Abstract
The enantiomer pair androsterone and ent-androsterone are positive allosteric modulators of γ-aminobutyric acid type A (GABAA) receptors. Each enantiomer was shown to bind at the same receptor site. Binding orientations of the enantiomers at this site were deduced using enantiomer pairs containing OBn substituents at either C-7 or C-11. 11β-OBn substituted steroids and 7α-OBn substituted ent-steroids potently displace [35S]TBPS, augment GABA currents and anesthetize tadpoles. In contrast, 7β-OBn substituted steroids and 11α-OBn substituted ent-steroids have diminished actions. The results suggest that the binding orientations of the active analogues are inverted relative to each other with the 7α and 11β substituents similarly located on the edges of the molecules not in contact with the receptor surface. Analogue potentiation of GABA current was abrogated by an α1 subunit Q241L mutation indicating that the active analogues act at the same sites in α1β2γ2L receptors previously associated with positive neurosteroid modulation.
Introduction
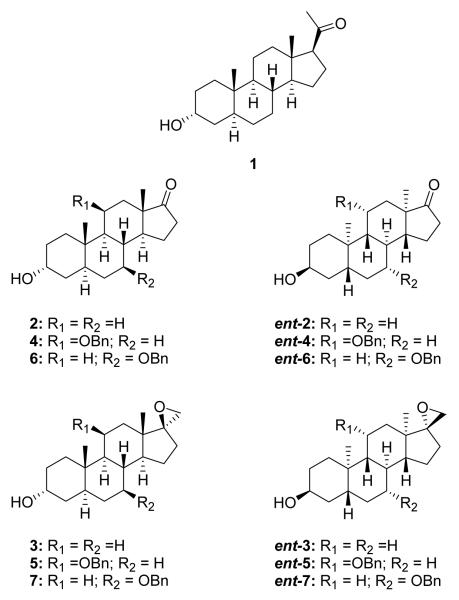
Endogenous steroids like allopregnanolone (1) and androsterone (2) as well as other endogenous 3α-hydroxysteroids and synthetic analogues potentiate GABA-mediated chloride currents at GABAA receptors (Chart 1).1-4 One consequence of potentiation of GABAA receptor function is an increase in neuronal inhibition in the brain. Consequently, steroids having this action are of interest as anxiolytic, anticonvulsant, sedative/hypnotic and anesthetic agents.5,6 Site-directed mutagenesis experiments have shown that the binding sites for this type of steroid modulation are located in the transmembrane domains of the α1 subunits of the pentameric α1β2γ2 subtype of the mouse and rat receptor.7,8 Similarly located sites exist on other forms of the α subunits.9
Chart 1.
Because of the lack of GABAA protein crystal structure data, the molecular details of steroid binding to the receptor have not been established. Nevertheless, numerous analogue studies have established some general features of the structure-activity relationships (SAR) for steroid potentiation.1,10,11 For example, highly active steroids nearly always contain a 3α-hydroxyl group on the steroid A-ring and, for the most active compounds, a 17β-hydrogen bond acceptor group on the steroid D-ring. Only a few ent-steroids have been evaluated for their effects at GABAA receptors and much remains to be learned about their SAR at this class of receptors.12-14
In this study, we investigate SAR related to the enantioselectivity observed for steroid modulation of GABAA receptors by naturally occurring steroid 2 and its unnatural enantiomer ent-2. Both of these steroids have been shown previously to potentiate GABAA receptors.14 Unexpectedly, the activity of the unnatural enantiomer is greater than that of the natural enantiomer. This same activity relationship (unnatural > natural) is also true for the more potent spiroepoxide analogues 3 and ent-3.14
The first goal of this study was to establish that potentiators like steroids 2 and 3 and their enantiomers ent-2 and ent-3, respectively, exerted their effects at the same potentiation site previously identified on the α1 subunits (one site on each of the two α1 subunits) in the pentameric α1β2γ2L GABAA receptor. The second goal was to gain a better understanding of how active natural and enantiomeric steroids are oriented relative to each other at these receptor sites. Our strategy for achieving these two goals was to initially assume, and then later confirm, that there was indeed a common binding site for potentiating steroids and ent-steroids on GABAA receptors. This assumption allowed us to design analogues that would inform us as to how natural and enantiomeric steroids were aligned in a common binding site.
It seemed likely to us that the active steroids and ent-steroids would have the 3α-hydroxy group similarly positioned in the receptor binding sites since this group is critical for high potentiation activity. This is only possible if the active steroids and active ent-steroids are bound upside down relative to each other. Less immediately apparent is one consequence of this relative orientation of a pair of enantiomers. When oriented in this way, the C-6, C-7 edge of the natural steroids and the C-11, C-12 edge of the ent-steroids can be located proximate to each other (see Discussion for alignment model) and a testable prediction can be made about the effect that substituents at C-11 or C-7 will have on the activity of pairs of enantiomeric analogues.
Accordingly, since it is known that a steroid analogue with both an 11β-OBn and an 11α-Me substituent is a strong potentiator at GABAA receptors and steroid analogues with either a 7α- or 7β-Me group are not,15,16 it can be confidently predicted that analogues 4 and 5 will have high activity and analogues 6 and 7 will not. Less confidently predicted, but of more interest, are the activities of the enantiomers of these analogues. If the ent-steroids are bound upside down relative to the natural steroids, then the 11α-substituents in ent-4 and ent-5 will be located proximate to the 7β-substituents in steroids 6 and 7, and ent-4 and ent-5 are predicted to be inactive. Conversely, the 7α-substituents in analogues ent-6 and ent-7 will be located proximate to the 11β-substituents in steroids 4 and 5, and ent-6 and ent-7 are predicted to be active.
Hence, to accomplish our goals, we prepared steroids 4–7 and their enantiomers ent-4–ent-7. We evaluated these agents for their ability to non-competitively displace [35S]-t-butylbicyclophosphorothionate ([35S]TBPS) from the picrotoxin binding site on GABAA receptors, potentiate GABA-mediated chloride currents of rat α1β2γ2L GABAA receptors expressed in Xenopus laevis oocytes, and cause loss of righting reflex (LRR) and loss of swimming reflex (LSR) in tadpoles. We then carried out site-directed mutagenesis studies to determine if analogues that were active in all three bioassays acted at the same sites on the GABAA receptor.
We found that steroids 4 and 5, which have an 11β-benzyloxy group, have high activity whereas their enantiomers ent-4 and ent-5 do not. Conversely, we found that steroids 6 and 7, which have a 7β-benzyloxy group have weak activity whereas their enantiomers ent-6 and ent-7 have high activity. We found the potentiation effects of the active steroids and ent-steroids were either eliminated or greatly reduced when the known potentiation sites on the α1 subunits were rendered ineffective by the Q241L mutation that is known to disrupt steroid actions at rat α1β2γ2L GABAA receptors8.
Chemistry
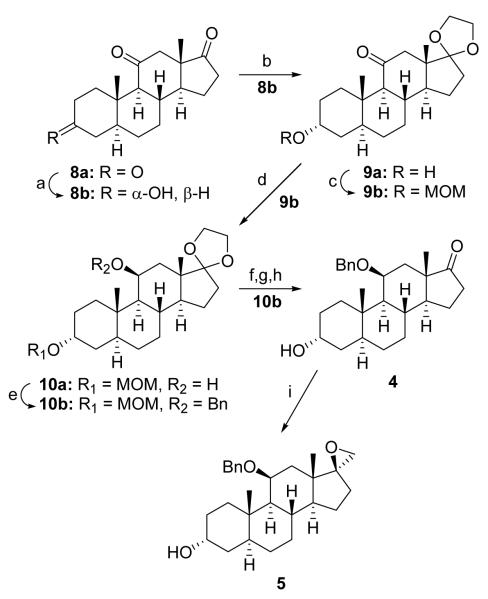
The synthesis of analogues 4 and 5 is summarized in Scheme 1. The starting material was purchased triketone 8a. Regio- and stereoselective reduction of the 3-ketone using K(sec-Bu)3BH yielded after workup predominately the 3α-hydroxysteroid 8b (72%). The 17-ketone was then selectively protected as the cyclic ketal in the standard manner (9a, 70%), and the 3α-OH group was protected with a MOM group (9b, 91%). The 11-ketone is then reduced with LAH to yield the 11β-OH of steroid 10a (80%), and the 11β-OH is alkylated with BnBr to yield steroid 10b (75%). Removal of the MOM protecting group yielded target compound 4 (89%) which contained an impurity that was not easily removed. Acetylation of the 3α-OH group (95%), purification of the acetate derivative by flash column chromatography and removal of the acetyl group (96%) allowed pure steroid 4 to be prepared. Epoxidation of the 17-ketone using (CH3)3SI, KOtBu in DMF gave, the 17-spiroepoxide 5 (61%). This epoxidation is highly stereoselective with a minor amount (ca. 5%) of the epimeric epoxide being removed by a combination of flash column chromatography and recrystallization. The stereochemistry at all new chiral centers formed in this Scheme, and synthetic Schemes 2-4, was assigned based on well-known literature precedents and 1H NMR data.
Scheme 1.
aReagents: a) i: K(sec-Bu)3BH, THF, −78 °C, ii: 3 N NaOH, 30% H2O2 (72%); b) PTSA, HO(CH2)2OH, benzene, reflux (70%); c) MOMCl, (i-Pr)2EtN, DMAP, CH2Cl2 (91%); d) LAH, Et2O (80%); e) KH, BnBr, THF, reflux (75%); f) MeOH, 6 N HCl (89%); g) Ac2O, pyridine, DMAP (95%); h) K2CO3, MeOH (96%); i) (CH3)3SI, DMF, KOtBu (61%).
Scheme 2.
aReagents: a) Li, liq. NH3, toluene, THF, −78 °C (81%); b) Jones reagent, acetone (92%); c) i: K(sec-Bu)3BH, THF, −78 °C, ii: 3 N NaOH, 30% H2O2 (65%); d) PPTS, HO(CH2)2OH, benzene, reflux (87%); e) MOMCl, DMAP, (i-Pr)2EtN, CH2Cl2 (97%); f) i: BH .3THF, THF, 0 °C, ii: 3 N NaOH, 30% H2O2 (67%); g) PCC, CH2Cl2 (96%); h) LAH, Et2O (95%); i) KH, THF, BnBr (69%); j) MeOH, 6 N HCl (92%); k) (CH3)3SI, DMF, KOtBu (61%).
Scheme 4.
aReagents: a) PTSA, HO(CH2)2OH, benzene, reflux (83%); b) 70% aqueous t-BuOOH, NaClO2, aqueous ACN, 50 °C (31%); c) 10% Pd/C, H2 (50 psi), EtOAc (76%); d) Raney Ni, H2 (60 psi), i:PrOH (96%); e) KH, THF, BnBr (72%); f) MeOH, 6 N HCl (89%); g) i: K(sec-Bu)3BH, THF, −78 °C, ii: 3 N NaOH, 30% H2O2 (73%); h) (CH3)3SI, DMF, KOtBu (68%).
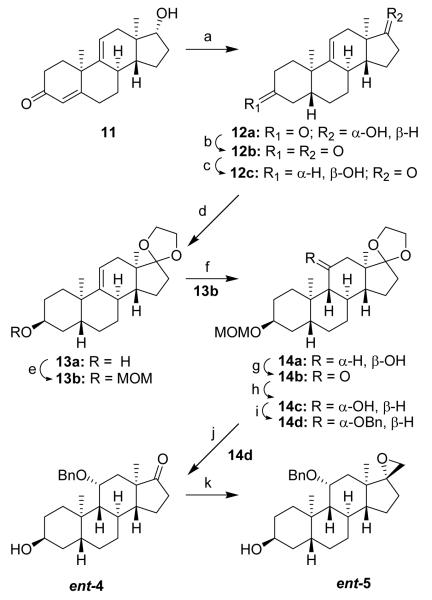
The preparation of analogues ent-4 and ent-5 is presented in Scheme 2. The starting material, ent-steroid 11, was prepared by our previously described method.17 Li/liq. NH3 reduction of the Δ4-3-ketone group yielded the trans A,B ring fused product 12a (81%). Jones oxidation of ent-steroid 12a gave the diketone 12b (92%). The 3-ketone was then reduced with K(sec-Bu)3BH to the 3β-OH group of ent-steriod 12c (97%). The 17-ketone was next protected as the cyclic ketal to yield product 13a (87%), and the 3β-OH group was protected with a MOM group (13b, 97%). The Δ9(11) double bond was then removed by hydroboration to give ent-steroid 14a (67%) which contained the 9β-H and 11β-OH group. The stereochemistry of the 11-OH group was changed from the β configuration to the desired α configuration by a two step procedure-PCC oxidation (14b, 96%), followed by LAH reduction (14c, 95%). Benzylation of the 11α-OH group gave ent-steroid 14d (69%), and removal of the MOM protecting group gave required analogue ent-4 (92%). The minor impurity that complicated purification of steroid 4 was not present in enantiomer ent-4 making purification of the enantiomer possible without conversion to its 3β-acetate derivative. Epoxidation of 17-ketone ent-4 using (CH3)3SI, KOtBu in DMF gave, the 17-spiroepoxide ent-5 (61%).
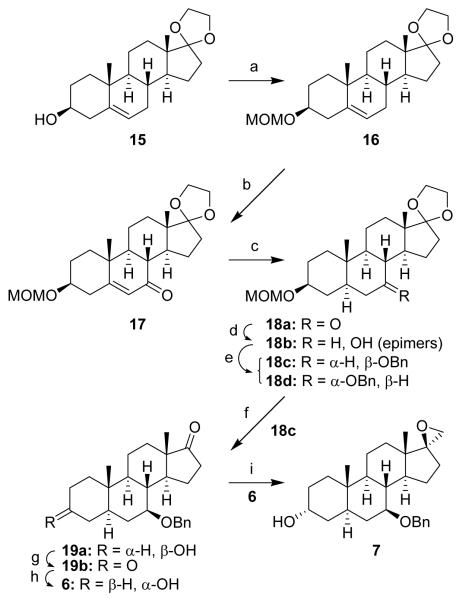
The synthesis of analogues 6 and 7 is shown in Scheme 3. Dehydroepiandrosterone was purchased, converted in the usual manner to its cyclic ketal derivative 15, and used as the starting material. The 3β-OH group was protected with a MOM group to yield steroid 16 (91%). Allylic oxidation of the Δ5 double bond using NaClO2 and aqueous t-BuOOH gave the Δ5-6-ketone 17 in adequate, but not high, yield (34%). Catalytic hydrogenation of steroid 17 using using Pd/C gave product 18a in high yield (80%). LAH reduction of the C-7 ketone group gave an inseparable mixture of epimeric 7α and 7β-alcohols 18b (86%). The decision was made to benzylate the 7-OH groups (68%) to determine if the benzylated epimers were separable. This turned out to be the case and the desired 7β-OBn epimer 18c, which was formed by benzylation of the minor LAH reduction product, was obtained after flash column chromatography in 23% yield. The undesired 7α-OBn epimer 18d was obtained in 45% yield. Removal of the MOM protecting group from steroid 18c gave product 19a (91%), PCC oxidation of steroid 19a gave steroid 19b (86%), and K(sec-Bu)3BH reduction of the 3-ketone group of steroid 19b gave target compound 6 (67%). Epoxidation of the 17-ketone using (CH3)3SI, KOtBu in DMF gave, the 17-spiroepoxide 7 (61%). As observed for the epoxidation of the compounds described in Schemes 1 and 2, this epoxidation was also highly stereoselective and yielded almost exclusively the desired spiroepoxide product.
Scheme 3.
a Reagents: a) MOMCl, DMAP, (i-Pr)2EtN, CH2Cl2 (91%); b) 70% aqueous t-BuOOH, NaClO2, aqueous ACN, 50 °C (34%); c) 10% Pd/C; EtOAc (80%); d) LAH, Et2O (86%); e) KH, THF, BnBr (68%); f) MeOH, 6 N HCl (91%); g) PCC, CH2Cl2 (86%); h) i: K(sec-Bu)3BH, THF, −78 °C, ii: 3 N NaOH, 30% H2O2 (67%); i) (CH3)3SI, DMF, KOtBu (57%).
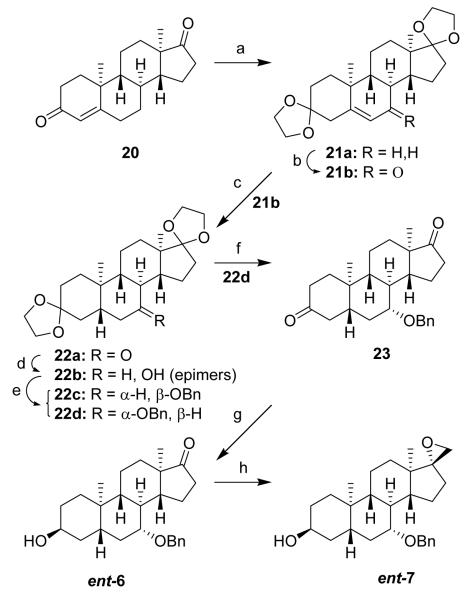
The preparation of analogues ent-6 and ent-7 is demonstrated in Scheme 4. The starting material was ent-androstenedione (20) which was prepared as we described earlier.18 This ent-steroid was first converted into its Δ5-3,17-bis cyclic ketal 21a in the usual manner (83%) and subjected to allylic oxidation, in the manner described earlier for the preparation of steroid 17, to obtain ent-steroid 21b (31%). Catalytic hydrogenation of enone 21b gave the 7-ketone product 22a (76%). Because the LAH reduction of the 7-ketone group of steroid 18a described in Scheme 3 gave, after benzylation, the undesired 7α-OBn product 18b as the major product, a different method was used for the reduction of the 7-ketone in ent-steroid 22a in an attempt to increase the amount of the desired epimer. Raney Ni reduction19 of the 7-ketone in ent-steroid 22a gave product 22b (96%) as an inseparable mixture of 7α- and 7β-alcohols, and benzylation (72%) gave the readily separated 7β-OBn product 22c (22%) and 7α-OBn product 22d (50%). Presumably, steroid approach to the surface of the Raney Ni from the ent-steroid β face (i.e., opposite to the C-19 Me group on the α face) explains why the desired 7α-OH product was the major epimer formed in the Raney Ni reduction. For natural steroids, this means that the major alcohol product of Raney Ni reduction of a 7-ketone group would be the 7β-alcohol. Removal of the 3,17-bis cyclic ketal groups from ent-steroid 22d gave product 23 (89%), K(sec-Bu)3BH reduction of ent-steroid 23 gave target compound ent-6 (73%), and epoxidation of product ent-6 gave target compound ent-7 (68%).
[35S]-t-Butylbicyclophosphorothionate ([35S]TBPS) Displacement Results
The enantiomer pairs shown in Chart 1 were evaluated as noncompetitive displacers of [35S]TBPS from the picrotoxin binding site on the heterogeneous GABAA receptors found in rat brain membranes. The IC50 displacement values are given in Table 1. The values reported for the reference compounds 2, ent-2 and 3, ent-3 are our previously reported values.14 Relative to steroid 2, the reported IC50 values indicate that the axial 11β-OBn substituent present in steroid 4 slightly increases displacement potency, whereas the equatorial 7β-OBn substituent present in steroid 6 drastically decreases displacement potency. Relative to compound ent-2, the 11α-OBn group present in enantiomer ent-4 drastically reduces binding potency and the 7α-OBn substituent present in enantiomer ent-6 increases binding potency.
Table 1. Inhibition of [35S]TBPS Binding by Steroids 1–7 and Steroid Enantiomers ent-2–ent-7a.
| compd | IC50 (nM) | nHill |
|---|---|---|
| 1 b | 74 ± 7 | 0.89 ± 0.06 |
| 2 c | 410 ± 130 | 0.89 ± 0.20 |
| ent-2 c | 311 ± 36 | 1.00 ± 0.10 |
| 3 c | 105 ± 12 | 1.32 ± 0.16 |
| ent-3 c | 467 ± 93 | 4.28 ± 1.90 |
| 4 | 285 ± 37 | 0.90 ± 0.09 |
| ent-4 | >10 μMd | – |
| 5 | 15 ± 2 | 1.1 ± 0.1 |
| ent-5 | 2,050 ± 400 | 2.04 ± 0.7 |
| 6 | >10 μMe | – |
| ent-6 | 168 ± 8 | 1.10 ± 0.05 |
| 7 | 6,750 ± 1,000 | 1.4 ± 0.2 |
| ent-7 | 52 ± 5 | 1.12 ± 0.10 |
Binding results obtained with the 17-spiroepoxide enantiomer pairs 5, ent-5 and 7, ent-7 followed the same pattern observed for the binding results obtained with enantiomer pairs 4, ent-4 and 6, ent-6. Relative to steroid 3, the 11β-OBn substituent present in steroid 5 increases displacement potency, whereas the 7β-OBn substituent present in steroid 7 decreases displacement potency. Relative to analogue ent-3, the 11α-OBn substituent present in analogue ent-5 reduces displacement potency, whereas the 7α-OBn substituent present in analogue ent-7 increases displacement potency. Both compounds 5 and ent-7 are more potent displacers of [35S]TBPS than the endogenous neurosteroid 1.
Electrophysiology Results
Enantiomer pairs were evaluated for their ability to potentiate chloride currents mediated by 2 TM GABA at rat α1β2γ2L GABAA receptors expressed in Xenopus laevis oocytes (Table 2). This GABA concentration gates, on average, ~4% of the maximum response recorded from an oocyte. The maximum achievable potentiation of currents by an analogue varies for different batches of oocytes. Hence, since the different compounds in Table 2 were evaluated on different batches of oocytes, it is not possible to confidently compare the absolute potentiation caused by each analogue shown in Table 2. The low aqueous solubility of these compounds also prevented us from determining the maximal potentiation. Inspection of the concentration effect data in Table 2 suggests that there may be differences in both potency and efficacy for the different compounds. However, the conclusions we draw from the results presented in Table 2 do not require a comparison of absolute potentiation values.
Table 2. Modulation of Rat α1β2γ2L GABAA Receptor Function by Steroids 1–7 and Steroid Enantiomers ent-2–ent-7.
| compd | oocyte electrophysiologya | |||
|---|---|---|---|---|
| 0.1 μM | 1 μM | 10 μM | (gating) 10 μM | |
| 1 b | 1.26 ± 0.14 | 3.89 ± 1.34 | 9.65 ± 3.87 | 0.37 ± 0.07 |
| 2 c | 0.97 ± 0.02 | 1.41 ± 0.01 | 5.44 ± 0.19 | 0.02 ± 0.01 |
| ent-2 c | 1.27 ± 0.29 | 3.66 ± 0.89 | 18.87 ± 2.38 | 0.03 ± 0.21 |
| 3 c | 3.11 ± 0.17 | 21.92 ± 1.30 | 33.73 ± 2.04 | 0.22 ± 0.02 |
| ent-3 c | 2.62 ± 0.29 | 15.89 ± 3.89 | 26.28 ± 7.90 | 0.10 ± 0.02 |
| 4 | 1.08 ± 0.03 | 2.96 ± 0.14 | 24.37 ± 1.47 | 0.20 ± 0.03 |
| ent-4 | 0.89 ± 0.03 | 0.85 ± 0.02 | 0.60 ± 0.01 | 0.00 ± 0.01 |
| 5 | 2.99 ± 0.45 | 21.19 ± 2.59 | 31.15 ± 2.87 | 0.42 ± 0.06 |
| ent-5 | 1.01 ± 0.05 | 1.30 ± 0.09 | 3.21 ± 0.65 | 0.05 ± 0.03 |
| 6 | 0.97 ± 0.02 | 0.90 ± 0.04 | 0.76 ± 0.02 | 0.00 ± 0.02 |
| ent-6 | 1.25 ± 0.03 | 5.74 ± 0.94 | 25.23 ± 7.16 | 0.11 ± 0.02 |
| 7 | 0.83 ± 0.05 | 0.88 ± 0.05 | 0.77 ± 0.20 | 0.09 ± 0.16 |
| ent-7 | 3.47 ± 0.13 | 20.29 ± 2.75 | 32.39 ± 5.42 | 0.22 ± 0.03 |
The GABA concentration used for the control response was 2 μM. Each compound was evaluated on at least four different oocytes at the concentrations indicated, and the results reported are the ratio of currents measured in the presence/absence of added compound. Gating represents direct current gated by 10 μM compound in the absence of GABA, and this current is reported as the ratio of compound-only current/2 μM GABA current. Error limits are calculated as standard error of the mean (N ≥ 4).
Literature values.27
Literature values.14
As reported previously, steroids 2, 3 and their enantiomers ent-2, ent-3, all cause a concentration dependent increase in GABA-gated chloride currents.14 Steroids 4 and 5, which contain 11β-OBn substituents, also cause a concentration dependent increase in chloride currents. Steroids 6 and 7, which contain 7β-OBn substituents, do not. For the analogues ent-4 and ent-5, the 11α-OBn substituents, either do not potentiate chloride currents (ent-4) or only weakly potentiate at the highest concentration, 10 TM (ent-5). Analogues ent-6 and ent-7, which contain 7α-OBn substituents, both cause a concentration dependent increase in GABA-gated chloride currents. The active benzyloxy-substituted compounds (4, 5, ent-6, ent-7) at a concentration of 10 TM also directly gate a chloride current in the absence of GABA, a well known effect of active neurosteroid analogues.
The results reported in Table 2 correlate with the results presented in Table 1. Compounds that potently displace [35S]TBPS also strongly potentiate GABA-mediated chloride currents. Compounds that either weakly displace or do not displace [35S]TBPS at a concentration of 10 TM either weakly potentiate or do not potentiate GABA-mediated chloride currents.
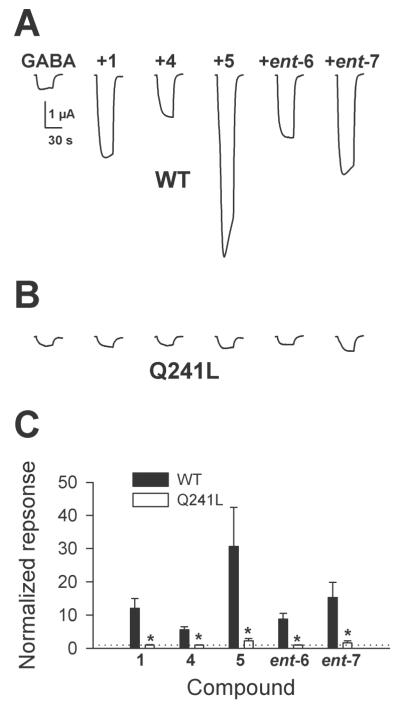
We next addressed the question of whether the steroid and ent-steroid potentiators act at the potentiation site previously identified for neurosteroid 1 by site-directed mutagenesis studies.8 We did this to rule out the possibility that the steroid and ent-steroid potentiators act at different sites on the rat α1β2γ2L GABAA receptor. Accordingly, residue 241 in the α1 subunit was changed from glutamine to leucine. As reported previously20 and shown in Figure 1, this amino acid change eliminates the potentiation caused by neurosteroid 1. It also eliminates or nearly eliminates the potentiation caused by the active analogues prepared in this study. The results support the conclusion that the potentiation caused by all the active compounds is mediated through a common site of action on the GABAA receptor. Figure 1 also provides information on the relative activity of the potentiating compounds. The 17-spiroepoxides 5 (0.5 TM) and ent-7 (0.5 TM) potentiate more than the 17-ketones 4 (1 TM) and ent-6 (1 TM) when compared on the same oocyte. This result is consistent with the greater potency of the 17-spiroepoxides for [35S]TBPS displacement (Table 1).
Figure 1.
Effects of a steroid-insensitive α1(Q241L) subunit on potentiation of GABA currents by analogues. A. Oocytes expressing WT α1β2γ2L GABAA receptor subunits were exposed to GABA alone or GABA co-applied with the indicated analogues at a membrane potentiationtential of −70 mV. Concentrations of compounds were as follows: GABA, 2 TM; compound 1, 0.5 TM; compound 4, 1 TM, compound 5, 0.5 TM, compound ent 6, 1 TM; compound ent 7, 0.5 TM. Concentrations were adjusted to partially account for different potencies observed in initial screening and to thereby yield reasonably similar potentiation values. B. Same sequence of compound presentation in oocytes injected with RNA encoding a point mutation (Q241L) in the α1 subunit that renders receptors insensitive to compound 1.8 WT β2 RNA and γ2L RNA were coinjected. C. Summary of normalized responses of 4 WT oocytes and 4 α1(Q241L)β2γ2L oocytes in experiments like that depicted in A and B. Normalizing response to GABA alone is denoted by a dotted line at y = 1. * p < 0.05 by independent sample t-test.
Tadpole Loss of Righting Reflex (LRR) and Loss of Swimming Reflex (LSR) Results
The anesthetic effects in tadpoles of the compounds are reported in Table 3. The EC50 values for LRR and LSR reported in Table 3 for steroids 2, 3 and their enantiomers ent-2, ent-3 are the values we reported previously.14 Steroids 4 and 5, which contain axial 11β-OBn substituents, are both more potent in causing LRR and LSR in tadpoles than the reference steroids 2 and 3, respectively. The 17-ketosteroid 6 (7β-OBn substituent) does not have an EC50 value of <10 TM for either LRR or LSR. The results correlate with the actions of this analogue in the other two bioassays (Tables 1 and 2). The corresponding 17-spiroepoxide 7 with the 7β-OBn substituent does have weak anesthetic activity as it produces both LRR (EC50, 3.22 TM) and LSR (EC50, 7.94 TM). This result for analogue 7 is consistent with its weak ability to displace [35S]TBPS (Table 1), but not with its failure to potentiate GABA-mediated chloride currents (Table 2).
Table 3. Effects of Steroids 1–7 and Steroid Enantiomers ent-2–ent-7 on Tadpole Righting and Swimming Reflexesa.
| compd | tadpole LRR EC50 (μM) |
tadpole LRR nHill |
Tadpole LSR EC50 (μM) |
Tadpole LSR nHillb |
|---|---|---|---|---|
| 1 c | 0.42 ± 0.04 | −1.83 ± 0.32 | 5.5 ± 0.5 | −7.5 ± 1.1 |
| 2 d | 3.38 ± 0.9 | −2.83 ± 2.66 | Nonee | – |
| ent-2 d | 1.42 ± 0.18 | −2.17 ± 0.48 | 5.48 ± 0.12 | −33.3 ± 0.1 |
| 3 d | 1.35 ± 0.01 | −3.69 ± 0.08 | 2.76 ± 0.01 | −21.1 ± 0.7 |
| ent-3 d | 1.08 ± 0.01 | −18.1 ± 1.3 | 2.71 ± 0.01 | −21.8 ± 1 |
| 4 | 0.20 ± 0.00 | −2.61 ± 0.07 | 0.87 ± 0f | −20.4 ± 0.4 |
| ent-4 | 1.96 ± 0.02 | −3.27 ± 0.07 | 3.45 ± 0g | −21.1 ± 0 |
| 5 | 0.07 ± 0.01 | −1.58 ± 0.21 | 0.27 ± 0h | −21.4 ± 0.5 |
| ent-5 | 2.64 ± 0.01 | −22.8 ± 1.0 | 2.74 ± 0i | −23.2 ± 0 |
| 6 | >10j | – | Nonee | – |
| ent-6 | 1.21 ± 0.4 | −4.27 ± 6.44 | 2.93 ± 0 | −22.0 ± 0.5 |
| 7 | 3.22 ± 0.03 | −15.6 ± 1.8 | 7.94 ± 0k | −27.3 ± 0 |
| ent-7 | 0.31 ± 0.04 | −2.19 ± 0.61 | 0.55 ± 0.01 | −33.3 ± 0.1 |
Error limits are calculated as the standard error of the mean (N = 10 or more tadpoles at each of five or more different concentrations (ranging from 0.01 μM to 30 μM). Unless stated otherwise, all tadpoles regained LRR and LSR after overnight recovery.
LSR for compounds with weak activity typically has a very steep concentration–response curve. When nHill values are in the range of −20 to −33 the nHill values reflect the fact that at one concentration nearly all tadpoles had a swimming reflex and at the next highest concentration tested nearly all or all tadpoles did not.
Literature values.27
Literature values.14
“None” indicates that all tadpoles had a swimming response at 10 μM.
Recovery from LRR and/or LSR was partial at concentrations ≥ 1 μM. At 10 μM, 10/10 tadpoles died without recovering overnight from LSR.
At 10 μM, 10/10 tadpoles died without recovering overnight from LSR.
At 10 μM, 5/10 tadpoles died without recovering overnight from LSR.
At 10 μM, 6/10 tadpoles died without recovering overnight from LSR.
Some tadpoles had LRR at 10 μM but the EC50 was above this value.
At 10 μM, 4/10 tadpoles died without recovering overnight from LSR.
The enantiomeric 17-ketosteroid ent-4 (11α-OBn substituent), which neither displaces [35S]TBPS (Table 1) nor potentiates GABA-mediated chloride currents (Table 2) at concentrations up to 10 TM, unexpectedly causes both LRR and LSR at concentrations below 10 TM. The corresponding enantiomeric 17-spiroepoxysteroid ent-5 with the 11α-OBn substituent also causes both LRR and LSR at concentrations below 10 TM. However, this analogue is also weakly active in the other two bioassays (Table 1 and 2), so its ability to cause LRR and LSR in tadpoles is not surprising.
The enantiomeric analogues ent-6 and ent-7 (7α-OBn substituents) both cause, as expected, LRR and LSR in tadpoles. The enantiomeric 17-ketoanalogue ent-6 is less potent than the enantiomeric 17-spiroepoxide analogue ent-7. This order of potency for their anesthetic effects correlates with their order of potency for [35S]TBPS displacement (Table 1) and electrophysiological actions at GABAA receptors (Figure 1).
Discussion
The prior observation that steroids 2, 3 and their enantiomers ent-2, ent-3 all potentiated GABA-mediated chloride currents at GABAA receptors raised two interesting questions. Are the pairs of enantiomers (steroid and corresponding ent-steroid) acting at the same sites on the GABAA receptor? How are the pairs of enantiomers aligned relative to each other if they act at the same sites on the receptors? The goal of this study was to provide answers to these two questions.
An analogue approach, used in conjunction with site-directed mutagenesis methodology, was chosen to address both questions. The analogues chosen were designed based on an initial assumption that all enantiomer pairs acted at a common site on the receptor and on previous steroid SAR results. It was shown previously that modifying neurosteroid 1 by introducing an 11α-Me substituent together with an 11β-OBn substituent gave an analogue with increased potentiation activity.15 Hence, we expected that new steroid analogues having 11β-OBn substituents (4, 5) would have activity. Since it was also shown previously that adding a group as small as either a 7α- or 7β-Me group to neurosteroid 1 produced an analogue with greatly diminished activity,16 we also expected that new steroid analogues having 7β-OBn substituents (6, 7) would have little, if any, activity.
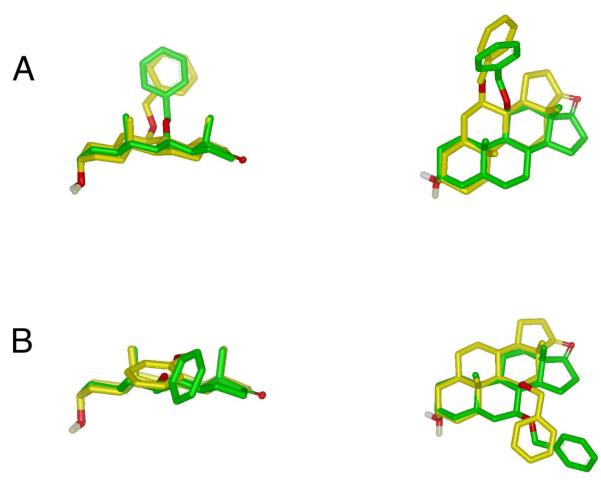
Expected activity outcomes for the enantiomeric compounds, ent-4–ent-7, depend on the choice made to align each steroid with its corresponding enantiomer. We made this alignment choice based on the assumption that the critical 3-OH groups will be similarly positioned in three-dimensional space if enantiomer pairs are bound to the same GABAA receptor binding sites. To satisfy this assumption, active ent-steroids must be oriented upside down relative to active steroids. When so oriented, an 11β-OBn substituent in a natural steroid and a 7α-OBn substituent in an ent-steroid can occupy similar regions of three-dimensional space (Figure 2, panel A). Hence, we expected that new ent-steroids having 7α-OBn substituents (ent-6, ent-7) would, like the 11β-OBn steroids 4 and 5, have potentiation activity. Similarly, since a 7β-OBn substituent in a natural steroid and an 11α-OBn substituent in an upside down oriented ent-steroid can occupy similar regions of three-dimensional space (Figure 2, panel B), we expected that new ent-steroid analogues having 11α-OBn substituents (ent-4, ent-5) would, like the 7β-OBn steroids 6 and 7, have greatly diminished potentiation activity.
Figure 2.
(A) Molecular superimpositions of active compounds 4 (green) and ent-6 (yellow) and (B) inactive compounds 6 (green) and ent-4 (yellow). In both panels a low energy conformation of the analogue with the absolute configuration of natural steroids was used as the template and is shown in green and the best result from fitting a library of conformers of the analogues with the absolute configuration opposite to that of natural steroids (ent-steroids) is shown in yellow. The alignments maximize the overlap of the molecular volumes as well as structural features such as hydrogen bond donors and acceptors. Edge views are shown on the left and views from above the molecules are shown on the right. Hydrogens other than that of the hydroxyl group are removed for clarity. Alignments were made using the software program ROCS (OpenEye Scientific Software).
Other factors also influenced our choice of analogues chosen for this study. Firstly, since the enantiomer of neurosteroid 1 is essentially inactive,12 these studies could not have been done with analogues of neurosteroid 1 containing benzyloxy groups at C-7 or C-11 since no active enantiomers of neurosteroid 1 bearing benzyloxy groups at either position would be possible. Secondly, 11β substituents in the steroids have the axial configuration whereas the 7α subsituents in the ent-steroids have the equatorial configuration. Thus, a relatively large and flexible group like the benzyloxy group was considered advantageous for maximizing possible overlap of substituents having different configurations at the C-7 and C-11 positions. Thirdly, we considered it important to have the C-11 and C-7 substituents be identical to avoid significant differences in logP for the analogues used in the study. LogP can have a major effect on observed [35S]TBPS displacement and potentiation activity because the amount of steroid that accumulates in the cell membrane will determine its effective concentration at the transmembrane steroid binding sites located on the GABAA receptor.21, 22
As shown by the [35S]TBPS displacement results (Table 1) and electrophysiology results (Table 2), our expected outcomes were observed in these two bioassays. Two unexpected outcomes were found in the tadpole behavioral bioassay (Table 3). The analogues ent-4 and 7 both caused LRR and LSR at concentrations below 10 TM even though the compounds neither effectively displace [35S]TBPS nor potentiate GABA-mediated chloride currents. We suggest that the anomalous behavioral effects of these two compounds result from actions on receptors other than GABAA receptors.
The site-directed mutagenesis study (Figure 1) provides evidence that the two active steroids (4, 5) and the two active ent-steroids (ent-6, ent-7) are acting at the same GABAA receptor binding sites. The Q241L mutation abolishes, completely or nearly completely, the activity of all four active compounds at concentrations of either 0.5 TM (the 17-spiroepoxides) or 1 TM (the 17-ketones). The GABAA receptor sites of action were not determined for the analogues ent-4, ent-5, 6 and 7. These analogues neither strongly displace [35S]TBPS nor strongly potentiate GABA-mediated currents. It is interesting to note that compounds ent-4, 6 and 7 appear to weakly inhibit GABA-mediated currents. We have observed previously that 3β-hydroxysteroids can show a use-dependent block of GABAA receptors that is removed by a V256S mutation of the α1 subunit.23 Future studies will be required to determine whether the effects of ent-4, 6 and 7 can be explained by this mechanism which is independent of potentiation.
This enantioselectivity study examined only 5α-reduced analogues. An earlier study examined the effect of a Q241 mutation in the α1 subunit on the actions of a 5β-reduced steroid potentiator and its active enantiomer.24 It was reported that mutation of the Q241 residue eliminated the actions of the 5β-reduced steroid and reduced the actions of its enantiomer, consistent with the present results. Because weak potentiation remained in the previous study and was statistically significant for analogue ent-6 in the present study, the possibility of additional binding sites cannot be excluded.
The modeling results in Figure 2 were obtained with the program ROCS which maximizes the volume overlap between a query molecule (low energy conformers of compounds 4 and ent-6) and a library of other molecules or conformers while also maximizing the overlap of selected chemical features such as ring centroids and hydrogen bond donors and acceptors.25 The alignments should not be interpreted to imply the precise arrangements shown, as the modeling is only intended to demonstrate that when steroids and ent-steroids are oriented as shown in Figure 2, the substituents that adversely affect activity are located along one edge of the aligned molecules, and those that do not adversely affect activity are located on the opposite edge of the aligned molecules. Data are currently insufficient to interpret the alignments in a more precise manner.
Conclusion
Based on studies of newly prepared enantiomeric pairs of steroid analogues, we conclude that androsterone and ent-androsterone bind at the same sites on GABAA receptors. We further conclude that ent-androsterone is bound in an upside down orientation relative to androsterone at these sites. We also provide the first information describing the effects of C-7 or C-11 substituents on the GABAergic effects of ent-steroids. The results obtained will be useful for the design of new potentiators of GABAA receptors with a structure based on that of an ent-steroid.
General Methods
Solvents were either used as purchased or dried and purified by standard methodology. Extraction solvents were dried with anhydrous Na2SO4 and after filtration, removed on a rotary evaporator. Flash column chromatography was performed using silica gel (32–63 μm) purchased from Scientific Adsorbents (Atlanta, GA). Melting points were determined on a Kofler micro hot stage and are uncorrected. FT-IR spectra were recorded as films on a NaCl plate. NMR spectra were recorded in CDCl3 at ambient temperature at 300 MHz (1H) or 74 MHz (13C). Purity of > 95% was determined for all evaluated compounds by combustion analysis for C,H performed by M-H-W Laboratories (Phoenix, AZ). Steroids 8a and dehydroepiandrosterone were purchased from Steraloids (Newport, RI). K(sec-Bu)3BH (K-Selectride ®) was purchased from Aldrich Chemical Co. (Milwaukee, WI).
(3α,5α,11β)-11-Benzyloxy-3-hydroxyandrostan-17-one (4)
A mixture of steroid 10b (242 mg, 0.5 mmol), MeOH (15 mL) and 6 N HCl (3mL) was stirred at room temperature for 36 h. The MeOH was removed under reduced pressure and the residual solution was extracted with EtOAc, dried and concentrated to give a viscous liquid which was purified by flash column chromatography (silica gel eluted with 30–40% EtOAc in hexanes) to give crude product 4 (176 mg, 89%). This crude product was acetylated (95% yield) in the standard manner (Ac2O, pyridine, DMAP, room temperature) and purified by column chromatography to give the pure acetate derivative: mp 117-119 °C; IR νmax 2927, 2856, 1736, 1452, 1359, 1260, 1244 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 5.00 (m, 1H), 4.65 (d, 1H, J = 11.3 Hz), 4.26 (d, 1H, J =11.3 Hz), 4.01 (m, 1H), 2.55–2.35 (m, 2H), 2.04 (s, 3H), 1.08 (s, 3H), 1.01 (s, 3H); 13C NMR δ 219.9, 170.5, 138.4, 128.1 (2 × C), 127.7(2 × C), 127.2, 74.6, 70.2, 69.8, 58.6, 53.2, 47.1, 40.8, 36.1, 35.3, 32.8, 32.7, 32.3, 31.3 (2 × C), 27.5, 25.7, 21.5, 21.4, 14.9, 14.3.
The acetate derivative was then hydrolyzed using K2CO3/MeOH to give product 4 (152 mg, 96% yield): mp 62–65 °C; [α]20D +82.9 (c 0.1, CHCl3); IR νmax 3436, 2922, 1738, 1452, 1354 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.65 (d, 1H, J = 11.3 Hz), 4.26 (d, 1H, J = 11.3 Hz), 4.03 (b s, 1H), 4.02 (b s, 1H), 2.51-2.37 (m, 2H), 1.07 (s, 3H), 0.99 (s, 3H); 13C NMR δ 220.1, 138.5, 128.1 (2 × C), 127.6 (2 × C), 127.1, 74.7, 70.2, 66.2, 58.7, 53.2, 47.2, 39.9, 36.3, 35.3, 35.3, 32.9, 32.0, 31.5, 31.3, 28.6, 27.6, 21.5, 15.0, 14.2. Anal. (C26H36O3) C, H.
(3β,5β,8α,9β,10α,11α,13α,14β)-11-Benzyloxy-3-hydroxyandrostan-17-one (ent-4)
A mixture of steroid 14d (121 mg, 0.25 mmol), MeOH (15 mL) and 6 N HCl (3mL) was stirred at room temperature for 36 h. The MeOH was removed under reduced pressure and the residual solution was extracted with EtOAc, dried and concentrated to give an oily liquid which was purified by flash column chromatography (silica gel eluted with 30-40% EtOAc in hexanes) to give product ent-4 (92 mg, 92%): mp 62–64 °C; [α]20D −84.6 (c 0.08, CHCl3); IR νmax 3401, 2921, 1738, 1452, 1354 cm−1; 1H NMR: 7.40–7.20 (m, 5H), 4.66 (d, 1H, J = 11.2 Hz), 4.27 (d, 1H, J = 11.2 Hz), 4.04 (b s, 1H), 4.03 (b s, 1H), 2.54–2.37 (m, 2H), 1.08 (s, 3H), 1.01 (s, 3H); 13C NMR: 220.1, 138.5, 128.1 (2 × C), 127.6 (2 × C), 127.1, 74.7, 70.2, 66.1, 58.7, 53.2, 47.1, 39.9, 36.3, 35.3, 35.2, 32.8, 32.0, 31.4, 31.3, 28.6, 27.6, 21.5, 14.9, 14.2. Anal. (C26H36O3) C, H.
(3α,5α,11β,17β)-Spiro[11-benzyloxyandrostane-17,2′-oxiran]-3-ol (5)
Trimethylsulfonium iodide (40.5 mg, 0.2 mmol) followed by KtOBu (16.5 mg, 0.15 mmol) was added to steroid 4 dissolved in DMF (4 mL) and the mixture was stirred at room temperature for 2.5 h. Brine was added and the product was extracted into EtOAc (20 mL × 3). The combined extracts were dried, and concentrated to give a viscous liquid which was purified by flash column chromatography (silica gel eluted with 30–40% EtOAc in hexanes) to give product 5 (25 mg, 61%): mp 144-146 °C; [α]20D +49.6 (c 0.05, CHCl3); IR νmax 3400, 2921, 2854, 1587, 1455, 1355 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.60 (d, 1H, J = 11 Hz), 4.17 (d, 1H, J = 11 Hz), 4.02 (b s, 1H), 3.96 (m, 1H), 2.90 (d, 1H, J = 4.9 Hz), 2.60 (d, 1H, J = 4.9 Hz), 1.11 (s, 3H), 0.98 (s, 3H); 13C NMR δ 138.8, 128.1 (2 × C), 127.7 (2 × C), 127.1, 74.6, 71.1, 70.2, 66.4, 58.5, 54.7, 53.7, 40.1, 39.5, 36.3, 35.4, 35.1, 32.19, 32.09, 32.03, 28.8, 28.7, 27.8, 23.4, 15.7, 14.2. Anal. (C27H38O3) C, H.
(3β,5β,8α,9β,10α,11α,13α,14β,17α)-Spiro[11-benzyloxyandrostane-17,2′-oxiran]-3-ol (ent-5)
Compound ent-4 (40 mg, 0.10 mmol) was converted into steroid ent-5 using the procedure reported for the preparation of steroid 5. Flash column chromatography (silica gel eluted with 20–35% EtOAc in hexanes) gave product ent-5 (25 mg, 61%): mp 143–146 °C; [α]20D −44.5 (c 0.05, CHCl3); IR νmax 3369, 2921, 2853, 1595, 1454, 1357 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.61 (d, 1H, J = 11.3 Hz), 4.18 (d, 1H, J = 11.3Hz), 4.03 (s, 1H) 3.97 (m, 1H), 2.91 (d, 1H, J = 5.0 Hz), 2.61 (d, 1H, J = 5.0 Hz), 1.11 (s, 3H), 0.98 (s, 3H); 13C NMR: 138.8, 128.1 (2 × C), 127.7 (2 × C), 127.1, 74.6, 71.1, 70.2, 66.5, 58.5, 54.7, 53.7, 40.1, 39.5, 36.3, 35.4, 35.1, 32.1, 32.0, 32.0, 28.8, 28.7, 27.8, 23.4, 15.7, 14.2. Anal. (C27H38O3) C, H.
(3α,5α,7β)-7-Benzyloxy-3-hydroxyandrostan-17-one (6)
Steroid 19b (59 mg, 0.15 mmol) was dissolved in THF (5 mL), cooled to −78 °C and a 1M solution of K-Selectride ® in THF (0.15 mL) was added. The reaction was stirred at −78 °C for 1.5 h and quenched by adding a few drops of water. Then 3 N aqueous NaOH (5 mL) followed by 30% H2O2 (5 mL) were added and stirring was continued at room temperature for 1.5 h. The product was extracted with Et2O (2 × 30 mL) followed by EtOAc (2 × 40 mL). The combined extracts were washed with brine, dried, and concentrated to give an off-white solid which was purified by flash column chromatography (silica gel eluted with 20-40% EtOAc in hexanes) to give product 6 (40 mg, 67%): mp 130-132 °C; [α]20D = +131.5 (c 0.04, CHCl3); IR νmax 3400, 2928, 2858, 1736, 1453, 1361 cm−1; 1H NMR δ 7.40-7.22 (m, 5H), 4.62 (d, 1H, J = 11 Hz), 4.38 (d, 1H, J = 11 Hz), 4.08 (b s, 1H), 3.26 (m, 1H), 0.88 (s, 3H), 0.83 (s, 3H); 13C NMR δ 221.7, 138.6, 128.4 (2 × C), 127.8 (2 × C), 127.5, 82.0, 70.2, 66.2, 53.2, 51.4, 48.4, 41.0, 36.1, 36.0, 35.7 (2 × C), 33.5, 32.2, 31.6, 29.1, 25.0, 20.3, 14.2, 11.3. Anal. (C27H36O3) C, H.
(3β,5β,7α,8α,9β,10α,13α,14β)-7-Benzyloxy-3-hydroxyandrostan-17-one (ent-6)
Compound 23 (105 mg, 0.27 mmol) was converted into compound ent-6 using the procedure reported for the preparation of steroid 6. Flash column chromatography (silica gel eluted with 20-40% EtOAc in hexanes) gave product ent-6 (78 mg, 73%): mp 136–138 °C; [α]20D= −135.5 (c 0.07); IR νmax 3401, 2927, 2857, 1736, 1453, 1361 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.62 (d, 1H, J = 11 Hz), 4.38 (d, 1H, J = 11 Hz), 4.08 (b s, 1H), 3.26 (1H, m), 0.88 (s, 3H), 0.83 (s, 3H); 13C NMR δ 221.8, 138.6, 128.4 (2 × C), 127.8 (2 × C), 127.5, 82.0, 70.2, 66.2, 53.2, 51.4, 48.4, 41.0, 36.14, 36.06, 35.7 (2 × C), 35.6, 33.5, 32.1, 31.6, 29.1, 25.0, 20.3, 14.2, 11.3. Anal. (C27H36O3) C, H.
(3α,5α,7β,17β)-Spiro-[7-Benzyloxyandrostane-17,2′-oxiran]-3-ol (7)
Steroid 6 (60 mg, 0.15 mmol) was converted into steroid 7 using the procedure reported for the preparation of steroid 5. Flash column chromatography (silica gel eluted with 20-35% EtOAc in hexanes) gave product 7 (35 mg, 57%): mp 146–148 °C; [α]20D +55.5 (c 0.06, CHCl3); IR νmax 3436, 2927, 2855, 1497, 1454, 1358, 1265 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.58 (d, 1H, J = 11 Hz), 4.37 (d, 1H, J = 11 Hz), 4.07 (b s, 1H), 3.18 (m, 1H), 2.90 (d, 1H, J = 5.2 Hz), 2.59 (d, 1H, J = 5.2 Hz), 0.89 (s, 3H), 0.82 (s, 3H); 13C NMR δ 138.8, 128.3 (2 × C), 127.8 (2 × C), 127.3, 82.4, 70.2, 66.2, 53.7, 53.1, 52.8, 41.5, 40.9, 36.2 (2 × C), 35.7 (2 × C), 34.0, 33.6, 32.2, 29.4, 29.1, 26.6, 20.4, 14.7, 11.3. Anal. (C27H38O3) C, H.
(3β,5β,7α,8α,9β,10α,13α,14β,17α)-Spiro[7-Benzyoxyandrostane-17,2′-oxiran]-3-ol (ent-7)
Compound ent-6 (39 mg, 0.1 mmol) was converted into steroid ent-7 using the procedure reported for the preparation of steroid 5. Flash column chromatography (silica gel eluted with % EtOAc in hexanes) gave product ent–7 (28 mg, 68%): mp 145–148 °C; [α]20D −59.5 (c 0.05, CHCl3); IR νmax 3435, 2926., 2855, 1454, 1358, 1265 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.59 (d, 1H, J = 11 Hz), 4.37 (d, 1H, J = 11Hz), 4.08 (b s, 1H), 3.18 (m, 1H), 2.91 (d, 1H, J = 5 Hz), 2.60 (d, 1H, J = 5 Hz), 0.89 (s, 3H), 0.82 (s, 3H); 13C NMR δ 138.8, 128.3 (2 × C), 127.8 (2 × C), 127.4, 82.4, 70.2, 66.3, 53.7, 53.1, 52.8, 41.5, 40.9, 36.2 (2 × C), 35.7 (2 × C), 34.0, 33.6, 32.2, 29.5, 29.1, 26.6, 20.4, 14.7, 11.3. Anal. (C27H38O3) C, H.
(3α,5α)-3-Hydroxyandrostane-11,17-dione (8b)
Steroid 8a (3.18 g, 10.4 mmol) was converted into compound 8b using the procedure reported for the preparation of steroid 6. After flash column chromatography (silica gel eluted with 20–40% EtOAc in hexanes) product 8b (2.28, 72%) had: mp 146–149 °C; IR νmax 3461, 2923, 1741, 1705, 1454, 1233 cm−1; 1H NMR δ 4.05 (b s, 1H), 1.02 (s, 3H), 0.82 (s, 3H); 13C NMR δ 217.5, 209.0, 66.1, 64.9, 50.6 (2 × C), 50.4, 38.9, 36.1, 36.0, 35.9, 35.2, 31.3, 30.8, 28.8, 27.6, 21.5, 14.6, 11.0. Anal. (C19H28O3) C,H.
(3α,5α)-3-Hydroxyandrostane-11,17-dione, cyclic 17-1,2-ethanediyl acetal (9a)
A mixture of 8b (609 mg, 2 mmol), ethylene glycol (1 mL), PTSA (100 mg) in benzene (100 ml) was heated at reflux using a Dean Stark apparatus for 16 h. The reaction mixture was cooled and basified with aqueous saturated NaHCO3 and extracted with EtOAc (50 mL × 4). The combined extracts were dried and concentrated to give a white solid which was purified by flash column chromatography (silica gel eluted with 20-35% EtOAc in hexanes) as solvent to give product 9a (488 mg, 70%): mp 92–95 °C; IR νmax 3420, 2923, 1704, 1456, 1385, 1313, 1275, 1203 cm−1; 1H NMR δ 4.03 (b s, 1H), 4.00–3.78 (m, 4H), 2.62 (d, 1H, J = 11.5 Hz), 1.00 (s, 3H), 0.79 (s, 3H); 13C NMR δ 211.3, 117.8, 66.2, 65.3, 64.5, 64.3, 50.2, 49.7, 49.5, 39.0, 37.1, 35.7, 35.3, 34.3, 31.9, 30.9, 28.8, 27.8, 22.1, 14.8, 10.9; HRMS (EI) m/z Calcd for C21H32O4: 348.2301. Found: 348.2296.
(3α,5α)-(3-Methyloxymethyloxy)-androstane-11,17-dione, cyclic 17-1,2-ethanediyl acetal (9b)
Steroid 9a (452 mg, 1.3 mmol), chloromethyl methyl ether (0.53 mL, 7 mmol), N,N-diisopropyl ethylamine (1.74 mL, 10 mmol) and a catalytic amount of DMAP (40 mg) dissolved in CH2Cl2 (15 mL) was stirred at room temperature for 16 h. The reaction was poured into an aqueous saturated NaHCO3 solution and extracted with CH2Cl2 (100 mL × 3). The combined extracts were dried and concentrated to give a viscous liquid which was purified by flash column chromatography (silica gel eluted with 20–25% EtOAc in hexanes) to give product 9b (464 mg, 91%) as an oil: IR νmax 2924, 1705, 1455, 1385, 1365, 1314, 1275, 1204 cm−1; 1H NMR δ 4.64 (dd, 2H, J = 8.5, 6.6 Hz), 3.98–3.75 (m, 4H), 3.35 (s, 3H), 2.61 (d, 1H, J = 11.8 Hz), 1.01 (s, 3H), 0.79 (s, 3H); 13C NMR δ 211.0, 117.6, 94.4, 71.3, 65.2, 64.4, 64.2, 54.9, 50.0, 49.5, 49.4, 39.5, 36.9, 35.4, 34.2, 33.1, 31.7, 31.4, 27.7, 25.9, 22.0, 14.7, 11.0. HRMS (FAB) m/z Calcd for C23H36O5Na: 415.2460. Found: 415.2466
(3α,5α,11β)-(3-Methyloxymethyloxy)-11-hydroxyandrostan-17-one, cyclic 17-1,2-ethanediyl acetal (10a)
Steroid 9b (392 mg, 1 mmol) dissolved in dry Et2O was added to an ice cold, stirred suspension of LAH (114 mg, 3 mmol) in Et2O. The reaction was warmed to room temperature and stirring was continued for 2 h. Water (0.5 mL) was added, then a drop of aqueous 5 N NaOH (0.5 mL) was added and the mixture was stirred for 0.5 h. Water (1 mL) was again added and stirring was continued for another 0.5 h. The Et2O was decanted and the remaining solid was washed with Et2O. The combined Et2O solutions were dried and concentrated to give product 10a as a liquid (315 mg, 80%): IR νmax 3503, 2927, 1454, 1279, 1212 cm−1; 1H NMR δ 4.58 (dd, 2H, J = 6.3, 5.5 Hz), 4.31 (b s, 1H), 3.90–3.70 (m, 4H), 3.30 (s, 3H), 1.01 (s, 3H), 0.98 (s, 3H); 13C NMR δ 119.3, 94.4, 71.3, 67.8, 64.9, 64.3, 57.8, 55.0, 51.8, 45.0, 40.4, 39.5, 35.9, 33.9, 32.9, 32.4, 31.5, 31.3, 27.8, 25.9, 22.5, 16.8, 14.3. Anal. (C23H38O5) C, H.
(3α,5α,11β)-11-Benzyloxy-3-(methyloxymethyloxy)-androstan-17-one, cyclic 17-1,2-ethanediyl acetal (10b)
KH (400 mg, 40% in mineral oil, 4 mmol) and then benzyl bromide (0.31 mL, 2.5 mmol) were added to steroid 10a dissolved in THF (10 mL) and the mixture was refluxed for 2 h. The reaction was cooled 0 °C and the excess KH was carefully destroyed by MeOH (5 mL) addition. Water (20 mL) was then added and the product was extracted with EtOAc. The EtOAc was washed with brine, dried and concentrated to give a residue which was purified by flash column chromatography (silica gel eluted with 20–35% EtOAc in hexanes) to give product 10b as a liquid (294 mg, 75%): IR νmax 2926, 1454, 1279, 1210 cm−1; 1H NMR δ 7.40–7.18 (m, 5H), 4.70–4.52 (m, 3H), 4.20 (d, 1H, J = 11.3 Hz), 4.00–3.70 (m, 5H), 3.35 (s, 3H), 1.07 (s, 3H), 0.98 (s, 3H); 13C NMR δ 139.0, 128.0 (2 × C), 127.5 (2 × C), 126.9, 119.4, 94.4, 75.1, 71.5, 70.1, 65.0, 64.3, 58.2, 55.0, 52.1, 45.3, 40.5, 36.0, 33.9, 33.0, 32.6, 31.9, 31.8, 31.6, 27.9, 26.0, 22.5, 15.7, 14.4. HRMS (FAB) m/z Calcd for C30H44O5Na: 507.3086. Found: 507.3083.
(5β,8α,10α,13α,14β,17α)-17-Hydroxyandrost-9(11)-en-3-one (12a)
NH3 (150mL) was condensed into a cold (-78 °C) 2-necked flask (250mL) fitted with a Dewar condenser. Toluene (15 mL) and THF (20 mL) were added. Lithium (294 mg, 42.3 mmol), in small pieces, was added to the solution and stirred for 10 min resulting in the formation of a deep blue colored solution. Compound 1117 (2.4 g, 8.45 mmol) in THF (20 mL) was added and the mixture was stirred at −78 °C for 45 min. Solid ammonium chloride (6 g) was added and the ammonia was allowed to evaporate. Water (200 mL) was added and the reaction mixture was extracted with EtOAc (100 ml × 3). The combined EtOAc extracts were washed with brine, dried and concentrated to give a white solid which was purified by flash column chromatography (silica gel eluted with 20–35% EtOAc in hexanes) to give product 12a (1.97 g, 81%): mp 166-168 °C; IR νmax 3391, 2921, 2869, 1713, 1596, 1445, 1374, 1271 cm−1; 1H NMR δ 5.41 (m, 1H), 3.74 (t, 1H, J = 9.1 Hz), 1.16 (s, 3H), 0.72 (s, 3H); 13C NMR δ 211.6, 146.1, 116.7, 81.9, 48.4, 45.0, 44.6, 41.4, 38.3, 38.1, 37.8, 37.0, 36.9, 32.2, 30.7, 28.7, 24.2, 17.3, 10.5. Anal. (C19H28O2) C, H.
(5β,8α,10α,13α,14β)-Androst-9(11)-ene-3,17-dione (12b)
Compound 12a (1.9 g, 6.6 mmol) was dissolved in acetone (50 mL) and stirred. Jones reagent was added dropwise until the orange color persisted and stirring was continued for 1 h. The excess Jones reagent was quenched by adding few drops of isopropyl alcohol, and the acetone was removed under reduced pressure to give a green liquid. Water was added and the resulting solution was extracted with EtOAc. The EtOAc was dried and removed to give a white solid. Flash column chromatography (silica gel eluted with 20–35% EtOAc in hexanes) yielded product 12b (1.73 g, 92%): mp 147-148 °C; IR νmax 2925, 2852, 1739, 1713, 1595, 1450, 1404, 1370, 1244, 1210 cm−1; 1H NMR δ 5.43 (m, 1H), 1.18 (s, 3H), 0.85 (s, 3H); 13C NMR δ 221.4, 211.1, 146.4, 116.2, 48.8, 45.9, 44.8, 44.6, 38.1, 36.9, 36.2 (3 × C), 33.3, 31.7, 28.5, 22.7, 17.3, 13.8. Anal. (C19H26O2) C, H.
(3β,5β,8α,10α,13α,14β)-3-Hydroxyandrost-9(11)-en-17-one (12c)
Compound 12b (1.69 g, 5.94 mmol) was converted into compound 12c using the procedure reported for the preparation of steroid 6. After flash column chromatography (silica gel eluted with 20–40% EtOAc in hexanes) product 12c (1.1 g, 65%) had: mp 186-188 °C; IR νmax 3401, 2921, 2854, 1738, 1596, 1451, 1370, 1279, 1211 cm−1; 1H NMR δ 5.38 (m, 1H), 4.06 (b s, 1H), 0.94 (s, 3H), 0.82 (s, 3H); 13C NMR δ 222.1, 148.0, 114.7, 66.3, 49.1, 46.0, 38.6, 37.7, 36.3, 36.2, 36.1, 33.3, 32.2, 30.6, 29.1, 28.1, 22.7, 17.0, 13.8. Anal. (C19H28O2) C, H.
(3β,5β,8α,10α,13α,14β)-3-Hydroxyandrost-9(11)-en-17-one, cyclic-17-1,2-ethanediyl acetal (13a)
Compound 12c (1g, 3.49 mmol) was converted into compound 13a using the procedure reported for the preparation of steroid 9a (except that PPTS was used as the catalyst instead of PTSA). Flash column chromatography (silica gel eluted with 20–40% EtOAc in hexanes) gave product 13a (1 g, 87%): mp 138–140 °C; IR νmax 3350, 2968, 2920, 2873, 1595, 1454, 1374, 1308, 1274, 1204 cm−1; 1H NMR δ 5.35 (m, 1H), 4.04 (b s, 1H), 4.00-3.80 (m, 4H), 2.38 (d, 1H, J = 16.5 Hz), 0.92 (s, 3H), 0.78 (s, 3H); 13C NMR δ 147.0, 119.2, 115.4, 66.4, 65.1, 64.5, 48.1, 44.2, 38.4, 37.9, 37.2, 36.2, 34.0, 32.6, 32.2, 30.7, 29.1, 28.3, 23.6, 16.9, 14.1. HRMS (EI) m/z Calcd for C21H32O3: 332.2351. Found: 332.2352.
(3β,5β,8α,10α,13α,14β)-(3-Methyloxymethyloxy)-androst-9(11)-en-17-one, cyclic-17-1,2-ethanediyl acetal (13b)
Compound 13a (1 g, 3 mmol) was converted into compound 13b using the procedure reported for the preparation of steroid 9b. Flash column chromatography (silica gel eluted with 15–25% EtOAc in hexanes) gave product 13b (1.1 g, 97%): mp: 73–75 °C; IR νmax 2968, 2923, 1595, 1454, 1374, 1308, 1275, 1207 cm−1; 1H NMR δ 5.33 (d, 1 H, J = 6.1 Hz), 4.65 (dd, 2H, J = 9.1, 6.9 Hz), 3.96–3.80 (m, 4H), 3.36 (s, 3H), 2.37 (d, 1H, J = 16.2 Hz), 0.93 (s, 3H), 0.79 (s, 3H); 13C NMR δ 147.1, 119.2, 115.3, 94.5, 71.5, 65.1, 64.5, 55.1, 48.1, 44.3, 28.4, 38.2, 37.2, 34.0, 33.9, 32.56, 32.2, 31.4, 28.4, 26.5, 23.6, 17.2, 14.1. Anal. (C23H36O4) C, H.
(3β,5β,8α,9β,10α,11β,13α,14β)-(3-Methyloxymethyloxy)-11-hydroxyandrostan-17-one, cyclic-17-1,2-ethanediyl acetal (14a)
Compound 13b was dissolved in THF (10 mL) and stirred at 0 °C. A 1 M borane–THF complex in THF (3 mL, 3 mmol) was added and the reaction was stirred at room temperature for 8 h. The reaction was cooled to 0 °C and excess borane complex was carefully quenched with a few drops of water. 3 N aqueous NaOH (10 mL) followed by 30% H2O2 (10 mL) were added and the reaction was stirred at room temperature for 16 h. The mixture was extracted with Et2O (3 × 75 mL) followed by EtOAc (2 × 50 mL). The combined extracts were dried and concentrated to give an oil which was purified by flash column chromatography (silica gel eluted with 20–40% EtOAc in hexanes) to give product 14a as a colorless liquid (351 mg, 67%): IR νmax 3435, 2923, 1595, 1457, 1380, 1312, 1282, 1212 cm−1; 1H NMR δ 4.59 (dd, 2H, J = 10.7, 6.6 Hz), 3.93–3.68 (m, 5H), 3.30 (s, 3H), 0.88 (s, 3H), 0.78 (s, 3H); 13C NMR δ 118.7, 94.2, 71.1, 69.2, 65.0, 64.4, 60.4, 54.9, 49.3, 46.2, 42.5, 39.5, 37.6, 34.9, 34.5, 34.1, 34.1, 31.1, 28.9, 26.2, 22.5, 15.0, 11.7. Anal. (C23H38O5) C, H.
(3β,5β,8α,9β,10α,13α,14β)-(3-Methyloxymethyloxy)-androstane-11,17-dione, cyclic-17-1,2-ethanediyl acetal (14b)
Compound 14a (250 mg, 0.63 mmol) was dissolved in stirred CH2Cl2 (8 mL), solid NaOAc (154 mg, 1.89 mmol) and PCC (407.4 mg, 1.89 mmol) were added and the reaction was stirred at room temperature for 3 h. The CH2Cl2 solution was directly purified by flash column chromatography (silica gel eluted with 10–35% EtOAc in hexanes) to give product 14b (237 mg, 96%) as an oil: IR νmax 2924, 1705, 1594, 1456, 1385, 1204 cm−1; 1H NMR δ 4.63 (dd, 2H, J = 8.2, 6.9 Hz), 3.94–3.70 (m, 5H), 3.32 (s, 3H), 2.57 (d, 1H, J = 12 Hz), 0.98 (s, 3H), 0.75 (s, 3H); 13C NMR δ 211.4, 117.7, 94.4, 71.4, 65.2, 64.5, 64.2, 55.0, 50.1, 49.6, 49.5, 39.6, 37.0, 35.5, 34.3, 33.2, 31.8, 31.5, 27.8, 25.9, 22.1, 14.8, 11.1. Anal. (C23H36O5) C, H.
(3β,5β,8α,9β,10α,11α,13α,14β)-(3-Methyloxymethyloxy)-11-hydroxyandrostan-17-one, cyclic-17-1,2-ethanediyl acetal (14c)
Compound 14b (208 mg, 0.53 mmol) was converted into compound 14c using the procedure reported for the preparation of steroid 10a. The reaction time was 3 h. Flash column chromatography (silica gel eluted with 35% EtOAc in hexanes) gave product 14c (199 mg, 95%) as an oil: IR νmax 3504, 2925, 1455, 1279, 1212 cm−1; 1H NMR δ 4.58 (dd, 2H, J = 8.0, 6.6 Hz), 4.31 (b s), 3.90–3.70 (m, 4H), 3.29 (s, 3H), 1.01 (s, 3H), 0.96 (s, 3H); 13C NMR δ 119.4, 94.4, 71.3, 67.9, 65.0, 64.4, 57.8, 55.0, 51.8, 45.1, 40.4, 39.6, 35.9, 33.9, 32.9, 32.4, 31.6, 31.3, 27.8, 25.9, 22.6, 16.8, 14.3. HRMS (FAB) m/z Calcd for C23H38O5Na: 417.2617. Found: 417.2617.
(3β,5β,8α,9β,10α,11α,13α,14β)-11-Benzyloxy-(3-Methyloxymethyloxy)-androstan-17-one, cyclic-17-1,2-ethanediyl acetal (14d)
Compound 14c (200 mg, 0.51 mmol) was converted into compound 14d using the procedure reported for the preparation of steroid 10b. Flash column chromatography (silica gel eluted with 20–35% EtOAc in hexanes) gave product 14d (170 mg, 69 %) as an oil: IR νmax 2924, 1454, 1278 cm−1; 1H NMR δ 7.40–7.18 (m, 5H), 4.70–4.52 (m, 3H), 4.20 (d, 1H, J = 11.2 Hz), 4.02–3.69 (m, 5H), 3.36 (s, 3H), 1.06 (s, 3H), 0.98 (s, 3H); 13C NMR δ 139.0, 128.0 (2 × C), 127.6 (2 × C), 127.0, 119.5, 94.5, 75.2, 71.5, 70.1, 65.1, 64.4, 58.2, 55.1, 52.1, 45.3, 40.6, 36.0, 34.0, 33.1, 32.7, 31.9, 31.9, 31.7, 27.9, 26.0, 22.6, 15.8, 14.4. HRMS (FAB) m/z Calcd for C30H44O5Na: 507.3087. Found: 507.3091.
(3β)-(3-Methyloxymethyloxy)-androst-5-en-17-one, cyclic-17-1,2-ethanediyl actal (16)
Steroid 1526 (3 g, 9 mmol) was converted into steroid 16 using the procedure reported for the preparation of steroid 9b. Flash column chromatography (silica gel eluted with 15–20% EtOAc in hexanes) gave product 16 (3.1 g, 91%): mp 94–96 °C; IR νmax 2926, 2893, 2823, 1667, 1466, 1437, 1381, 1305, 1277 cm−1; 1H NMR δ 5.33 (d, 1H, J = 5.2 Hz), 4.66 (s, 2H), 4.00–3.78 (m, 4H), 3.36 (m, 1H), 3.34 (s, 3H), 0.99 (s, 3H), 0.83 (s, 3H); 13C NMR δ 140.6, 121.4, 119.4, 94.6, 76.8, 65.1, 64.5, 55.1, 50.5, 49.9, 45.6, 39.5, 37.2, 36.7, 34.1, 32.1, 31.2, 30.5, 28.8, 22.7, 20.4, 19.3, 14.1. Anal. (C23H36O4) C, H.
(3β)-(3-Methyloxymethyloxy)-androst-5-ene-7,17-dione, cyclic-17-1,2-ethanediyl acetal (17)
A mixture of steroid 16 (2.26 g, 6 mmol), 70% aqueous t: BuOOH (4.32 mL, 30 mmol), NaOCl2 (813 mg, 7.2 mmol) in premixed acetonitrile (60 mL) and water (20 mL) was heated at 50 °C for 36 h. The reaction was cooled, poured into aqueous 10% Na2SO3 (100 mL) and stirred for 0.5 h. The product was extracted into Et2O (100 mL × 4) and the combined extracts were washed with brine, dried and concentrated to give a viscous liquid which was purified by flash column chromatography (silica gel eluted with 15–25% EtOAc in hexanes) to yield recovered steroid 16 (450 mg, 20%) and product 17 (800 mg, 34%): mp 136–138 °C; IR νmax 2946, 2880, 1668, 1629, 1461, 1382, 1295, 1215 cm−1; 1H NMR δ 5.70 (s, 1H), 4.69 (dd, 2H, J = 8.0, 6.9 Hz), 4.00–3.80 (m, 4H), 3.56 (m, 1H), 3.38 (s, 3H), 1.20 (s, 3H), 0.87 (s, 3H); 13C NMR δ 201.2, 165.3, 125.9, 118.5, 94.9, 75.5, 65.1, 64.3, 55.2, 49.8, 46.0, 45.2, 44.3, 39.3, 38.3, 36.2, 34.0, 29.5, 28.5, 25.0, 20.5, 17.2, 14.3. Anal. (C23H34O5) C, H.
(3β,5α)-(3-Methyloxymethyloxy)-androstane-7,17-dione, cyclic-17-1,2-ethanediyl acetal (18a)
Steroid 17 (586 mg, 1.5 mmol), 10% Pd/C (300 mg) and EtOAc (80 mL) were placed in a Parr hydrogenation flask and hydrogenated (50 psi) for 18 h. The Pd/C was filtered under vacuum through a pad of Celite 454 ® on a sintered glass funnel. The filter-cake was washed with EtOAc. The combined filtrate and washings were concentrated to give an off-white solid which was purified by flash column chromatography (silica gel eluted with 15–25% ethyl acetate in hexanes) to give product 18a (471 mg, 80%); mp 117–119 °C; IR νmax 2944, 2882, 1708, 1448, 1379, 1292, 1223 cm−1; 1H NMR δ 4.67 (s, 2H), 4.00–3.76 (m, 4H), 3.50 (m, 1H), 3.36 (s, 3H), 1.08 (s, 3H), 0.84 (s, 3H); 13C NMR δ 210.9, 118.6, 94.7, 75.7, 65.2, 64.4, 55.1, 50.0, 46.4, 45.9, 45.7, 43.4, 36.2, 36.0, 35.2, 34.1, 29.7, 28.4, 23.8, 21.3, 14.4, 11.7. Anal. (C23H36O5) C, H.
(3β,5α)-7-Hydroxy-3-(Methyloxymethyloxy)-androstan-17-one, cyclic-17-1,2-ethanediyl acetal (18b)
Steroid 18a (498 mg, 1.27 mmol) was converted into an inseparable mixture of the 7α,7β-hydroxysteroids 18b using the procedure reported for the preparation of steroid 10a. Filtration through a short column of silica gel eluted with 40% EtOAc in hexanes gave product 18b (431 mg, 86%) which was then converted without characterization into the separable steroids 18c and 18d.
(3β,5α,7β)-7-Benzyloxy-3-(Methyloxymethyloxy)-androstan-17-one, cyclic-17-1,2-ethanediyl acetal (18c) and (3β,5α,7α)-7-Benzyloxy-3-(Methyloxymethyloxy)-androstan-17-one, cyclic-17-1,2-ethanediyl acetal (18d)
Steroid 18b (431 mg, 1.09 mmol) was converted into products 18c and 18d using the procedure reported for the benzylation of steroid 10b. Flash column chromatography (silica gel eluted with 10–35% EtOAc in hexanes) gave product 18c (120 mg, 23%), product 18d (240 mg, 45%) and recovered steroid 18b (120 mg, 23%). Product 18d eluted from the column before product 18c.
18c
oil; IR νmax 2936, 1454, 1307 cm−1; 1H NMR δ 7.40–7.19 (m, 5H), 4.68 (s, 2H), 4.55 (d, 1H, J = 11 Hz), 4.34 (d, 1H, J = 11 Hz), 4.00–3.79 (m, 4H), 3.49 (m, 1H), 3.37 (s, 3H), 3.13 (m, 1H), 0.86 (s, 3H), 0.84 (s, 3H); 13C NMR δ 138.9, 128.3 (2 × C), 127.9 (2 × C), 127.3, 119.0, 94.6, 82.7, 76.1, 70.4, 65.2, 64.5, 55.1, 52.9, 50.2, 46.7, 42.0, 41.5, 37.0, 35.2, 35.1, 34.3, 33.8, 30.4, 28.7, 25.4, 20.9, 14.7, 12.4. Anal. (C30H44O5) C, H.
18d
oil; IR νmax 2935, 1453, 1306 cm−1; 1H NMR δ 7.43–7.20 (m, 5H), 4.68 (s, 2H), 4.57 (d, 1H, J = 12 Hz), 4.32 (d, 1H, J = 11.8 Hz), 3.97–3.76 (m, 4H), 3.48 (m, 1H), 3.46 (b, s, 1H), 3.37 (s, 3H), 0.81 (s, 3H), 0.81 (s, 3H); 13C NMR δ 139.5, 128.2 (2 × C), 127.4 (2 × C), 127.2, 119.4, 94.6, 76.4, 74.5, 70.4, 65.1, 64.6, 55.1, 46.3, 46.0, 44.2, 40.4, 37.2, 36.8, 35.7, 35.0, 34.3, 31.6, 30.4, 28.7, 22.4, 20.6, 14.1, 11.4. Anal. (C30H44O5) C, H.
(3β,5α,7β)-7-Benzyloxy-3-hydroxyandrostan-17-one (19a)
Steroid 18c (120 mg, 0.25 mmol) was converted into steroid 19a using the procedure reported for the preparation of compound ent-4. Flash column chromatography (silica gel eluted with 30–40% EtOAc in hexanes) gave product 19a (90 mg, 91%): mp 175–177 °C; IR νmax 3447, 2930, 2855, 1735, 1497, 1453, 1405, 1362, 1202 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.64 (d, 1H, J = 11 Hz), 4.38 (d, 1H, J = 11Hz), 3.60 (m, 1H), 3.23 (m, 1H), 0.87 (s, 3H), 0.86 (s, 3H); 13C NMR δ 221.6, 138.5, 128.4 (2 × C), 127.7 (2 × C), 127.5, 81.9, 70.9, 70.2, 53.0, 51.3, 48.4, 41.8, 40.9, 37.9, 36.9, 36.1, 35.2, 33.6, 31.6, 31.4, 24.9, 20.8, 14.1, 12.4. Anal. (C26H36O3) C, H
(5α,7β)-7-Benzyloxyandrostane-3,17-dione (19b)
Steroid 19a (71 mg, 0.18 mmol) was converted into steroid 19b using the procedure reported for the preparation of steroid 14b. Flash column chromatography (silica gel eluted with 25% EtOAc in hexanes) gave product 19b (61 mg, 86%): mp 181–183 °C; IR νmax 2945, 2921, 2856, 1733, 1716, 1454, 1367, 1289, 1257, 1227 cm−1; 1H NMR δ 7.40–7.24 (m, 5H), 4.63 (d, 1H, J = 11 Hz), 4.40 (d, 1H, J = 11 Hz), 3.26 (m, 1H), 1.07 (s, 3H), 0.90 (s, 3H); 13C NMR δ 221.2, 210.9, 138.3, 128.4 (2 × C), 127.8 (2 × C), 127.6, 81.5, 70.5, 52.2, 51.2, 48.3, 44.2, 43.7, 40.8, 38.2, 37.9, 36.0, 35.3, 33.8, 31.5, 24.9, 21.2, 14.1, 11.6. Anal. (C26H34O3) C, H.
(8α,9β,10α,13α,14β)-Androst-5-ene-3,17-dione, cyclic-3,17-bis(1,2-ethanediyl acetal) (21a)
Compound 2018 (1.6 g, 5.6 mmol) was converted into compound 21a using the procedure reported for the preparation of compound 9a. Flash column chromatography (silica gel eluted with 15–25% EtOAc in hexanes) gave product 21a (1.74 g, 83%): mp 158–160 °C; IR νmax 2943, 2885, 1431, 1381, 1305 cm−1; 1H NMR δ 5.34 (m, 1H), 4.00–3.80 (m, 8H), 1.04 (s, 3H), 0.86 (s, 3H); 13C NMR δ 140.0, 121.8, 119.3, 109.3, 65.0, 64.4, 64.3, 64.1, 50.4, 49.4, 45.6, 41.7, 36.6, 36.2, 34.1, 32.1, 31.0, 30.9, 30.5, 22.7, 20.3, 18.7, 14.1. Anal. (C23H34O4) C, H.
(8α,9β,10α,13α,14β)-Androst-5-ene-3,7,17-trione, cyclic-3,17-bis(1,2-ethanediyl acetal) (21b)
Compound 21a (1.73g, 4.62 mmol) was converted into compound 21b using the procedure reported for the preparation of steroid 17. Flash column chromatography (silica gel eluted with 15–25% EtOAc in hexanes) gave recovered compound 21a (500 mg, 28%) and product 21b (560 mg, 31 %): mp 198–200 °C; IR νmax 2953, 2882, 1672, 1634, 1457, 1383, 1295 cm−1; 1H NMR δ 5.66 (s, 1H), 4.03–3.78 (m, 8H), 2.69 (d, 1H, J = 14.8 Hz), 1.22 (s, 3H), 0.88 (s, 3H); 13C NMR δ 201.2, 164.7, 126.5, 118.6, 108.8, 65.1, 64.5, 64.5, 49.5, 46.2, 45.3, 44.4, 41.7, 38.2, 35.5, 34.1, 31.0, 29.6, 25.1, 20.6, 17.0, 14.4. Anal. (C23H32O5) C, H.
(5β,8α,9β,10α,13α,14β)-Androstane-3,7,17-trione, cyclic-3,17-bis(1,2-ethanediyl acetal) (22a)
Compound 21b (500 mg, 1.28 mmol) was converted into compound 22a using the procedure reported for the preparation of steroid 18a. Flash column chromatography (silica gel eluted with 20–30% EtOAc in hexanes) gave product 22a (380 mg, 76%): mp 208–210 °C; IR νmax 2952, 2880, 1705, 1456, 1386, 1293 cm−1; 1H NMR δ 4.00–3.70 (m, 8H), 1.08 (s, 3H), 0.84 (s, 3H); 13C NMR δ 210.8, 118.6, 108.6, 65.1, 64.4, 64.3, 64.1, 54.7, 50.0, 45.7, 45.6, 45.2, 43.4, 37.7, 35.9, 35.2, 34.1, 31.1, 29.7, 23.8, 21.3, 14.4, 10.9. Anal. (C23H34O5) C, H.
(5β,8α,9β,10α,13α,14β)-7-Hydroxyandrostane-3,17-dione, cyclic-3,17-bis(1,2-ethanediyl acetal) (22b)
Compound 22a (140 mg, 0.36 mmol) dissolved in 2-propanol (30 mL) and Raney nickel were placed in a Parr hydrogenation flask and hydrogenated (H2, 60 psi) for 18 h. The Raney nickel was removed by filtration under vacuum through Celite 454 ® in a sintered glass funnel. The Celite 454 ® was washed with methanol and the filtrate was evaporated to yield a solid product which was purified by flash column chromatography (silica gel eluted with 40% EtOAc in hexanes) to give the inseparable mixture of 7α- and 7β-alcohol products 22b (136 mg, 96%). This product was not characterized.
(5β,7β,8α,9β,10α,13α,14β)-7-Benzyloxyandrostane-3,17-dione, cyclic-3,17-bis(1,2-ethanediyl acetal) (22c) and (5β,7α,8α,9β,10α,13α,14β)-7-Benzyloxyandrostane-3,17-dione, cyclic-3,17-bis(1,2-ethanediyl acetal) (22d)
The inseparable epimeric products 22b (130 mg, 0.33 mmol) were converted into separable compounds 22c (35 mg, 22%) and 22d (80 mg, 50%) using the procedure reported for the preparation of steroids 18c and 18d from the inseparable 7α- and 7β-alcohols 18b.
22c
mp 141–143 °C; IR νmax 2943, 2872, 1496, 1456, 1362, 1306, 1286, 1245 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.57 (d, J = 12.1 Hz), 4.33 (d, J = 12.4 Hz), 3.96–3.78 (m, 8H), 3.45 (b s, 1H), 0.81 (s, 6H); 13C NMR: 139.7, 128.1 (2 × C), 127.4 (2 × C), 127.0, 119.4, 109.2, 74.5, 70.4, 65.0, 64.5, 64.0 (2 × C), 45.9, 45.9, 44.1, 40.3, 37.6, 36.1, 35.7, 35.5, 34.2, 31.4, 31.2, 30.4, 22.3, 20.5, 14.0, 10.5. Anal. (C30H42O5) C, H.
22d
mp 145–147 °C; IR νmax 2943, 2871, 1586, 1454, 1361, 1307, 1205 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.54 (d, 1H, J = 11 Hz), 4.34 (d, 1H, J = 11Hz), 3.96–3.80 (m, 8H), 3.15 (m, 1H), 0.86 (s, 3H), 0.84 (s, 3H); 13C NMR δ 138.8, 128.3 (2 × C), 127.8 (2 × C), 127.7, 118.9, 109.1, 82.7, 70.4, 65.1, 64.5, 64.1 (2 × C), 52.4, 50.4, 46.6, 41.4, 40.8, 37.8, 35.9, 35.1, 34.3, 33.6, 31.1, 30.4, 25.4, 20.9, 14.7, 11.5. Anal. (C30H42O5) C, H.
(5β,7α,8α,9β,10α,13α,14β)-7-Benzyloxyandrostane-3,17-dione (23)
Compound 22d (193 mg, 0.4 mmol) was converted into compound 23 using the procedure reported for the preparation of steroid 4. Flash column chromatography (silica gel eluted with 30–40% EtOAc in hexanes) gave product 23 (140 mg, 89%): mp 183–185 °C; IR 2921, 2855, 1733, 1716, 1453, 1367 cm−1; 1H NMR δ 7.40–7.20 (m, 5H), 4.63 (d, 1H, J = 10.7 Hz), 4.40 (d, 1H, J = 11 Hz), 3.26 (m, 1H), 1.07 (s, 3H), 0.91 (s, 3H); 13C NMR 221.2, 210.9, 138.3, 128.4 (2 × C), 127.8 (2 × C), 127.6, 81.4, 70.4, 52.2, 51.2, 48.3, 44.2, 43.7, 40.8, 38.2, 37.9, 36.0, 35.3, 33.8, 31.5, 24.9, 21.2, 14.1, 11.6. Anal. (C26H34O3) C, H.
[35S]-TBPS Binding Methods
The methods used were as described previously.27
Xenopus Oocyte Electrophysiological Methods
cRNA encoding rat GABAA receptor subunits was injected into stage V-VI oocytes harvested from sexually mature female X. laevis frogs (Xenopus One, Northland, MI). Frogs were anesthetized with 0.1% tricane (3-aminobenzoic acid ethyl ester), and oocytes obtained by partial ovariectomy. The follicular layer was removed from oocytes by shaking for 20 min at 37° C in 2 mg/mL collagenase dissolved in calcium-free solution containing 96 mM NaCl, 2 mM KCl, 1 mM MgCl2, 5 mM HEPES, pH 7.4. Capped RNA for α1, β2, and γ2L subunits was prepared in vitro (mMESSAGE mMachine kit, Ambion, Austin, TX) from linearized pBluescript vectors containing subunit coding regions. The α1 Q241L mutation was introduced as described previously.20 Subunit RNA was injected in equal parts (20-40 ng total RNA), after which oocytes were incubated at 18° C in ND96 solution containing 96 mM NaCl, 2 mM KCl, 2 mM CaCl2, 1 mM MgCl2, 5 mM HEPES, pH 7.4. ND96 was supplemented with pyruvate (5 mM), penicillin (100 U/mL), streptomycin (100 μg/mL), and gentamycin (50 μg/mL).
Oocyte responses were recorded 2-5 days following RNA injection. GABA currents were recorded using two-electrode voltage clamp (OC725C amplifier, Warner Instruments) at a membrane potential of −70 mV. The bath solution was ND96 solution, and glass recording pipettes (~1 Ma resistance) were filled with 3 M KCl. Compounds were applied to oocytes using a multibarrel pipette with a common output tip. Data acquisition and analysis were performed with pCLAMP software (Molecular Devices, Sunnyvale, CA). Statistical differences were assessed with 1-tailed or 2-tailed paired or unpaired t-tests as indicated.
Tadpole Behavioral Methods
The methods used were as described previously.27
Supplementary Material
Acknowledgement
This work was supported by NIH Grant GM47969 (D. F. C., A. S. E., C. F. Z., J.H.S.) and the Bantly Foundation (C. F. Z). A. S. E. is a consultant for Sage Therapeutics. D. F. C. and C. F. Z. are members of the Scientific Advisory Board of Sage Therapeutics and may receive income based on equity holdings in Sage Therapeutics. Washington University may receive income based on a license of related technology by the University to Sage Therapeutics. Sage Therapeutics did not support this work.
Abbreviations
- GABA
γ-aminobutyric acid
- GABAA
γ-aminobutyric acid type A
- [35S]TBPS
[35S]-tert-butylbicyclophosphorothionate
- SAR
structure-activity relationships
- LRR
loss of righting reflex
- LSR
loss of swimming reflex
Footnotes
Supporting Information Available: Table of elemental analysis results. This material is available free of charge via the Internet at http://pubs.acs.org.
References
- 1.Veleiro AS, Burton G. Structure-activity relationships of neuroactive steroids acting on the GABAA receptor. Curr. Med. Chem. 2009;16:455–472. doi: 10.2174/092986709787315522. [DOI] [PubMed] [Google Scholar]
- 2.Belelli D, Lambert JJ. Neurosteroidsendogenous regulators of the GABAA receptor. Nat. Rev. Neurosci. 2005;6:565–575. doi: 10.1038/nrn1703. [DOI] [PubMed] [Google Scholar]
- 3.Akk G, Covey DF, Evers AS, Mennerick S, Zorumski CF, Steinbach JH. Kinetic and structural determinants for GABA-A receptor potentiation by neuroactive steroids. Curr. Neuropharmacol. 2010;8:18–25. doi: 10.2174/157015910790909458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lambert JJ, Cooper MA, Simmons RD, Weir CJ, Belelli D. Neurosteroidsendogenous allosteric modulators of GABAA receptors. Psychoneuroendocrinology. 2009;34(Suppl 1):S48–S58. doi: 10.1016/j.psyneuen.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 5.Zorumski CF, Mennerick S, Isenberg KE, Covey DF. Potential clinical uses of neuroactive steroids. IDrugs. 2000;3:1053–1063. [PubMed] [Google Scholar]
- 6.Reddy DS. Neurosteroidsendogenous role in the human brain and therapeutic potentials. Prog. Brain Res. 2010;186:113–137. doi: 10.1016/B978-0-444-53630-3.00008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hosie AM, Wilkins ME, da Silva HMA, Smart TG. Endogenous neurosteroids regulate GABAA receptors through two discrete transmembrane sites. Nature. 2006;444:486–489. doi: 10.1038/nature05324. [DOI] [PubMed] [Google Scholar]
- 8.Akk G, Li P, Bracamontes J, Reichert DE, Covey DF, Steinbach JH. Mutations of the GABA-A receptor α1 subunit M1 domain reveal unexpected complexity for modulation by neuroactive steroids. Mol. Pharmacol. 2008;74:614–627. doi: 10.1124/mol.108.048520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hosie AM, Clarke L, da Silva H, Smart TG. Conserved site for neurosteroid modulation of GABAA receptors. Neuropharmacology. 2009;56:149–154. doi: 10.1016/j.neuropharm.2008.07.050. [DOI] [PubMed] [Google Scholar]
- 10.Hamilton NM. Interactions of steroids with the GABAA receptor. Curr. Top. Med. Chem. 2002;2:887–902. doi: 10.2174/1568026023393570. [DOI] [PubMed] [Google Scholar]
- 11.Phillipps GH. Structure-activity relationships in steroidal anesthetics. J. Steroid Biochem. 1975;6:607–613. doi: 10.1016/0022-4731(75)90041-2. [DOI] [PubMed] [Google Scholar]
- 12.Wittmer LL, Hu Y, Kalkbrenner M, Evers AS, Zorumski CF, Covey DF. Enantioselectivity of steroid-induced γ-aminobutyric acidA receptor modulation and anesthesia. Mol. Pharmacol. 1996;50:1581–1586. [PubMed] [Google Scholar]
- 13.Covey DF, Nathan D, Kalkbrenner M, Nilsson KR, Hu Y, Zorumski CF, Evers AS. Enantioselectivity of pregnanolone-induced γ-aminobutyric acidA receptor modulation and anesthesia. J. Pharmacol. Exp. Ther. 2000;293:1009–1016. [PubMed] [Google Scholar]
- 14.Katona BW, Krishnan K, Cai ZY, Manion BD, Benz A, Taylor A, Evers AS, Zorumski CF, Mennerick S, Covey DF. Neurosteroid analogues. 12. Potent enhancement of GABA-mediated chloride currents at GABAA receptors by entandrogens. Eur. J. Med. Chem. 2008;43:107–113. doi: 10.1016/j.ejmech.2007.02.017. [DOI] [PubMed] [Google Scholar]
- 15.Shu HJ, Zeng CM, Wang C, Covey DF, Zorumski CF, Mennerick S. Cyclodextrins sequester neuroactive steroids and differentiate mechanisms that rate limit steroid actions. Br. J. Pharmacol. 2007;150:164–175. doi: 10.1038/sj.bjp.0706973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeng CM, Manion BD, Benz A, Evers AS, Zorumski CF, Mennerick S, Covey DF. Neurosteroid analogues. 10. The effect of methyl group substitution at the C-6 and C-7 positions on the GABA modulatory and anesthetic actions of (3α,5α)- and (3α,5β)-3-hydroxypregnan-20-one. J. Med. Chem. 2005;48:3051–3059. doi: 10.1021/jm049027+. [DOI] [PubMed] [Google Scholar]
- 17.Katona BW, Rath NP, Anant S, Stenson WF, Covey DF. Enantiomeric deoxycholic acid-total synthesis, characterization, and preliminary toxicity toward colon cancer cell lines. J. Org. Chem. 2007;72:9298–9307. doi: 10.1021/jo701559q. [DOI] [PubMed] [Google Scholar]
- 18.Nilsson KR, Zorumski CF, Covey DF. Neurosteroid analogues. 6. The synthesis and GABAA receptor pharmacology of enantiomers of dehydroepiandrosterone sulfate, pregnenolone sulfate, and (3α,5β)-3-hydroxypregnan-20-one sulfate. J. Med. Chem. 1998;41:2604–2613. doi: 10.1021/jm980148h. [DOI] [PubMed] [Google Scholar]
- 19.Schreifels JA, Maybury PC, Swartz WE., Jr. Comparison of the activity and lifetime of Raney nickel and nickel boride in the hydrogenation of various functional groups. J. Org. Chem. 1981;46:1263–1269. [Google Scholar]
- 20.Bracamontes JR, Steinbach JH. Steroid interaction with a single potentiating site is sufficient to modulate GABA-A receptor function. Mol. Pharmacol. 2009;75:973–981. doi: 10.1124/mol.108.053629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chisari M, Eisenman LN, Krishnan K, Bandyopadhyaya AK, Wang C, Taylor A, Benz A, Covey DF, Zorumski CF, Mennerick S. The Influence of Neuroactive Steroid Lipophilicity on GABAA Receptor Modulation-Evidence for a Low-Affinity Interaction. J. Neurophysiol. 2009;102:1254–1264. doi: 10.1152/jn.00346.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chisari M, Eisenman LN, Covey DF, Mennerick S, Zorumski CF. The sticky issue of neurosteroids and GABAA receptors. Trends Neurosci. 2010;33:299–306. doi: 10.1016/j.tins.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang M, He Y, Eisenman LN, Fields C, Zeng CM, Mathews J, Benz A, Fu T, Zorumski E, Steinbach JH, Covey DF, Zorumski CF, Mennerick S. 3β-Hydroxypregnane steroids are pregnenolone sulfate-like GABAA receptor antagonists. J. Neurosci. 2002;22:3366–3375. doi: 10.1523/JNEUROSCI.22-09-03366.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li P, Bracamontes J, Katona BW, Covey DF, Steinbach JH, Akk G. Natural and enantiomeric etiocholanolone interact with distinct sites on the rat α1β2γ2L GABAA receptor. Mol. Pharmacol. 2007;71:1582–1590. doi: 10.1124/mol.106.033407. [DOI] [PubMed] [Google Scholar]
- 25.Hawkins PCD, Skillman AG, Nicholls A. Comparison of shape-matching and docking as virtual screening tools. J. Med. Chem. 2007;50:74–82. doi: 10.1021/jm0603365. [DOI] [PubMed] [Google Scholar]
- 26.Shen Y, Burgoyne DL. Efficient synthesis of IPL576,092: a novel anti-asthma agent. J. Org. Chem. 2002;67:3908–3910. doi: 10.1021/jo0108717. [DOI] [PubMed] [Google Scholar]
- 27.Jiang X, Manion BD, Benz A, Rath NP, Evers AS, Zorumski CF, Mennerick S, Covey DF. Neurosteroid analogues. 9. Conformationally constrained pregnanes-structure-activity studies of 13,24-cyclo-18,21-dinorcholane analogues of the GABA modulatory and anesthetic steroids (3α,5α)- and (3α,5β)-3-hydroxypregnan-20-one. J. Med. Chem. 2003;46:5334–5348. doi: 10.1021/jm030302m. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.