Abstract
Background Little is known about the balance between work demands and treatment plans for >4.3 million working-age cancer survivors in the USA.
Aims To describe changes in work status for gynaecological cancer survivors during the first 6 months following diagnosis and their experience with their employers’ programmes and policies.
Methods One hundred and ten gynaecological cancer survivors who were working at the time of their cancer diagnosis completed a survey. Case record reviews documented their clinical characteristics and treatment details.
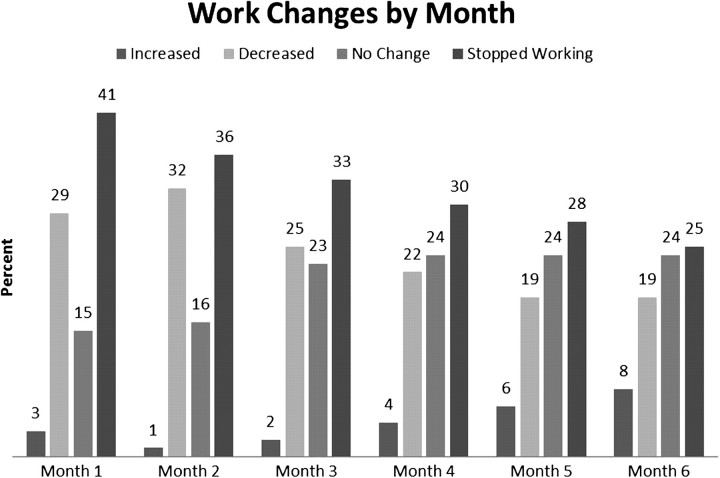
Results Ninety-five women (86%) had surgery; 81 (74%) received chemotherapy, radiotherapy or both in addition to surgery. Nine per cent of women said that they changed their treatment plan because of their jobs; in contrast, 62% of women said that they changed their work situation to accommodate their treatment plan. Overall, the most common month for women to stop working was Month 1 (41%), to decrease hours was Month 2 (32%) and to increase hours was Month 6 (8%). Twenty-eight per cent of women were aware of employer policies that assisted the return to work process; 70% of women were familiar with the Family and Medical Leave Act (FMLA) and 56% with the Americans with Disabilities Act (ADA). Only 26% completed a formal request for work accommodations. After 6 months, 56 of 83 women (67%) remained working or had returned to work.
Conclusions Work patterns varied for these gynaecological cancer survivors over the first 6 months following diagnosis. Opportunities exist to improve communication about work and treatment expectations between cancer survivors, occupational health professionals, employers and treating clinicians.
Keywords: Cancer, restrictions, survivorship, work
Introduction
As cancer treatment options improve, the number of cancer survivors continues to grow. The US National Cancer Institute estimates that there were ∼11.4 million Americans with a history of cancer alive in January 2006 [1]. Of these survivors, ∼38% are in the typical working age range of 20–64 years [2]. A recent review of 14 studies found a range of return to work rates (30–93%). Factors associated with lower rates included the type of work (manual labour), the work environment (non-supportive versus supportive) and the type of cancer (head and neck cancer survivors had lower rates of return to work) [3].
Most studies of female cancer survivors’ return to work experience focus specifically on breast cancer. Survivors of gynaecological cancers (cervix, uterine corpus, ovary, vulva and vagina) are often overlooked and yet, these account for >11% of all incident cancers among women in the USA [1]. An estimated 88 080 women in the USA were expected to be diagnosed with a gynaecological cancer in 2011 and certain types, such as uterine cancer, have high rates of survival [1]. In addition, treatment for some cancers, including ovarian cancers, is usually protracted requiring multiple cycles of chemotherapy, which presents additional challenges for working women.
Laws governing employment and return to work processes vary by country. In the USA, several laws may pertain, including the Family and Medical Leave Act (FMLA) and the Americans with Disabilities Act (ADA). The FMLA provides up to 12 weeks of unpaid, job-protected leave and continuation of group health benefits for qualified employees. FMLA applies to all public agencies, all public and private elementary and secondary schools and to companies with ≥50 employees. To be eligible for FMLA benefits, an employee must meet several criteria, including working for an employer covered by the FMLA for at least 1250 h in the previous 12 months. The ADA is a federal law that prohibits discrimination against individuals with disabilities [4]. New ADA provisions that took effect in March 2011 clarify that in some situations, cancer may be considered a disability, with protection under the ADA. Despite these legal protections, it is unclear how many cancer patients are aware of these laws.
The aims of this paper are to describe changes in work status for gynaecological cancer survivors in the USA during the first 6 months following diagnosis and the experience of employers’ programmes and policies concerning return to work after illness.
Methods
The subjects included in this study were a convenience sample of all gynaecological cancer patients within 24 months of diagnosis seen at the Women’s Health Center Clinic at the University of Minnesota Fairview during the 17 weeks between 3 November 2008 and 27 February 2009. A research nurse reviewed the schedule weekly to identify eligible subjects (women diagnosed with gynaecological cancer, time since diagnosis <24 months, age at least 21 years and English speaking). A research nurse provided a survey questionnaire, information sheet and consent form to eligible patients. Completed materials were collected in a sealed envelope and returned to clinic staff. Women also consented to a medical record review by the research nurse to document cancer type, stage, diagnosis date and treatment.
Ethical approval for this study was given by the University of Minnesota Institutional Review Board. Data from completed questionnaires and record reviews were entered and verified in an Access database and SAS 9.2 (SAS Institute, Cary, NC) was used for analysis. A conceptual model identified hypothesized relationships between clinical characteristics and variables related to the survivor, physicians and work situation that may influence the return to work experience for the survivor. Descriptive statistics were used to identify overall characteristics of the survivors. To explore relationships within the dataset, cross tabulations were performed. Open–ended responses were entered, reviewed and grouped into categories based on keywords.
Results
Of a total of 276 women invited to participate in this study, 155 responded (56%). Of the 155 respondents, 110 (71%) reported working at the time of their cancer diagnosis. These women are the focus of our study.
Participant characteristics are presented in Table 1(available as Supplementary data at Occupational Medicine Online). The primary types of cancer were ovary (47%), uterus (33%) and cervix (9%); 39% were Stage I, 15% Stage II, 33% Stage III and 5% Stage IV. Age ranged from 24 to 79 years, with a median of 53 years.
Time since diagnosis ranged from 1 to 24 months, with a mean of 11.8 months. Most (84%) of the women who reported working at the time of their diagnosis were also working at the time they completed the questionnaire. Sixteen women provided reasons they were not working. Ten of these (63%) stated that their cancer was the primary reason they were not currently working while additional causes included: retirement (two), layoff (one), restrictions related to treatment preventing working (one) and termination of employment during treatment (one).
Health care and education were the most frequent sectors of employment (21 and 20%, respectively), with another 11% working in service industries. The remaining 48% worked in a variety of industries including finance, insurance, real estate and government. Three quarters of them (74%) were offered health care coverage by their employer.
Of the 110 women, 51 had chemotherapy, 10 had radiotherapy, 20 had both and 29 received neither; 95 women had had a surgical procedure beyond a diagnostic biopsy. Nine per cent of women said that they changed their treatment plan because of work concerns, including scheduling treatment during days off work or trying to minimize lost time. In contrast, 62% of women said that they changed their work situation because of their treatment plan, by taking time off, decreasing hours worked or decreasing the physical demands of their jobs.
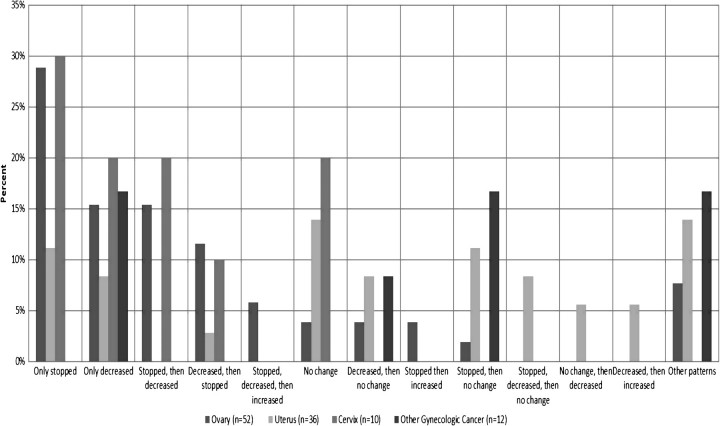
Analysis of hours worked each month following diagnosis compared with pre-diagnosis schedules, identified several patterns of decreasing work hours, stopping work completely, making no changes or increasing hours (Figure 1). These patterns also varied by cancer type: women with ovarian cancer were more likely to stop working completely during these first 6 months (29%), while women with uterine cancer most typically made no changes to their hours worked. When described in general by month following diagnosis (Figure 2), the month in which women most frequently stopped working was the first month (41%) and that in which a decrease in working hours occurred most frequently was the second month post-diagnosis (32%). An increase in hours worked occurred most frequently in Month 6 (8%) and overall after 6 months; 67% of women had either remained working or had returned to work. The impact of a cancer diagnosis on work changes varied considerably across cancer types (Figure 3). For example, a high percentage of women with ovarian cancer stopped working (37–56% each month) or decreased their hours (21–37% each month), while only 14−28% of women with uterine cancer stopped working during any of the first 6 months following diagnosis.
Figure 1.
Work patterns during first 6 months post-diagnosis.
Figure 2.
Change in hours worked over first 6 months.
Figure 3.
Work changes by month and cancer type.
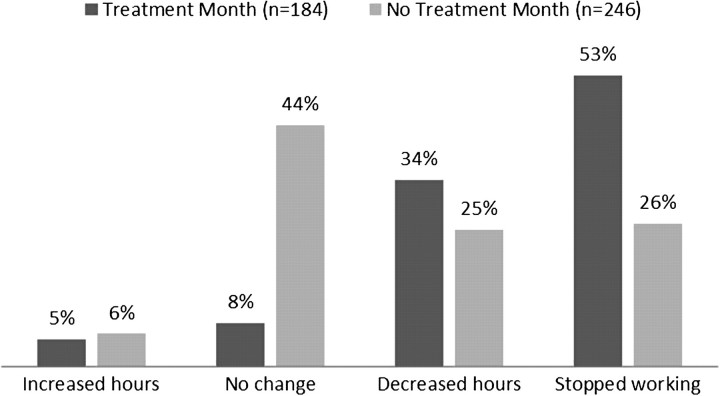
When compared by whether or not women were undergoing active chemotherapy treatment during the months following diagnosis, different patterns emerged (Chi-square P < 0.001). Month 1 was excluded in this figure because 90% did not begin chemotherapy until the end of Month 1 or later. Changes were analysed by month because the duration of chemotherapy treatment varied between women and because work changes are also dynamic and may change from month to month. If a woman had chemotherapy in a particular month (n = 184 months), 5% increased their work hours during that month, 8% had no change, 34% decreased their hours and 53% did not work that month. In contrast, of the months women did not have chemotherapy (n = 246 months), 6% increased hours, 44% had no change, 25% decreased their work hours and 26% stopped working (see Figure 4).
Figure 4.
Work changes for months 2–6 following diagnosis, by chemotherapy reatment status.
Reasons given for decreasing working hours included the cancer treatment itself (58%) and cancer symptoms (25%). Women who increased hours reported reasons including renewed energy (n = 5), the need to make up for financial losses (n = 3) and to maintain/acquire health insurance (n = 4). Eighty per cent of women missed some time from work, varying from 70% of women with cervical cancer to 90% of women with ovarian cancer. Half of the women said that physical or mental symptoms, most often fatigue and nausea, restricted their ability to work (Table 2, available as Supplementary data at Occupational Medicine Online).
Women also described their concerns about returning to work in qualitative open-ended responses. Most frequently they cited concerns about the physical symptoms or side effects that would limit their ability to keep up (n = 18), fatigue or lack of energy (n = 16), decreased ability to concentrate, which some women referred to as ‘Chemo brain’ (n = 11) and the ability to work full-days (n = 10).
Fifty-eight per cent of the women discussed their treatment plan and work situation with their physician, and 26% of women completed a formal request for work accommodations. Reasonable accommodations under the ADA include changes or adjustments to a job or work environment that permits the employee to perform the job, such as modifying a work schedule. However, 35% of women said that they did not discuss their treatment plan and work situation with their physician. Only 28% of women said that they were aware that their employer had written policies that assisted in the return to work process, while more were aware of other legal protections.
Women were also asked about the degree to which their desire to work changed following diagnosis (Table 2). Overall, 74% of the women reported a somewhat or very strong desire to work and 18% reported a ‘somewhat’ or ‘very’ strong desire to quit. However, when stratified by cancer type, 25% of women with ovarian cancer reported somewhat or very strong desires to quit. Of the 81 women who stated that they had a very strong/somewhat strong desire to work, 31 (38%) never stopped working compared to 5 women (25%) who never stopped working, even though they indicated having a somewhat/very strong desire to quit.
Fear of losing health insurance and of not being able to obtain health insurance with a new employer were factors that concerned over one-quarter of the women. Some women said that, in retrospect, they wished they had taken more time off, even if it was unpaid or part-time (n = 8) and that they wished they had made better financial choices, including choosing short-term disability benefits or increased financial savings choices (n = 4).
Women also shared their thoughts regarding factors that made the return process easier or more difficult. Overwhelmingly, women spontaneously reported that co-workers made the return easier (n = 28, 25%), as did supportive employers (n = 21, 19%). Flexibility in work schedules was the third most frequently cited helpful factor (n = 17, 15%). Family (n = 4, 4%), work as a distraction (n = 4, 4%) and prayers and exercise (n = 1, 1%) were also mentioned. In contrast, physical limitations (n = 24, 22%), decreased energy/fatigue (n = 14, 13%), and ‘Chemo brain’ (n = 5, 5%) were all reported to have made the return more difficult.
Discussion
The women in our study had multifaceted patterns of increasing or decreasing work hours, stopping work and returning to original work schedules in the first 6 months following diagnosis of gynaecological cancer. Women most frequently stopped working in the first month following diagnosis and decreased their hours in the second month; however, the trends differed by cancer type, perhaps due to treatment regimen or prognosis, and women with ovarian cancer were more likely to stop working or decrease their work hours than those with cervical or uterine cancers. A better understanding of some of the typical work patterns in this critical phase shortly after diagnosis may help both occupational health professionals and treating physicians suggest work plans for their patients.
Most of the women in this study who were working at the time of their gynaecological cancer diagnosis returned to work, consistent with previous research [3,5,6,7]. Desire to work is an important facet of this picture. We found return rates varied by desire to return, such that those who reported having a strong desire to quit following diagnosis were more likely to have done so at the time of participation in the study.
The overall high rate of return to work may mask the need for accommodations as survivors make the transition back to work. Research specifically examining the impact of accommodations on return to work experience appears to be particularly lacking. In our study, only 26% of women requested accommodations, although a significant number of women on chemotherapy experienced changes in their work pattern.
In our study, only 58% of women had discussed their treatment plan and work situation with their physician. This lack of communication, consistent with previous research [12], identifies opportunities for occupational health professionals and treating physicians to work with survivors to assist and thereby improve the return to work transition. Only 26% of women had formally received work accommodations, again presenting an important opportunity for discussions with the health care team, occupational health professionals and the survivor. In the USA, a survivor and treating physician typically discuss a request for a work accommodation, such as reduced work hours or modifications to a job task, such as decreasing the amount of time standing during a shift. Employers review the request and decide whether they can ‘reasonably’ accommodate the request, although what is reasonable may vary by industry, employer size and other factors. Occupational health professionals, if available within the organization, are critical in assessing these requests based on their medical knowledge of exposure and outcome assessments and familiarity with the job demands within the organization. Clear communication about treatment, effects and work demands early in the treatment phase may provide the best opportunity to improve return to work outcomes for cancer survivors. Unfortunately, currently, communication concerning return to work appears to be less than ideal [8,9,10,11].
Best practices for US employers’ return to work programmes and policies are unclear. No single policy or procedure will cover all industries, occupations or survivor situations, and assessment of ‘disability’ and ‘reasonable accommodation’ under the ADA must be addressed in a case-by-case basis. Implications from the recent health care legislation, such as requirements for health care coverage regardless of pre-existing health conditions, may assist with other concerns for cancer survivors, including ‘job lock’, which is the fear of leaving a current job because of concerns the survivor will be unable to obtain health care coverage with a new employer due to a history of cancer.
As identified in a previous focus group study [13], some survivors describe a strong desire to return to work following a cancer diagnosis because they feel a close identity with their job, while others choose to leave their job completely because their priorities have changed. The individual job demands and clinical characteristics also vary from case to case but understanding some of the more common concerns and trends in timing over the first 6 months following diagnosis, based on age, gender and cancer type, may assist in developing policy and clinical practice. Over half of the women said that they changed their working arrangements because of their treatment plan, but only 28% said that they were aware that their employer had written policies that assisted the return to work process.
Occupational health professionals are in a unique position to assist the smooth transition back to work for cancer survivors, given their clinical expertise, knowledge of the workplace and awareness of legal protections available to workers. There is also a need for clear communication between cancer survivors, occupational health professionals at the worksite and the treating health care team, taking into account the physical and mental demands of various jobs, so that potential accommodations to assist in a healthy return to work can be identified and recommended to cancer survivors and their employers.
There are limits to the extent to which the results of this pilot study can be generalized to all gynaecological cancer survivors. Our sample consisted of gynaecological cancer patients who were within 24 months of diagnosis. Due to IRB requirements that we may not review a patient’s medical records without the patient’s written consent, we cannot determine whether participants and non-participants differed significantly. This group of women was also highly educated, with 44% having a bachelor’s degree or higher, which may result in better occupational opportunities than for those with less education. Participants self-reported their work experiences and are subject to recall bias since some participants had been diagnosed up to 24 months prior to survey administration. In addition, because of a limited sample size, multivariate results based on industry, job type or job demands were not possible. However, this study also has important strengths that should not be ignored, in particular in combining self-reported perceptions of work status with medical record data to confirm clinical characteristics. By choosing to share their experience, our study subjects have provided insight into some of the more prevalent issues that need additional research in future studies.
Most gynaecological cancer survivors in our study returned to work within 6 months of diagnosis but return to work patterns varied according to cancer type and whether or not the survivor was currently receiving chemotherapy. Understanding the experiences of other gynaecological survivors may help inform conversations between survivors, oncologists and occupational health physicians and nurses about opportunities to assist and improve the return to work process. Only one-quarter of survivors formally requested work accommodations, indicating the need for improved employer-based policies and programmes and education about legal protection such as the ADA and the FMLA.
Key points
A majority of gynaecological cancer survivors in this study modified their work situation to fit their cancer treatment plan, though only about a quarter of women requested formal work accommodations.
Women who were undergoing chemotherapy frequently reduced their work hours, or stopped working completely, during months with active chemotherapy.
Approximately one-quarter of women said employer-based policies assisted in the return to work process; however, co-worker support was the most frequently cited factor that made the return to work process easier for gynaecological cancer survivors.
Funding
This work was supported in part by the Minnesota Medical Foundation and the National Institutes of Health (P30 CA77598) utilizing the Masonic Cancer Center, University of Minnesota Biostatistics and Informatics Shared Resource.
Conflicts of interest
None declared.
Supplementary Material
Acknowledgments
A special thank you to Sadie Brendalen for data entry and verification; Barbara Glubka for assistance in participant recruitment, survey administration and medical record reviews and the cancer survivors who were willing to share their experiences with us.
References
- 1.American Cancer Society. Cancer Facts & Figures 2011. Atlanta, GA: American Cancer Society; 2011. [Google Scholar]
- 2.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: The National Academies Press; 2006. [Google Scholar]
- 3.Spelten ER, Sprangers MAG, Verbeek JHAM. Factors reported to influence the return to work of cancer survivors: a literature review. Psychooncology. 2002;11:1562–1567. doi: 10.1002/pon.585. [DOI] [PubMed] [Google Scholar]
- 4. U.S. Equal Employment Opportunity Commission. Questions and Answers About Cancer in the Workplace and the Americans with Disabilities Act (ADA). http://www.eeoc.gov/facts/cancer.html (31 December 2010, date last accessed)
- 5.Villaverde RM, Batlle JF, Yllan AV, et al. Employment in a cohort of breast cancer patients. Occup Med (Lond) 2008;58:509–511. doi: 10.1093/occmed/kqn092. [DOI] [PubMed] [Google Scholar]
- 6.Drolet M, Maunsell E, Mondor M, et al. Work absence after breast cancer diagnosis: a population-based study. CMAJ. 2005;173:765–7. doi: 10.1503/cmaj.050178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bradley CJ, Neumark D, Luo Z, Bednarek H, Schenk M. Employment outcomes of men treated for prostate cancer. J Natl Cancer Inst. 2005;97:958–9. doi: 10.1093/jnci/dji171. [DOI] [PubMed] [Google Scholar]
- 8.Amir Z, Wynn P, Whitaker S, Luker K. Cancer survivorship and return to work: UK occupational physician experience. Occup Med (Lond) 2009;59:390–396. doi: 10.1093/occmed/kqn150. [DOI] [PubMed] [Google Scholar]
- 9.Taskila T, Lindbohm ML, Martikainen R, Lehto LUS, Hakanen J, Hietanen P. Cancer survivors’ received and needed social support from their work place and the occupational health services. Support Care Cancer. 2006;14:427–435. doi: 10.1007/s00520-005-0005-6. [DOI] [PubMed] [Google Scholar]
- 10.Verbeek J, Spelten E, Kammeijer M, Sprangers M. Return to work of cancer survivors: a prospective cohort study into the quality of rehabilitation by occupational physicians. Occup Environ Med. 2003;60:352–357. doi: 10.1136/oem.60.5.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DeBoer AGEM, Frings-Dresen MHW. Employment and the common cancers: return to work of cancer survivors. Occup Med (Lond) 2009;59:378–380. doi: 10.1093/occmed/kqp087. [DOI] [PubMed] [Google Scholar]
- 12.Yarker J, Munir F, Bains M, Kalawsky K. Haslam C. The role of communication and support in return to work following cancer-related absence. Psychoncology. 2009;19:1078–1085. doi: 10.1002/pon.1662. [DOI] [PubMed] [Google Scholar]
- 13.Nachreiner NM, Dagher R, McGovern PM, Baker B, Alexander B, Gerberich SG. Successful return to work for cancer survivors. AAOHN J. 2007;55:290–295. doi: 10.1177/216507990705500705. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.