Abstract
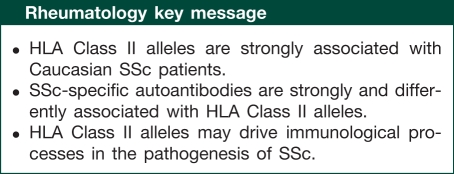
Objective. To determine the role of Class II HLAs in SSc patients from Italy and Spain and in SSc patients of Caucasian ancestry.
Methods. Nine hundred and forty-four SSc patients (Italy 392 patients; Spain 452 patients) and 1320 ethnically matched healthy controls (Italy 398 patients; Spain 922 patients) were genotyped up to the fourth digit by PCR with sequence-specific oligonucleotides for HLA-DRB1, DQA1 and DQB1 loci. Patients included 390 ACA-positive and 254 anti-topo I-positive subjects. Associations between SSc or SSc-specific antibodies and HLA alleles or HLA haplotypes were sought via the chi-square test after 10 000-fold permutation testing. A meta-analysis including this study cohort and other Caucasoids samples was also conducted.
Results. In both the cohorts, the strongest association was observed between the HLA-DRB1*1104 allele and SSc or anti-topo I antibodies. The HLA-DRB1*1104 -DQA1*0501 -DQB1*0301 haplotype was overrepresented in Italian [odds ratio (OR) = 2.069, 95% asymptotic CIs (CI95) 1.486, 2.881; P < 0.001] and in Spanish patients (OR = 6.707, CI95 3.974, 11.319; P < 0.001) as well as in anti-topo-positive patients: Italy (OR = 2.642, CI95 1.78, 3.924; P < 0.001) and Spain (OR = 20.625, CI95 11.536, 36.876; P < 0.001). In both the populations we also identified an additional risk allele (HLA-DQB1*03) and a protective allele (HLA-DQB1*0501) in anti-topo-positive patients. The meta-analysis showed different statistically significant associations, the most interesting being the differential association between HLA-DRB1*01 alleles and ACAs (OR = 1.724, CI95 1.482, 2.005; P < 0.001) or topo I antibodies (OR = 0.5, CI95 0.384, 0.651; P < 0.001).
Conclusions. We describe multiple robust associations between SSc and HLA Class II antigens in Caucasoids that may help to understand the genetic architecture of SSc.
Keywords: systemic sclerosis, HLA, genetics, epidemiology
Introduction
SSc is a complex CTD characterized by fibrosis of the skin and internal organs, widespread vasculopathy and abnormalities of the immune system [1, 2]. Several lines of evidence underline the importance of the individual’s genetic background in SSc susceptibility and/or phenotypic expression and associations with a number of single nucleotide polymorphisms (SNPs) and SSc have consistently been replicated in different populations [3]. Similarly, a number of discovery and replication studies describing associations with SSc and the HLA Class II alleles in different ethnic groups have been published so far [3, 4]. The major contribution in this field comes from reports conducted in North Americans, and most notably from the large case–control study recently published by Arnett et al. [5]. Conversely, the association between major histocompatibility Class II (MHC) antigens and SSc in other geographical regions and/or ethnicities, such as European Caucasoids, has been limited to reports with a small to moderate number of cases and/or controls, seldom reaching the hundreds [5–12]. The limited number of cases/controls employed in the vast majority of HLA case–control studies in Caucasoids may help to explain the variability of results observed in these samples, either in terms of pure associations with SSc susceptibility or in terms of associations with specific SSc autoantibodies. Indeed, while differences among ethnicities may account for the inconsistent results across the different reports, the lack of power should also be carefully considered as a potential source of variance. Owing to the existence of extended linkage disequilibrium (LD) within the HLA region, it may be difficult to ascertain the primary disease-associated HLA allele(s) in underpowered case–control studies.
In the present study, we aimed to elucidate the role of HLA Class II alleles in two vast case–control sets of European Caucasoid individuals recruited from tertiary referral centres in Spain and Italy. To our knowledge, this is the largest case–control MHC Class II-association study conducted in SSc patients of European ancestry.
Method
Patients selection
Four hundred and two consecutive SSc patients referring to one single centre in northern Italy and 398 unrelated ethnically and sex-matched healthy controls were considered (case–control Series 1). The majority of these patients (90.8%) fulfilled the preliminary criteria for the classification of SSc proposed by the ACR [13], yet a proportion of patients with definite SSc who did not fulfil these criteria was also considered [14]. Additionally, 452 patients, of whom 438 (96.9%) with SSc according to the ACR criteria, who were referred to 15 tertiary institutions in Spain and 922 unrelated ethnically and sex-matched controls were also considered (case–control Series 2). In both series, all the patients and the controls gave written consent for the research. The local ethic committees approved the study (Comité de Bioética del Consejo Superior de Investigaciones Científicas and U.O. Comitato di Etica e Sperimentazione Farmaci Fondazione IRCCS Ca’ Granda–Ospedale Maggiore Policlinico di Milano).
All the patients were categorized as having the lcSSc or dcSSc subset of the disease, according to LeRoy et al. [15]; patients with the CREST syndrome features were grouped into the lcSSc subset [16]. The patients’ autoantibody profile was obtained by reviewing the patients’ medical records.
HLA Class II genotyping
Case–control Series 1 was genotyped in one single laboratory; similarly, Series 2 genotyping was performed at a single institution [Instituto de Parasitologia y Biomedicina ‘Lopez-Neyra’ (CSIC), Granada]. In both institutions, high-resolution HLA Class II typing (up to the fourth digit) was performed by means of PCR with sequence-specific primers (PCR-SSP) as previously described [17].
Statistical analysis
Associations between HLA alleles and SSc or between HLA alleles and SSc-specific autoantibodies, such as ACA or anti-topo I (topo I, Scl70), were sought via the χ2-test with 1 degree of freedom. Only alleles with a frequency >3% in cases/controls were considered for the analysis. To correct for multiple testing, 10 000 permutations were used; the advantage of permutation resampling, in this context, is the capability to derive the null distribution of high-dimensional test statistics while preserving the dependence structure (e.g. LD) among HLA alleles. Moreover, irregularities of the observed data are maintained in the permuted data sets and are included in the estimation of the permutation probability [18, 19]. Results were considered significant at the 0.05 level for the controls vs SSc comparison or at the 0.025 level for the autoantibody vs controls or for the SSc subsets vs controls comparison with further account for multiple testings. For significant results, odds ratios (ORs) and their relative 95% asymptotic confidence intervals (CI95) were calculated.
HLA haplotypes were derived in both cohorts via the PHASE software [20] (available at http://stephenslab.uchicago.edu/software.html). Associations between HLA Class II haplotypes and SSc or SSc-specific autoantibodies were then conducted as described above. Underrepresented HLA Class II halpotypes were excluded from the analysis.
Finally, to gauge the overall contribution of HLA alleles in Caucasoid populations, a meta-analysis that included the present and previously published data was conducted. To be considered for the meta-analysis, literature data had to report both high-resolution HLA typing results and HLA Class II allele frequencies. Meta-analysis was thus restricted to the present study, to the works by Vlachoyiannopoulos et al. [10] and by Arnett et al. [5]; in the latter case African-Americans and Hispanics were not considered for meta-analysis owing to the different genetic background from Caucasoids. Indeed, as observed by Bryc et al. [21], the Hispanic population is a genetic amalgamation of native Americans, Europeans and West Africans. To perform the meta-analysis, the Microsoft Excel add-in Mix software was used [22] (available at http://www.meta-analysis-made-easy.com/) and the Mantel–Haenszel procedure with fixed effects was applied. When the percentage of total variation across studies that is due to heterogeneity (I2) [23] was >50%, the meta-analysis was not performed to avoid any bias in the determination of the generalizability of the findings. Meta-analysis results were declared significant at the 0.001 threshold.
Result
Series 1 included 271 (67.4%) lcSSc and 94 (23.4%) dcSSc patients; 168 (41.8%) patients tested positive for ACAs, while 155 (38.6%) tested positive for Scl70 antibodies. Series 2 included 323 (71.5%) lcSSc and 115 (25.4%) dcSSc patients; 222 (49.1%) patients tested positive for ACAs, while 99 (21.9%) tested positive for Scl70 antibodies.
In both the cohorts, ACAs and Scl70 antibodies were strongly correlated with the lcSSc and the dcSSc subset, respectively (P < 1 × 10−20). For the sake of brevity, hereafter we will report only the most significant results, while an exhaustive description of the single-allele analysis in both series as well as of the meta-analysis is reported in the supplementary data, available at Rheumatology Online.
The HLA-DRB1*1104 allele and the DR11 haplotype are associated with SSc and anti-topo I antibodies
In both cohorts, the HLA-DRB1*1104 allele was strongly associated with SSc (Table 1) and to a somewhat stronger extent with Scl70 antibodies (Table 2). Due to heterogeneity issues an exhaustive meta-analysis for the HLA-DRB1*1104 was not possible, yet the HLA-DRB1*11 allele was found to be strongly associated with SSc in Caucasoids (cases: 999/3826, 26.1% and controls: 692/3980, 17.4%; P < 0.001; OR = 1.573, CI95 1.403, 1.764).
Table 1.
HLA Class II associations with SSc
| HLA | Ctrl, n (%) | SSc, n (%) | Uncorrected P | Corrected P | OR (CI95) |
|---|---|---|---|---|---|
| Italy | |||||
| DRB1*1104 | 83 (10.40) | 151 (18.78) | <0.001 | <0.001 | 1.992 (1.493, 2.657) |
| DRB1*11 | 227 (28.45) | 284 (35.32) | 0.003 | 0.04 | 1.374 (1.124, 1.697) |
| DQA1*0501 | 250 (31.33) | 337 (41.92) | <0.001 | <0.001 | 1.582 (1.289, 1.942) |
| DQA1*05 | 326 (40.85) | 396 (49.25) | 0.001 | 0.01 | 1.405 (1.153, 1.712) |
| Spain | |||||
| DRB1*0701 | 283 (15.35) | 91 (10.07) | <0.001 | 0.006 | 0.617 (0.48, 0.793) |
| DRB1*1104 | 20 (1.08) | 64 (7.08) | <0.001 | <0.001 | 6.499 (4.178, 11.556) |
| DRB1*11 | 230 (12.47) | 153 (16.92) | 0.002 | 0.03 | 1.43 (1.145, 1.785) |
HLA Class II significant associations with SSc (after 10 000-fold permutation testing) in Italy and Spain. The table reports the number of positive alleles in cases and controls. Total number of alleles per series—Italy: SSc = 802; Ctrl = 798; Spain: SSc = 902; Ctrl = 1844. Ctrl: controls.
Table 2.
HLA Class II associations with ATAs
| HLA | Ctrl, n (%) | SSc, n (%) | Uncorrected P | Corrected P | OR (CI95) |
|---|---|---|---|---|---|
| Italy | |||||
| DRB1*1104 | 83 (10.4) | 64 (20.6) | <0.001 | <0.001 | 3.75 (2.588, 5.436) |
| DQA1*01 | 316 (39.6) | 84 (27.1) | <0.001 | <0.001 | 0.567 (0.425, 0.756) |
| DQA1*0501 | 250 (31.3) | 140 (45.2) | <0.001 | <0.000 | 1.784 (1.369, 2.334) |
| DQA1*05 | 326 (40.9) | 159 (51.3) | 0.002 | 0.03 | 1.525 (1.171, 1.985) |
| DQB1*03 | 301 (37.7) | 151 (48.7) | 0.001 | 0.02 | 1.569 (1.189, 2.017) |
| DQB1*05 | 192 (24.1) | 42 (13.5) | <0.001 | <0.001 | 0.491 (0.341, 0.706) |
| Spain | |||||
| DRB1*1104 | 20 (1.10) | 35 (17.70) | <0.001 | <0.001 | 19.58 (11.049, 34.707) |
| DRB1*11 | 230 (12.50) | 52 (26.30) | <0.001 | <0.001 | 2.493 (1.796, 3.53) |
| DRB1*1501 | 142 (7.70) | 38 (19.20) | <0.001 | <0.001 | 2.847 (1.922, 4.217) |
| DRB1*15 | 165 (8.90) | 43 (21.70) | <0.001 | <0.001 | 2.823 (1.943, 4.102) |
| DQB1*0301 | 359 (19.50) | 61 (30.80) | <0.001 | 0.02 | 1.842 (1.333, 2.544) |
| DQB1*0501 | 291 (15.80) | 12 (6.10) | <0.001 | 0.02 | 0.344 (0.189, 0.625) |
| DQB1*05 | 358 (19.50) | 17 (8.60) | <0.001 | 0.004 | 0.39 (0.234, 0.65) |
| DQB1*0602 | 121 (6.60) | 34 (17.20) | <0.001 | <0.001 | 2.952 (1.954, 4.461) |
| DQB1*06 | 316 (17.20) | 57 (28.80) | <0.001 | <0.001 | 1.955 (1.404, 2.721) |
HLA Class II significant associations with ATAs (after 10 000-fold permutation testing) in Italy and Spain. Total number of alleles per series—Italy: SSc = 310; cases (Ctrl) = 798; Spain: SSc = 198; Ctrl = 1844. Ctrl: controls.
The prominent role for the HLA-DRB1*1104 allele in SSc susceptibility also emerged from haplotype analysis. The DR11 haplotype (HLA-DRB1*1104 -DQA1*0501 -DQB1*0301) was overrepresented both in Italians (cases: 114/804, 14.2% and controls: 59/798, 7.2% haplotypes; P < 0.001; OR = 2.069, CI95 1.486, 2.881) and to a greater extent in Spaniards (cases: 59/904, 6.52% and controls 19/1844, 1% haplotypes; P < 0.001; OR = 6.707, CI95 3.974, 11.319). The DR11 haplotype was also significantly associated with anti-topo I antibodies (ATAs) both in the Italian (cases: 54/310, 17.4% and controls: 59/798, 7.4% haplotypes; P < 0.001; OR = 2.642, CI95 1.779, 3.924) and in the Spanish series (cases: 34/198, 17.7% and controls: 19/1844, 1% haplotypes; P < 0.001; OR = 20.625, CI95 11.536, 36.875).
The associations between the DR11 haplotype and SSc or between the DR11 haplotype and ATAs was previously described by Agarwal et al. [4]; nonetheless, these authors did not report the number and the proportion of cases/controls carrying the DR11 haplotype and thus it was not possible to conduct a proper meta-analysis to quantify the risk in Caucasoids.
The HLA-DRB1*01 allele is differently associated with ACAs and ATAs
The HLA-DRB1*01 allele was found to be underrepresented in Italian and Spanish patients with ATAs (Table 2) and overrepresented in Spanish subjects who tested positive for ACAs (Table 3). The opposite effects on risk susceptibility in patients with different anti-corpal specificities is also confirmed by the meta-analysis: Scl70 (cases: 73/818, 8.9% and controls: 588/3720, 15.8%; P < 0.001; OR 0.5001, CI95 0.384, 0.651) and ACAs (cases: 345/1342, 25.7% and controls: 588/372, 15.8%; P < 0.001; OR = 1.365, CI95 1.238, 1.511).
Table 3.
HLA Class II associations with ACAs
| HLA | Ctrl, n (%) | SSc, n (%) | Uncorrected P | Corrected P | OR (CI95) |
|---|---|---|---|---|---|
| DRB1*0101 | 139 (7.54) | 62 (13.96) | <0.001 | <0.001 | 1.991 (1.447, 2.739) |
| DRB1*0701 | 283 (15.35) | 28 (6.31) | <0.001 | <0.001 | 0.373 (0.248, 0.556) |
| DRB1*0801 | 46 (2.49) | 30 (6.76) | <0.001 | <0.001 | 2.832 (1.766, 4.542) |
| DRB1*1104 | 20 (1.08) | 23 (5.18) | <0.001 | <0.001 | 4.982 (2.711, 9.156) |
| DQA1*0201 | 282 (15.29) | 28 (6.31) | <0.001 | <0.001 | 0.373 (0.249, 0.558) |
| DQA1*0401 | 58 (3.15) | 36 (8.11) | <0.001 | <0.001 | 2.717 (1.768, 4.175) |
| DQB1*0202 | 232 (12.58) | 29 (6.53) | <0.001 | 0.007 | 0.485 (0.325, 0.725) |
| DQB1*02 | 468 (25.38) | 68 (15.32) | <0.001 | <0.001 | 0.532 (0.402, 0.703) |
| DQB1*0402 | 61 (3.31) | 37 (8.33) | <0.001 | <0.001 | 2.657 (1.742, 4.054) |
| DQB1*0501 | 291 (15.78) | 113 (25.45) | <0.001 | <0.001 | 1.822 (1.422, 2.336) |
HLA Class II significant associations with ACAs (after 10 000-fold permutation testing) in Spain. No significant associations were found in Italy. Number of positive alleles in cases = 444 and controls = 1844. Ctrl: controls.
To isolate the effect of the HLA-DRB1*01 allele from the individuals’ genetic background, we also performed a comparison between either ATA- or ACA-positive patients and SSc patients who tested positive for ANAs, but not to these specific SSc antibodies. Via a meta-analysis procedure, taking into account the Italian and the Spanish series, it was confirmed that the HLA-DRB1*01 allele is differently associated with ATAs or ACAs: Scl70 (cases: 29/508, 5.7% and SSc-ANA-positive subjects: 30/252, 11.9%; P = 0.002; OR = 0.417, CI95 0.235, 0.74); ACAs (cases: 130/776, 16.7% and SSc-ANA-positive subjects: 30/252, 11.9%; P = 0.005; OR = 1.844, CI95 1.2071, 2.816).
Summary of the associations between HLA Class II antigens and ACAs or ATAs
Table 2 lists all the significant associations we observed performing the ATAs vs controls comparisons, while Table 3 depicts the significant associations for the ACAs vs controls comparison; in this latter case, no significant results were observed in the Italian series. An exhaustive description of the comparison between SSc-specific antibodies and healthy controls is reported in the supplementary data, available at Rheumatology Online.
As described above, we also performed the ATAs vs ANAs and the ACAs vs ANAs comparisons in both series, yet a significant loss of power was observed due to the reduced sample size. When the two populations were analysed together via the meta-analysis procedure, we found an exclusive association between ATAs and the DR11 haplotype or the HLA-DRB1*1104 allele, which was not observed when the ACAs vs ANAs comparison was taken into account. Table 4 summarizes the significant results after the above-mentioned meta-analysis procedure. It should be observed that as far as the ACAs vs ANAs analysis is concerned, many comparisons were not possible due to heterogeneity issues, yet in the sole Spanish series, the associations with HLA-DRB1*01, DRB1*0701, DQA1*0201, DQB1*02 or DQB1*0501, previously found when healthy subjects were used as the control group, were confirmed (detailed results not shown).
Table 4.
HLA Class II associations with ATA or ACA using anti-nuclear-positive patients as controls
| HLA | ANA, n (%) | Specific antibodies, n (%) | P-value | OR (CI95) |
|---|---|---|---|---|
| ATAs | ||||
| HLA-DRB1*01 | 30 (11.9) | 29 (5.7) | 0.002 | 0.468 (0.235, 0.739) |
| DRB1*1104 | 21 (8.3) | 99 (19.4) | <0.001 | 2.392 (1.460, 3.919) |
| DQB*0501 | 30 (11.9) | 32 (6.3) | 0.01 | 0.506 (0.297, 0.861) |
| DQB*05 | 30 (11.9) | 59 (11.6) | 0.002 | 0.513 (0.336, 0.782) |
| DR11 haplotype | 15 (5.9) | 86 (16.9) | <0.001 | 3.073 (1.738, 5.432) |
| ACAs | ||||
| HLA-DRB1*01 | 30 (11.9) | 130 (16.7) | 0.005 | 1.744 (1.207, 2.816) |
HLA Class II significant associations with ATAs or ACAs after meta-analysis in the Italian and the Spanish series using ANA-positive patients as controls. Total number of alleles: ATAs = 508; ACAs = 776; ANAs = 252.
Associations with SSc subsets
In both the case series, the association between the HLA-DRB1*1104 allele and SSc was not restricted to any of the two cutaneous subsets (Tables 5 and 6) despite its strong association with ATAs, and the tight link between these antibodies and the dcSSc subset. Similarly, the DR11 haplotype was found to be significantly increased in dcSSc and lcSSc patients, both in Italian subjects (dcSSc cases: 32/188, 17% and controls: 59/798, 7.4% haplotypes; P < 0.001; OR = 2.569, CI95 1.616, 4.085; lcSSc cases: 77/542, 14.2% and controls: 59/798, 7.4% haplotypes; P < 0.001; OR = 20.625, CI95 11.536, 36.876) and in Spanish patients (dcSSc cases: 29/230, 12.6% and controls: 63/1844, 3.41% haplotypes; P < 0.001; OR = 3.69, CI95 2.328, 5.85; lcSSc cases: 57/646, 8.8% and controls: 63/1844, 3.4% haplotypes; P = 0.008; OR = 2.583, CI95 1.785, 3.736).
Table 5.
HLA Class II associations with dcSSc
| HLA | Ctrl, n (%) | dcSSc, n (%) | Uncorrected P | Corrected P | OR (CI95) |
|---|---|---|---|---|---|
| Italy | |||||
| DRB1*1104 | 83 (10.4) | 38 (20.2) | <0.001 | 0.001 | 2.182 (1.43, 3.329) |
| DQA*0501 | 250 (31.3) | 87 (46.3) | <0.001 | <0.001 | 1.888 (1.366, 2.609) |
| DQB*03 | 301 (37.7) | 95 (50.5) | 0.001 | 0.02 | 1.687 (1.225, 2.322) |
| Spain | |||||
| DRB1*01 | 255 (13.8) | 12 (5.2) | <0.001 | 0.004 | 0.343 (0.189, 0.622) |
| DRB1*0402 | 27 (1.5) | 11 (4.8) | <0.001 | 0.02 | 3.38 (1.654, 6.909) |
| DRB1*1104 | 20 (1.1) | 26 (11.3) | <0.001 | <0.001 | 11.623 (6.375, 21.193) |
| DRB1*11 | 230 (12.5) | 49 (21.3) | <0.001 | 0.004 | 1.9 (1.346, 2.681) |
| DRB1*15 | 165 (8.9) | 36 (15.7) | 0.001 | 0.02 | 1.883 (1.278, 2.789) |
| DQB*0501 | 291 (15.8) | 14 (6.1) | <0.001 | 0.008 | 0.346 (0.199, 0.602) |
| DQB*05 | 358 (19.4) | 23 (10) | <0.001 | 0.007 | 0.461 (0.295, 0.72) |
HLA Class II significant associations with the diffuse cutaneous subset (dcSSc) (after 10 000-fold permutation testing) in Italy and Spain. Total number of alleles per series: Italy, dcSSc = 188; controls = 798; Spain, dcSSc = 230; Ctrl = 1844. Ctrl: control.
Table 6.
HLA Class II associations with lcSSc
| HLA | Ctrl, n (%) | lcSSc, n (%) | Uncorrected P | Corrected P | OR (CI95) |
|---|---|---|---|---|---|
| Italy | |||||
| DRB1*1104 | 83 (10.4) | 100 (18.5) | <0.001 | <0.001 | 1.949 (1.423, 2.669) |
| DQA*0501 | 250 (31.3) | 231 (42.6) | <0.001 | <0.001 | 1.628 (1.298, 2.042) |
| DQA*05 | 326 (40.8) | 274 (50.5) | <0.001 | 0.01 | 1.48 (1.188, 1.844) |
| Spain | |||||
| DRB1*0701 | 283 (15.3) | 59 (9.1) | <0.001 | 0.003 | 0.055 (0.412, 0.745) |
| DRB1*0801 | 46 (2.5) | 36 (5.6) | <0.001 | 0.004 | 2.307 (1.477, 3.602) |
| DRB1*1104 | 20 (1.1) | 38 (5.9) | <0.001 | <0.001 | 5.7 (3.291, 9.871) |
| DRB1*1301 | 135 (7.3) | 22 (3.4) | <0.001 | 0.01 | 0.446 (0.282, 0.707) |
| DQA*0103 | 158 (8.6) | 26 (4.0) | <0.001 | 0.004 | 0.447 (0.293, 0.684) |
| DQA*0401 | 58 (3.1) | 43 (6.7) | <0.001 | 0.003 | 2.196 (1.464, 3.293) |
| DQB*0402 | 61 (3.3) | 44 (6.8) | <0.001 | 0.004 | 2.136 (1.434, 3.182) |
| DQB*05 | 358 (19.4) | 163 (25.3) | 0.002 | 0.02 | 1.401 (1.133, 1.731) |
HLA Class II significant associations with the limited cutaneous subset (lcSSc) (after 10 000-fold permutation testing) in Italy and Spain. Total number of alleles per series—Italy: lcSSc = 542; Ctrl = 798; Spain: lcSSc = 646; Ctrl = 1844. Ctrl: controls.
Meta-analysis for the HLA-DRB1*1104 yielded inconsistent results due to heterogeneity issues. The DQA1*0501 and the DQB1*0301 alleles, which are in tight LD with HLA-DRB1*1104 in the DR11 haplotype, were associated with the dcSSc and the lcSSc subset, respectively. These results suggest and confirm that indeed, in Caucasoids, the HLA-DRB1*1104 allele or the DR11 haplotype do not associate with a specific cutaneous subset.
As far as other associations with the dcSSc or lcSSc subsets were concerned (Tables 5 and 6), they mostly mirrored associations with ATAs or ACAs, respectively. A larger number of associations were observed in the Spanish series, most likely owing to the larger number of subjects or to the tighter link between autoantibodies and SSc subsets (Italy: P = 1 × 10−22; Spain: P = 1 × 10−38 for the ATA/ACA vs dcSSc/lcSSc comparison).
Discussion
The present study represents the largest ever performed in European Caucasoids and confirms and extends previous observations from North American Caucasoids [5]. We were able to replicate the strong association between the HLA-DRB1*11(04) allele(s) and SSc and, more notably, the association between the DR11 haplotype and scleroderma. To our knowledge, ours and Arnett et al.'s [5] studies are the first to describe a full HLA Class II haplotype analysis in SSc. The study of haplotypes provides several advantages over an analysis based on individual polymorphisms in the presence of multiple susceptibility alleles, including an increased power to detect an association in case–control studies, even when markers with multiple alleles, such as HLA, are taken into account [23].
Our analysis confirms that the well-documented association between the HLA-DRB1*11(04) allele and SSc in Caucasians is not restricted to any of the cutaneous subsets and that this allele is overrepresented in Scl70-positive patients. The latter finding may be related to the unique presence of a valine at position 86 of the antigen-binding region, which may affect peptide binding [24] and autoantigen presentation, promoting autoimmunity [25]. A different, yet similar, mechanism may favour the presentation of self or foreign peptides to autoreactive T lymphocytes via the HLA-DRB1*01 allele to promote the production of ACAs. The peculiar conformation of the antigen-presenting cleft of the HLA-DRB1*01 or HLA-DRB1*11(04) alleles would thus determine the targeting of particular autoantigens, which eventually results in specific associations with disease-specific autoantibodies. The finding that in SSc patients ACAs and ATAs are substantially mutually exclusive [26] suggests that their production is the result of a different activation of the immune system. These autoimmune processes may eventually lead to different clinical entities where, for instance, ATAs are associated with interstitial pulmonary fibrosis and cardiac involvement, whereas ACAs are associated with pulmonary arterial hypertensions [27–29]. Preliminary studies suggest that it could be possible to dampen MHC-driven autoimmune processes by directly and selectively targeting the antigen-presenting region on MHC molecules [30]. Whether this strategy could provide an effective means of immunointervention in SSc remains an intriguing possibility to be verified in the future.
HLA Class II may also contribute to the pathogenesis and progression of SSc by other mechanisms that do not involve antigen presentation. It has been observed that HLA Class II may transduce the signals into fibroblasts promoting the secretion of IL-6 and monocyte chemoattractant protein 1 (MCP-1) [31], whose levels are increased in SSc patients, particularly in those clinical forms that are associated with ATAs [32].
The robust identification of SSc-associated HLA alleles in large cohorts may have important practical implications for an improved understanding of SSc development, progression and treatment. Despite high ORs and very low P-values, the discriminative and prognostic value of HLA Class II alleles in SSc remains weak, with a balanced predictive accuracy (e.g. the mathematical mean of sensitivity and specificity) no greater than 55% in the meta-analysis that we conducted (results not shown). Thus, we believe our findings, especially those from the meta-analysis, may primarily serve as a tool to focus future research on the characterization of the mechanisms that promote the development of SSc, may they be related or not to antigen presentation.
Supplementary data
Supplementary data are available at Rheumatology Online.
Acknowledgements
J.M. was sponsored by grants SAF2009-1110, CTS-4977, CTS-180, by RETCIS program, RD08/0075 from Instituto de Salud Carlos III (ISCIII) and by the Orphan Disease Program grant from the European League Against Rheumatism (EULAR).
Funding: This work was supported in part by NIH grants UO1AI090909-1, FIS 07/0061 and CTS-197.
Disclosure statement: The authors have declared no conflicts of interest.
References
- 1.Silver RM. Clinical aspect of systemic sclerosis (scleroderma) Ann Rheum Dis. 1991;50:854–61. doi: 10.1136/ard.50.suppl_4.854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Varga J, Abraham D. Systemic sclerosis: a prototypic multisystem fibrotic disorder. J Clin Invest. 2007;117:557–67. doi: 10.1172/JCI31139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agarwal SK, Reveille JD. The genetics of scleroderma (systemic sclerosis) Curr Opin Rheumatol. 2010;22:133–8. doi: 10.1097/BOR.0b013e3283367c17. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal SK, Tan FK, Arnett FC. Genetics and genomic studies in scleroderma (systemic sclerosis) Rheum Dis Clin North Am. 2008;34:17–40. doi: 10.1016/j.rdc.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Arnett FC, Gourh P, Shete S, et al. Major histocompatibility complex (MHC) class II alleles, haplotypes, and epitopes which confer susceptibility or protection in the fibrosing autoimmune disease systemic sclerosis: analyses in 1300 Caucasian, African-American and Hispanic cases and 1000 controls. Ann Rheum Dis. 2010;69:822–7. doi: 10.1136/ard.2009.111906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Briggs D, Welsh KI. Major histocompatibility complex class II genes and systemic sclerosis. Ann Rheum Dis. 1991;50:862–5. doi: 10.1136/ard.50.suppl_4.862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simeón CP, Fonollosa V, Tolosa C, et al. Association of HLA class II genes with systemic sclerosis in Spanish patients. J Rheumatol. 2009;36:2733–6. doi: 10.3899/jrheum.090377. [DOI] [PubMed] [Google Scholar]
- 8.Frezza D, Giambra V, Tolusso B, et al. Polymorphism of immunoglobulin enhancer element HS1,2A: allele *2 associates with systemic sclerosis. Comparison with HLA-DR and DQ allele frequency. Ann Rheum Dis. 2007;66:1210–5. doi: 10.1136/ard.2006.066597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Favalli E, Ingegnoli F, Zeni S, et al. [HLA typing in sistemi sclerosis] Reumatismo. 2001;53:210–4. doi: 10.4081/reumatismo.2001.210. [DOI] [PubMed] [Google Scholar]
- 10.Vlachoyiannopoulos PG, Dafni UG, Pakas I, et al. Systemic scleroderma in Greece: low mortality and strong linkage with HLA-DRB1*1104 allele. Ann Rheum Dis. 2000;59:359–67. doi: 10.1136/ard.59.5.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fanning GC, Welsh KI, Bunn C, et al. HLA associations in three mutually exclusive autoantibody subgroups in UK systemic sclerosis patients. Br J Rheumatol. 1998;37:201–7. doi: 10.1093/rheumatology/37.2.201. [DOI] [PubMed] [Google Scholar]
- 12.Hietarinta M, Ilonen J, Lassila O, Hietaharju A. Association of HLA antigens with anti-Scl-70-antibodies and clinical manifestations of systemic sclerosis (scleroderma) Br J Rheumatol. 1994;33:323–6. doi: 10.1093/rheumatology/33.4.323. [DOI] [PubMed] [Google Scholar]
- 13.Preliminary criteria for the classification of systemic sclerosis (scleroderma) Subcommittee for scleroderma criteria of the American Rheumatism Association Diagnostic and Therapeutics Criteria Committee. Arthritis Rheum. 1980;23:581–90. doi: 10.1002/art.1780230510. [DOI] [PubMed] [Google Scholar]
- 14.Hudson M, Taillefer S, Steele R, et al. Improving the sensitivity of the American College of Rheumatology classification criteria for systemic sclerosis. Clin Exp Rheumatol. 2007;25:754–7. [PubMed] [Google Scholar]
- 15.LeRoy EC, Black C, Fleischmajer R, et al. Scleroderma (systemic sclerosis): classification, subset and pathogenesis. J Rheumatol. 1988;15:202–5. [PubMed] [Google Scholar]
- 16.Le Roy EC, Medsger TA., Jr Criteria for the classification of early systemic sclerosis. J Rheumatol. 2001;28:1573–6. [PubMed] [Google Scholar]
- 17.Dalva K, Beksac M. Sequence-specific primed PCR (PCR-SSP) typing of HLA Class I and Class II alleles. Methods Mol Med. 2007;134:51–60. doi: 10.1007/978-1-59745-223-6_4. [DOI] [PubMed] [Google Scholar]
- 18.Good PI. Permutation tests. A practical guide to resampling methods for testing hypotheses. New York: Springer; 2000. [Google Scholar]
- 19.Cheverud JM. A simple correction for multiple comparisons in interval mapping genome scans. Heredity. 2001;87:52–8. doi: 10.1046/j.1365-2540.2001.00901.x. [DOI] [PubMed] [Google Scholar]
- 20.Stephens M, Smith N, Donnelly P. A new statistical method for haplotype reconstruction from population data. Am J Hum Genet. 2001;68:978–89. doi: 10.1086/319501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bryc K, Velez C, Karafet T, et al. Colloquium paper: genome-wide patterns of population structure and admixture among Hispanic/Latino populations. Proc Natl Acad Sci USA. 2010;107:8954–61. doi: 10.1073/pnas.0914618107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bax L, Yu LM, Ikeda N, et al. Development and validation of MIX: comprehensive free software for meta-analysis of causal research data. BMC Med Res Methodol. 2006;6:50. doi: 10.1186/1471-2288-6-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 24.Ong B, Willcox N, Wordsworth P, et al. Critical role for the Val/Gly86 HLA-DR beta dimorphism in autoantigen presentation to human T cells. Proc Natl Acad Sci USA. 1991;88:7343–7. doi: 10.1073/pnas.88.16.7343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Busch R, Hill CM, Hayball JD, et al. Effect of natural polymorphism at residue 86 of the HLA-DR beta chain on peptide binding. J Immunol. 1991;147:1292–8. [PubMed] [Google Scholar]
- 26.Dick T, Mierau R, Bartz-Bazzanella P, et al. Coexistence of antitopoisomerase I and anticentromere antibodies in patients with systemic sclerosis. Ann Rheum Dis. 2002;1:121–7. doi: 10.1136/ard.61.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Steen VD, Powell DL, Medsger TA., Jr Clinical correlations and prognosis based on serum autoantibodies in patients with systemic sclerosis. Arthritis Rheum. 1988;31:196–203. doi: 10.1002/art.1780310207. [DOI] [PubMed] [Google Scholar]
- 28.Ferri C, Valentini G, Cozzi F, et al. Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine. 2002;81:139–53. doi: 10.1097/00005792-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 29.Hamaguchi Y. Autoantibody profiles in systemic sclerosis: predictive value for clinical evaluation and prognosis. J Dermatol. 2010;37:42–53. doi: 10.1111/j.1346-8138.2009.00762.x. [DOI] [PubMed] [Google Scholar]
- 30.Oshima M, Deitiker P, Atassi MZ. Targeting the antigen-binding site of HLA-restricting alleles in treatment of autoimmune disease. Crit Rev Immunol. 2007;27:271–88. doi: 10.1615/critrevimmunol.v27.i3.60. [DOI] [PubMed] [Google Scholar]
- 31.Ohyama H, Nishimura F, Meguro M, et al. Counter-antigen presentation: fibroblasts produce cytokines by signalling through HLA class II molecules without inducing T-cell proliferation. Cytokine. 2002;17:175–81. doi: 10.1006/cyto.2001.0976. [DOI] [PubMed] [Google Scholar]
- 32.Scala E, Pallotta S, Frezzolini A, et al. Cytokine and chemokine levels in systemic sclerosis: relationship with cutaneous and internal organ involvement. Clin Exp Immunol. 2004;138:540–6. doi: 10.1111/j.1365-2249.2004.02642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


