Abstract
Since 1996, 16 states and the District of Columbia in the United States have enacted legislation to decriminalize marijuana for medical use. Although marijuana is the most commonly detected nonalcohol drug in drivers, its role in crash causation remains unsettled. To assess the association between marijuana use and crash risk, the authors performed a meta-analysis of 9 epidemiologic studies published in English in the past 2 decades identified through a systematic search of bibliographic databases. Estimated odds ratios relating marijuana use to crash risk reported in these studies ranged from 0.85 to 7.16. Pooled analysis based on the random-effects model yielded a summary odds ratio of 2.66 (95% confidence interval: 2.07, 3.41). Analysis of individual studies indicated that the heightened risk of crash involvement associated with marijuana use persisted after adjustment for confounding variables and that the risk of crash involvement increased in a dose-response fashion with the concentration of 11-nor-9-carboxy-delta-9-tetrahydrocannabinol detected in the urine and the frequency of self-reported marijuana use. The results of this meta-analysis suggest that marijuana use by drivers is associated with a significantly increased risk of being involved in motor vehicle crashes.
Keywords: accidents, traffic; automobiles; cannabis; motor vehicles; substance abuse detection
In the United States, marijuana possession and use were banned by the Controlled Substances Act of 1970; however, in the last 14 years, 16 states and the District of Columbia have enacted legislation to decriminalize medical marijuana (1–3). For nearly half a century, decriminalization of marijuana has been an issue of international debate (4–9). Recent support for decriminalization and legalization of marijuana has been motivated partly by the established and putative medical benefits of this substance. Efficacy studies of marijuana in the United States have been limited by categorization of marijuana as a schedule I drug—a classification reserved for drugs with “no currently accepted medical use” (10–13). Despite this classification, a number of studies have shown the efficacies of marijuana in reducing muscle spasms, increasing appetite, reducing ocular pressure, and relieving pain (14–28). These medical benefits notwithstanding, marijuana is a psychoactive substance associated with distortion of time, increased reaction time, decreased sensory perception, and loss of coordination (29–31). Furthermore, long-term use has been associated with a host of adverse effects, including cognitive impairment, respiratory symptoms, suppression of the immune system, dizziness, memory loss, loss of decision-making capability, psychosis, and other mental health disorders (8, 30, 32–38).
The relation between marijuana use and motor vehicle crashes has been examined using both experimental and observational approaches (39). Simulator and laboratory studies have found that a component of marijuana—delta-9-tetrahydrocannabinol (THC)—is associated with decreased driving performance (40). Experimental studies have shown modest functional impairment, but debate exists over how well these experimental studies translate into real-life driving situations (41). Epidemiologic studies, however, have shown contradictory results (39, 42, 43). Some studies indicate that marijuana use alone has minimal effect on driving performance, while others report an increased crash risk particularly when combined with other drugs or used within 4 hours prior to driving (39, 42–45). A few studies suggest a dose-response association of whole-blood THC concentration with crash risk and crash culpability (39, 45, 46). It is evident that marijuana users may engage in compensatory behaviors that may mitigate some sensory and motor deficits (41, 47).
Drug-impaired driving has emerged as a serious public safety concern in the United States. In the 2009 National Survey on Drug Use and Health, 10.5 million persons 12 or more years of age were estimated to have driven under the influence of illicit drugs in the prior year (48). Furthermore, studies show that marijuana is the most commonly detected drug other than alcohol among US drivers (42, 49, 50). Although epidemiologic studies have identified a variety of drugs such as benzodiazepines, amphetamines, hypnotics, opiates, and antidepressants as independent risk factors for motor vehicle crashes (51–55), it is unclear whether marijuana plays a significant role in crash causation. To assess the empiric evidence for the effect of marijuana use on driving safety, and to inform policy development regarding medical marijuana, we performed a meta-analysis of epidemiologic studies examining the association of marijuana use by drivers with crash risk.
METHODS
This meta-analysis follows the guidelines put forth in the PRISMA statement and MOOSE guidelines for reporting systematic reviews and meta-analyses of observational studies in epidemiology (56, 57).
Eligibility criteria
Studies were eligible for analysis if they presented data on marijuana use based on laboratory tests or self-reports. Articles not published in the English language, published before 1990, or based on secondary analyses of previously published data were excluded. Also excluded from the analysis were roadside surveys of drug prevalence and other studies that contained no crash data (e.g., studies based on data for drivers pulled over by law enforcement for suspected driving under the influence of drugs, experimental studies in which human subjects were given marijuana, and studies that investigated driving infractions). Additionally, case-series studies and studies without a comparison group of drivers at risk of being involved in a crash were excluded.
Information sources and search
We performed a systematic search of the medical and transportation literature for epidemiologic studies related to marijuana use and motor vehicle crashes using PubMed Medline (1949–present), Cochrane Library (1960–present), Cumulative Index to Nursing and Allied Health Literature (1981–present), Allied and Complementary Medicine Database (1985–present), Health and Psychosocial Instruments (1985–present), American Psychological Association Psyc Info (1967–present), and ISI Web of Knowledge (1968–present). (The most recent search was conducted on November 24, 2010. A limited update was performed from November 24, 2010, to June 9, 2011.) The following search terms were used for all databases: “marijuana,” “THC,” and “cannabi*” in combination with the terms “motor vehicle,” “crash,” “driving,” “accidents,” and “systematic.” We used the “related citations” feature to capture additional references for selected articles. We also examined the references of papers we considered relevant to the search. We included studies that addressed the issue of crash risk. Our search strategy was not peer reviewed.
Study selection and data collection
Studies identified as potentially relevant based on electronic search results were entered into the computer program EndNote X3 (58) for further investigation. Duplicate articles were removed, and abstracts were reviewed to remove nonrelevant studies. Full-text files were obtained for each of the remaining articles. These remaining articles were then reviewed based on eligibility criteria. Eligibility assessment was performed independently in a standardized manner by 2 trained reviewers (M. L. and J. E. B.). Disagreements between the 2 reviewers were resolved by 2 senior researchers (C. J. D. and G. L.). In 3 instances in which data were missing or incomplete, we attempted to contact the corresponding authors for further information and were able to receive the requested information from one of these authors. One of the present authors (M. L.) reviewed full-text versions of articles entered into the study database, coding the following variables: sample size, study population characteristics, study design, study outcome (crash risk), and type of assessment (e.g., blood, urine, or self-report). The study-level data were then checked and verified by 3 coauthors (J. E. B., C. J D., and G. L.). Study quality was assessed by using a 28-item critical appraisal checklist (59). Where possible, data were extracted to directly calculate unadjusted odds ratios of crash involvement associated with marijuana use.
Data analysis
For each study, we calculated an unadjusted odds ratio measuring the association between marijuana use and crash risk. We analyzed these point estimates for heterogeneity of the mean effect size by using the Q statistic (60) and generated a summary odds ratio based on the random-effects model. To assess heterogeneity, we conducted analyses stratified by study design, type of drug assessment, study time period, study location, and age of study subjects. We assessed publication bias with funnel plots and Rosenthal’s (61) fail-safe N and conducted analyses in Excel software (Microsoft Corporation, Redmond, Washington) and in Comprehensive Meta Analysis version 2 (Biostat Inc., Englewood, New Jersey).
RESULTS
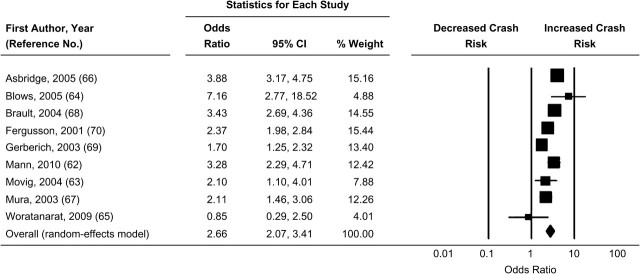
The electronic database search returned 2,960 references. Duplicates and studies published prior to 1990 were then removed, leaving 831 references to be reviewed. Following the abstract and title review, commentaries, case reports, general review articles, essays, and other ineligible studies were removed, leaving 122 studies deemed relevant to marijuana use and driving safety. Full-text articles for the 122 studies were retrieved for further review. Of those 122 articles, 8 were found to contain data for assessing crash risk. We identified an additional 17 studies of possible relevance through manual review of the references cited in the 8 articles from which we extracted data. Of these 17 studies, 1 met the inclusion criteria and was added to the meta-analysis (Figure 1). Critical appraisal of the studies included in our analysis revealed that they were of high quality and credibility.
Figure 1.
Identification, review, and selection of articles included in the meta-analysis of marijuana use and motor vehicle crashes. AMED, Allied and Complementary Medicine Database; APA Psych Info, American Psychological Association Psych Info; CINAHL, Cumulative Index to Nursing and Allied Health Literature.
Characteristics of included studies
Four of the 9 eligible studies were based on inner city or urban populations (62–65), 1 study was based on a population that was more than 50% rural (66), and the remaining 4 studies contained no data regarding location (67–70). Two of the 9 selected papers included study populations that were more than 50% white (64, 69). The remaining 7 studies did not provide data regarding the ethnicities of the populations (62, 63, 65–68, 70). Four studies addressed populations that were more than 50% male (63–65, 68), 3 studies addressed populations that were more than 50% female (62, 66, 69), and the remaining 2 studies did not provide data regarding gender (67, 70). Two studies explicitly studied adolescents and young adults (66, 70). One of the 9 eligible studies involved fatal crashes (68), 6 studies exclusively addressed nonfatal crashes (62, 64–67, 69), and 2 studies assessed both types (63, 70).
Marijuana use and crash risk
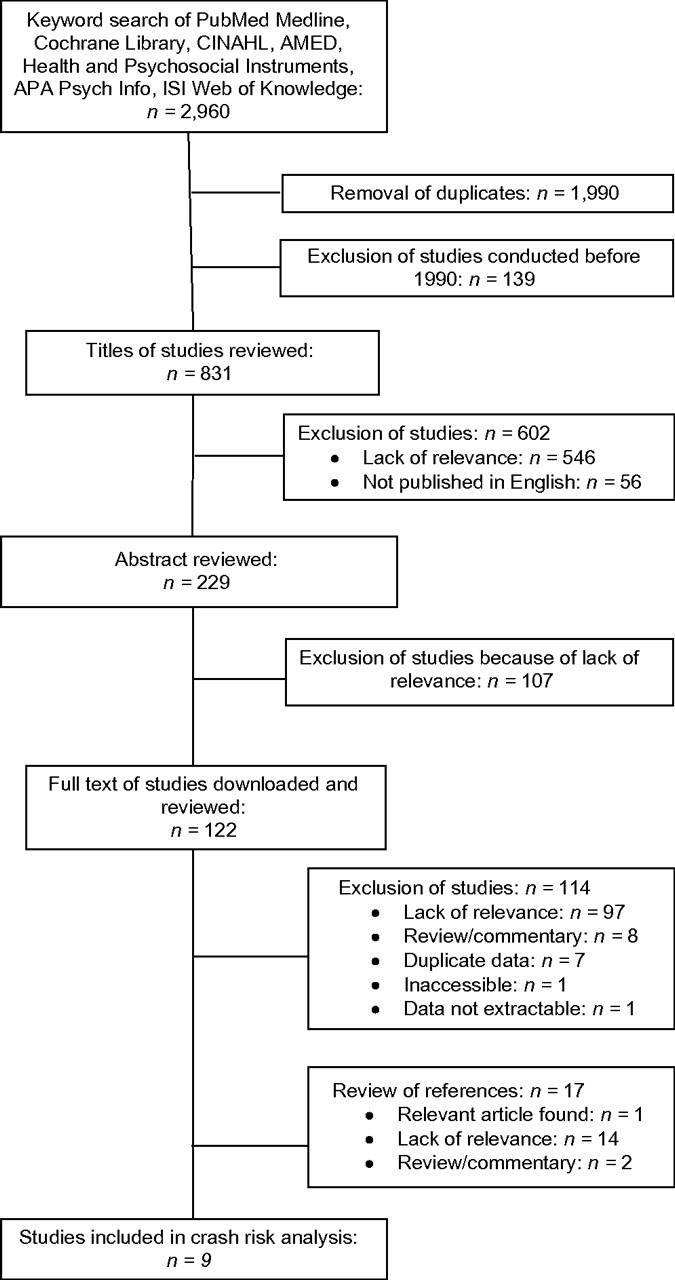
The 9 studies included in this meta-analysis were conducted in 6 different countries (Table 1). Of the 9 studies, 2 were cross-sectional surveys, 5 were case-control analyses, and 2 had a cohort design. Five studies assessed marijuana use based on self-reported data, and 4 were based on urine or blood tests (Table 1). All of the studies except one (65) reported a statistically significantly increased risk of crash involvement associated with marijuana use (Figure 2). The estimated odds ratios were heterogeneous across the studies (Q statistic chi-square = 38.21, degrees of freedom = 8, P < 0.001; I2 = 79.1). The summary odds ratio estimated from the random-effects model was 2.66 (95% confidence interval: 2.07, 3.41). Rosenthal’s fail-safe N indicated that 705 additional null effects (P < 0.001) would be needed to render the overall effect size estimate nonsignificant at the P = 0.05 level.
Table 1.
Characteristics of Studies Evaluating the Association of Marijuana Use With Motor Vehicle Crash Involvement
| First Author, Year (Reference No.) | Study Subjects | No. Involved in Crash | Marijuana Use, % | No. Not Involved in Crash | Marijuana Use, % | Country of Origin | Study Design | Study Time Period | Exposure to Marijuana Assessed | Source of Exposure Data |
| Asbridge, 2005 (66) | High school seniors | 485 | 36.1 | 5,527 | 12.7 | Canada | Cross-sectional survey | 2002–2003 | Driving within 1 hour of marijuana use | Self-report |
| Blows, 2005 (64) | Drivers from all age groups | 552 | 5.8 | 587 | 0.9 | New Zealand | Case-control | March 1998–July 1999 | Driving within 3 hours of marijuana use | Self-report |
| Brault, 2004 (68) | Drivers aged 16 years or older | 512 | 19.7 | 5,931 | 6.7 | Canada | Case-control | April 1999–December 2002 | Metabolite of THC | Urine test |
| Fergusson, 2001 (70) | Drivers aged 18–21 years | 626a | 56.1 | 2,095a | 35.0 | New Zealand | Prospective cohort | 1977–1998 | Marijuana use in the past year | Self-report |
| Gerberich, 2003 (69) | Members of a medical insurance program aged 15–49 years | 188 | 31.9 | 64,469 | 21.6 | United States | Retrospective cohort | 1979–1985 | Currently using marijuana or having used marijuana 6 times or more during lifetime | Self-report |
| Mann, 2010 (62) | Drivers aged 18 years or older | 634 | 6.2 | 7,819 | 2.0 | Canada | Cross-sectional survey | 2002–2007 | Driving within an hour of marijuana use | Self-report |
| Movig, 2004 (63) | Drivers aged 18 years or older | 110 | 11.8 | 816 | 6.0 | The Netherlands | Case-control | May 2000–August 2001 | THC and metabolites | Urine and/or blood test |
| Mura, 2003 (67) | Drivers aged 18 years or older treated in emergency rooms | 900 | 10.0 | 900 | 5.0 | France | Case-control | June 2000–September 2001 | THC | Blood test |
| Woratanarat, 2009 (65) | Drivers aged 15 years or older | 200 | 2.0 | 849 | 2.4 | Thailand | Case-control | February 2006–December 2006 | Marijuana | Urine test |
Abbreviation: THC, delta-9-tetrahydrocannabinol.
No. of person-years at risk.
Figure 2.
Forest plot of study level, summary odds ratio, and 95% confidence interval (CI) of crash involvement associated with marijuana use. The size of each square is proportional to the relative weight that each study contributed to the summary odds ratio. The summary odds ratio is indicated by the diamond. Horizontal bars indicate the 95% confidence interval. Heterogeneity: Q = 38.21; P < 0.0001; I2 = 79.1.
Effect size by study characteristics
The data were stratified and analyzed according to study design, type of drug assessment, study time period, study location, or age of the study subjects. A more than 2-fold increased crash risk associated with marijuana use was found in each of the subsets of studies (Table 2).
Table 2.
Random-effects Summary Odds Ratios and 95% Confidence Intervals of Crash Involvement Associated With Marijuana Use, by Study Characteristics
| Study Characteristic | OR | 95% CI |
| Study design | ||
| Case-control | 2.63 | 1.87, 3.71 |
| Cohort | 2.04 | 1.36, 3.07 |
| Cross-sectional | 3.61 | 2.37, 5.49 |
| Type of drug assessment | ||
| Self-report | 2.93 | 2.07, 4.17 |
| Blood or urine test | 2.26 | 1.46, 3.49 |
| Study time period | ||
| Before 2000 | 2.82 | 1.77, 4.50 |
| 2000 and after | 2.58 | 1.89, 3.53 |
| Study location | ||
| North America | 2.97 | 2.13, 4.14 |
| Other | 2.31 | 1.59, 3.35 |
| Age of study subjects | ||
| <25 years | 3.03 | 1.83, 5.01 |
| All ages | 2.50 | 1.81, 3.46 |
Abbreviations: CI, confidence interval; OR, odds ratio.
Adjustment for confounding variables
Five of the 9 studies (62–64, 66, 68) reported odds ratios adjusted for a variety of covariates, including alcohol use. While adjustment for confounding variables generally attenuated the estimated effect size to some degree, all the adjusted odds ratios except one (64) remained statistically significant (data not shown).
Dose-response effect
Two studies (68, 70) provided data for assessing the dose-response relation between marijuana use and crash risk. Brault et al. (68) found that the risk of crash involvement increased progressively with the concentration of 11-nor-9-carboxy-THC (THC-COOH); relative to that for drivers testing negative for the substance, the estimated odds ratios of crash involvement were 1.1 (95% confidence interval: 0.5, 2.6) for those with low THC-COOH concentrations in their urine, 1.8 (95% confidence interval: 1.0, 3.5) for those with medium THC-COOH concentrations, and 3.3 (95% confidence interval: 1.9, 5.9) for those with high THC-COOH concentrations. Fergusson and Horwood (70) found that the risk of crash involvement increased significantly as self-reported frequency of marijuana use in the past year increased.
DISCUSSION
Results of this meta-analysis indicate that marijuana use by drivers is associated with a significantly increased risk of crash involvement. Specifically, drivers who test positive for marijuana or self-report using marijuana are more than twice as likely as other drivers to be involved in motor vehicle crashes. The increased risk of crash involvement associated with marijuana use is generally consistent across studies that were conducted in different geographic regions and driver populations, used different research design approaches, and were based on different methods for measuring marijuana use. Of the 9 studies included in the meta-analysis, all but one found a statistically significant association between marijuana use and crash risk. The only study that failed to detect a significant association between marijuana use and crash risk was a small case-control study conducted in Thailand (65), where the prevalence of marijuana use appears to be far lower than reported elsewhere (63, 67, 68). The validity of the association between marijuana use and crash risk is further strengthened by the empirical evidence that a dose-response relation exists between the dose and frequency of marijuana use by drivers and their risk of being involved in motor vehicle crashes (68, 70).
The crash risk associated with marijuana, if confirmed by further research, may have important implications for driving safety and public policy. Drug-impaired driving is a serious problem in the United States. Toxicologic testing data indicate that 28% of fatally injured drivers (71) and more than 11% of the general driver population test positive for nonalcohol drugs (72), with marijuana being the most commonly detected substance.
Although this meta-analysis provides compelling evidence for an association between marijuana use and crash risk, it is impossible to infer causality from these epidemiologic data alone. A more rigorous assessment of the nature of the relation between marijuana use and crash risk is complicated by several factors. Among them are bias from measured and unmeasured confounding and the difficulty posed by polydrug use. Although most of the studies included in this meta-analysis considered some confounding variables in evaluating the association between marijuana use and crash risk, adjustment was usually limited to a few measured covariates, such as age, sex, and alcohol use. Additional variables that may confound the relation between marijuana use and crash risk, such as exposure to driving and risk-taking propensity, are often difficult to measure and thus are not readily available. Other factors confounding the relation between marijuana use and crash risk are divergent definitions and assessments of marijuana use across studies.
Different methods of assessing marijuana use (e.g., self-report, urine tests, and blood tests) may have different levels of validity and reliability (39). Most of these screenings determine whether marijuana was used within the past few weeks, whereas acute impairment in driving skills from marijuana use lasts only 3–4 hours (39). Furthermore, because marijuana is an illicit drug in most countries, it is possible that drivers in the comparison groups might be less likely than those involved in crashes to submit to testing, which could lead to overestimation of the effect of marijuana use on crash risk (43).
Polydrug use represents another challenge to determining the role of marijuana in motor vehicle crashes. Polydrug use by drivers is common, with up to a quarter of drivers injured in crashes testing positive for 2 or more drugs (including alcohol) (42, 73, 74). Although it is necessary to understand the effect of individual drugs on driving performance, the high prevalence of polydrug use by drivers makes it difficult to do so. On the other hand, assessing interaction effects on driving safety of different drug combinations based on epidemiologic data would require very large study samples, comprehensive drug testing data, and tremendous financial and other resources (42–44, 75, 76). One of the studies included in the meta-analysis evaluated the effect of marijuana in combination with alcohol on crash risk and found that the combination of marijuana and alcohol confers an exceptionally heightened risk to driving safety (68). Experimental studies show that cannabis and alcohol affect different cognitive functions that may interact with driving performance (41). Specifically, cannabis seems to impair automatic behaviors, such as tracking, at low doses and impair ability to perform more complex tasks at higher doses, whereas alcohol seems to more readily affect functions requiring cognitive control (41). While both marijuana and alcohol can impair driving performance, there appears to be greater variations in effects of marijuana compared with alcohol (41).
It is worth noting that the studies included in this meta-analysis did not directly assess medical marijuana use. Recreational marijuana is often administered differently than medical marijuana. The Institute of Medicine advises against smoking marijuana, the typical method of recreational consumption, and recommends using pills or a vaporizer (77). The cannabinol and THC components in pills do not entirely correspond to the components in the plant form of the substance (17, 77, 78). Medical marijuana, including cannabinoid medicines, may be administered in regulated doses, whereas recreational use is less quantifiable (78). It is conceivable that differences in administration modes and dosages of marijuana between medical use and recreational use may have different effects on driving ability and crash risk. Although legislation permitting medical marijuana use and marijuana decriminalization has proliferated in the United States, many state medical marijuana laws include provisions prohibiting driving under the influence of marijuana. Quantifying the excess crash risk associated with marijuana use is essential for understanding the overall health consequences of legalizing medical marijuana and the effectiveness of policy interventions on drug-impaired driving in reducing injury morbidity and mortality from motor vehicle crashes.
CONCLUSIONS
Epidemiologic studies published in the past 2 decades demonstrate that marijuana use by drivers is associated with a significantly increased crash risk. The crash risk appears to increase progressively with the dose and frequency of marijuana use. The empiric evidence supporting the association between marijuana use and crash risk was derived from studies conducted in different countries and based on different research designs. To further assess the role of marijuana use in motor vehicle crashes, additional research is needed to rigorously address the effects on crash risk of dose, recency, and administrative modes of marijuana and of marijuana in combination with other drugs. Given the ongoing epidemic of drug-impaired driving and the increased permissibility and accessibility of marijuana for medical use in the United States, it is urgent to better understand the role of marijuana in crash causation and outcomes.
Acknowledgments
Author affiliations: Department of Anesthesiology, Columbia University College of Physicians and Surgeons, New York, New York (Charles J. DiMaggio, Guohua Li, Joanne E. Brady, Arielle R. Lusardi, Mu-Chen Li, Keane Y. Tzong); and Department of Epidemiology, Columbia University Mailman School of Public Health, New York, New York (Charles J. DiMaggio, Guohua Li, Joanne E. Brady).
This work was supported by grant R01AA009963 from the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health and by grant R21DA029670 from the National Institute on Drug Abuse, National Institutes of Health.
The authors thank Barbara Lang for her editorial and administrative assistance.
Conflict of interest: none declared.
Glossary
Abbreviations
- THC
delta-9-tetrahydrocannabinol
- THC-COOH
11-nor-9-carboxy-THC
References
- 1.Controlled Substances Act, 21 USC §801. 2007 ( http://www.deadiversion.usdoj.gov/21cfr/21usc/801.htm). (Accessed August 2, 2011) [Google Scholar]
- 2.Yarett I. How high are you? Newsweek. 2010;155(7):56. [Google Scholar]
- 3.Santa Monica, CA: ProCon.org; 15 Legal medical marijuana states and DC: laws, fees, and possession limits. ( http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881). (Accessed December 16, 2010) [Google Scholar]
- 4.Ndetei DM, Arboleda-Flórez J, Gawad T. Forum: decriminalization versus criminalization of cannabis. Curr Opin Psychiatry. 2008;21(2):127–128. doi: 10.1097/YCO.0b013e3282f57e24. [DOI] [PubMed] [Google Scholar]
- 5.Cohen PJ. Medical marijuana: the conflict between scientific evidence and political ideology. Part one of two. J Pain Palliat Care Pharmacother. 2009;23(1):4–25. doi: 10.1080/15360280902727973. [DOI] [PubMed] [Google Scholar]
- 6.Reinarman C, Cohen PD, Kaal HL. The limited relevance of drug policy: cannabis in Amsterdam and in San Francisco. Am J Public Health. 2004;94(5):836–842. doi: 10.2105/ajph.94.5.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Medical marijuana on trial. Lancet Oncol. 2001;2(5):251. doi: 10.1016/s1470-2045(00)00334-x. [DOI] [PubMed] [Google Scholar]
- 8.Martin BR. Medical marijuana—moving beyond the smoke. Lancet. 2002;360(9326):4–5. doi: 10.1016/S0140-6736(02)09360-1. [DOI] [PubMed] [Google Scholar]
- 9.Christenson V. Courts protect Ninth Circuit doctors who recommend medical marijuana use. J Law Med Ethics. 2004;32(1):174–177. doi: 10.1111/j.1748-720x.2004.tb00463.x. [DOI] [PubMed] [Google Scholar]
- 10.Hoffmann DE, Weber E. Medical marijuana and the law. N Engl J Med. 2010;362(16):1453–1457. doi: 10.1056/NEJMp1000695. [DOI] [PubMed] [Google Scholar]
- 11.Controlled Substances Act, 21 USC §812. 2007 ( http://www.deadiversion.usdoj.gov/21cfr/21usc/812.htm). (Accessed August 2, 2011) [Google Scholar]
- 12.Gathering the evidence on medical marijuana. Nature. 2001;410(6829):613. doi: 10.1038/35070729. [DOI] [PubMed] [Google Scholar]
- 13.Cohen PJ. Medical marijuana 2010: it’s time to fix the regulatory vacuum. J Law Med Ethics. 2010;38(3):654–666. doi: 10.1111/j.1748-720X.2010.00519.x. [DOI] [PubMed] [Google Scholar]
- 14.Chang AE, Shiling DJ, Stillman RC, et al. Delta-9-tetrahydrocannabinol as an antiemetic in cancer patients receiving high-dose methotrexate. A prospective, randomized evaluation. Ann Intern Med. 1979;91(6):819–824. doi: 10.7326/0003-4819-91-6-819. [DOI] [PubMed] [Google Scholar]
- 15.Rog DJ, Nurmikko TJ, Friede T, et al. Randomized, controlled trial of cannabis-based medicine in central pain in multiple sclerosis. Neurology. 2005;65(6):812–819. doi: 10.1212/01.wnl.0000176753.45410.8b. [DOI] [PubMed] [Google Scholar]
- 16.Rog DJ, Nurmikko TJ, Sarantis NS, et al. A long-term open-label trial of safety and efficacy of Sativex®, a cannabis based medicine, in central neuropathic pain due to multiple sclerosis. J Neurol. 2006;253(suppl 2):S100. [Google Scholar]
- 17.Zajicek J, Fox P, Sanders H, et al. Cannabinoids for treatment of spasticity and other symptoms related to multiple sclerosis (CAMS study): multicentre randomised placebo-controlled trial. UK MS Research Group. Lancet. 2003;362(9395):1517–1526. doi: 10.1016/S0140-6736(03)14738-1. [DOI] [PubMed] [Google Scholar]
- 18.Zajicek JP, Sanders HP, Wright DE, et al. Cannabinoids in multiple sclerosis (CAMS) study: safety and efficacy data for 12 months follow up. J Neurol Neurosurg Psychiatry. 2005;76(12):1664–1669. doi: 10.1136/jnnp.2005.070136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Duran M, Pérez E, Abanades S, et al. Preliminary efficacy and safety of an oromucosal standardized cannabis extract in chemotherapy-induced nausea and vomiting. Br J Clin Pharmacol. 2010;70(5):656–663. doi: 10.1111/j.1365-2125.2010.03743.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ware MA, Wang T, Shapiro S, et al. Smoked cannabis for chronic neuropathic pain: a randomized controlled trial. CMAJ. 2010;182(14):E694–E701. doi: 10.1503/cmaj.091414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martín-Sánchez E, Furukawa TA, Taylor J, et al. Systematic review and meta-analysis of cannabis treatment for chronic pain. Pain Med. 2009;10(8):1353–1368. doi: 10.1111/j.1526-4637.2009.00703.x. [DOI] [PubMed] [Google Scholar]
- 22.Abrams DI, Jay CA, Shade SB, et al. Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology. 2007;68(7):515–521. doi: 10.1212/01.wnl.0000253187.66183.9c. [DOI] [PubMed] [Google Scholar]
- 23.Chang AE, Shiling DJ, Stillman RC, et al. A prospective evaluation of delta-9-tetrahydrocannabinol as an antiemetic in patients receiving adriamycin and cytoxan chemotherapy. Cancer. 1981;47(7):1746–1751. doi: 10.1002/1097-0142(19810401)47:7<1746::aid-cncr2820470704>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 24.Ellis RJ, Toperoff W, Vaida F, et al. Smoked medicinal cannabis for neuropathic pain in HIV: a randomized, crossover clinical trial. Neuropsychopharmacology. 2009;34(3):672–680. doi: 10.1038/npp.2008.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greenberg HS, Werness SA, Pugh JE, et al. Short-term effects of smoking marijuana on balance in patients with multiple sclerosis and normal volunteers. Clin Pharmacol Ther. 1994;55(3):324–328. doi: 10.1038/clpt.1994.33. [DOI] [PubMed] [Google Scholar]
- 26.Wilsey B, Marcotte T, Tsodikov A, et al. A randomized, placebo-controlled, crossover trial of cannabis cigarettes in neuropathic pain. J Pain. 2008;9(6):506–521. doi: 10.1016/j.jpain.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Merritt JC, Crawford WJ, Alexander PC, et al. Effect of marihuana on intraocular and blood pressure in glaucoma. Ophthalmology. 1980;87(3):222–228. doi: 10.1016/s0161-6420(80)35258-5. [DOI] [PubMed] [Google Scholar]
- 28.Turcotte D, Le Dorze JA, Esfahani F, et al. Examining the roles of cannabinoids in pain and other therapeutic indications: a review. Expert Opin Pharmacother. 2010;11(1):17–31. doi: 10.1517/14656560903413534. [DOI] [PubMed] [Google Scholar]
- 29.Barnes MP. Sativex: clinical efficacy and tolerability in the treatment of symptoms of multiple sclerosis and neuropathic pain. Expert Opin Pharmacother. 2006;7(5):607–615. doi: 10.1517/14656566.7.5.607. [DOI] [PubMed] [Google Scholar]
- 30.Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374(9698):1383–1391. doi: 10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- 31.Moskowitz H. Marihuana and driving. Accid Anal Prev. 1985;17(4):323–345. doi: 10.1016/0001-4575(85)90034-x. [DOI] [PubMed] [Google Scholar]
- 32.Solowij N, Stephens RS, Roffman RA, et al. Cognitive functioning of long-term heavy cannabis users seeking treatment. Marijuana Treatment Project Research Group. JAMA. 2002;287(9):1123–1131. doi: 10.1001/jama.287.9.1123. [DOI] [PubMed] [Google Scholar]
- 33.Tashkin DP, Coulson AH, Clark VA, et al. Respiratory symptoms and lung function in habitual heavy smokers of marijuana alone, smokers of marijuana and tobacco, smokers of tobacco alone, and nonsmokers. Am Rev Respir Dis. 1987;135(1):209–216. doi: 10.1164/arrd.1987.135.1.209. [DOI] [PubMed] [Google Scholar]
- 34.Aldington S, Williams M, Nowitz M, et al. Effects of cannabis on pulmonary structure, function and symptoms. Thorax. 2007;62(12):1058–1063. doi: 10.1136/thx.2006.077081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cabral GA, Dove Pettit DA. Drugs and immunity: cannabinoids and their role in decreased resistance to infectious disease. J Neuroimmunol. 1998;83(1-2):116–123. doi: 10.1016/s0165-5728(97)00227-0. [DOI] [PubMed] [Google Scholar]
- 36.Bolla KI, Brown K, Eldreth D, et al. Dose-related neurocognitive effects of marijuana use. Neurology. 2002;59(9):1337–1343. doi: 10.1212/01.wnl.0000031422.66442.49. [DOI] [PubMed] [Google Scholar]
- 37.Degenhardt L, Hall WD. The adverse effects of cannabinoids: implications for use of medical marijuana. CMAJ. 2008;178(13):1685–1686. doi: 10.1503/cmaj.080585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang T, Collet JP, Shapiro S, et al. Adverse effects of medical cannabinoids: a systematic review. CMAJ. 2008;178(13):1669–1678. doi: 10.1503/cmaj.071178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grotenhermen F, Leson G, Berghaus G, et al. Developing limits for driving under cannabis. Addiction. 2007;102(12):1910–1917. doi: 10.1111/j.1360-0443.2007.02009.x. [DOI] [PubMed] [Google Scholar]
- 40.MacDonald S, Anglin-Bodrug K, Mann RE, et al. Injury risk associated with cannabis and cocaine use. Drug Alcohol Depend. 2003;72(2):99–115. doi: 10.1016/s0376-8716(03)00202-3. [DOI] [PubMed] [Google Scholar]
- 41.Sewell RA, Poling J, Sofuoglu M. The effect of cannabis compared with alcohol on driving. Am J Addict. 2009;18(3):185–193. doi: 10.1080/10550490902786934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kelly E, Darke S, Ross J. A review of drug use and driving: epidemiology, impairment, risk factors and risk perceptions. Drug Alcohol Rev. 2004;23(3):319–344. doi: 10.1080/09595230412331289482. [DOI] [PubMed] [Google Scholar]
- 43.Bates MN, Blakely TA. Role of cannabis in motor vehicle crashes. Epidemiol Rev. 1999;21(2):222–232. doi: 10.1093/oxfordjournals.epirev.a017998. [DOI] [PubMed] [Google Scholar]
- 44.Walsh JM, de Gier JJ, Christopherson AS, et al. Drugs and driving. Traffic Inj Prev. 2004;5(3):241–253. doi: 10.1080/15389580490465292. [DOI] [PubMed] [Google Scholar]
- 45.Ramaekers JG, Berghaus G, van Laar M, et al. Dose related risk of motor vehicle crashes after cannabis use. Drug Alcohol Depend. 2004;73(2):109–119. doi: 10.1016/j.drugalcdep.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 46.Drummer OH, Gerostamoulos J, Batziris H, et al. The involvement of drugs in drivers of motor vehicles killed in Australian road traffic crashes. Accid Anal Prev. 2004;36(2):239–248. doi: 10.1016/s0001-4575(02)00153-7. [DOI] [PubMed] [Google Scholar]
- 47.MacDonald S, Mann R, Chipman M, et al. Driving behavior under the influence of cannabis or cocaine. Traffic Inj Prev. 2008;9(3):190–194. doi: 10.1080/15389580802040295. [DOI] [PubMed] [Google Scholar]
- 48.Substance Abuse and Mental Health Services Administration. Rockville, MD: Department of Health and Human Services; 2010. Results from the 2009 National Survey on Drug Use and Health: volume I. Summary of National Findings. NSDUH series H-38A, HHS publication SMA 10–4856 findings. ( http://oas.samhsa.gov/NSDUH/2k9NSDUH/2k9Results.htm#1.1). (Accessed November 1, 2010) [Google Scholar]
- 49.Jones RK, Shinar D, Walsh JM. State of Knowledge of Drug-Impaired Driving. Washington, DC: National Highway Traffic Safety Administration; 2003. [Google Scholar]
- 50.Walsh JM, Flegel R, Cangianelli LA, et al. Epidemiology of alcohol and other drug use among motor vehicle crash victims admitted to a trauma center. Traffic Inj Prev. 2004;5(3):254–260. doi: 10.1080/15389580490465319. [DOI] [PubMed] [Google Scholar]
- 51.Engeland A, Skurtveit S, Mørland J. Risk of road traffic accidents associated with the prescription of drugs: a registry-based cohort study. Ann Epidemiol. 2007;17(8):597–602. doi: 10.1016/j.annepidem.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 52.Smink BE, Egberts AC, Lusthof KJ, et al. The relationship between benzodiazepine use and traffic accidents: a systematic literature review. CNS Drugs. 2010;24(8):639–653. doi: 10.2165/11533170-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 53.Orriols L, Salmi LR, Philip P, et al. The impact of medicinal drugs on traffic safety: a systematic review of epidemiological studies. Pharmacoepidemiol Drug Saf. 2009;18(8):647–658. doi: 10.1002/pds.1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sansone RA, Sansone LA. Driving on antidepressants: cruising for a crash? Psychiatry (Edgmont) 2009;6(9):13–16. [PMC free article] [PubMed] [Google Scholar]
- 55.Gustavsen I, Bramness JG, Skurtveit S, et al. Road traffic accident risk related to prescriptions of the hypnotics zopiclone, zolpidem, flunitrazepam and nitrazepam. Sleep Med. 2008;9(8):818–822. doi: 10.1016/j.sleep.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 56.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 58.New York, NY: Thomson Reuters; 2009. Endnote (computer program). Version X3. [Google Scholar]
- 59.Centre for Occupational and Environmental Health, University of Manchester. Manchester, United Kingdom: University of Manchester, Centre for Occupational and Environmental Health; 2010. Critical appraisal checklist. ( http://www.medicine.manchester.ac.uk/oeh/undergraduate/specialstudymodules/criticalappraisal/). (Accessed June 17, 2011) [Google Scholar]
- 60.Lipsey MW, Wilson D. Practical Meta-Analysis. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- 61.Persaud R. Misleading meta-analysis. “Fail safe N” is a useful mathematical measure of the stability of results. BMJ. 1996;312(7023):125. doi: 10.1136/bmj.312.7023.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mann RE, Stoduto G, Ialomiteanu A, et al. Self-reported collision risk associated with cannabis use and driving after cannabis use among Ontario adults. Traffic Inj Prev. 2010;11(2):115–122. doi: 10.1080/15389580903536704. [DOI] [PubMed] [Google Scholar]
- 63.Movig KL, Mathijssen MP, Nagel PH, et al. Psychoactive substance use and the risk of motor vehicle accidents. Accid Anal Prev. 2004;36(4):631–636. doi: 10.1016/S0001-4575(03)00084-8. [DOI] [PubMed] [Google Scholar]
- 64.Blows S, Ivers RQ, Connor J, et al. Marijuana use and car crash injury. Addiction. 2005;100(5):605–611. doi: 10.1111/j.1360-0443.2005.01100.x. [DOI] [PubMed] [Google Scholar]
- 65.Woratanarat P, Ingsathit A, Suriyawongpaisal P, et al. Alcohol, illicit and non-illicit psychoactive drug use and road traffic injury in Thailand: a case-control study. Accid Anal Prev. 2009;41(3):651–657. doi: 10.1016/j.aap.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 66.Asbridge M, Poulin C, Donato A. Motor vehicle collision risk and driving under the influence of cannabis: evidence from adolescents in Atlantic Canada. Accid Anal Prev. 2005;37(6):1025–1034. doi: 10.1016/j.aap.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 67.Mura P, Kintz P, Ludes B, et al. Comparison of the prevalence of alcohol, cannabis and other drugs between 900 injured drivers and 900 control subjects: results of a French collaborative study. Forensic Sci Int. 2003;133(1-2):79–85. doi: 10.1016/s0379-0738(03)00052-5. [DOI] [PubMed] [Google Scholar]
- 68.Brault M, Dussault C, Bouchard J, et al. The contribution of alcohol and other drugs among fatally injured drivers in Quebec: final results [abstract] Paper presented at the 17th International Conference on Alcohol, Drugs and Traffic Safety, Glasgow, United Kingdom, August 8–13, 2004. ( www.saaq.gouv.qc.ca/publications/dossiers_etudes/drogue_an.pdf). (Accessed January 14, 2011) [Google Scholar]
- 69.Gerberich SG, Sidney S, Braun BL, et al. Marijuana use and injury events resulting in hospitalization. Ann Epidemiol. 2003;13(4):230–237. doi: 10.1016/s1047-2797(02)00411-8. [DOI] [PubMed] [Google Scholar]
- 70.Fergusson DM, Horwood LJ. Cannabis use and traffic accidents in a birth cohort of young adults. Accid Anal Prev. 2001;33(6):703–711. doi: 10.1016/s0001-4575(00)00082-8. [DOI] [PubMed] [Google Scholar]
- 71.Alcohol and other drug use among victims of motor-vehicle crashes—West Virginia, 2004–2005. MMWR Morb Mortal Wkly Rep. 2006;55(48):1293–1296. [PubMed] [Google Scholar]
- 72.Lacey JH, Kelley-Baker T, Furr-Holden D, et al. 2007 National Roadside Survey of Alcohol and Drug Use by Drivers: Drug Results. Washington, DC: National Highway Traffic Safety Administration; 2009. (DOT HS 811 249) [Google Scholar]
- 73.Walsh JM, Flegel R, Atkins R, et al. Drug and alcohol use among drivers admitted to a level-1 trauma center. Accid Anal Prev. 2005;37(5):894–901. doi: 10.1016/j.aap.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 74.O’Malley PM, Johnston LD. Drugs and driving by American high school seniors, 2001–2006. J Stud Alcohol Drugs. 2007;68(6):834–842. doi: 10.15288/jsad.2007.68.834. [DOI] [PubMed] [Google Scholar]
- 75.Williams AF, Peat MA, Crouch DJ, et al. Drugs in fatally injured young male drivers. Public Health Rep. 1985;100(1):19–25. [PMC free article] [PubMed] [Google Scholar]
- 76.Robbe H. Marijuana’s impairing effects on driving are moderate when taken alone but severe when combined with alcohol. Hum Psychopharmacol. 1998;13:S70–S78. [Google Scholar]
- 77.Watson SJ, Benson JA, Jr, Joy JE. Marijuana and medicine: assessing the science base: a summary of the 1999 Institute of Medicine report. Arch Gen Psychiatry. 2000;57(6):547–552. doi: 10.1001/archpsyc.57.6.547. [DOI] [PubMed] [Google Scholar]
- 78.Aggarwal SK, Carter GT, Sullivan MD, et al. Medicinal use of cannabis in the United States: historical perspectives, current trends, and future directions. J Opioid Manag. 2009;5(3):153–168. doi: 10.5055/jom.2009.0016. [DOI] [PubMed] [Google Scholar]