Abstract
Background. Given sparse knowledge on dissemination, this study sought to explore key benefits, barriers and contextual factors that are perceived to be important to the adoption and implementation of the ‘Community Guide's’ evidence-based physical activity recommendations. Design. We conducted case studies in two states where extensive adoption and implementation of the Guide's recommendations have occurred and in two states where widespread dissemination has lagged. Interviews (n = 76) were semi-structured and included both quantitative and qualitative methods. Participant perceptions from the following areas were examined: (i) priority of physical activity, (ii) awareness of and ability to define the term ‘evidence-based approaches’ and (iii) awareness, adoption, facilitators, benefits, challenges and barriers to Guide adoption. Results. Key enabling factors among high capacity states included: funds and direction from the Centers for Disease Control and Prevention; leadership support; capable staff; and successful partnerships and collaborations. Restraining forces among low capacity states included: the Guide recommendations being too new; participants being too new to current job; lack of time and training on how to use the Guide recommendations; limited funds and other resources and lack of leadership. Conclusion. To be effective, we must gain an understanding of contextual factors when designing for dissemination.
Introduction
Lack of physical activity is closely linked with incidence of several chronic diseases and a lower quality of life [1, 2]. To help reduce the burden of physical inactivity, the Task Force on Community Preventive Services has produced a set of evidence-based approaches for promoting physical activity in its systematic review, the Guide to Community Preventive Services (the Community Guide) [3, 4]. In the Community Guide, there are eight specific intervention strategies found to have sufficient or strong evidence of effectiveness [3, 4]. Too often, the products of research (e.g. the Community Guide) do not get disseminated or translated into community settings where the information is likely to be applied [5].
These effective intervention strategies can be implemented in community settings through the efforts of numerous agencies, organizations and individuals. Data are presently lacking on effective methods of disseminating physical activity interventions in community settings via public health agencies. State and local health departments are in key positions to promote these evidence-based physical activity interventions. Their role is crucial because of their ability to assess public health problems, develop appropriate programs or policies and assure that evidence-based programs and policies are effectively delivered and implemented [6, 7].
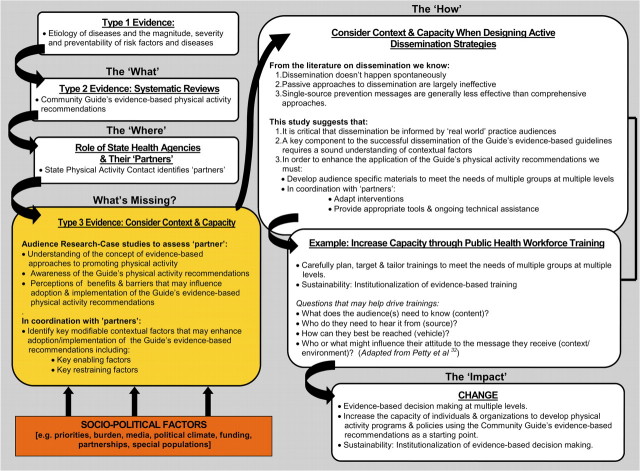
We know that the dissemination of effective programs and policies is likely to occur in stages [8] and that factors that influence dissemination include: the actions of the researchers, characteristics of practitioners and the specific methods used for communicating and disseminating an intervention [9–12]. There is a gap between research and practice in the systematic dissemination of the Guide's physical activity recommendations [13]. Dissemination strategies are based on different types of evidence. For example, Brownson et al. [14, 15] categorize two types of evidence: ‘Type 1’ evidence (etiologic research) points to the fact that ‘something should be done’ and ‘Type 2’ evidence (intervention research) can help to determine that ‘this should be done’. For evidence to inform public health policy and practice, Rychetnik et al. proposed a third category that highlights the importance of descriptive and/or qualitative information. ‘Type 3’ evidence tells us ‘how something should be done’. Type 3 evidence shows how and under what contextual conditions interventions were implemented and how they were received. Although invaluable to practitioners and policy makers, type 3 evidence is often unavailable from published papers and intervention reports [16]. Sparse knowledge exists regarding effective approaches for dissemination of research-tested interventions among ‘real-world’ practice audiences. Authors agree that type 3 evidence is sorely lacking and may prove to be the critical link to the successful dissemination and application of the Guide's evidence-based physical activity recommendations [16]. Rychetnik [17] suggests, and authors agree, that we must improve the quantity, quality and availability of type 3 evidence [16]. Many of these type 3 factors are contextual variables such as organizational culture, leadership, political challenges, funding challenges and workforce training needs [17]. Any of these could justify adaptation of evidence-based interventions to fit contextual conditions [17].
Researchers get caught in a ‘one size fits all’ process of dissemination, failing to tailor the content, timing, setting and format of dissemination to unique real-world settings [18]. Disseminating evidence-based interventions is therefore an art that needs to take contextual conditions into account [18]. It is critical that dissemination science be informed by real-world practice audiences (e.g. public health practitioners). A key component to the successful dissemination of the Guide's evidence-based guidelines requires a sound understanding of contextual factors that may yield the information that will enable successful translation of the Guide's recommendations into knowledge and insight that is actionable and relevant (i.e. type 3 evidence).
This study was undertaken to better understand (type 3 evidence) as a crucial first step in the dissemination of physical activity interventions, focusing particularly on the evidence-based reviews in the Community Guide. Our exploratory study provides a method to inform evidence-based dissemination strategies that can be adapted to other settings and risk factors. Therefore, the purposes of this article are to: (i) examine two states where extensive adoption and implementation of the Community Guide's physical activity recommendations have occurred [High Capacity (HC)] and two states where widespread dissemination has lagged [Low Capacity (LC)]; (ii) describe real-world contexts by sharing participant perceptions related to: personal commitment to physical activity; awareness of evidence-based approaches including the Guide; adoption of the Guide's physical activity recommendations; facilitators, benefits, challenges and barriers to Guide adoption as well as contextual factors that have the potential to influence ‘if’ and ‘how well’ the promising interventions in the Guide are implemented and (iii) suggest strategies for changing behavior that strengthen the driving forces and weaken the restraining forces to the adoption and application of the Guide's evidence-based physical activity recommendations that can then be incorporated into a comprehensive program for improving outcomes.
Methods
Selecting states
Case studies are a useful research tool for explanatory rather than predictive questions, they allow one to observe changes in a real life setting, can guide future programs and are most useful when the investigator has relatively little opportunity to manipulate the behavior of interest (e.g. non-experimental conditions) [19]. We conducted four case studies from January 2005–April 2005, as a component of a larger study [20, 21]. A quantitative baseline survey assisted us in choosing sites for case studies [20, 21]. As frequently used in case studies [22], we used purposive sampling—that is, we examined two states where extensive adoption and implementation of the Guide's physical activity recommendations have occurred and two states where widespread dissemination has lagged. In addition, we examined the following factors related to capacity and disease burden: funding level and attitude toward physical activity promotion; level of physical activity; level of obesity; death rate related to chronic disease and geographic location. By examining extreme cases, we maximized the likelihood that the qualitative approach would illustrate key contextual enabling factors and barriers to change.
Sample
A three-level-modified snowball sampling method was used to identify ‘physical activity partners’ for our study. The Physical Activity Contact person was contacted in the four selected states. These individuals were identified via the Centers for Disease Control and Prevention's State-based Physical Activity Program Directory [23] and through leadership information listed within the Chronic Disease Directors within each state health department [24]. The role of the Physical Activity Contact person is to lead and/or facilitate activities in promoting physical activity, serve as a clearinghouse for information and develop new initiatives—it is a set of responsibilities rather than a specific job title. The physical activity contact was chosen to fill out a list of physical activity partners because she/he was likely to be the individual most familiar with physical activity programs, policies and priorities within each state health department. Project details were sent via email and follow-up phone calls were made to answer questions and to schedule interviews. As part of the interview, participants were asked to identify ‘champions’ for physical activity in their state, thus expanding the sample group of key partners. Champions that were mentioned two or more times were contacted and interviewed when possible.
Interview guide
Based on previous literature and the project team input [20, 25–28], an initial semi-structured interview guide was developed that included 64 questions. Based on project team feedback, the draft instrument was revised to include 25 questions covering seven major areas: (i) biographical information; (ii) awareness of the importance of physical activity/obesity; (iii) political climate and support for physical activity; (iv) financial climate related to physical activity; (v) existing physical activity programs; (vi) awareness, adoption, implementation and maintenance of the Community Guide and (vii) physical activity promotion networks and champions. (The interview guide is available from the first author on request.) The draft interview guide was pre-tested for length, clarity and organization via phone interviews with staff members at the Missouri State Department of Health and Senior Services. Revisions were made and the revised interview guide was then pre-tested in-person with staff members at the St Louis County Health Department. Cognitive response testing is routinely used in refining questionnaires to improve the quality of data collection [29–31]. In order to determine (i) ‘question comprehension’ (What does the respondent think the question is asking? and What do specific words or phrases in the question mean to the respondent?); (ii) ‘information retrieval’ (What information does the respondent need to recall from memory in order to answer the question? and How do they retrieve this information?) and (iii) ‘decision processing’ (How do they choose their answer?) [29–31], we examined the draft interview guide using cognitive response testing with staff members at the St Louis County Health Department.
Data collection
We collected the majority of data via semi-structured face-to face interviews (n = 59); others were conducted via telephone interviews to accommodate participant schedules (n = 17). We used a combination of quantitative and qualitative methods. Qualitative methods gave us the opportunity to collect rich contextual information along with corroboratory evidence. For example, if during the interview, it was noted that Guide recommendations had been incorporated into the objectives of a particular program in the health department; we collected a copy of that program's objectives. Using key informant methods [8, 19], we conducted interviews with 16–24 ‘key informants’ from each site. Key informant interviews are one-on-one interviews conducted with opinion leaders who have expertise in the area being studied. In our study, each contributed a unique perspective related to physical activity programs and/or policies. We conducted a total of 76 interviews with an average interview length of 50 min.
Analysis
Interviews were professionally transcribed, edited and imported into NUD*IST 6 (QSR International Inc. NUDIST 6.0 Durham, UK, 2002). We developed an outline of a qualitative analysis codebook that was based on the topic areas and interview questions. Codes were applied to the text units of each transcript. We defined a unit as a block of text containing both the interviewer's question and the participant's response. Multiple codes could be assigned to each text unit depending on the content and new codes were added as needed.
Four team members were trained on coding to ensure reliability among raters. Coders were assigned transcripts to code independently, developing the codebook as needed to capture new themes and subcategories. Updated codebooks were distributed after each coding session. Coding pairs systematically exchanged transcripts and checked codes, noting any discrepancies and making notes of anything they would have coded differently. The team met to discuss each transcript and to address any coding discrepancies. Final coding decisions were made in the team setting; reaching consensus was the goal. Raters created a section called ‘coder notes’ which served as a summary for major themes, patterns and insights. Coded interviews were entered into a database. A check was made to assess consistency across entered codes and those on the original data documents. After final reports were run for each state, each team member summarized findings for a subset of questions for each state. Thematic content analysis was used to analyze the data by topic. Emerging themes were identified from the aggregated responses for a particular code or topic. Once analysis of state-specific data was complete, themes were examined across all four states. In the results section, selected thematic results are presented, supporting quantitative analyses and representative quotes from the interviews.
Results
Participant characteristics
Participants were from varying backgrounds including state/local public health professionals/practitioners; contractors/grantees; coalitions; voluntaries and advocacy groups; other state agencies; advisory and consulting agencies; as well as several policy-makers. Table I summarizes characteristics of the sample. The majority of interviews were completed by a program manager/administrator. Almost 50% of HC and almost 60% of LC participants worked in their current position for <5 years. In contrast, only a small percentage of participants in both categories worked in their current position for >10 years.
Table I.
Characteristics of full sample, high capacity and low capacity case study participants, 2005
| Characteristic | Full sample, n (%) | High capacity, n (%) | Low capacity, n (%)a |
| Job title | |||
| Program manager/administrator | 49 (63) | 23 (56) | 26 (70) |
| Health educator | 4 (5) | 3 (7) | 1 (3) |
| Epidemiologist | 1 (1) | 1 (2) | — |
| Division or bureau head | 4 (5) | 2 (5) | 2 (5) |
| Department head | 2 (3) | 1 (2) | 1 (3) |
| Other | 18 (23) | 11(27) | 7 (19) |
| Years working in current position | |||
| <2 years | 17 (22) | 8 (20) | 9 (24) |
| 2 to <5 years | 25 (32) | 12 (30) | 13 (35) |
| 5 to <10 years | 24 (31) | 15 (37) | 9 (24) |
| 10 to <15 years | 7 (9) | 4 (10) | 3 (8) |
| 15 or more years | 5 (6) | 2 (5) | 3 (8) |
| Years working in agency/organization | |||
| <2 years | 12 (15) | 5 (12) | 7 (19) |
| 2 to <5 years | 21 (27) | 12 (29) | 9 (24) |
| 5 to <10 years | 21 (27) | 10 (24) | 11 (30) |
| 10 to <15 years | 9 (12) | 5 (12) | 4 (11) |
| 15 or more years | 15 (19) | 9 (22) | 6 (16) |
| Percentage of time spent working in physical activity programs | |||
| <10% | 6 (8) | 3 (7) | 3 (9) |
| 10 to <25% | 21 (28) | 11 (27) | 10 (29) |
| 25 to <50% | 17 (22) | 8 (20) | 9 (26) |
| 50 to <75% | 15 (20) | 11 (27) | 4 (11) |
| 75–100% | 16 (21) | 7 (17) | 9 (26) |
| Don't know/NA | 1 (1) | 1 (2) | — |
Two participants from LC cases brought program managers to the interviews to answer questions related to specific physical activity programs. We included them when collecting job title and years working in current position and agency/organization. For the remaining questions, only the lead participant responded.
Qualitative findings
Personal commitment
Passion for physical activity.
An overwhelming majority of participants in both HC and LC states reported that physical activity was a priority in their lives both personally and professionally. Qualitative methods allowed participants an opportunity to express their enthusiasm, passion and personal commitment to physical activity:
Physical activity is very important … it's my profession … my responsibility; it's what I'm advocating for. (HC1)
Participants ‘walk the walk’.
HC and LC capacity participants clearly demonstrated that they don't just talk about the importance of physical activity; they ‘walk the walk’. The following comment reflects participant's enthusiasm for physical activity and a commitment to ‘practicing what they preach’:
I'm not one to just tell other people they need to be active; I actually practice it … I usually work out four to five days a week. (LC2)
Awareness
Awareness of evidence-based approaches.
Awareness of the term ‘evidence-based approaches to promoting physical activity’ was high among participants of both HC and LC states (Table II). The majority of participants demonstrated a clear understanding of what an evidence-based approach is when they were asked to define it. Most felt that it was an approach based on making decisions about programs and policies that are based on an evaluation of reliable data. The following quote provides a sample definition:
Evidence-based to me, may mean something different than others that have PhD's in public health. To me, it means there's a science; there's been an evaluation done … these are effective ways of doing what you need to do to get behavior change in the folks you're serving. (LC1)
Table II.
Participant knowledge of: (i) ‘evidence-based approaches to promoting physical activity’ and (ii) the Community Guide's evidence-based physical activity recommendations, 2005
| Knowledge or skill | HC (n = 41) | LC (n = 35) | P-value for difference in % |
| Awareness of the term ‘evidence-based approaches to promoting physical activity’ | 39/41 (95.1%) | 32/35 (91.4%) | 0.259 |
| Ability to define ‘evidence-based approach’ | 37/41 (90.2%) | 29/34 (85.3%) | 0.258 |
| Awareness of the Community Guide's evidence-based physical activity recommendations | 26/41 (63.4%) | 10/35 (28.6%) | 0.001 |
| Awareness of existing programs based on the evidence-based physical activity recommendations outlined in the Community Guide | 14/41 (34.1%) | 5/35 (14.3%) | 0.023 |
| Read or seen physical activity materials of Guide | 14/41 (34.1%) | 5/35 (14.3%) | 0.023 |
| Visited Community Guide website | 16/41 (39.0%) | 4/35 (11.4%) | 0.003 |
| Printed physical activity materials from the Community Guide website | 12/41 (29.3%) | 4/35 (11.4%) | 0.028 |
| Attended training to learn about the physical activity section of the Community Guide | 4/41 (9.8%) | — | — |
| Attended professional meeting where the physical activity section of the Community Guide was discussed | 13/41 (31.7%) | 3/35 (8.6%) | 0.007 |
Awareness of the Community Guide.
Table II illustrates the level of awareness among participants regarding the Guide's evidence-based physical activity recommendations. The majority (63%) of participants of HC states were familiar with the recommendations. In contrast, only 29% of LC participants were familiar with the Guide's physical activity recommendations as illustrated by the following comment:
I've heard of the Guide, but I don't think I've used it though … I'll definitely take a look at it … I'm pretty new in the game and didn't happen to run across it. (LC1)
How participants learned about the Community Guide.
The majority of HC participants reported that they learned about the Guide through the Centers for Disease Control and Prevention (CDC). A small number of participants reported that they learned about the recommendations through their Division of Public Health, the Internet, peers, conferences, University of Kansas Community Toolbox, the American College of Sports Medicine, Prevention Research Centers and through professional trainings. LC participants, who were aware of the Guide, appeared to learn about them through passive dissemination strategies as illustrated by the following explanation:
As the CDC physical activity contact person, we get list serves … I found out about the Guide by clicking on the links to look at what they're talking about. (LC1)
Several LC participants indicated that they were unclear about how they learned about the Guide:
How did I become aware of the Guide? I'm always doing research on stuff, and I probably just ran across it. (LC2)
Adoption
Are physical activity programs based on Guide recommendations?
Approximately 34% of HC participants and 14% of LC participants reported existing programs based on the evidence-based physical activity recommendations outlined in the Guide (Table II). The following participants' quote provides a sample response to this question:
Point of decision prompts is an example of an evidence-based physical activity recommendation that's being done and promoted. The grants we give to communities … in all of those we use the Guide. (HC2)
It was apparent that many LC participants were unsure whether their existing physical activity programs were based on the Guide's recommendations as illustrated by the following comment:
I've heard of the Guide. I don't believe any existing physical activity programs are based on it. I'm not as familiar with it … I'm relatively new. (LC1)
The ‘HOW’: HC participants share key facilitators to successful Guide adoption.
Participants from HC states described four key enabling factors to successful adoption and implementation of the Guide's physical activity recommendations. Facilitators cited most often included:
Sustained funding and direction from the CDC
Leadership support
Staff that is capable, dedicated and motivated
Successful partnerships/collaborations
In addition to the key enabling factors, participants of HC states reported the following facilitators: training, assistance and motivation of the staff; incentives for and willingness of the target population to engage and buy-in from the community.
Adoption: How is the evidence being applied?
Participants who reported that they personally used the Guide's findings in their work used them to plan physical activity programs, for strategic planning, to develop grants, to support initiatives and for training purposes. This viewpoint is best stated in the quote below:
The Guide is used when we plan physical activity programs; it is also used for strategic planning, grant planning and for training purposes (HC2).
Benefits
Why apply the Guide's physical activity recommendations?
Participants were asked to share perceptions regarding why the Guide's physical activity recommendations have been incorporated into their agency/organization. HC participants cited the following reasons most often:
The Community Guide is evidence-based
The Community Guide is recommended by the CDC
Adopting the Guide's recommendations increases the likelihood of being funded
The following quote offers a sample HC participant response illustrating reasons why the Guide's recommendations were incorporated into her agency/organization:
We perceive the Guide as very authoritative … and we want to use the best that's out there. We want to use what's effective. (HC2)
One perspective suggested that adopting these guidelines increases the likelihood of being funded, adds strength to initiatives and is the best resource available.
The Guide's physical activity recommendations have been incorporated into our agency because they're evidence-based and they're accepted enough, that it's tough to get funding unless you're consistent with them. (HC1)
LC participants suggest benefits to applying Guide recommendations.
LC participants suggested the following benefits for incorporating the Guide's physical activity recommendations:
To increase credibility
To contribute to consistency
Because they're evidence-based
To increase the likelihood of being funded
LC participants provide the following examples of benefits to applying the Guide's recommendations:
My knowledge of the Guide is really limited … recommendations haven't been incorporated. Benefits to incorporating Guide recommendations would be that we're using something that has credibility … (LC1)
Challenges and barriers
HC participants describe key challenges to Guide adoption.
Even though the majority of HC participants reported new funding for physical activity programs and policies, there were participants that reported organizational budget cuts. Approximately 39% of HC participants reported budget cuts that have affected their organization's ability to develop and implement physical activity programs and policies. Viewpoints shared included challenges regarding sustaining funding, the possibility of future budget cuts and effects of budget cuts to staff. Others described the effect that budget cuts can have on long-term progress of physical activity efforts:
How have budget cuts affected my agency's ability to develop and implement physical activity programs and policies? It disables you is what it does … it hampers the conversation, the progress, the dialogue … everything that you need to move forward. (HC1)
Other barriers cited by HC participants included: lack of resources; the need to focus on partnership development, especially with those considered to be non-traditional such as transportation organizations and the challenges of reaching special populations as illustrated by the following comment:
We are struggling reaching our minority populations. When you look at our state, we meet several of the Healthy People 2010s already. But when you look at it broken into race/ethnicity we don't. (HC1)
LC participants describe key barriers to Guide adoption.
Those participants of LC states (Table II), who knew about the evidence-based physical activity recommendations outlined in the Guide, reported that few existing programs are based on these recommendations. These individuals provided the following explanations:
The Community Guide recommendations are too new
Participant is too new to current job
Lack of familiarity with the Community Guide
Lack of time and training on how to use the Guide recommendations
The Community Guide was not available at the time of program implementation
Lack of funds and resources
Need for leadership
The following comments provide a sample of responses from LC participants to explain why Guide recommendations are ‘not’ being applied:
I've heard of the Guide. We haven't utilized it. Why has it not been incorporated? I think just lack of time and training on how to use the resources. (LC2)
Leadership wasn't onboard at the beginning; we've been slow to take off. Funding is also a roadblock … leadership support is the whole key when you're working at a public health agency. (LC2)
Another common perspective described the challenge of wearing ‘many hats’ within organizations. Many public health practitioners are responsible for multiple tasks as illustrated by the following comment:
Sometimes those of us who oversee physical activity programs have multiple roles and duties … we wear two, three, four, five hats in our agency and we're only one person. (LC2)
Context counts: potential facilitators to Guide adoption
The influence of the ‘Obesity Epidemic’.
An overwhelming majority of participants in both HC and LC states reported that developing physical activity programs to address the obesity epidemic and chronic disease is a way to develop interest, political support and funding for physical activity programs.
I think pointing out the scale or scope of the obesity epidemic, how pervasive it is … I don't know how better to generate interest and support for physical activity programs. It's a pay now or pay later situation. (LC1)
When physical activity is framed in the context of disease management or prevention … it provides more leverage in the minds of policy and decision-makers. (HC2)
The media's powerful effect on public health priorities.
Participants across HC and LC states report that thanks to media attention, obesity and physical activity have become public ‘hot topics’. The importance of the media in shaping the political, policy, organizational and public agenda related to obesity and on increasing physical activity is clearly illustrated by the following participant comments:
… with increased media attention and increased awareness of the childhood obesity epidemic … it's become more of a priority because it's in the limelight …(LC1)
We are one the more fit states … but our kids are getting fat at the same rate as anyone else … but I think the climate is good for intervention because of the media around obesity. (HC1)
Political support for physical activity.
Participants across HC and LC states reported varying levels of political support for physical activity, but the majority of participants across sites agreed that improvements could be made if verbal support for physical activity was backed by funding as illustrated by the following quotes:
We have verbal support for physical activity programs and policies. We don't have funding … you would be hard pressed to find a politician these days who wouldn't line up behind increased physical activity for children … but, are they going to put it up against changes in academic performance scores? (HC1)
I think the Governor and the Legislature are aware of the problems and issues with physical inactivity, obesity, chronic diseases … but because of funding limitations, they're not really ready to put their money where their mouth is … (LC1)
Educating politicians: a crucial strategy to gain political support.
An interesting perspective shared by participants of HC states is the need to educate politicians in order to gain their support for physical activity programs and policies. Participants shared the following perspectives:
We haven't done a good job of educating political leaders … we've got to do a better job … we make the mistake of not making it clear in budgets what they're actually cutting … it's called health promotion money and it's not clear that it's physical education and nutrition to fight obesity and overweight. (HC2)
The obesity epidemic and chronic illness has forced people to take a look at physical activity … I think people who make decisions want to see the ‘evidence’. (HC1)
Perspectives from policy-makers.
Only a few policy makers were included in ‘physical activity partner’ lists across sites, but their perspective was invaluable and demonstrated how decision makers can be powerful advocates in the promotion of physical activity policies if they are armed with the evidence. A policy advisor reported that she was not familiar with evidence-based approaches nor was she familiar with the Guide. She offered the following explanation:
I haven't heard of evidence-based approaches to promoting physical activity … I'm fairly new to all this … we are doing all we can to learn about programs and methods of measuring outcomes and evidence-based approaches. (LC1)
A senator we interviewed told us that education from a credible source such as the CDC could be a key factor in influencing priorities. He reported looking at long-term benefits when making decisions and also described a powerful strategy to get legislators on board—the power of combining stories with statistics.
I've heard a lot of speeches. I've been in the business for over 20 years, there's not very much I'm impressed with. But I think that personal stories and statistics are two of the best way to perk somebody's interest. (LC2)
Discussion
This study was undertaken to better understand the importance of studying context (type 3 evidence) as a crucial step in the dissemination of physical activity interventions, focusing particularly on the evidence-based reviews in the Community Guide. Contextual factors have the potential to influence how well the evidence-based interventions in the Guide are implemented. Our exploratory study provides a method to inform evidence-based dissemination strategies that can be adapted to other settings and risk factors. One-size does not fit all as illustrated by our study. We must learn about context and capacity before attempting to actively disseminate the Guide's recommendations. Case studies provide a method to learn more about context and capacity from the target audiences. Building on these cases, we propose a framework for rethinking the design of dissemination (Fig. 1). Our proposed framework illustrates the need to more fully consider context and capacity when designing active dissemination strategies in order to impact population-level change. There is a need to identify key contextual factors that may enhance adoption and implementation of the Guide's evidence-based recommendations (Fig. 1 in particular, the highlighted box).
Fig. 1.
Proposed framework: rethinking the design of dissemination. This figure is available in black and white in print and in colour at Health Education Research online.
For physical activity researchers and practitioners, we have effective intervention approaches and analytic tools available for use, such as the Community Guide. However, it is now widely recognized that the mere existence of scientific knowledge is not sufficient to ensure effective application. Public health practitioners are on the front lines experts on how to best disseminate what we know works. We should invest the time and money to learn from this key stakeholder group. They hold the keys on how to best translate and disseminate evidence-based strategies, even when they don't know about them. Identifying physical activity partners and assessing competencies in evidence-based decision making may be a way to inform how best to train our public health workforce in the use of evidence-based decision making. Dissemination of the recommendations should then be carefully planned, targeted toward and tailored to meet the needs of the intended audiences [32, 33] (Fig. 1). Successful dissemination of the Guide's evidence-based guidelines requires a sound understanding of contextual factors, which may yield the necessary information to enable successful translation of the recommendations into knowledge and insight that is actionable and relevant.
Our findings build upon findings from previous research showing that dissemination of interventions occurs as a series of phases rather than as one event [8, 20, 21, 34, 35]. Dissemination does not stop at the level of initial uptake; further steps are critical to ensure the long-term utilization of an intervention [36]. As described earlier, understanding context (type 3 evidence) [16] and delivery context for the intervention are essential for the success of the dissemination and are closely linked to the concepts of fidelity and adaptation [37]. Active dissemination methods are crucial to success in this phased approach; however, few studies have been done on the dissemination of effective physical activity interventions [38].
Existing frameworks do not capture variables in local conditions. For example, Wandersman et al. [39] have developed an ‘Interactive Framework for Dissemination (ISF)’ which is intended to be a heuristic for understanding key systems, key functions and key relationships relevant to the dissemination and implementation process. What is missing, however, is the broader context not captured by the systems identified within the ISF framework. Wandersman acknowledges the need to include these important contextual factors in order to capture the broader context not fully captured by the systems identified within the framework [39]. Our framework (Fig. 1) seeks to fill this gap. Those identified as key informants by the State Physical Activity Contact are the experts. They hold the ‘keys’ to effective dissemination of the Community Guide's physical activity recommendations. Change requires leadership and it is important to get the appropriate leaders ‘on board’ early in the dissemination process. Identifying gatekeepers is an important dissemination strategy in order to find out how information is channeled. It is also important to consider ‘opinion leaders’, that is, people to whom others listen. Conducting qualitative studies to assess state/local context are critical to ensure that the Community Guide's physical activity recommendations fit with local conditions. Dissemination activities that build on existing individual and organizational capacity of targeted agencies and populations will be more likely to succeed.
We should consider strategies of dissemination that take into account the real-world challenges faced by practitioners in a climate of uncertain resources and increasing accountability. Green and Glasgow [13] suggest that ‘if we want more evidence-based practice, we need more practice-based evidence’. Collaborative partnerships between researchers, practitioners, advocacy groups, policy-makers and ‘non-traditional’ partners such as those in planning, transportation and the media are crucial in bridging the gap between discovery and application.
It is important to note several limitations. Even though we attempted to develop a reliable and comprehensive instrument, there were few models on which to base physical activity items. Consequently, we had to develop numerous questions de novo. The data are from only four states. Second, while we are confident about the coverage and level of agency participation among states, in many cases, only one representative was interviewed per agency/organization. Although these key informants were the individual's most familiar with their agencies' physical activity efforts, it provided only a single viewpoint. Modified snowball sampling methods are subject to biases; however, this technique allowed respondents to drive the research sample that allowed us to learn about the social networks connecting the physical activity networks. Despite these limitations, our study provides valuable information regarding the importance of contextual information in order to ensure the successful dissemination of evidence-based interventions such as those outlined in the Guide.
Practice-relevant dissemination of evidence-based interventions is highly innovative, yet is an area that remains largely uncharted. Sparse knowledge exists regarding effective approaches for dissemination of research interventions among real-world practice audiences. Case studies are a useful research tool for explanatory rather than predictive questions; they allow one to observe changes in a real life setting and can guide future programs. Our study suggests that disseminating evidence-based guidelines are not a ‘one size fits all’ process and will require a blend of ‘science and art’ in order to be successful. Contextual factors are likely to be important predictors of successful adoption and implementation of evidence-based guidelines. Learning about each state's unique context will help to understand the key modifiable enabling and restraining forces that are present when attempting to disseminate the Guide's physical activity recommendations. Identifying the partners who possess this expertise is essential. They may not have the evidence but they hold the keys to successful application of evidence-based guidelines such as the Community Guide's physical activity recommendations. What they do possess is the expertise of local contextual factors which are the keys to successful dissemination of what we know works. Audience research using qualitative methods can provide the opportunity for researchers to learn from the experts about how best to share the ‘evidence’ with those who have expertise of local contexts and populations they serve. These are the front line agents who can actually turn the science into action. Several emerging areas of study that could be considered in combination with our proposed framework include:
‘Establishing marketing and distribution infrastructure’ to disseminate evidence-based public health programs and policies more efficiently and effectively. To date, marketing and distribution systems have received little attention in public health conversations about putting science into action. Reframing the dissemination challenge to reflect this perspective and investing in system infrastructure to implement it has the potential to transform public health practice [40].
‘Adopting the concept of knowledge brokers’, a knowledge translation and exchange strategy emerging in Canada to promote interaction between researcher and end users, as well as to develop capacity for evidence-informed decision making [41]. Dobbins et al. suggest that strategies that are more interactive and involve face-to-face contact show promising results and the involvement of decision makers in the research process is associated with a higher degree of research uptake.
Reframing the dissemination challenge to reflect the issues outlined in this article has the potential to transform public health practice. We invite researchers, practitioners and policy-makers to address the issues outlined in this study to bridge the gap between new knowledge on effective evidence-based physical activity interventions and the widespread application of these approaches into real-world settings where they can truly ‘make a difference’ in improving health. If we can document effective ways to make practice more evidence based, the impact of prevention research will be enhanced. Much work has gone into the development of the Community Guide. We must ensure that the products of this important research are applied. Perhaps, one of our study participants says it best:
Our work is not all science-based or proven effective, but there's lots of energy here … it's up to the people at the state and their federal partners to recommend what's evidence-based, to provide technical assistance and to provide methods on evaluating and reporting … . we don't want to waste our time on ineffective programming …
Human Participant Protection
Human subjects approval was obtained from St Louis University Institutional Review Board.
Funding
Centers for Disease Control and Prevention (U48/DP000060) (Prevention Research Centers Program, Special Interest Project 10-02).
Conflict of interest statement
None declared.
Acknowledgments
The authors are grateful to the participants who generously shared their time and expertise with this project. The authors acknowledge the advice and assistance with this study from Mary Massey-Douglas, Jimmy Newkirk, Rachel Oys and Tom Tracy. We also thank Graduate students: Borsika Rabin, Corrie Joshu and Katie Brown.
References
- 1.US Department of Health and Human Services. Physical Activity and Health. A Report of the Surgeon General. Atlanta, GA: US Department of Health and Human Services; Centers for Disease Control and Prevention; 1996. [Google Scholar]
- 2.Zaza S, Briss PA, Harris KW, editors. The Guide to Community Preventive Services: What Works to Promote Health? New York, NY: Oxford University Press; 2005. [Google Scholar]
- 3.Heath GW, Brownson RC, Kruger J, et al. The effectiveness of urban design and land use and transport policies and practices to increase physical activity: a systematic review. J Phys Act Health. 2006;3(Suppl. 1):S55–76. doi: 10.1123/jpah.3.s1.s55. [DOI] [PubMed] [Google Scholar]
- 4.Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity. A systematic review(1,2) Am J Prev Med. 2002;22(4 Suppl. 1):73–107. doi: 10.1016/s0749-3797(02)00434-8. [DOI] [PubMed] [Google Scholar]
- 5.MacLean DR. Positioning dissemination in public health policy. Can J Public Health. 1996;87(Suppl. 2):S40–3. [PubMed] [Google Scholar]
- 6.Institute of Medicine. The Future of the Public's Health in the 21st Century. Washington, DC: National Academies Press; 2003. [Google Scholar]
- 7.IOM. Committee for the Study of the Future of Public Health. The Future of Public Health. Washington, DC: National Academy Press; 1988. [Google Scholar]
- 8.Rogers EM. Diffusion of Innovations. 5th edn. New York, NY: Free Press; 2003. [Google Scholar]
- 9.Basch CE. Research on disseminating and implementing health education programs in the schools [Review] Health Educ. 1984;15:57–66. [PubMed] [Google Scholar]
- 10.Murray DM. Dissemination of community health promotion programs: the Fargo-Moorhead Heart Health Program. J Sch Health. 1986;56:375–81. doi: 10.1111/j.1746-1561.1986.tb05776.x. [DOI] [PubMed] [Google Scholar]
- 11.Huberman M. Linkage between researchers and practitioners: a qualitative study. Am Educ Res J. 1990;27:363–91. [Google Scholar]
- 12.Lomas J. Diffusion, dissemination and implementation: who should do what? Ann N Y Acad Sci. 1993;703:226–37. doi: 10.1111/j.1749-6632.1993.tb26351.x. [DOI] [PubMed] [Google Scholar]
- 13.Green LW, Glasgow RE. Evaluating the relevance, generalization, and applicability of research; issues in translation methodology. Eval Health Prof. 2006;29:126–53. doi: 10.1177/0163278705284445. [DOI] [PubMed] [Google Scholar]
- 14.Brownson RC, Gurney JG, Land GH. Evidence-based decision making in public health. J Public Health Manag Pract. 1999;5:86–97. doi: 10.1097/00124784-199909000-00012. [DOI] [PubMed] [Google Scholar]
- 15.Brownson RC, Baker EA, Leet TL, et al. Evidence-based Public Health. Oxford, UK: Oxford University Press; 2003. p. 7. [Google Scholar]
- 16.Rychetnik L, Hawe P, Waters E, et al. A glossary for evidence based public health. J Epidemiol Community Health. 2004;58:538–45. doi: 10.1136/jech.2003.011585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175–201. doi: 10.1146/annurev.publhealth.031308.100134. [DOI] [PubMed] [Google Scholar]
- 18.Lomas J. Improving Research Dissemination and Uptake in the Health Sector: Beyond the Sound of One Hand Clapping. Hamilton, Ontario, Canada: McMaster University Centre for Health Economics and Policy Analysis, Policy Commentary C97-1; 1997. [Google Scholar]
- 19.Yin RK. Case Study Research Design and Methods. Newbury Park, CA: Sage Publications; 2003. [Google Scholar]
- 20.Brownson RC, Ballew P, Dieffenderfer B, et al. Evidence-based interventions to promote physical activity: what contributes to dissemination by state health departments. Am J Prev Med. 2007;33(1 Suppl.):S66–73. doi: 10.1016/j.amepre.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Brownson RC, Ballew P, Brown KL, et al. The effect of disseminating evidence-based interventions that promote physical activity to health departments. Am J Public Health. 2007;97:1900–7. doi: 10.2105/AJPH.2006.090399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Balbach ED. Using Case Studies to do Program Evaluation. Sacramento, CA: California Department of Health Services; 1999. [Google Scholar]
- 23.Centers for Disease Control and Prevention. State-based Physical Activity Program Directory. Centers for Disease Control and Prevention. Available at: http://apps.nccd.cdc.gov/DNPAProg/. Accessed: 3 February 2010. [Google Scholar]
- 24.Chronic Disease Directors. Chronic Disease Directors. Expanding Public Health Horizons. Available at: www.chronicdisease.org. Accessed: 3 February 2010. [Google Scholar]
- 25.Brink SG, Basen-Engquist KM, O'Hara-Tompkins NM, et al. Diffusion of an effective tobacco prevention program. Part I: evaluation of the dissemination phase. Health Educ Res. 1995;10:283–95. doi: 10.1093/her/10.3.283. [DOI] [PubMed] [Google Scholar]
- 26.Parcel GS, O'Hara-Tompkins NM, Harrist RB, et al. Diffusion of an effective tobacco prevention program. Part II: evaluation of the adoption phase. Health Educ Res. 1995;10:297–307. doi: 10.1093/her/10.3.297. [DOI] [PubMed] [Google Scholar]
- 27.Steckler A, Goodman RM, McLeroy KR, et al. Measuring the diffusion of innovative health promotion programs. Am J Health Promot. 1992;6:214–24. doi: 10.4278/0890-1171-6.3.214. [DOI] [PubMed] [Google Scholar]
- 28.Riley BL. Dissemination of heart health promotion in the Ontario Public Health System: 1989-1999. Health Educ Res. 2003;18:15–31. doi: 10.1093/her/18.1.15. [DOI] [PubMed] [Google Scholar]
- 29.Forsyth BH, Lessler JT. Cognitive laboratory methods: a taxonomy. In: Biemer PP, Groves RM, Lyberg LE, Mathiowetz NA, Sudman S, editors. Measurement Errors in Surveys. New York, NY: Wiley-Interscience; 1991. pp. 395–418. [Google Scholar]
- 30.Jobe JB, Mingay DJ. Cognitive research improves questionnaires. Am J Public Health. 1989;79:1053–5. doi: 10.2105/ajph.79.8.1053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jobe JB, Mingay DJ. Cognitive laboratory approach to designing questionnaires for surveys of the elderly. Public Health Rep. 1990;105:518–24. [PMC free article] [PubMed] [Google Scholar]
- 32.Petty RE, Cacioppo JT. Dubuque, IA: William C. Brown; 1981. Attitudes and persuasion: classic and contemporary approaches. [Google Scholar]
- 33.Petty RE, Cacioppo JT, Strathman AJ, et al. To think or not to think. Exploring two routes to persuasion. In: Shavitt S, Brock TC, editors. Persuasion. Psychological Insights and Perspectives. Boston, MA: Allyn and Bacon; 1994. pp. 113–47. [Google Scholar]
- 34.Goodman RM, Tenney M, Smith DW, et al. The adoption process for health curriculum innovations in schools: a case study. J Health Educ. 1992;23:215–20. [Google Scholar]
- 35.Mayer JP, Davidson WS. Dissemination of innovations. In: Rappaport J, Seidman E, editors. Handbook of Community Psychology. (pp. 421-438) New York, NY: Plenum Publishers; 2000. pp. 215–20. [Google Scholar]
- 36.Oldenburg B, Hardcastle DM, Kok G. Diffusion of innovations. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education. 2nd edn. San Francisco, CA: Jossey-Bass Publishers; 1997. pp. 270–86. [Google Scholar]
- 37.Bauman LJ, Stein RE, Ireys HT. Reinventing fidelity: the transfer of social technology among settings. Am J Community Psychol. 1991;19:619–39. doi: 10.1007/BF00937995. [DOI] [PubMed] [Google Scholar]
- 38.Bauman AE, Sallis JF, Dzewaltowski DA, et al. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23(2 Suppl.):5–14. doi: 10.1016/s0749-3797(02)00469-5. [DOI] [PubMed] [Google Scholar]
- 39.Wandersman A, Duffy J, Flaspohler P, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41:171–81. doi: 10.1007/s10464-008-9174-z. [DOI] [PubMed] [Google Scholar]
- 40.Kreuter MW, Bernhardt JM. Reframing the dissemination challenge: a marketing and distribution perspective. Am J Public Health. 2009;99:2123–7. doi: 10.2105/AJPH.2008.155218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dobbins M, Robeson P, Ciliska D. A description of a knowledge broker role implemented as part of a randomized controlled trial evaluating three knowledge translation strategies. Implement Sci. 2009;4:23. doi: 10.1186/1748-5908-4-23. [DOI] [PMC free article] [PubMed] [Google Scholar]