Abstract
Purpose:
Tumor bleeding continues to remain a challenge in an oncological setting, and radiotherapy has been studied as a local hemostatic agent. We studied the role of local radiotherapy in controlling bleeding at our center.
Materials and Methods:
We reviewed 25 treated cases (cancer urinary bladder: 12, lung cancer: 5, cervical cancer: 4, uterine cancer: 1, rectal cancer: 2, schwanoma: 1) at our center from March 2008 to December 2010. All patients had either an advanced or recurrent disease. Radiotherapy schedule was either 20 Gray in 5 fractions or 15 Gray in 5 fractions and was delivered with Cobalt 60.
Results and Conclusion:
Of 25 patients, 22 (88%) responded, and there was complete cessation of bleeding. Both 15 Gray and 20 Gray dose schedule had equal efficacy. Treatment was well tolerated without any intermission. Radiotherapy is a safe and effective option in controlling tumor bleeding.
Keywords: Hemostasis, Hypofractionation, Radiotherapy
INTRODUCTION
Bleeding occurs in approximately 6–10% of the patients with advanced cancer,[1] and remains a challenge because of the failure of local healing pathways. In some patients, it may be the immediate cause of death. Hemorrhage may manifest in a variety of ways, including hematemesis, hematochezia, melena, hemoptysis, hematuria, epistaxis, vaginal bleeding or ulcerated skin lesions. Besides non-adherent dressings, hemostatic dressings, hemostatic agents (epinephrine, acetone, thrombin/thromboplastin, etc.), surgery (vessel ligation, tissue resection), endoscopy, interventional radiology (transcutaneous arterial embolization, transcutaneous arterial balloons), radiotherapy remains a potential and practical option in controlling the local tumor bleeding at various anatomic sites. External beam radiotherapy has been used in various situations where other local therapies have failed, producing durable response rates, and has been tried as a first-line treatment for controlling active bleeding in tumors. It has been used in various fractionation schedules (hypofractionated or conventional). We have been treating selective patients with radiotherapy at our Institute and, in this study, we present our experience where radiotherapy has been instituted as the local hemostatic agent in various situations.
MATERIALS AND METHODS
We reviewed 25 patients who received palliative hemostatic radiotherapy between March 2008 and December 2010 at our center. All patients were registered in the Regional Cancer Centre and had either an advanced stage disease or failure to primary treatment or recurrence of disease. In all patients, the cause of local bleeding was direct invasion of tumor. A complete hemogram including platelet count and coagulogram was performed in all patients, and was found to be normal. Bleeding diathesis was hence ruled out in these patients. No patient was on any anticoagulant therapy like warfarin or heparin. The primary sites that were treated were urinary bladder (12), cervix (4), lung (5), uterus (1), rectum (2)and schwanoma (1). All patients received external beam radiotherapy with Telecobalt 60 with energy of 1.25 MV. A hypofractionated dose of 15 Grays in five fractions was delivered to 15 patients and 20 Grays in five fractions to 10 patients. Response was assessed at the end of treatment. Complete cessation of bleeding for at least 1 month was considered response to therapy. All patients were reviewed weekly after the completion of radiotherapy. They received supportive care, and management of other symptoms was done as per the needs of the individual patient.
RESULTS AND OBSERVATIONS
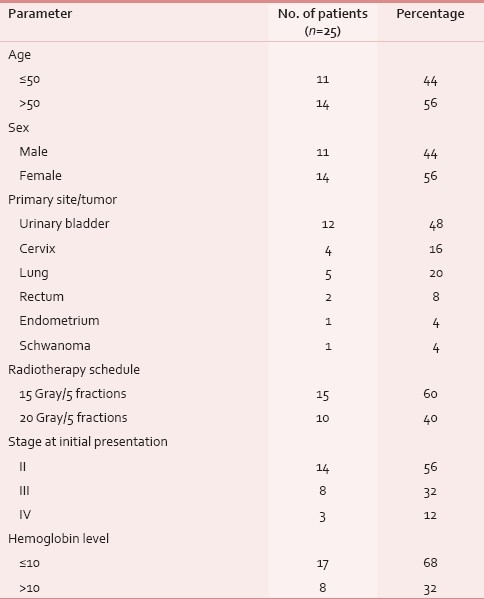
We reviewed 25 patients presenting with tumor bleed. Depending on the primary site and stage of the disease, all patients had more than one symptom besides bleeding. As per the involvement of the primary site, hemorrhage was found in the form of haematuria (12 patients), bleeding per vaginum (6 patients), hemoptysis (6 patients) and bleeding per rectum (2 patients). The patient with schwanoma had lung metastasis presenting as hemoptysis. Table 1 gives the baseline parameters of patients in the study.
Table 1.
Baseline clinical parameters of the patients
All patients had normal blood counts and normal coagulogram and no patient was on any form of anticoagulant therapy. Of the total of 25 patients reviewed, 22 had complete cessation of bleeding (88%). In no patient intention to treat was cure or elimination of disease; rather, it was palliative.
DISCUSSION
Tumor bleeding continues to remain a significant cause of morbidity and mortality in various cancers. At our center, we receive many such patients, but radiotherapy is infrequently used in achieving hemostasis. In this study, radiotherapy controlled hematuria in 11 of 12 patients (91%) in bladder cancer. Other studies have found that external beam radiotherapy may be successful in controlling bleeding in up to 59% of cases of hematuria from bladder cancer.[2] These results have encouraged us to consider radiation therapy in bladder carcinoma in such situations.
The response for cessation of hemoptysis with radiation has also been documented in various studies. A single fraction of 10 Grays has been shown to be as effective as multiple fractions in patients with hemoptysis due to lung cancer,[3] and the response rates have been found to be up to 80%.[4] In our study, four out of five (80%) patients had complete cessation of hemoptysis. We suggest radiotherapy should be considered as first line of treatment in advanced or recurrent lung cancers in patients who present with hemoptysis, and radiation therapy can improve quality of life in such patients. Radiotherapy should also be considered for bleeding from cancerous lesions of the vagina[5] and skin.[6] External beam radiotherapy may be successful in controlling bleeding in up to 85% of cases of rectal bleeding. Only two patients with rectal cancer were included in this study who had recurrence of disease and responded. All patients of rectal cancer who were started on neoadjuvant radiotherapy were not included.
Although in our study the response rates are higher, we recommend that fractionation and dose of radiation should be tailored as per the performance score of the patient. Both schedules i.e 15 Grays in five fractions and 20 Grays in five fractions were equally effective, which suggests that lesser dose is equally efficacious. All patients in the study tolerated radiation well and completed the 5-day treatment without any interruption.
Upper gastrointestinal hemorrhage from malignant disease is less amenable to radiotherapy. While radiotherapy can be useful in controlling bleeding from head and neck cancers, many of these patients have already received maximal doses of radiotherapy when they present with bleeding, therefore limiting further dose escalation.[7] Cancer of uterine cervix although the most common malignancy among females in India, is relatively rare in Kashmir. Of the four patients, bleeding per vaginum stopped in three (75%) patients.
The exact mechanism of radiation acting as a hemostatic agent is not known. Although malignancy itself is a prothrombotic state, antineoplastic treatments also enhance this state, more so locally where radiation is given. Radiotherapy might cause local thombus formation through various mechanisms such as it causes vascular endothelial injury as demonstrated by increase in the levels of von Willebrand factor. Antitumor therapy results in the release of a series of soluble mediators that can act on the endothelial cells by altering their normal antithrombotic and antiadhesive status.
On the basis of this study, we suggest that radiotherapy should be considered in controlling bleeding in advanced cancer that is directly related to tumor invasion. Short fractionation schedules should be preferred. Single or reduced fraction regimens appear to be as effective as multiple fractions in controlling bleeding.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pereira J, Mancini I, Bruera E. The management of bleeding in patients with advanced cancer. In: Portenoy RK, Bruera E, editors. Topics in Palliative Care. Vol. 4. New York: Oxford University Press; 2000. pp. 163–83. [Google Scholar]
- 2.Srinivasan V, Brown CH, Turner AG. A comparison of two radiotherapy regimens for the treatment of symptoms from advanced bladder cancer. Clin Oncol (R Coll Radiol) 1994;6:11–3. doi: 10.1016/s0936-6555(05)80362-0. [DOI] [PubMed] [Google Scholar]
- 3.Hoskin PJ. In: Radiotherapy in symptom management. 2nd ed. Macdonald N, Hanks GW, Macdonald N, editors. Oxford University Press: New York; 1998. pp. 278–80. [Google Scholar]
- 4.Brundage MD, Bezjak A, Dixon P, Grimard L, Larochelle M, Warde P, et al. The role of palliative thoracic radiotherapy in non-small cell lung cancer. Can J Oncol. 1996;6(Suppl 1):25–32. [PubMed] [Google Scholar]
- 5.Biswal BM, Lal P, Rath GK, Mohanti BK. Hemostatic radiotherapy in carcinoma of the uterine cervix. Int J Gynaecol Obstet. 1995;50:281–5. doi: 10.1016/0020-7292(95)02454-k. [DOI] [PubMed] [Google Scholar]
- 6.Miller CM, O’Neill A, Mortimer PS. Skin problems in palliative care: nursing aspects. In: Doyle D, Hanks GW, editors. Oxford Textbook of Palliative Medicine. New York: Oxford University Press; 1993. pp. 395–407. [Google Scholar]
- 7.MacDougall RH, Munro AJ, Wilson JA. Palliation in head and neck cancer. In: Doyle D, Hanks GW, editors. Oxford Textbook of Palliative Medicine. New York: Oxford University Press; 1993. pp. 422–33. (38). [Google Scholar]


