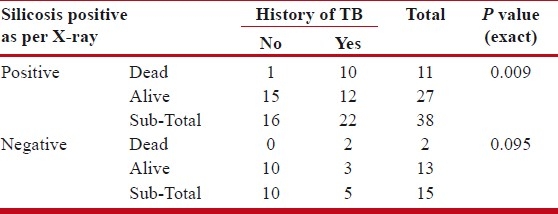
History of TB
On exploring the history of TB, it was found that 27 out of 53, that is, half of the participants had taken treatment for TB, of which, nearly a half (13) died during the follow-up period. Incidentally among the dead, the two cases negative for silicosis had history of TB[Table 3]. There was highly significant association between fatality and TB among the silicosis positive (P<0.01, Fishers’ exact test). The odds ratio for an association between silicosis and TB was 2.75.
Table 3.
Association between silicosis status and history of tuberculosis
The lung function tests
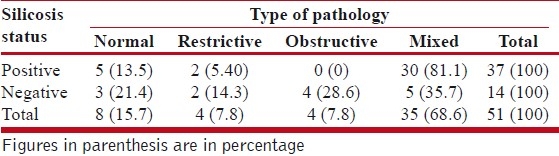
Table 4 shows that pure restrictive pattern is not very common but a mixed pattern of lung function dominates the scene. In silicosis negative cases, there is an expectedly large number of obstructive and mixed pattern suggesting the presence of COPD, but two cases of restrictive type pathology are seen as well, which are positive for TB. Among men (n=33), 22 (70%) had either mixed or purely obstructive pattern (3 cases) while among women (n=18) there were 15 (89%) with mixed pattern and 1 woman having a purely obstructive pattern. This reflects the prevalence of a high proportion of obstructive pathology in combination with restrictive pathology. The results of a post-bronchodilator test on the patients with obstructive and mixed patterns were consistent with coexisting COPD. All the participants with a mixed obstructive and restrictive pattern showed symptomatic improvement with inhaled bronchodilators and inhaled corticosteroids in subsequent follow-ups.
Table 4.
Type of lung pathology from pulmonary function tests
On running a multivariable logistic regression analysis using the stepwise method, we found that BMI and total body fat (%) were the most significant predictors of fatality, among variables that also included silicosis positivity, history of TB and duration of exposure. Considering that malnutrition is an intermediate pathway for silicosis or TB leading to mortality, we excluded it from the model and found only TB as a significant contributor for mortality with an odds ratio of 12 (P<0.05, 95% CI (1.33, 107.92)) for association of mortality with TB.
DISCUSSION
The authors admit the lack of strong causal inference in this study owing to the absence of a control group and small sample size. In fact, recruiting and following up a suitable control group would have been next to impossible in the given circumstances at Shakarpur, which itself is a remote, underserved and resource poor area inhabited by mostly people below poverty line, in spite of being within the vicinity of the ancient port town of Khambhat. But the prospective nature and the quality of the data collected give the study some robustness in order for the authors to derive implications for possible interventions by health providers as well as policy makers.
It was earlier documented among stone quarry workers in India that their nutritional status was poor besides coexistence of silicosis, which is corroborated by our findings among the agate polishing workers. Malnutrition itself has been labeled as one of the factors associated with all cause mortality in silicosis victims.[4,10] The fact that males in our study have significantly lower nutritional status than the females as reflected in their BMIs needs further exploration although both male and female workers are engaged in the occupation and their mean and median duration of exposure are similar. Possibly the extent of debilitation due to both silicosis and other co-morbidities such as COPD from chronic smoking, which is not a marked phenomenon among women, may be higher in men than that in women. Malnutrition itself may be a dependent, independent, or intermediate variable with respect to other co-morbidities of silicosis.
Besides a lower body mass index, abnormal lung function itself has been documented to be a predictor of all cause mortality in silicosis, especially in sand stone quarries. The situation is no different than this at Shakarpur.[5] The mixed pattern of pulmonary function in the majority of participants can be due to coexisting chronic obstructive airway disease, for which smoking may be a significant risk factor independent of silicosis. As smoking history was difficult to elicit, we refrain from commenting on this issue. Local volunteers confirmed that the women participants were subjected to household smoke due to use of bio-mass fuel for cooking. While smoking and household smoke, both can be responsible for the co-existence of COPD among the participants, review of studies suggest evidence of chronic bronchitis and emphysema developing from chronic exposure to respirable silica dust and leading to obstructive pathology, which more or less explains our finding.[11] Yet, more robust studies would be needed to ascertain the association of COPD in these victims. For both malnutrition and abnormal lung function, TB is also an important co-morbidity, which is reflected in our study. An earlier study established that prevalence of active TB in the same population was at least 10.7% with more than three times higher odds ratio for smokers.[12] However, the results of regression analysis point towards the fact that TB is a strong candidate for targeted intervention among agate stone workers to prevent early mortality. The authors are of the opinion that irrespective of the small sample size, the longitudinal nature of the study definitely throws important clues associated with the mortality of the agate stone workers. Besides silicosis, we have documented important co-morbid conditions including TB and under nutrition debilitating the lives of the agate workers potentially leading to a large proportion of fatalities within less than 3 years from date of diagnosis. Treatment options for TB are simpler and cheaper than that of silicosis. Treatment of under nutrition is more complex because of association of poverty which is one of its known determinants.[13,14] Even the dosage of anti-TB drugs may vary with severe under nutrition. But the knowledge of under nutrition will definitely assist the physician in prescribing drugs for both TB and silicosis (e.g. steroids depend on body mass). Hence, in our opinion, suspected silicosis victims should be investigated early and aggressively treated for TB and under nutrition if diagnosed, irrespective of the silicosis status. This would go a long way in preventing or delaying morbidity and mortality among the agate workers and their relatives from various preventable and treatable co-morbidities if not from silicosis. Further, long-term follow-up studies are necessary to establish the hypothesis that TB and under nutrition may positively modify the association between silicosis and early mortality. Besides, such studies will help in developing both preventive and curative interventions not only for silicotics but also for other victims who die of causal interactions among multiple environmental, clinical and social factors.
Footnotes
Source of Support: The Charutar Arogya Mandal, Karamsad, and Peoples’ Training and Research Centre, Vadodara
Conflict of Interest: None declared.
REFERENCES
- 1.Jindal SK, Aggarwal AN, Gupta D. Dust-induced interstitial lung disease in the tropics. Curr Opin Pulm Med. 2001;7:272–7. doi: 10.1097/00063198-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Saiyed HN, Tiwari RR. Occupational health research in India. Ind Health. 2004;42:141–8. doi: 10.2486/indhealth.42.141. [DOI] [PubMed] [Google Scholar]
- 3.Ahmedabad: Prevention control and treatment of silicosis and Silico-tuberculosis in agate industry; [cited 2011 June 1]. National Institute of Occupational Health [Internet] Available from: http://icmr.nic.in/000004/project1/project.htm#results . [Google Scholar]
- 4.Ahmedabad: Silicosi; [cited 2011 June 1]. National Institute of Occupational Health [Internet] Available from: http://www.nioh.org/niohachiveprosilicosis1.htm . [Google Scholar]
- 5.Mathur ML. Pattern and predictors of mortality in sandstone quarry workers. Indian J Occup Environ Med. 2005;9:80–5. [Google Scholar]
- 6.Chaudhury N, Phatak A, Paliwal R, Raichaudhari C. Silicosis among agate workers at Shakarpur: An analysis of clinic-based data. Lung India. 2010 Oct;27:221–4. doi: 10.4103/0970-2113.71955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al-Ashkar F, Mehra R, Mazzone PJ. Interpreting pulmonary function tests: Recognize the pattern and the diagnosis will follow. Cleve Clin J Med. 2003;70:866–81. doi: 10.3949/ccjm.70.10.866. [DOI] [PubMed] [Google Scholar]
- 8.Hosking J, Metcalf BS, Jeffery AN, Voss LD, Wilkin TJ. Validation of foot-to-foot bioelectrical impedance analysis with dual-energy X-ray absorptiometry in the assessment of body composition in young children: the Early Bird cohort. Br J Nutr. 2006;96:1163–8. doi: 10.1017/bjn20061960. [DOI] [PubMed] [Google Scholar]
- 9.WHO expert consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 10.Madhavan P, Raj S. Budhapura ‘Ground Zero‘ Sandstone quarrying in India. India Committee of the Netherlands. [Cited 2011 June 1]. Available from: http://www.indianet.nl/budhpura.pdf .
- 11.Tiwari R, Sharma YK, Saiyed H. Tuberculosis among workers exposed to free silica dust. Indian J Occup Environ Med. 2007;11:61–4. doi: 10.4103/0019-5278.34530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Faye LR. Silica related disease: It's just not silicosis. Global Occupational Health Network (GOHNET) Newsletter. 2007. [Cited 2011 June 1]. Available from: http://www.who.int/occupational_health/publications/newsletter/gohnet12e.pdf .
- 13.Cheah WL, Muda WA, Zamh ZH. A structural equation model of the determinants of malnutrition among children in rural Kelantan, Malaysia. [cited 2011 June 1];Rural Remote Health. 2010 10:1248. Available from http://www.rrh.org.au/articles/subviewnew.asp?ArticleID=1248. Epub . [PubMed] [Google Scholar]
- 14.Khan Y, Bhutta ZA. Nutritional deficiencies in the developing world: current status and opportunities for intervention. Pediatr Clin North Am. 2010;57:1409–41. doi: 10.1016/j.pcl.2010.09.016. [DOI] [PubMed] [Google Scholar]


